Lecture 9 - Feeding of Vulnerable Groups
39
These groups are affected too much greater extent than
the general population with nutritional deficiency due to
their physiological status and these include:
1. Feeding of infants
2. Feeding of children
3. Feeding of mothers [pregnant and lactating].
4. Feeding of adolescence
5. Feeding of the elderly.
1) Feeding of the infants
Infants need adequate feeding for, normal growth and
development and for promotion of health and more
resistance to infection.
Principles of feeding:
1) Milk.
2) Dietary supplementation.
3) Weaning practice.
1) Milk:
the essential food and is either:
- human milk
- animal milk: this either powder milk , liquid milk
Breast feeding
Lactation is a physiological function with two processes:
milk secretion and milk letdown each controlled by a
special hormones of the posterior pituitary [prolactin and
oxytocin].
Requirement of breast feeding:
1) Must be started very early after delivery, for:
Stimulates milk secretion and emptying of breasts
Allows sulking of colostrum that is of anti-
infection value.
Early mother/ baby bonding.
2) Baby must be given sufficient time for suckling.
3) Mother must be at comfort, and psychologically
relaxed, to help the letdown.
4) Pattern of breast feeding:
Exclusive breast feeding giving breast milk only
[no other food], for the first four months. It may be
recommended for 6 months, especially in less
developed areas.
Weaning is then started, and gradually progresses,
together with dietary supplementation {given later}
Advantage of Breast – feeding:
Advantage to both baby and mother.
I] Advantage to Baby:
Nutritional.
Non – nutritional: anti – infection, convenience, and
psychological.
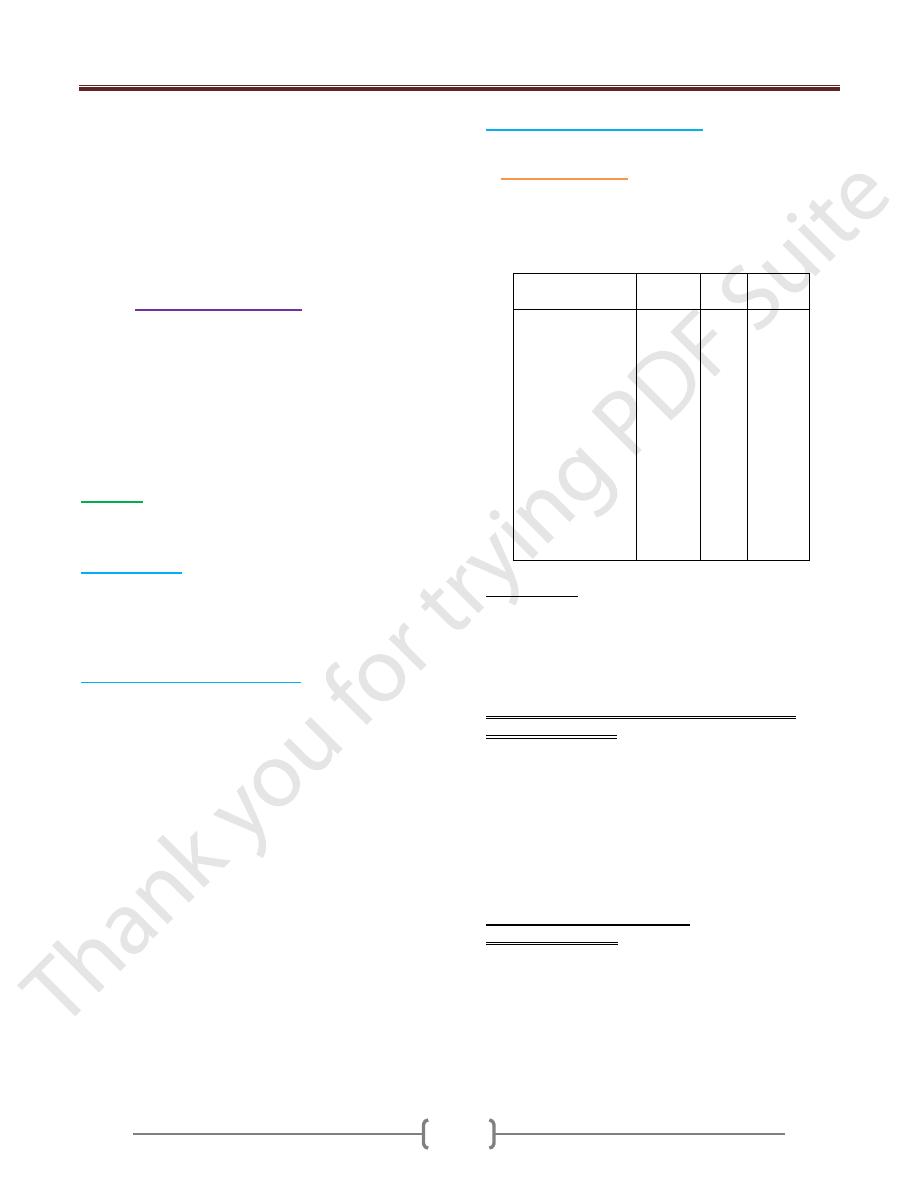
Composition of Milk
Milk Contents
Human
{%}
Cow
{%}
Buffalo
{%}
Protein gm
Fat gm
Lactose gm
Water ml
Energy kcal
Calcium mg
Phosphorus mg
Iron mg
Vitamin A IU
Vitamin D IU
Vitamin C mg
Thiamine mg
Riboflavin mg
Niacin mg
1.1
4.5
6.8
87.0
68.0
32.0
14.0
0.1
190.0
2.2
4.5
0.01
0.04
0.1
3.5
3.5
4.9
87.0
69.0
118.0
92.0
0.05
102.0
1.4
1.1
0.04
0.02
0.1
4.0
7.5
4.5
83.0
101.0
160.0
0.2
130.0
1.0
0.04
0.12
0.1
1. Nutritional:
Except for deficient iron and vitamin D that can be
