Unit 3: Helminthes (Nematodes)
06
Lecture 6 - Blood and tissue
nematodes
Filariae
The filariae, members of the superfamily filariodea .These
nematodes have a unique stage in their life cycle, the
microfilaria, which distinguishes them as a group.
The adult worm lives in various tissues of the definitive
host including the body cavities, subcutaneous tissues,
and the lymphatic and vascular systems.
The microfilariae produced by the female worm are
motile, and those of some species migrate into the blood
stream; others accumulate in the skin.
Host to host transmission is accomplished when the
microfilaria is ingested by a blood sucking arthropod
intermediate host, in whose tissues it develops to the
infective stage; when the infected arthropod again takes a
blood meal, the larva invades the tissues of the definitive
host through the bite site and develops to the sexually
mature adult stage.
Eight species of filariae are endemic in various parts of
the world, including, Wuchereria bancrofti, Brugia
malayi, Brugia temori, Loa loa, Onchocerca volvulus,
Mansonella ozzardi, Mansonella perstans, and
Mansonella streptocerca
Wuchereria bancrofti (Bancroftian
filariasis)
The disease is widely distributed through the tropical area
of Africa, Asia and Latin America.
Man is the only natural definitive host.
Intermediate host is the female mosquitoes especially
anopheles and culex species.
Morphology
Adult worms found in the lymphatic vessels .They are
small, thread like and have a smooth cuticle.
Females are viviparous. Young embryo fills the uterine
tubes and is confined in thin, hyaline, ovoid shells .The
female discharge motile microfilaria.
Microfilaria from peripheral blood measures 244-246 µm
in length by 75-100 µm in diameter. The anterior end is
bluntly rounded, the posterior end is tapered and the body
is enclosed in large sheath. In stained film the body
appears to be composed of no more than a column of dark
–staining nuclei that do not extend to the end of the tail.
The motile microfilaria make their way from lymphatic to
the blood stream and in most regions of the world,
Wuchereria bancrofti
microfilaria circulate in the peripheral; blood with a
marked nocturnal periodicity and the number is high
between 10 p.m-2 am and are scant , usually absent
during day light hours when they tend to accumulate in
the viscera and particularly in lungs.
Diurnal subperiodic in pacific region, microfilaria show a
