Lecture 2+3+4+5 - Food Constituents
10
1- Macronutrients
1) Protein
Lecture 2+3+4+5 - Food Constituents
11
Lecture 2+3+4+5 - Food Constituents
12
2) Carbohydrates
Lecture 2+3+4+5 - Food Constituents
13
Lecture 2+3+4+5 - Food Constituents
14
3) Fats
Lecture 2+3+4+5 - Food Constituents
15
Lecture 2+3+4+5 - Food Constituents
16
Lecture 2+3+4+5 - Food Constituents
17
Lecture 2+3+4+5 - Food Constituents
18
2- Micronutrients
Vitamins
Vitamins are essential organic compounds needed for
body functioning & metabolism. They are classified into:
Fat-soluble: A, D, E and K.
Water-soluble: B group and C.
Fat-soluble: A, D, E and K.
Vitamin A
Vitamin A is the name of a group of fat-soluble retinoid,
including retinol, retinal, retinoic acid, and retinyl esters
.
Vitamin A is involved in immune function, vision,
reproduction, and cellular communication. Vitamin A is
critical for vision as an essential component of rhodopsin,
a protein that absorbs light in the retinal receptors, and
because it supports the normal differentiation and
functioning of the conjunctival membranes and cornea.
Vitamin A also supports cell growth and differentiation,
playing a critical role in the normal formation and
maintenance of the heart, lungs, kidneys, & other organs.
2 forms of vitamin A are available in the human
diet:
1.
preformed vitamin A (retinol and its esterified form,
retinyl esters) is found in foods from animal sources,
including dairy products, fish, and meat (especially liver).
By far the most important
2.
provitamin A carotenoids . Is beta-carotene; other
provitamin A carotenoids are alpha-carotene and beta-
cryptoxanthin. The body converts these plant pigments
into vitamin A. Both provitamin A and preformed vitamin
A must be metabolized intracellularly to retinal and
retinoic acid, the active forms of vitamin A, to support the
vitamin's important biological functions.
Vitamin A is obtained from dietary sources, and
nondietary when necessary.
1-
Dietary Sources: animal and plant foods.
Animal foods: liver and liver product , egg yolk, whole-
milk & cheese, butter, cream, fatty fish & any animal fat.
Plant foods: not provide vitamin A, but the vitamin
precursor {provitamin}. Carotenes are found in pigments
of most vegetables and fruits {green, yellow, and red,
orange: - carrots, red peppers, tomatoes). Beta – carotene
in chlorophyll of dark – green leafy vegetables (spinach)
is particularly important.
2-
Non dietary Source: cod-liver oil and other fish-liver oils
can be given to supplement vitamin A for vulnerable
groups when necessary.
Physiological Functions
1- Normal growth of healthy epithelial cells, of Skin and
muous membranes, especially of respiratory passages and
urinary tract.
Vitamin A is known as "anti-infection vitamin", because
it is needed for formation of healthy epithelial surfaces,
which are the first line of natural barriers of infection that
resists invasion by pathogenic organisms. But once
infection occurs, vitamin A has no effect against infection
{i.e. anti-infection role is preventive, not therapeutic}.
2- vitaminA is essential for the production of
rhodopsin in the rods 0f the retina., which is
important for the adaptation of vision in the dark.
3- growth
4- cell differentiation
5- Emberyogenesis\
6- Immun response
Deficiency vitamin A
Eye changes : night blindness when vitamin A status
is marginal , and with prolonged or sever deficiency ,
changes to the cornea and congunctiva occur , these
eye changes are known collectively as Xerophthalmia
. these changes consist of conjunctival xerosis and
lack of tears , Bitot`s spots , corneal xerosis , corneal
ulceration and corneal scars
Epithelial tissues – skin keratinization , horny plugs
block the sebaceous glands leading to follicular
hyperkeratosis
Immunity: vitamin A deficiency results in increase
susceptibility to infectious diseases such as diarrhea
and respiratory infections due to Pathological changes
of mucous membranes that become more susceptible to
infection.
Requirements :
The established recommended dietary allowance standard
for adults is 800 µg for women and 1000 µg for men.