supplemented, breast milk is of suitable composition and
properties for optimal growth and development. It is
readily digestible, and satisfies needs of infant in the first
months.
Impact of nutrition status of lactating mother on
composition of milk:
Adequately nourished mother: composition is more or
less unchanged[ hind milk, however, is of more fat and
protein content than fore milk]
Inadequate nutrition is mild/ moderate: quantity of milk
may be somewhat affected while composition is not, due
to physiological adaptation, with depletion of mother.
Severe malnutrition: both quantity and quality of secreted
milk are affected.
2. Non – nutritional Advantage:
A. Anti-infection value: incidence of infection, specially the
diarrhoeal and respiratory, is significantly lower in the
breast –fed then the bottle fed, due to
Presence of immunoglobulin in colostrum
The presence of lysozyme [antibacterial],
macrophages [bactericidal], lactobacillus bifid us-
promoting factor, lactoferritien [inactivates E. coli]
Lecture 9 - Feeding of Vulnerable Groups
40
B. Convenient feeding: the baby can be nursed at any time.
Breast milk is fresh and needs no preparation, of optimal
temperature, and is usually sterile.
C. Psychological value: breast –feeding allows intimate
mother/ baby contact that are emotionally valuable for
both.
II] Advantages to BF to mother:
Postpartum value: suckling stimulates secretion of
oxytocin that causes contraction of the uterus and
enhances involution of uterus.
Lower risk of breast cancer.
Psychological/ emotional value.
Fertility regulation: exclusive breast feeding suppresses
ovarian activity and postpartum ovulation, and is thus
associated with lactation amenorrhea.
Drew back of bottle feeding:
Milk borne infection,
Hyperosmolarity: increased serum similarity, causing
hypertonic dehydration.
Hypocalcaemia, due to impaired utilization of calium by
neonates in the first days or weeks--- neonatal tetany.
Allergy to caw milk, with more susceptibility to diarrhea,
and intestinal and skin disorders.
Depriving the baby of the benefits of breast- feeding.
2) Dietary Supplementation:
Milk feeding of infant and young children must be
supplemented for:
Milk –deficient nutrients
Protein.
Vitamin A.