marked periodicity but tend to circulate continuously with
some increase in number during the afternoon and
evening hours.
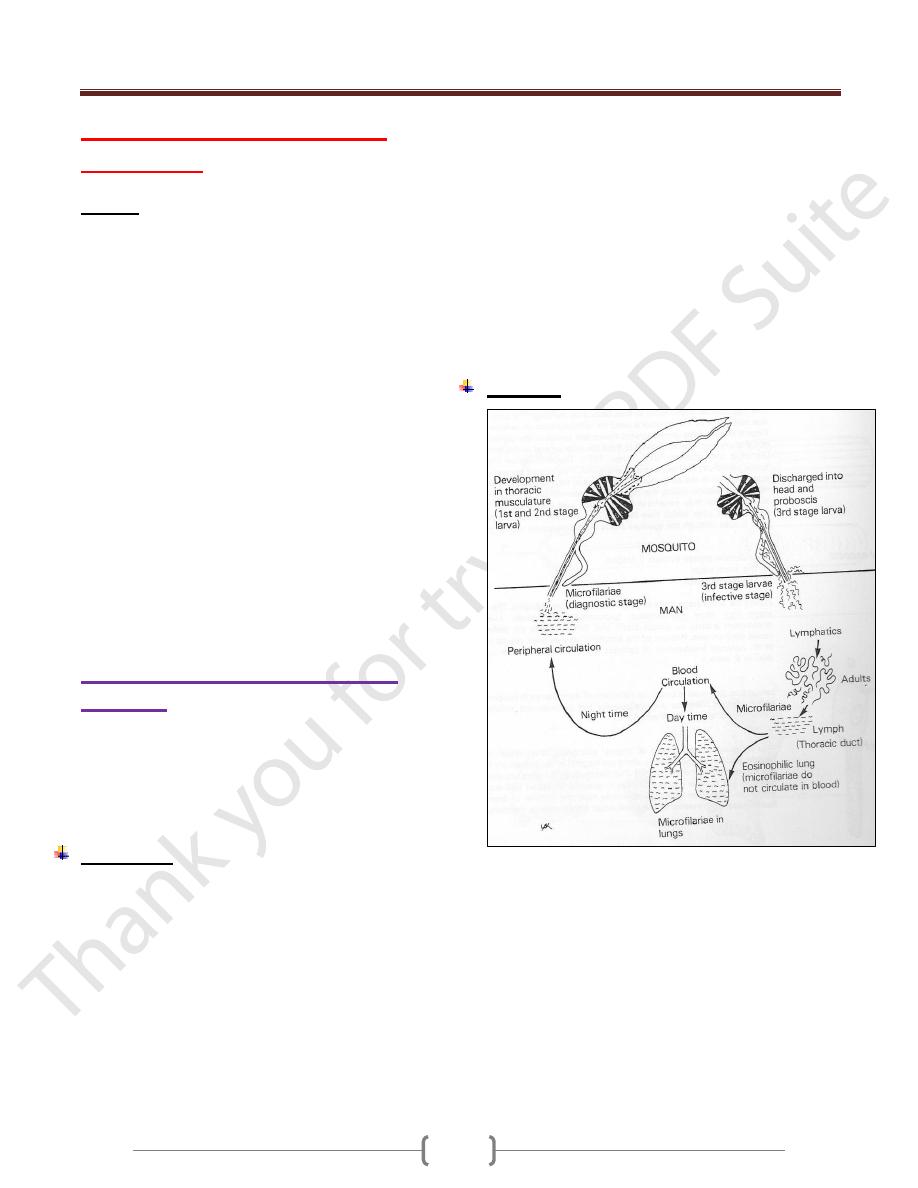
Life cycle
Microfilaria ingested by an appropriate mosquito vector
.within the mosquitoes the microfilaria produce infective
(third-stage) larvae that are transferred to human with the
next bite. After they enter the skin, the larvae move to the
afferent lymph vessels and subcapsular sinuses of the
regional lymph nodes. The time necessary for the worms
to grow to sexual maturity is several months. The mature
adult produces microfilaria which circulates in the blood,
chiefly at night, and are ingested by bitting mosquitoes to
repeat the cycle
Unit 3: Helminthes (Nematodes)
67
Pathogenesis
Adult worms are found in lymph vessels throughout the
body but principally in or around axillary, epitrochlear,
inguinal and pelvic nodes and the lymphatic distal to
them, as well as, in testis, epdidymus, and cord.
In acute stage: symptoms results from infection with
wucheraria bancrofti are caused primarily by locally and
systemic sensitization and tissue reaction to the parasite.
There is an accumulation of histeocyte, epitheloid cells,
lymphocytes, plasma cell, giant cell and eosinophills in
the lumen of the vessel around the worms.
Attacks of lymphangitis and lymphadenitis as a result of
reactions to the products of developing adult or dying
worms or from bacterial or fungal infection. These attacks
are marked by retrograde lymphadenitis, funiculitis,
epidydimytis or orchitis with fever.
Repeated attacks if lymphangitis lead to thickening of the
affected lymphatic vessels which may become
incompetent leading to lymphodema and the lymphatic
vessels tend to become fibrosed after the repeated attacks.
In chronic lymphodema, there will be hyperplasia of the
connective tissue and infiltration of plasma cells,
macrophage, and eosinophils. Finally woody indurations
of the tissues may take place with thick and verrucous
change in the skin leading to elephantiasis.
Clinical features:
1) Asymptomatic: patient is heavily infected without
showing any signs of the disease other than large number
of microfilariae in the circulating blood.
In some patient, the presence of even few numbers of
worms provokes severe reaction and this is character of
immunologically naïve patient rather than those who are
native to the endemic area.
