Unit 3 - Immunological factors in disease
24
Lecture 2 - Immune deficiency
The consequences of deficiencies of the immune system
include the followings:
1- Recurrent infections.
2- Autoimmunity.
3- Susceptibility to malignancy.
Primary ID
Secondary ID
Due to infection, drug therapy, malignancy and ageing.
Phagocyte deficiency
Leads to increased bacteria and fungi infection.
Complement deficiency
Leads to infection: Neisseria meningitides, Neisseria
gonorrhoeae, Haemophilus influenzae & Streptococcus
pneumonia
T lymphocytes deficiency leads to:
Bacterial infection (TB), fungi infection (Candida), viral
infection (CMV) & Protozoa infection (pneumocystis carini)
Antibody deficiency leads to
1- Bacterial infection (Staphylococcus aureus)
2- Viral infection (Enterovirus)
3- Protozoa infection (Giardia lamblia)
Presenting problems in immune deficiency
Recurrent infections
Warning signs of ID:
1)
Eight respiratory tract infection/ year in a child or more
than four respiratory tract infection/ year in an adult.
2)
More than one infection requiring hospital admission or
intravenous antibiotics.
3) Infection with unusual organisms
4) Infection at unusual sites
5) Chronic infection unresponsive to usual treatment
6) Early end organ damage (Bronchiectasis)
7) Family history of immune deficiency
Investigations:
1-Full blood count 2- white cell differential
3- Acute phase protein (C-reactive protein)
4-Liver function test 5-Renal function test
6-Urine dipstick 7-Serum Immunoglobulin
8- Protein electrophoresis 9- Microbiological test.
10- Virological test. 11- Radiological test.
If ID is suspected, patients should not receive live
vaccines because of the risk of vaccine – induced disease.
Primary Phagocyte Deficiencies:
Usually present with recurrent bacterial and fungal
infections affecting unusual sites and majority present in