1. Supplementation for milk –deficient nutrients:
Non powder milk is supplemented for
Iron: by iron rich food and medical preparations if
necessary, green leafy vegetables, eeg yolk, liver of
chicken then cattle
Vitamin C: giving fresh orange or tomato juice, green
vegetables.
Vitamin D: supplementation is non dietary by, proper
sun exposure ,giving vit D [ oral, parental]
2. Supplementation for protein:
As the infant grows older, increasing protein requirement
cannot be satisfied by milk, and so supplementary
protein- rich weaning foods are needed.
3. Vitamin A supplementation:
It is recommended to give two oral massive doses of vit.
A for healthy epithelial surfaces that support protection
against infection, especially measles.
Vitamin is available in blue capsules of 10000 IU, the
first capsule, at 9 months, with measles vaccine and
booster OPV.
Second dose, AT 18 months with MMR vaccine and
booster OPV, DPT vaccine.
3) Weaning:
Weaning is the process of gradually replacing milk feeds
of the baby, by a variety of foods until ultimately reaching
regular diet, and principally milk feeding is stopped, it is
recommended to start weaning from the 4
th
month and
progress to the age of 24 months.
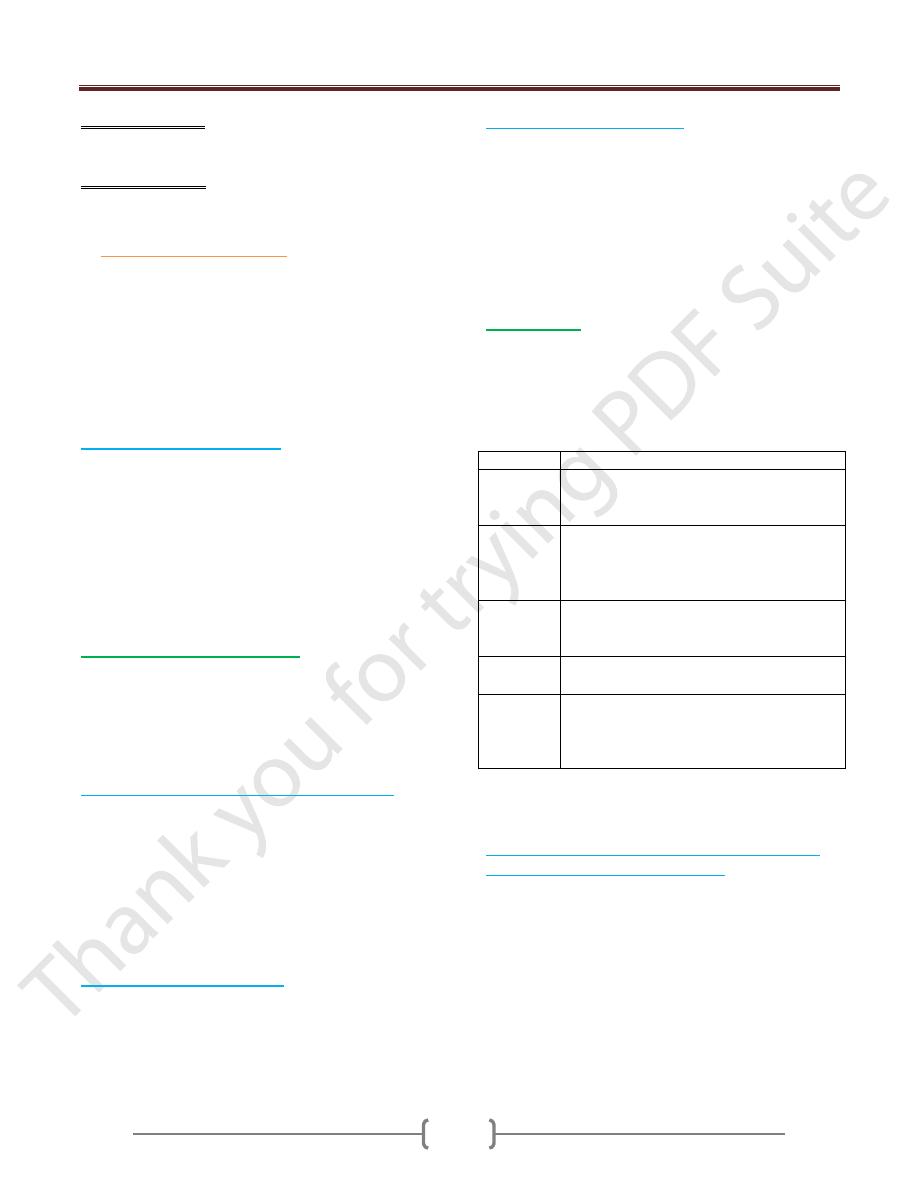
Months
Given food
4
th
Orange or tomato juice: for vitamin C
Milk pudding: for protein, starch and other
nutrients or yogurt.