2) Acute phase: characterized by fever, lymphangitis,
lymphodema, and fever. These attacks remain high for 1-
2 days and gradually subside over 2-5 days period.
3) Chronic phase: repeated acute attacks lead to Odem and
fibrosis of the leg and genitalia (scrotum) lymphatic
vessels. Elephantiasis occurs mainly in those with
repeated attacks over long period of time.
4) Tropical pulmonary eosinophilia is characterized by
coughing and wheezing especially at night .These
symptoms are caused by microfilariae in the lung that
elicit immediate hypersensitivity reaction characterized by
high IgE concentration and eosinophilis .Peripheral blood
don’t show any parasites.
Diagnosis:
1) Thick blood smears taken from the patient at night reveal
the microfilariae.
2) Antigen detection using an immunoassay for circulating
filarial antigens constitutes a useful diagnostic approach,
because microfilaremia can be low and variable. A rapid-
format immunochromatographic test, applicable to
Wuchereria bancrofti antigens, has been recently
evaluated in the field.
3) Molecular diagnosis using polymerase chain reaction is
available for W. bancrofti
Treatment:
Diethylcarbamazine is effective only against microfilariae
No drug therapy for adult worms is available.
Onchocerca volvulus (Onchocerchiasis)
It is endemic in Africa, Central America and small area in
Yemen.
The disease is a major cause of blindness and called (river
blindness), because the black flies develop in rivers and
people who live along those rivers are affected. Infection rate
are often greater than 80% in areas of endemic infection.
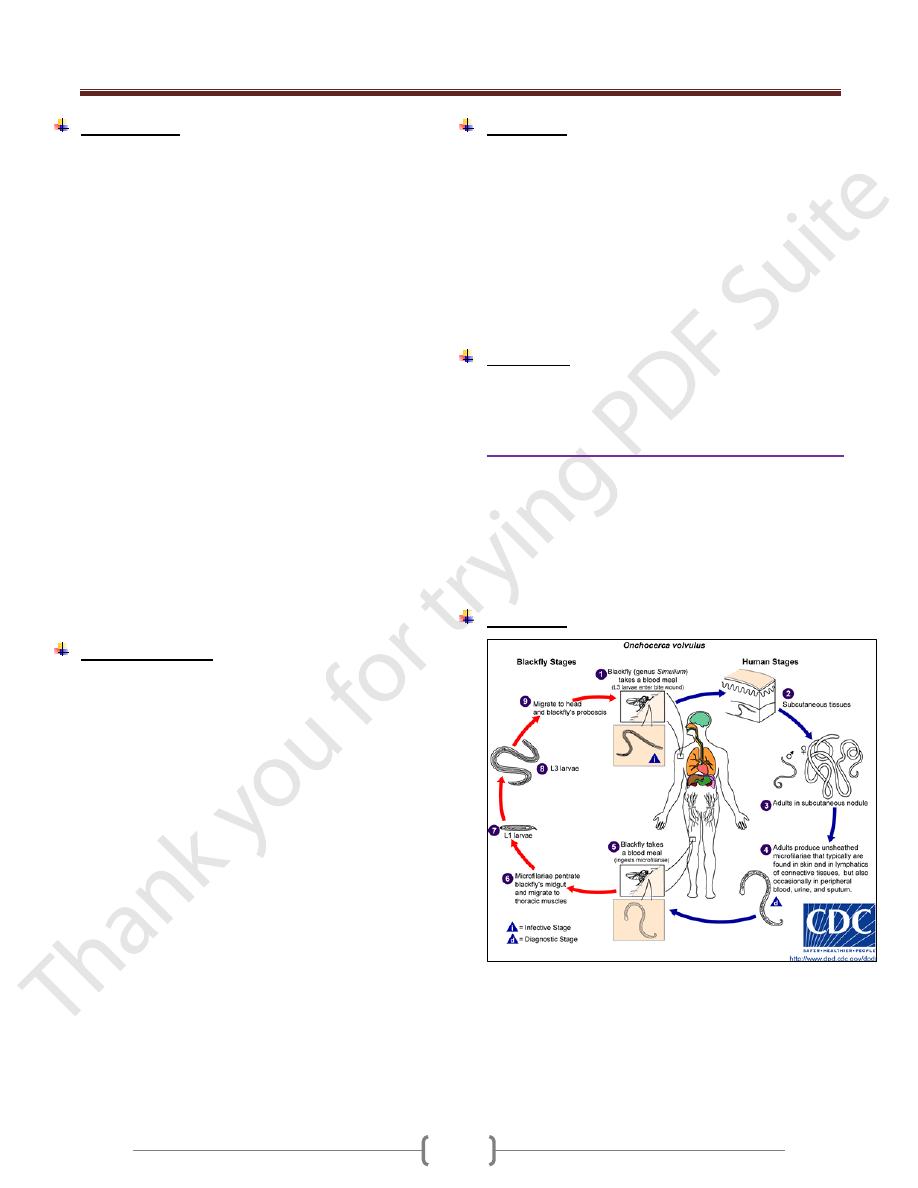
Life cycle:
Human are infected when the female blackfly ,simulium,
deposits infective larvae while bitting .The larvae enter
the wound and migrate into the subcutaneous tissue where