Lecture 2+3+4+5 - Food Constituents
19
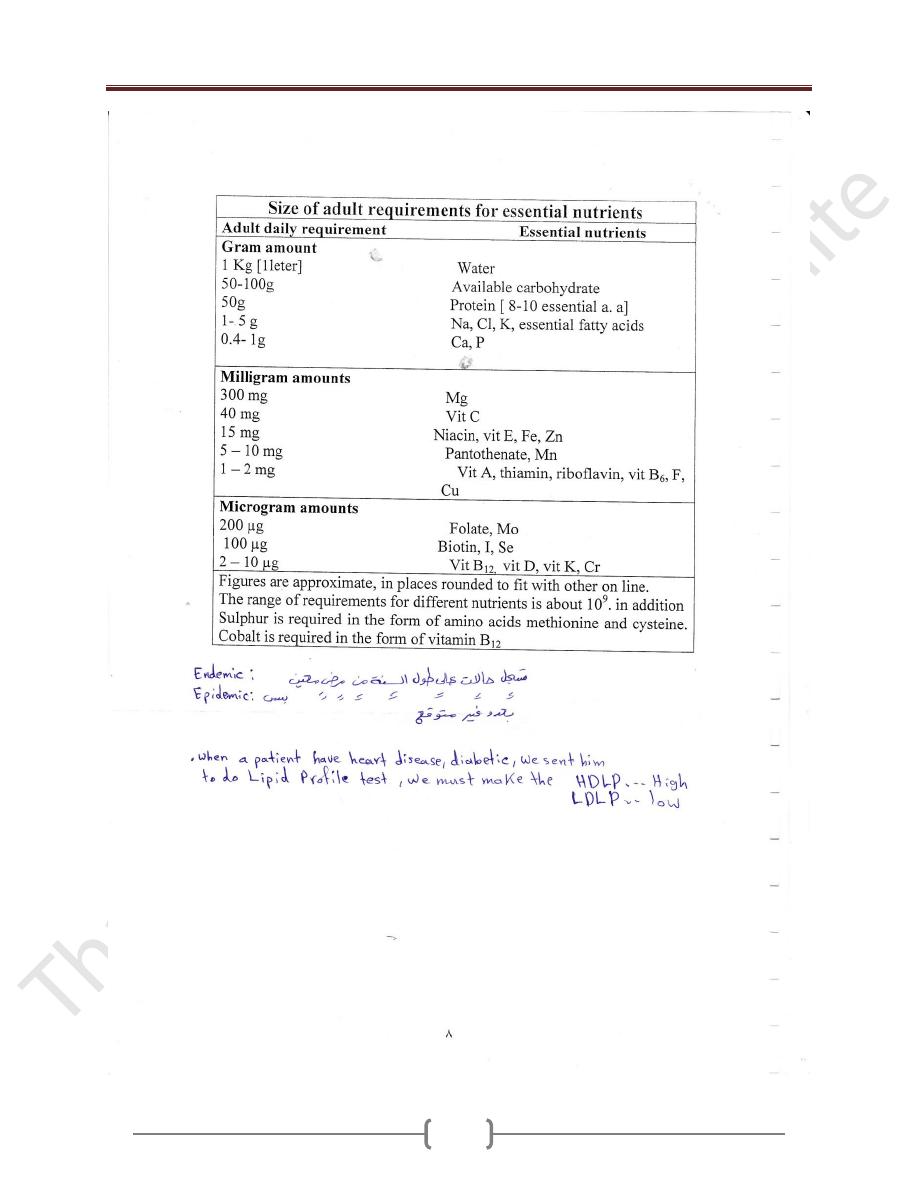
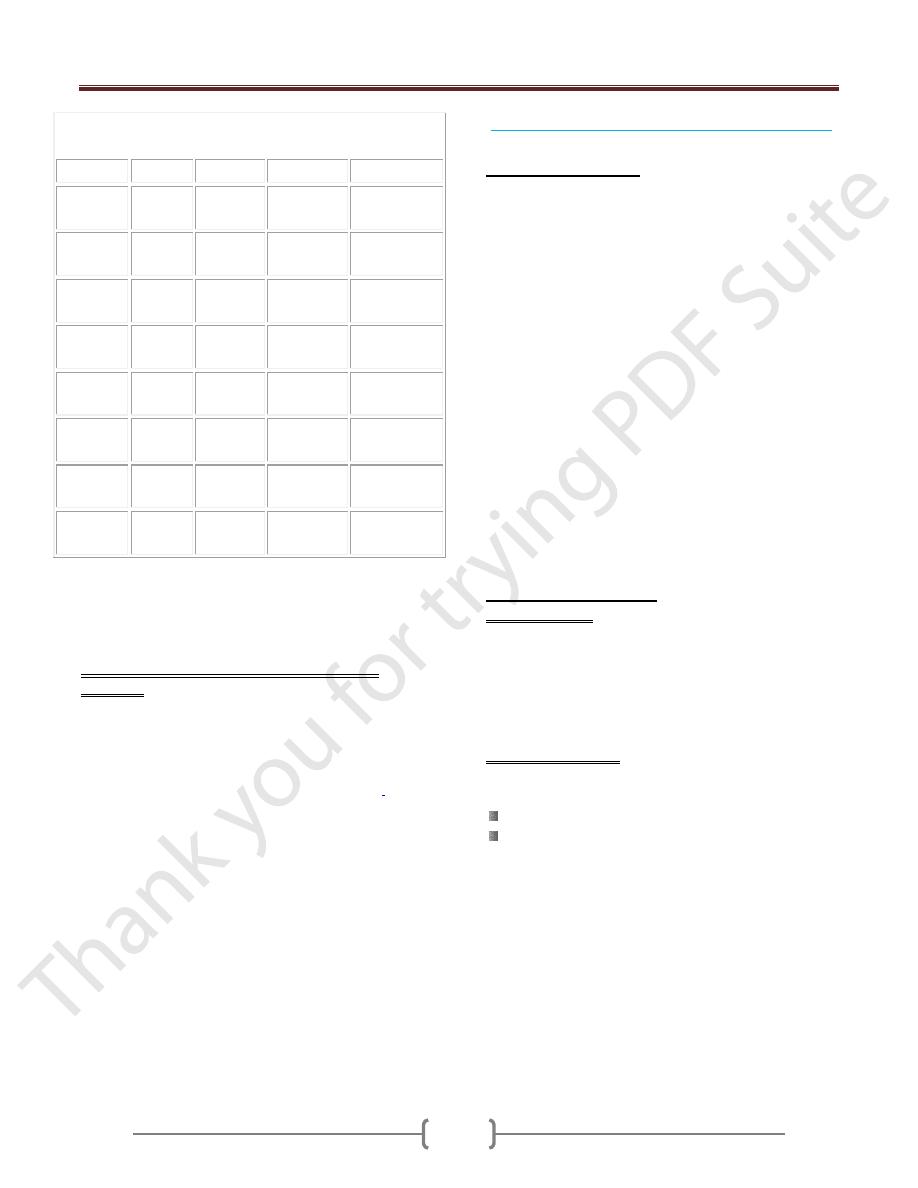
Table 1: Recommended Dietary Allowances (RDAs) for
Vitamin A
Age
Male
Female
Pregnancy Lactation
0–6
months*
400 mcg
RAE
400 mcg
RAE
7–12
months*
500 mcg
RAE
500 mcg
RAE
1–3 years
300 mcg
RAE
300 mcg
RAE
4–8 years
400 mcg
RAE
400 mcg
RAE
9–13 years
600 mcg
RAE
600 mcg
RAE
14–18
years
900 mcg
RAE
700 mcg
RAE
750 mcg
RAE
1,200 mcg
RAE
19–50
years
900 mcg
RAE
700 mcg
RAE
770 mcg
RAE
1,300 mcg
RAE
51+ years
900 mcg
RAE
700 mcg
RAE
RDAs for vitamin A are given as mcg of retinol activity
equivalents (RAE) to account for the different
bioactivities of retinol and provitamin A carotenoids
Pregnant and Lactating Women in Developing
Countries
Pregnant women need extra vitamin A for fetal growth
and tissue maintenance and for supporting their own
metabolism. The World Health Organization estimates
that 9.8 million pregnant women around the world have
xerophthalmia as a result of vitamin A deficiency
.
Other
effects of vitamin A deficiency in pregnant and lactating
women include increased maternal and infant morbidity
and mortality, increased anemia risk, and slower infant
growth and development.
The most common and readily recognized symptom of
vitamin A deficiency in infants and children is
xerophthalmia
Vitamin D (calciferols){Antirachitic Vitamin}
What is Vitamin D?
Vitamin D is a fat-soluble vitamin that's formed when
skin is exposed to the sun's ultraviolet rays. Vitamin D is
also found in food and dietary supplements.
There are two major types of vitamin D. Vitamin D3, also
called cholecalciferol, is the type made in the body in
response to sun exposure and found in certain foods.
Vitamin D2 (ergocalciferol) is the most common form