5
th
Vegetable soup [by bottle]: for iron, iodine, in
nongoitrous area and vit. C.
Yolk of boild egg: for protein, iron, Vitamins
and others
6
th
, 7
th
Fruits, for vitamins and minerals: mashed
bananas, or cooked.
Smashed vegetables by spoon.
8th,9
th
Boild potatoes or sweet potatoes
Piece of bread, or biscuits.
10th to 12th
Mashed liver or chicken, or mined meat of
chicken, cattle or fish.
Peeled mashed stewed beans[ with precaution
for fauvism]
During the second year: mother is guided how to make a
balanced diet from selected food plus milk feeds, until
weaning completed.
The characteristic of weaning practice in traditional
communities of developing countries:
Breast – feeding is usually stopped abruptly stopped,
not gradually.
Onset of weaning varies widely: BF is continued for
varied period that may be as short as 6 months- 3 years
according to circumstances.
Milk feeds are largely replaced by sweetened fluids
and starchy food, which are lack of protein.
Milk may be given but usually in small inadequate
amount.
Lecture 9 - Feeding of Vulnerable Groups
41
2. Feeding of Children
Includes preschool children, and schoolchildren.
a)
Feeding of preschool children:
Children of 1-5 years need special feeding that satisfies
normal growth and development, and health promotion
and body resistance to infection.
Deficiency:
infants [after the 6
months of age usually, or
earlier sometimes] and preschool children are exposed to
deficiency of protein, iron, vitamin D, and other nutrients.
1) Protein Deficiency: PEM, in infants and young
children, underweight, in older children.
2) Vitamin D deficiency: causes rickets. Age incidence
is usually 6 - 24 months.
3) Iron deficiency: causes iron-deficiency anemia, a
common deficiency problem.
4) Others:
Ariboflavinosis.
Dental caries.
Vitamin A deficiency.
b)
Feeding of school children:
Nutrition Deficiency Diseases
Protein deficiency: causes impaired growth and
underweight.
Iron-deficiency anemia: common problem.
Riboflavin deficiency, causing ariboflavinosis, with eye
and mouth manifestation, including cheilosis.
Dental caries: multifactorial problem, including
neglecting regular oral hygiene {the most important}, and
nutritional deficiency.
Vitamin A deficiency, giving skin and may be ocular
manifestations: occasional problem.
{What about rickets: active rickets is a preschool disease,
with age incidence of 6-24 months. Schoolchildren,
however, may show sequelae of untreated rickets, termed
"healed rickets"}.
Predisposing factors:
Inadequate home and school feeding.
1) Nutrition ignorance of child and family, including faulty
food habits, as:
Going to school without taking breakfast.
Spoiling appetite for principal meals, by in between-
meal nibbling {sweets, soft drinks and others}
Preferring snacks than vegetables and fruits.
2) Parasitic infection.
Manifestations:
General picture: impaired appetite, early fatigue, lowered
alertness and body resistance, and weak muscles.
Specific nutritional deficiency, giving characteristic
manifestations of missing or inadequate nutrient{s}.
3. Feeding of adolescence
There is a5-7 year period of rapid growth, during which
the adolescent will gain about half of their final adult
weight. The peak occurs at around 12 in girls and around
15 in boys. It is associated with the onset of sexual
maturity, after this is reached; growth tapers off until the
late teens in girls and the early twenties in boys.