they differentiate into adult ,usually within dermal
nodules. The female produces microfilaria that is ingested
when another blackfly bites. The microfilaria develops
into infective larvae to complete the cycle.
Unit 3: Helminthes (Nematodes)
67
The microfilaria lacks a sheath; the column of the nuclei
doesn't extend to the end of the tail.
The microfilaria typically found in the upper layers of the
dermis, frequently in the urine, in cytology smear and
rarely in blood.
Pathogenesis and symptomatology
The presence of the adult worm causes a local cellular
reaction of a fibrotic nature; results in encapsulation of the
worms. There may be only a single nodule or many.
In Africa the nodules are common about the pelvis (iliac
crest), trochanters and the lateral chest wall.
In America, nodules are more common on the head.
The dispersal of microfilaria into the dermal layers of the
skin throughout the body causes various types of acute
and chronic skin lesions
Sowda: localized onchocerchiasis in Yemen
Lymphadenopathy is commonly associated with
onchocerchiasis.
In some areas of Africa, hanging groin: a sac like
projection of loose, atrophied skin containing a mass of
large, fibrotic lymph gland.
Ocular complications are the most serious consequences
in some area of Africa and central America in which the
microfilaria invade all tissues of the eye, producing
congestion, hemorrhage and degeneration of the tissues as
well as degenerative changes in the optic nerve.
Diagnosis:
Biopsy of the affected skin reveals microfilaria.
Treatment
Ivermectin against microfilaria but not the adult.
Suramin kills adult worm but it is toxic and is used
particularly in those with eye disease.
Loa Loa
Disease: Loiasis.
The disease is endemic in tropical central and West Africa.