used in supplements. It's also used to fortify certain foods,
such as milk.
Both typ\es of vitamin D must be converted in the liver
and kidneys to the active form, 1,25 dihydroxyvitamin D,
to be useful to the body.
Present in two forms: Vitamin D
2
and Vitamin D
3.
Dietary ergocalciferol and cholecalciferol are
biologically inactive and are activated to 25-
hydroxyvitamin D in the liver ( this has limited
amount of biological activity ) . further conversion in
the kidney in the production of more active form
1,25- dihydroxyvitamin D ( Calciferol)
Sources of Vitamin D:
1- Dietary Sources:
Oil-rich salt-water fish {e.g. sardines and salmon}, liver,
egg yolk , , and other fat-containing animal foods:
provide but little vitamin D, not satisfying body need.
Cod liver oil
D-fortified foods {vitamin D is added}: baby powder
milk, and fortified butter and margarine.
2- Non dietary Sources: vitamin D supply is largely
nondietary.
a) Ultraviolet radiation of skin:
Exposure of bare skin to sunlight.
Exposure to artificial ultraviolet rays: only
occasionally used to treat rickets, if necessary.
b) Medicinal preparation of oral fish liver oil {provide
vitamin D and A}, or vitamin D2, oral or parenteral,
given, to supplement vitamin D
Lecture 2+3+4+5 - Food Constituents
20
What Does Vitamin D Do?
The main function of vitamin D is to maintain normal
levels of calcium and phosphorus in the blood to support
bone mineralization (hardening of bones), cell functions,
and proper nerve and muscle function. Vitamin D acts as
a hormone, enhancing the absorption of calcium and
phosphorus in the small intestine.
Vitamin D is needed for normal growth. Without it, bones
become weak and deformed, resulting in rickets in
children and a condition called osteomalacia in adults.