childhood but milder forms may present in adults.
It includes: 1- Leukocyte adhesion deficiencies
2- Chronic granulomatous disease
3- Defects in cytkines and cytokines receptors
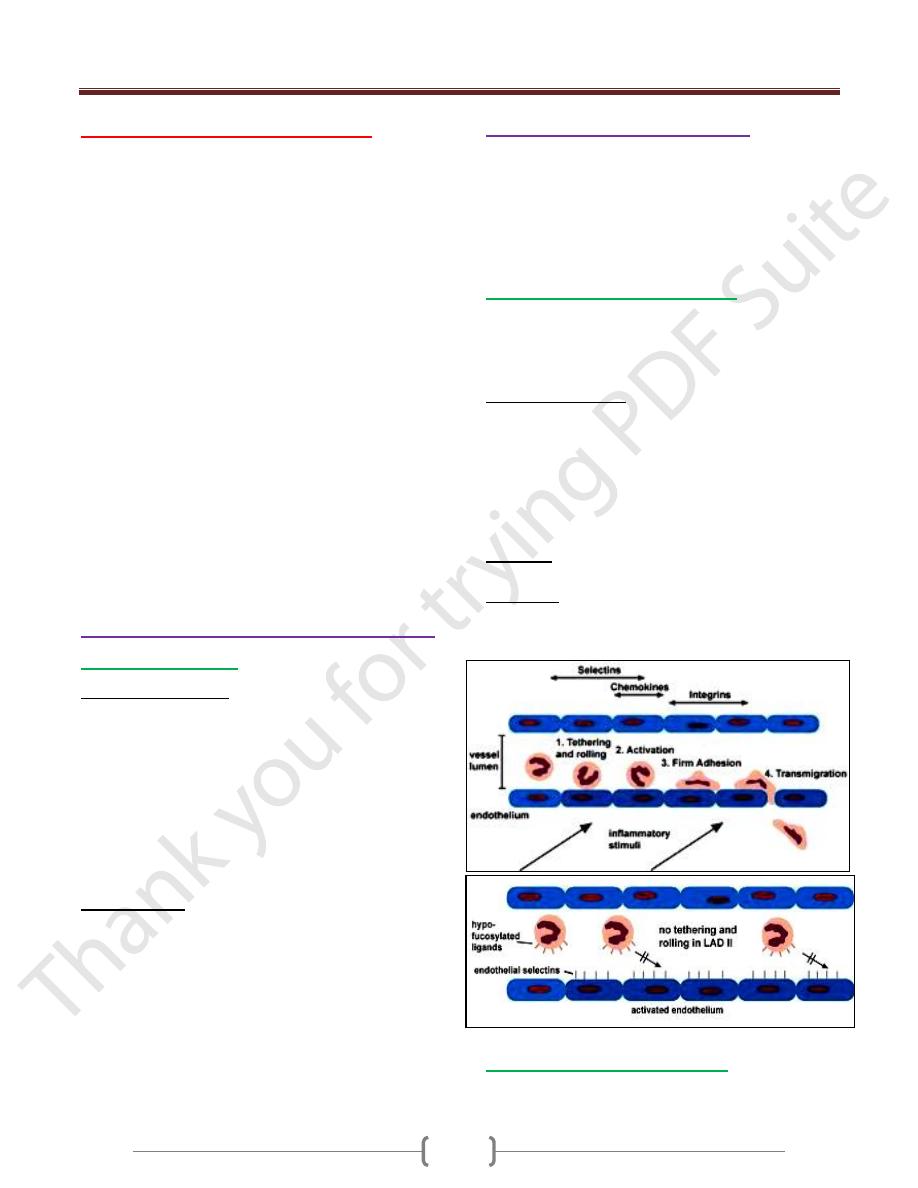
Leukocyte adhesion deficiencies:
It is an autosomal recessive disease.
These are disorders of phagocytes migration, where
failure to express adhesions molecules results in the
inability of phagocytes to exit the blood stream.
It is characterized by:
a) recurrent bacterial infections
b) Lack pus or neutrophils infiltration at site of infection
c) Peripheral neutrophils counts may be very high because of
the failure of mobilized N to exit blood vessels.
d) Infections are usually apparent from birth by presenting
infection is omphalitis with delayed separation of the
umbilical cord.
Diagnosis: by tests showed reduced or absent expression
of adhesions molecules on N.
Treatment: Prompt antibiotic therapy should be initiated
as early as possible in case of acute infection, bone
marrow transplantation and gene therapy.
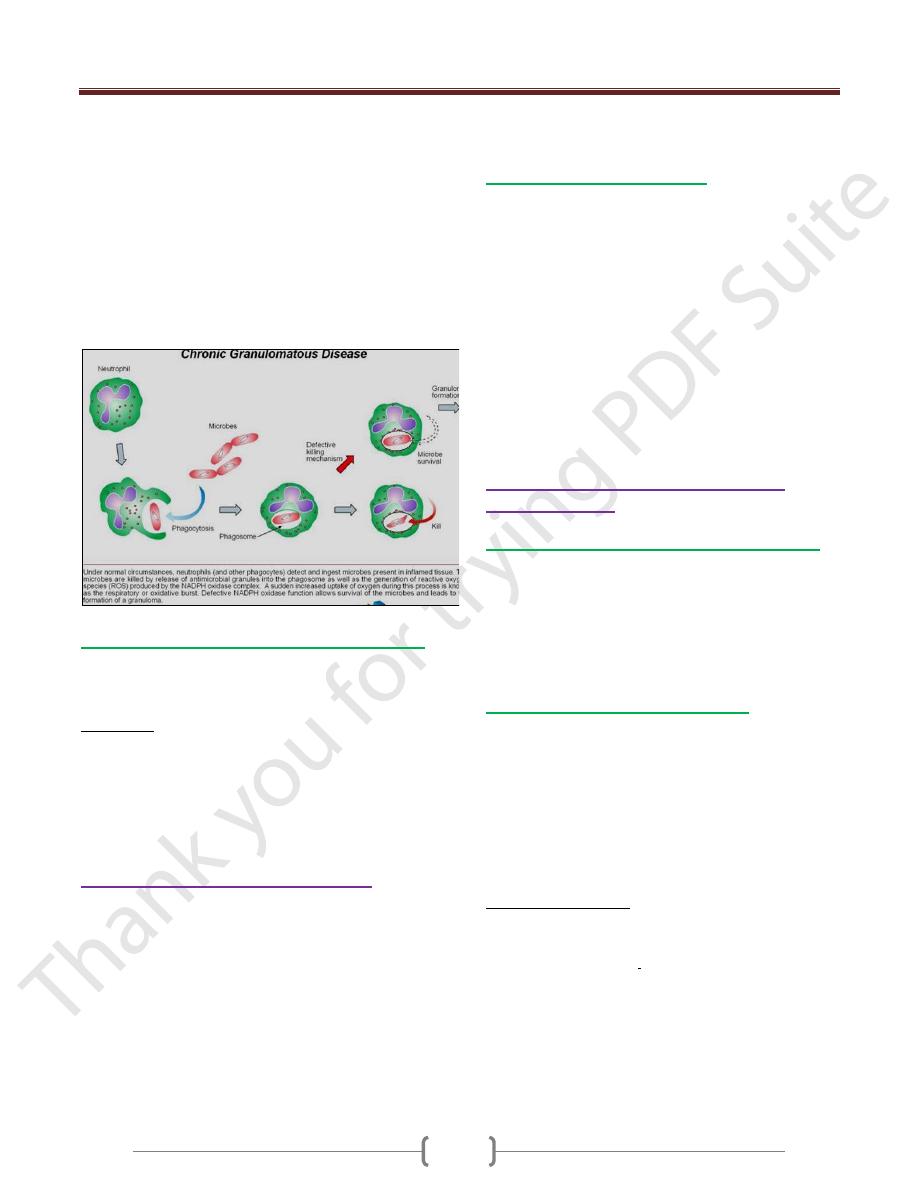
Chronic granulomatous disease:
This results from mutations in the genes encoding the
NADPH oxidase enzyme, causing a failure of oxidative
Unit 3 - Immunological factors in disease
25
killing. This may be demonstrated using the nitroblue
tetrazolium reduction test
The defect leads to susceptibility to catalase – positive
organisms such as Staphylococcus aureus
Intracellular killing of mycobacteria in macrophages is
also impaired.
Infections most commonly involve the lungs, lymph
nodes, soft tissues, bone, skin and urinary tract.
People with this condition often have areas of inflammation
(granulomas) in various tissues that can be damaging to
those tissues
Defects in cytokines and cytokines receptors:
Defect in cytokines such as IFN-γ, IL-12 or their receptors
results in failure of intracellular killing
Individuals are susceptible to mycobacterial infections
Treatment:
1- Intravenous antibiotics for treatment existing infection.
2 -surgical drainage of abscess.
3- Long term prophylaxis with antifungal agents
4- Specific treatment depends upon the nature of defect
and stem cell transplantation may be considered.
Complement pathways deficiencies
1) Genetic deficiency of classical complement pathway (C1,
C2, C4) are associated with high prevalence of
autoimmune disease particularly systemic lupus
erythematosus (SLE)
2) Deficiency in C9 increase Neisseria species infection
(Gonococcal & Meningococcal) and encapsulated bacteria
3) Deficiency of Mannose - binding lectin leads to increased
incidence of bacterial infection if subjected to additional
cause of immune compromise such as prematurity or
chemotherapy.
However, the important of this deficiency is not important
in healthy individuals.
Investigations and treatment:
1- Complement C3 and C4 measurements
2- CH50 test (Classical haemolytic pathway 50) or called
THC (Total Hemolytic Complement)
Sheep RBC coated with Abs + patient’s serum leads to
complete lysis RBC
There is no definitive treatment.
Patients should be vaccinated with meningococcal,
pneumococcal and H. influenzae vaccines in order to
boost their adaptive immune response.
Lifelong protective Penicillin to prevent infection
Family members should be screened for complement
deficiency.
Primary deficiencies of the adaptive
immune system
Combined B and T lymphocytes deficiency:
It is due to defect in lymphoid precursors
Results in combined failure of B and T cell Maturations
Cause recurrent bacterial, fungal and viral infections soon
after birth
Treated by stem cell transplantation or gene therapy still
under investigations.