Energy requirement for adolescents:
Energy need in girls reach a level of 2200 kcal/day at age
11-12 and stay at that level through adolescence. Boys,
with their later growth peak, start out at 2500 kcal/day
and go up to 3000 kcal/day during the period of maximum
growth, dropping back to adult levels during the late teens
and early twenties.
Minerals:
Some 45% of the overall skeletal growth occurs during
adolescence. Calcium requirement in adolescents is
therefore elevated to 1200 mg/day, with boys requiring
somewhat more than girls.
Zinc and magnesium are also required, girls under the
influence of estrogen, show an increase in bone density as
well as bone size during adolescence.
Iron:
The requirement in girls as they go through menarche are
somewhat greater, girls on the other hand, require adult
female levels of Iron Age 12 onward.
Vitamins:
A number of the B complex vitamins, specially thiamin,
riboflavin, niacin are required in large amounts to meet
high energy requirements and to support muscle
synthesis. Vitamin D is crucial to support the rapid
skeletal growth, its requirement are above adult levels
during adolescence. Vitamin A, C, E, B6 and foliate, are
required in adult amounts.
None of these should require supplementation in
individuals consuming a healthy and balanced diet.
Lecture 9 - Feeding of Vulnerable Groups
42
4. Feeding of mothers
{Pregnant and lactating}
Extra allowances of nutrients and energy are needed
during the latter half of pregnancy, and throughout
lactation, to satisfy physiological requirements of mother,
and needs of intrauterine growth and development.
Special consideration is given to:
Nutrition education of mothers for principles and
requirements of maternal and child feeding.
Dietary supplementation during pregnancy and lactation,
if necessary. Usually no supplementation is fed mothers.
Family planning service for optimal pregnancy spacing,
or postponing pregnancy for indicated period of time, for
restoration and promotion maternal health, and favourable
outcome of pregnancy.
Health appraisal of mothers, for:
Diagnosis and treatment of nutritional deficiency.
Morbidity that may predispose to malnutrition, if any,
e.g. parasitism.
Impact of malnutrition during pregnancy:
Impact on both the pregnant and fetus.
Impact on the pregnant:
General impairment of health.
May predispose to some maternal hazards.
Nutritional deficiency diseases, specially:
Nutritional anaemia: iron-deficiency anaemia,
pregnancy macrocytic anaemia
Osteomalacia.
Tetany, occasionally.
Impact on fetus:
More incidence of LBW.
Tendency to premature onset of labor, and more risk of
birth injuries.
Deficient body stores of the newborn, and susceptibility
to deficiency early in life, specially iron-deficiency
anemia and rickets.
Congenital cretinism in goitrous areas, when iodine
supplementation is not given during pregnancy.
Impact of malnutrition during lactation:
Impact on mother
: mother is exposed to the same
hazards of malnutrition of the pregnant, given before.
Impact on nursed baby
: composition of breast-milk is
unique, and not influenced by maternal malnutrition,
except with severe advanced deficiency.
5. Feeding of the elderly
Malnutrition is one of the main health problems of the
elderly.
Predisposing Factors:
Impaired physiological functioning with aging, including
digestion, absorption and metabolism.
Loss of teeth.
Chronic disease may be associated with anorexia.
Psychological disturbance may de associated with
anorexia, and neglecting or refusing food.
Deficiency Diseases
: varied types and severity, according
to nature and severity of deficiency. Important problems
include general debility and loss of weight, anemia, and
osteoporosis.
Prevention:
1) Establishing geriatric health centers, to provide
convenient accommodation, especially for the elderly
deprived of family care.
2) Nutrition education, of the elderly and family, for:
Foods of high nutritive value, and easy preparation,
consumption and digestion. Milk, cheese and yoghurt,
mashed potatoes, fish and minced chicken and meat
are valuable.
Diet therapy and restrictions, on medical prescription.
3) Dietary supplementation, by:
Powder milk, if regular liquid milk supply is not
available.
Supplementary geriatric foods: made of balanced,
readily digestible mixtures of HBV protein, vitamins
and minerals.
Polyvitamins – minerals preparations.
4) Regular health appraisal: for diagnosis and treatment of
morbidity, including nutritional deficiency and
predisposing disease.