Osteoporosis
Vitamin D deficiency can lead to the development of
osteoporosis because it reduces calcium absorption. In
older people, low vitamin D levels have been associated
with an increased risk of falling. Higher vitamin D levels
have been associated with stronger bones (greater bone
mineral density).
Cancer
Preliminary evidence suggests vitamin D may aid in
cancer prevention by blocking cell growth and
differentiation (cells mature and take on a specialized
form and function).
Since the late 1980s, the risk of developing and dying
from breast, prostate, ovarian, and other cancers has been
found to be increased in geographic areas located at
higher latitudes, where there's less sun exposure, and with
vitamin D deficiency.
Autoimmune Disease
Because vitamin D is thought to influence the immune
system, there is some evidence it may help with
autoimmune disease.
Other Conditions
Preliminary evidence suggests vitamin D may help with
muscle and bone pain, diabetes prevention,
fibromyalgiagum
, and proper immune
function.
Vitamin D supplements are also available.
Multivitamins and calcium supplements provide vitamin
D, but the amount varies widely so it's important to read
labels. Vitamin D3 (cholecalciferol) is the preferred
form.
Recommended Vitamin D Intake
Recommendations for vitamin D intake are as follows:
Birth to 50 years -- 200 IU (5 mcg)
Between 51 and 70 years -- 400 IU (10 mcg)
Over 71 years -- 600 IU (15 mcg)
Pregnant and nursing women -- 200 IU (5 mcg).
In a recent study that found a 7% reduction in mortality,
the average intake was about 500 IU per day.
Function:
Vitamin D is needed for bone metabolism:
1,25 dihydroxyvitamin D maintains plasma Ca by
controlling Ca absorption and excretion
Vitamin D and it's metabolites are involved in bone
mineralization
Deficiency:
Arises mainly from nonexposure of bare skin to sunlight.
Blood calcium and phosphorus level in blood is
inadequate for mineralization of growing bone, and
remineralization of mature bone, causing:
Rickets, (which is characterized by reduced
calcification of bone epiphyses) , and late eruption and
early decay of teeth in children.
Osteomalacia in adults: largely due to calcium
deficiency, and occasionally vitamin D deficiency.
Osteoporosis: vitamin D deficiency may contribute to
type II Osteoporosis of the elderly.
Vitamin E
Eight naturally occurring forms of Vit E are synthesized
in plants
Sources:
Wheat- germ oil
egg yolk and liver are rich sources.
Almonds.
sunflower seeds and oil
peanuts and peanut butter
corn oil
Recommended daily allowance
:
the recommended daily allowance
( RDA) standard for men and women age 14 and older is
15 mg / day , with lesser amounts required in childhood.
Needs during the first year of infancy do not have an
RDA figure, but an adequate intake amount of 4-6
mg/day is used .The UL ( Tolerable Upper Intake Level)
for adults is set at 1,000 mg /day .
Lecture 2+3+4+5 - Food Constituents
21
Function:
Antioxidant, vitamin E is a powerful antioxidant
and protects cell membranes and lipoproteins
from damage by free radicals
Maintenance of cell membrane integrity
Regulation of prostaglandin synthesis
DNA synthesis
Vitamin K
Naturally occurring vitamin K can be classified into
two groups , the major form of vitamin K 1 is found
in plants while the vitamin K2 group of compounds
are synthesized by intestinal bacteria
Sources:
Dietary: fresh dark- green leafy vegetables (spinach,
cabbage).
Biosynthesis: intestinal flora form vit. K.
Synthetic preparations: of K
3
, oral and parental
therapeutic purposes.
Function
Blood clotting: vitamin K is essential for maintaining
normal levels of four of the 11 blood clotting factors.
promotes the synthesis of γ - carboxyglutamic acid (
Gla ) in the liver . Gla is an essential part of
prothrombin ( factor II ) and other coagulation factors (
VII, IX , and X ) .vitamin K is therefore essential for
blood coagulation
Bone development: spesific proteins found in bone and
bone matrix require vitamin K for their synthesis and
are involved with calcium in bone development ,these
bone proteins bind calcium but function here to form bone
crystals .
Water-soluble Vitamins: B and C
** B-Vitamins
The B group of vitamin {water soluble} includes:
Thiamine: vitamin B1, antiberiberi vitamin.
Riboflavin: vitamin B2.
Niacin: nicotinic acid, PP factor {pellagra- preventing factor}.
Folic acid.
Cyancobalamin: vitamin B12.
Pyridoxine: vitamin B6.
Biotin
Pantothenic acid and others.
Sources:
Biosynthesis: by intestinal flora and tissues, except
B12 which is only dietary.
Dietary Sources: plant and animal foods, except B12
which is provided by animal foods only.
Plant foods: {yeast}, whole-grain cereals, pulses, nuts,
green leafy vegetables
Animal foods: egg yolk, meat, organ meat.
Physiological Role: B-vitamins are coenzymes of many
enzymes systems of body metabolism.