Primary T lymphocytes deficiency
Characterized by recurrent viral, protozoal and fungal
infections
It is associated with defective Abs productions because of
the importance of Tcell in providing help to B cells
These disorders present in childhood
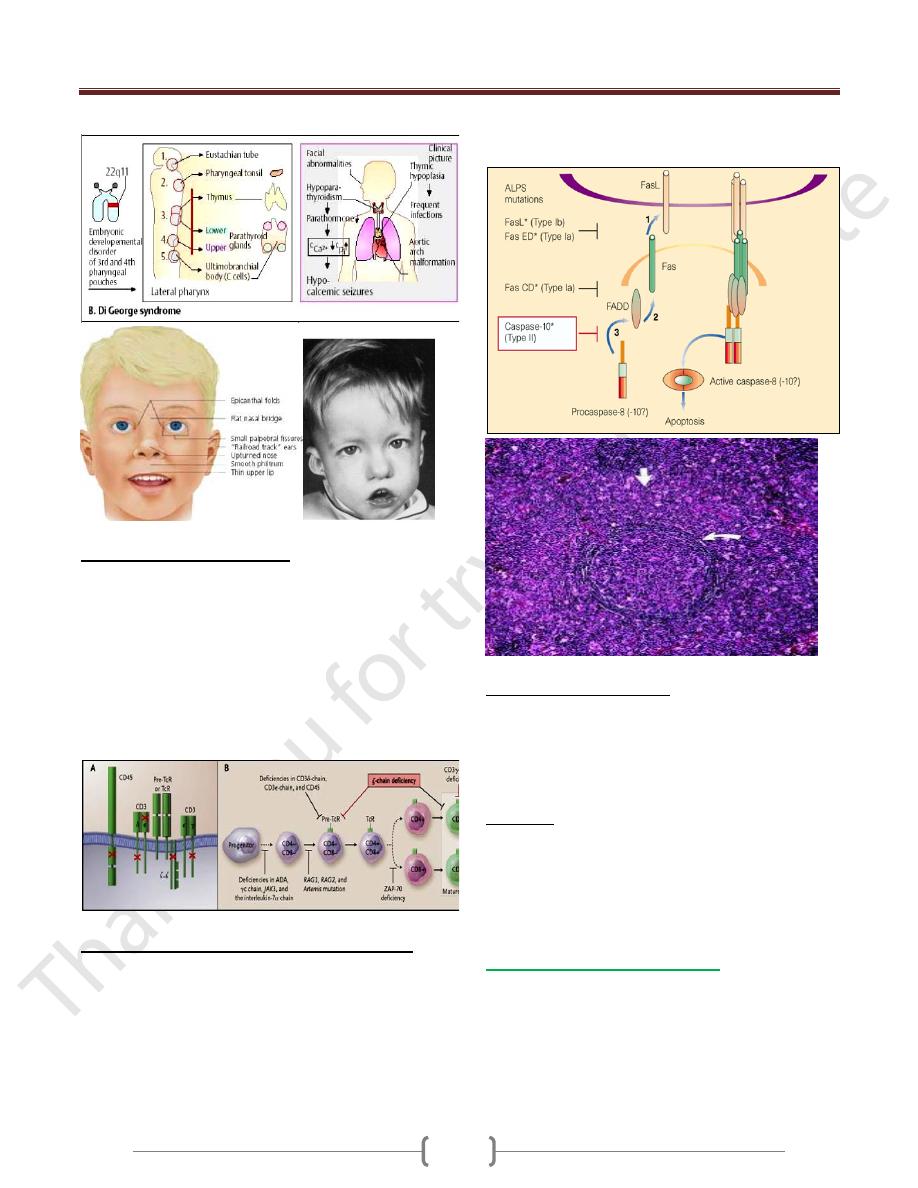
It includes the following diseases:
a- DiGeorge Syndrome b- Bare Lymphocytes Syndrome
c- Auto Immune Lymphoproliferative Syndrome
DiGeorge Syndrome
Results from failure of development of the 3
rd
and 4
th
pharyngeal pouch, usually caused by deletion of a small
piece of chromosome 22 at a location designated 22q11.2
produced by an error in recombination at meiosis
It is a congenital thymic aplasia & thymic hypoplasia,
It is associated with abnormalities of the aortic arch,
hypocalcaemia, tracheo-oesophageal fistula,
Cleft lip and palate and absent thymic development.