Thiamine {B1}
Physiological Role:
B1 is needed for carbohydrate metabolism
Deficiency:
Causes impaired carbohydrate metabolism, clinically
manifested as:
1- beriberi which is classified as dry beriberi involves
the nerves {peripheral neuropathy} and wet beriberi
which involve myocardium.
2- Wernicke- Korsakoff syndrome in chronic
alcoholics , ( encephalopathy and psychosis )
Recommended daily allowance:
Adult male 1.5 mg.
Increased during pregnancy and lactation.
Increased whenever dietary carbohydrate is increased to
provide more energy, according to energy need.
Riboflavin {B2}
B2 has fluorescent yellow-green color.
Sources:
Lecture 2+3+4+5 - Food Constituents
22
Milk is the richest source, hence also named "lactofavin".
Eggs, Liver & kidney, yeast extracts
Function:
1) promotion of normal growth
2) assisting of synthesis of steroids , glycogen
3) maintenance of mucous membranes , skin, eyes, and
the nervous system
4) aiding Fe absorption
Deficiency:
Shows mouth and eye manifestations.
Mouth: angular stomatitis {formation and fissures of
mouth angles}, cheilosis, glossitis & nasolabial dermatitis
Eyes: circumcorneal vascularization, with lacrimation,
photophobia, irritation and sandy feeling.
Recommended daily allowance:
Adult male 1.7mg.Increased during pregnancy & lactation
Niacin (nicotinamide, nicotinic acid )
Sources: dietary and biosynthesis.
Biosynthesis: animal protein foods provide the essential
amino acid tryptophan which is converted , by
biosynthesis, into niacin, and so tryptophan is
considered "niacin precursor".
Niacin deficiency: causes pellagra which is
characterized by:
Dermatitis, Diarrhea, Dementia.
Recommended daily allowance:
Adult male nearly 20 mg of total niacin, that depends on
dietary niacin and tryptophan. It is increased during
pregnancy and lactation
Vitamin B6
There are three naturally occurring forms of Vit B6 ,
pyridoxine, pyrridoxal, and pyridoxamine
Food sources:
Meat, Wholegrain cereals, and fortified cereals, Bananas
& Nuts
Deficiency : lead to lesions of the lips and corners of
the mouth and inflammation of the tongue. Vit B6
deficiency is usually associated with other vitamin
deficiency .
Folic acid
Physiological Role:
1) Folic acid is needed, together with B12, for development
of red blood cells in the bone marrow.
2) Folates are essential for the synthesis of DNA & RNA
Deficiency:
Causes "megaloblastic {macrocytic} anaemia", where
development of RBCs in the bone marrow stops at
megaloblast stage
Vitamin B12
Vitamin B12, (cobalamin is the natural form , &
cyanocobalamin is the commercially available one), is
water-soluble, crystalline red cobalt-containing
compound. It is absorbed in the small intestine; it needs
an intrinsic factor secreted by healthy stomach mucosa.
The liver stores enough vitamin B12 for 3 years
Sources: of B12 differ from other B-vitamins by being:
Only dietary, no biosynthesis.
Provided by animal foods only, especially liver, kidney,
meat and fish .
Physiological Role: B12 is involved in
1) Synthesis of nucleoproteins.
2) Formation of red cells in the bone marrow.
3) Normal myelination of nerves.
Deficiency:
Causes pernicious anemia (megaloblastic) & or nervous
manifestations. Deficiency May be primary or secondary.
Primary deficiency: dietary, with plant or largely plant diet.
Secondary deficiency:
When intrinsic factor is lacking, and so dietary B12 is
not absorbed in small intestine: with degeneration of
gastric mucosa, or gastrectomy.
The intestinal parasite "D. latum" consumes B12.
Recommended daily allowance: 2 micrograms for adults.
Intake increased during pregnancy and lactation.
Vitamin C {Ascorbic Acid}
Sources:
Plant foods, while animal foods, including milk, are poor
sources.
Citrus fruits {and their fresh juice}, Cauliflower, cabbage,
tomatoes, sprouting beans
Physiological Role:
1) Vit C is a powerful reducing agent (antioxidant)
Lecture 2+3+4+5 - Food Constituents
23
2) Vit C is required for the synthesis of collagen , the
main protein in connective tissue and therefore it is
essential for the maintenance of muscles, tendons,
arteries , bone, skin ,. It is essential for the normal
functioning of enzymes involved in collagen synthesis
3) Facilitates absorption of iron in the intestine ,when
consumed in the same meal.
4) Plays a role in amino acid metabolism.
5) Various peptide hormones and releasing factors
require activation by Vit C dependent enzyme
6) The hydroxylation of dopamine to the neurotransmitter
noradrenaline require vitamin C
Deficiency:
Scurvy is the clinical syndrome of deficiency. Scurvy is
characterized by bleeding anywhere in the body, specially
the gums, skin and mucous membranes, and near joints
and bones,
Recommended daily allowance:
60 mg for adults, and more during pregnancy & lactation.
Calcium
Ca. is the most abundant mineral in human body is about
1.4 gm\ kg and 99% in bones and teeth, and 1% in soft
tissues and body fluids.
The normal plasma range for Ca is 2.15 – 2.55 mmol \ l
Sources:
Caseinogen, of milk and cheese: the richest source.
Shellfish, canned fish [with bones],some green
vegetables, molasses, and sesame :good sources.
Deficiency:
1) Deficiency disease and metabolic disorder of bone:
Osteomalacia, rickets & osteoporosis.
1) Tetany: due to severe calcium deficiency, _
hypocalcaemia that causes increased irritability of motor
nerves, usually in children and occasionally in adults.
2) Other hazards related to blood clotting, & regulation of
pulse.
Phosphorus
The normal adult range of serum total phosphate level
is 0.7-1.5 mmol \ l .
Body phosphorus is found in:
Skelton, mainly: 80%
Body fluids and tissue cells: 20%
Sources:
Calcium – rich foods. Specially milk and cheese: provide
adequate phosphorus too.
Protein – rich animal foods. specially egg yolk and meat {
of cattle{ fish and poultry}: rich sources of phosphorus.
Bran of cereal grains contains phosphorus that is mostly,
however, as phytic acid: not only unutilizable, but also
interferes with absorption of calcium.
Physiological Role:
1) Bone and teeth formation, by complex calcium phosphate.
2) Phosphorus is a component of many enzymes of cell
metabolism and functional activities.
3) Formation of phospholipids.
4) Phosphorus contributes to normal blood chemistry.
Deficiency:
Practically unknown, since phosphorus requirement is
provided by animal and plant foods.
No dietary allowance is specified
Iron
There is approximately 4 gm of Fe in the body of an
adult man.
Sources: animal and plant foods.
Animal foods: organ meat {liver, heart, kidney}, lean
meat, shellfish and egg, while milk is poor in iron.
Plant foods: dried beans, nuts, green leafy vegetables, molasses.
Absorption: iron can be absorbed in the stomach and
upper part of small intestine. Not all, but a certain percent
only of dietary iron is absorbed: around 10%, normally.
Iron Deficiency:
Causes "hypochromic microcytic anaemia", with
diminished hemoglobin content of red cells, & oxygen-
carrying capacity of blood
Iodine
Sources:
Chief source: vegetables & fruits grown on Iodine- rich soil.
Other sources: sea foods, specially fish, and milk when
pasture is rich in iodine.
Physiological Role:
Iodine is essential component of thyroid hormones that
are needed for tissue metabolism and regulation of
metabolic rate.
Deficiency:
1) Goitre: simple or endemic, with enlarged thyroid.
Lecture 2+3+4+5 - Food Constituents
24
2) Cretinism: acquired, and occasionally congenital.
3) Congenital cretinism is due to inadequate supply of the
fetus with iodine.
Fluorine
Fluorine is found in enamel of teeth, making it decay –
resistant, and thus prevents dental caries {tooth decay}.
Sources:
Water supply: potable water is the chief source.
Tea and seafood are relatively rich.
Deficiency:
When potable water supply contains inadequate fluorine,
especially of less than 0.1 ppm. Children suffer high
incidence of dental caries.
Trace Elements
Zinc:
Required zinc is provided by foods of balanced diet,
especially muscle meats of farm animals and fish &
seafood
Zinc is coenzymes of zinc – containing enzymes of
protein and carbohydrate metabolism. They are essential
for synthesis of DNA and RNA.
Deficiency:
Balanced diet with adequate animal – protein foods
provides zinc requirement. Deficiency may arise with:
Plant, or largely plant, diet.
Using low – extraction flour, where phytate interferes
with absorption of zinc.
Morbidity associated with increased protein loss.
Deficiency causes growth retardation , failure to thrive ,
delayed sexual maturation{with hypogonadism, especially
in males}.
Relatively more dietary zinc is needed for:
Children below 10years.
Pregnant and lactating mothers.
Zinc intake can be assessed by zinc content of hair & nails.
Copper:
An adult has 80 mg of cu in their body
Sources:
liver, kidney, shellfish, dried beans, nuts and raisins are
good sources, while milk is poor in copper. Average diet,
however, provides copper requirement, and so dietary
deficiency is uncommon, if any.
Functions:
1) Plays a role in oxidation – reduction enzyme systems.
2) Haemopoietic role:
Better absorption of iron.
Synthesis of hemoglobin and cytochrome.
Deficiency:
Not reported in adults.
Deficiency in infants {rare} shows impaired growth,
mental retardation, brittle hair, anaemia {must be
managed by iron and copper}, and contributes to
manifestation of PEM.
Magnesium:
Sources:
Magnesium is widely available in most foods, specially
meat, organ meat, seafoods, green vegetables
{Hard water contains magnesium}.
Functions:
1) Extracellular magnesium: needed in neuromuscular
transmission.
2) Intracellular magnesium: A component of matrix of bone.
- Essential cofactor of many enzyme systems, e.g.
phosphorylation and synthesis of nucleic acid.
Deficiency:
Arises from some pathological conditions:
1) Acute diarrheal disease and PEM.