Characterized by very low numbers of T cells despite the
normal development in the bone marrow
Unit 3 - Immunological factors in disease
26
Bare Lymphocytes Syndrome
Characterized by absent expression of HLA molecules
within the thymus.
If HLA class I affected, CD8 + lymphocytes fail to
develop
If HLA class II affected, CD4 + lymphocytes fail to
develop
Uncontrolled activation of NK cell due to absence of
HLA class I expression
leads to recurrent infection and systemic vasculitis
Auto Immune Lymphoproliferative Syndrome:
Characterized by accumulation of lymphocytes and
persistence of autoreactive cells. Unusually high numbers
of white blood cells called lymphocytes accumulate in the
lymph nodes, liver, and spleen, which can lead to
enlargement of these organs
Caused by failure of apoptosis. This condition is usually
caused by mutations in the FAS gene
Patients develop lymphadenopathy, splenomegaly and a
variety of autoimmune diseases.
Investigations and treatment:
1) Measurement of total T- lymphocytes count
2) Measurement of T lymphocytes subsets
3) Immunoglobulin measurements
4) functional tests of T cells activation and proliferation
5) HIV test may be indicated
Treatment
1) Patients should receive anti-Pneumocystis and antifungal
prophylaxis treatment
2) Immunoglobulin replacement if disease associated with
defective Ab production.
3) Stem cell transplantation 4) Thymic transplantation
Primary Antibodies deficiency:
Characterized by recurrent bacterial infections.
Particularly of the respiratory and gastrointestinal tract.
The most causative organisms are bacteria such as
Streptococcus pneumonia and H influenzae .
Usually present at 5-6 months of age when the protective
benefit of transferred maternal Igs has decreased.
Unit 3 - Immunological factors in disease
27
3 major primary Abs deficiencies present in adulthood
1) Selective IgA deficiency
Characterized by low or undetectable IgA.
Most common primary Immune deficiency.
In some patients, there is a compensatory increase in
serum IgG levels.
30% of individuals experience recurrent mild respiratory
and GIT infections.
2) Common variable immune deficiency
It is a heterogeneous adult-onset primary immune
deficiency of unknown cause.
Characterized by low serum IgG levels and failure to
make Abs responses to exogenous pathogens.
Paradoxically, Ab mediated autoimmune diseases like
autoimmune hemolytic anemia
It is also associated with increased frequency of
malignancy like lymphoprolifrative diseases.
3) Specific Ab deficiency or Functional IgG Ab deficiency
It causes poor Ab responses to polysaccharide Ags.
Some patients are deficient in the Ab subclasses IgG2 & IgG4
It is previously called IgG subclass deficiency
Investigations:
1) Measurements of serum Igs.
2) Protein electrophoresis
3) Urine electrophoresis to exclude secondary causes of
hypogammaglobulineamia
4) Specific Ab responses to specific pathogens , if it is low ,
vaccinate the patient with killed vaccine
5) Quantitation of T and B lymphocytes
Treatment:
1) Treatment of infections by antibiotics and prophylaxis
antibiotics may be indicated.
2) Ig replacement intravenously which derived from pooled
plasma & contains IgG Abs & administered every 3-4 weeks
** Vaccinations with live vaccines is contraindicated
Secondary Immune deficiencies
It is more common than primary immune deficiency
Causes
1) Physiological: aging, prematurity, pregnancy.
2) Infection: HIV, measles, TB
3) Iatrogenic: Drugs like immunosuppressive drugs,
corticosteroids, antineoplastic, radiotherapy
4) Malignancy: Leukemia, lymphoma, myeloma, solid tumor
5) Biochemical and nutrional disorder:
6) Others: Burns, Asplenia.
Immune senescence:
It is a decline of the immune response in the elderly
characterized by:
1) Decline in the T cell response with reduced delayed type
hypersensitivity reaction.
2) Decrease in Abs production for many exogenous pathogens
3) AutoAbs rise but autoimmune diseases are less common
4) Reduced responses to vaccinations, about 30% of healthy
older people may not develop protective immunity after
influenza vaccine.
5) Allergic disorders and transplant rejection is less common
6) Increased susceptibility to infections like respiratory tract
infection, UTI, latent infections like TB and Herpes
Zoster may be reactivated.
7) Absent manifestations of infections e.g. leukocytosis &
pyrexia.