2) Chronic renal failure.
3) Chronic malabsorption syndrome.
4) Chronic alcoholism.
5) Manifestations: vary with the extent of deficiency that
may be mild {usually asymptomatic}, moderate or severe.
Cases may show irritability, emotional disturbance,
muscle disorders and other hazards.
Manganese:
Sources: dietary content varies, for example:
Cereals, whole unrefined grains, dried fruits, nuts and tea[
very rich], liver, peanuts and white bread [rich],
vegetables and fruits [ moderate].
Function: managanese activates many enzymes.
Deficiency: reported in animals not in man.
Lecture 2+3+4+5 - Food Constituents
25
Water:
Water forms about 70% of body weight. it is necessary
for life, being a constituent of all body cells, that is
needed for body functioning.
Daily requirement:
Not fixed, but varies with climate, physical activity and
other factors. An adult in temperate climate needs about
2.5 liters of water a day, obtained from potable water, and
water, content of ingested fluids and foods.
Fibers
Fiber is material from plant cell walls that is resistant to
digestion by enzymes of the human small intestine, and is
often classified according to its solubility in water. Water
soluble fibers tend to be efficiently broken by bacteria in the
colon. Water insoluble fibers pass through the body mostly
unchanged. Dietary fiber is a complex mixture of both.
Sources:
Fruits [banana], vegetables [potato], breads and cereals,
nuts and seeds.
Recommended daily intake:
Infant: 6-20 weeks ---------------------9.1 gm of fiber/L of
formula
Children: age + 5 gm / day [beginning at age 2- age 18].
Adults: 20-35 gm / day.
Conditions that can be improved by increasing fiber
intake:
1) Diseases of coln.
2) Diabetes mellitus: it improve glycemic control & increase
sensitivity insulin -----decrease the dose of medication
3) Hyperlipidemia ------ it decreases serum lipid levels LDL.
4) Obesity:fullness.
Lecture 6+7 - Disorders of Malnutrition
26
Protein Energy Malnutrition (PEM)
A) Kwashiorkor
Lecture 6+7 - Disorders of Malnutrition
27
B) Nutritional Marasmus
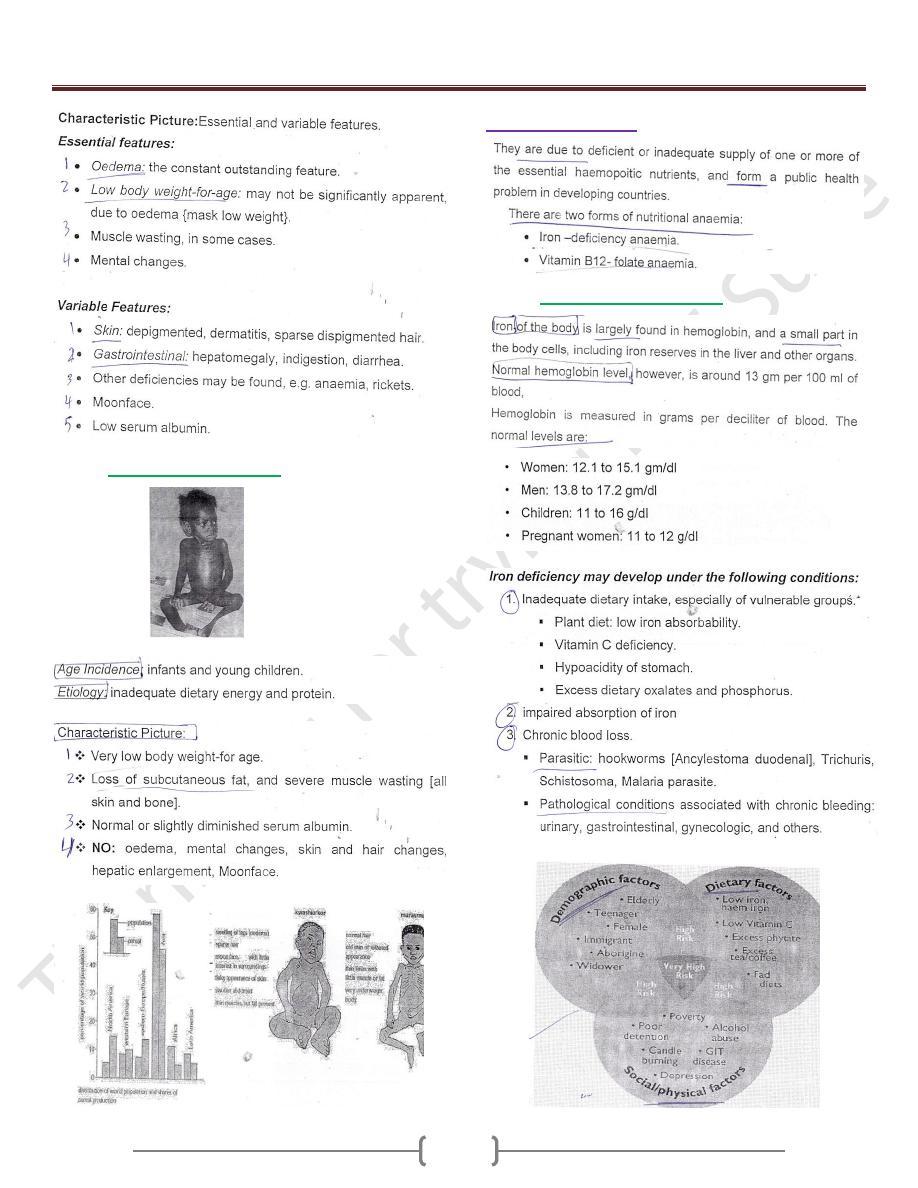
Nutritional Anemia
A) Iron Deficiency Anemia
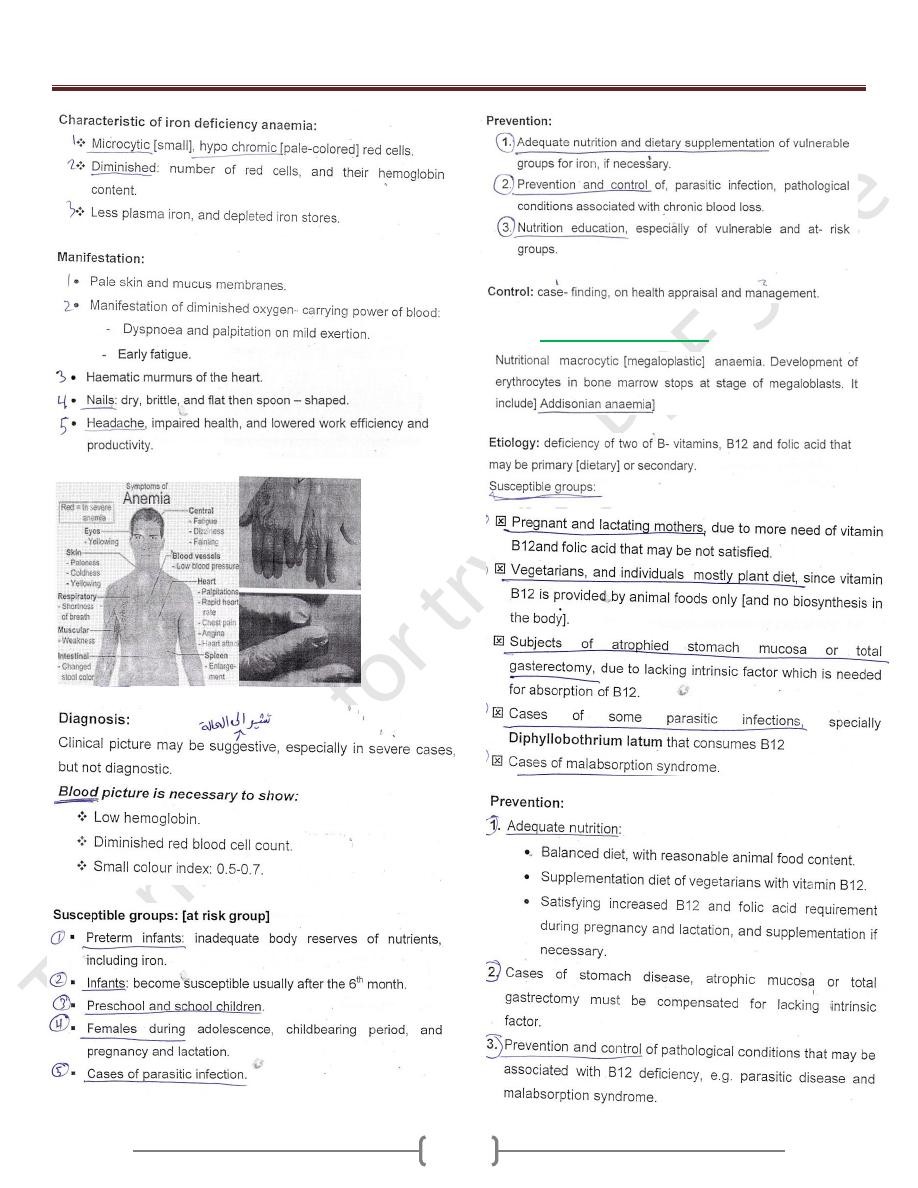
Lecture 6+7 - Disorders of Malnutrition
28
B) Folate-B12 Deficiency
Lecture 6+7 - Disorders of Malnutrition
29
Clinical manifestations:-
Children who have vitamin B-12 deficiency often presents
with nonspecific complaints such as:-
Weakness, Fatigue, Lethargy & FTT.
Other common findings include :-
Pallor, Glossitis (red smooth tongue), Vomiting, Diarrhea &
Icterus.
And Neurological symptoms also occur:-
Parasthesias, Sensory deficits, Hypotonia, Seizures &
Developmental delay.
Iodine Deficiency
Goitrous Areas
Endemic Goiter
Cretinism
Non-Goitrous Areas