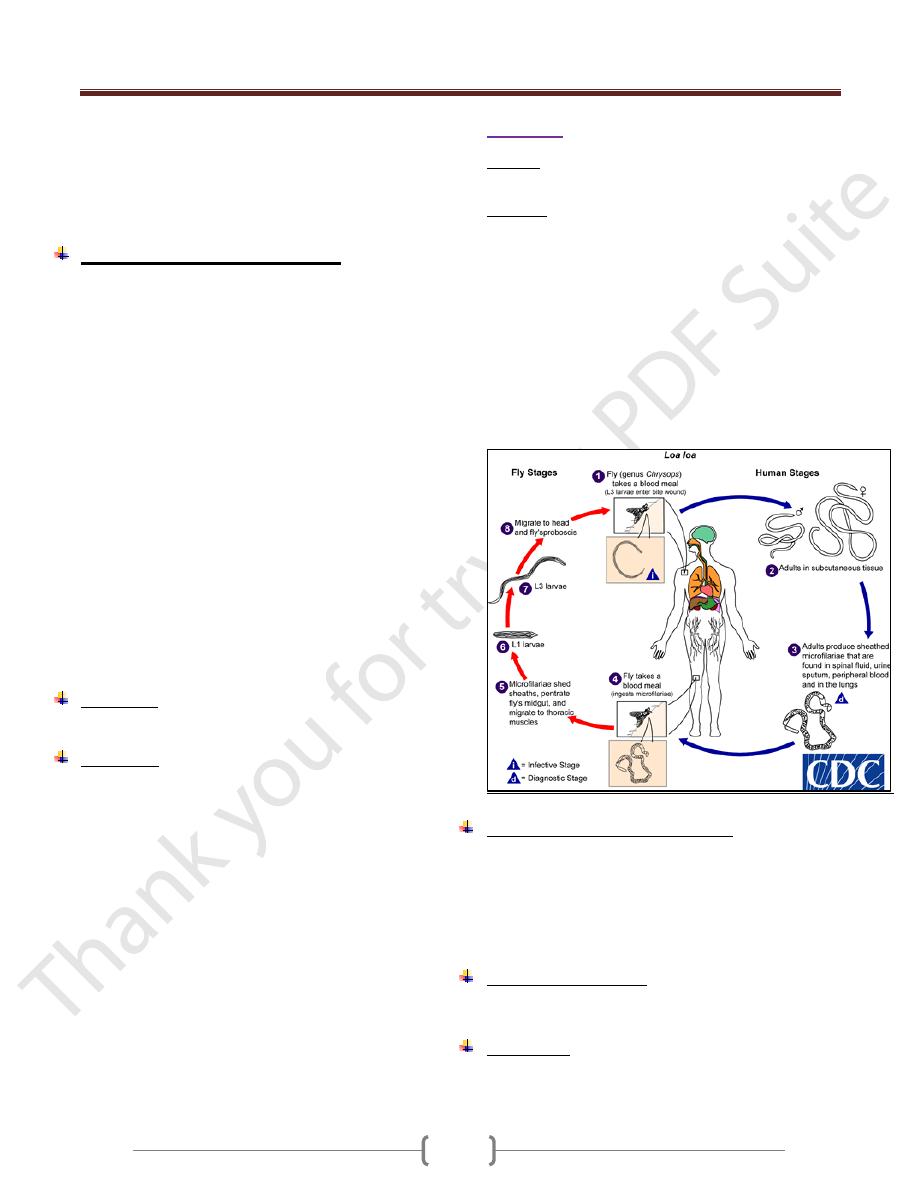
Life cycle
Humans are infected by the bite of the deer fly (mango
fly), Chrysops), which deposits infective larvae on the
skin. The larva enters the bite wound, wanders in the body
and develops into adults. The females release
microfilariae that enter the blood, particularly during the
day. The microfilariae are taken up by the fly during a
blood meal and differentiate into infective larvae, which
continue the cycle when the fly bites the next person.
The microfilaria is sheathed and exhibits a diurnal
periodicity in the peripheral blood .The column cells
(nuclei) extend to the tip of the tail.
Pathogenesis and clinical features:
There is no inflammatory response to the micofilariae or
the adults, but a hypersensitivity reaction causes transient
localized, non-erythematous, subcutaneous edema
(Calabar swelling) .The most dramatic finding is an adult
worm crawling across the conjunctiva of the eye, a
harmless but disconcerting event.
Laboratory diagnosis:
Visualization of the microfilariae in a blood smear
No serological test.
Treatment:
Diethylcarbamazine eliminates the microfilariae and may
kill the adults.Worms in the eye require surgical excision.
Unit 3: Helminthes (Nematodes)
67
Dracunculus medinensis.
Guinea fire worm
Dracunculiasis
The disease occurs over large areas of tropical Africa, the
Middle East, and India. Though it is sometimes classed
with filarial worms, Dracunculus is not a true filaria.
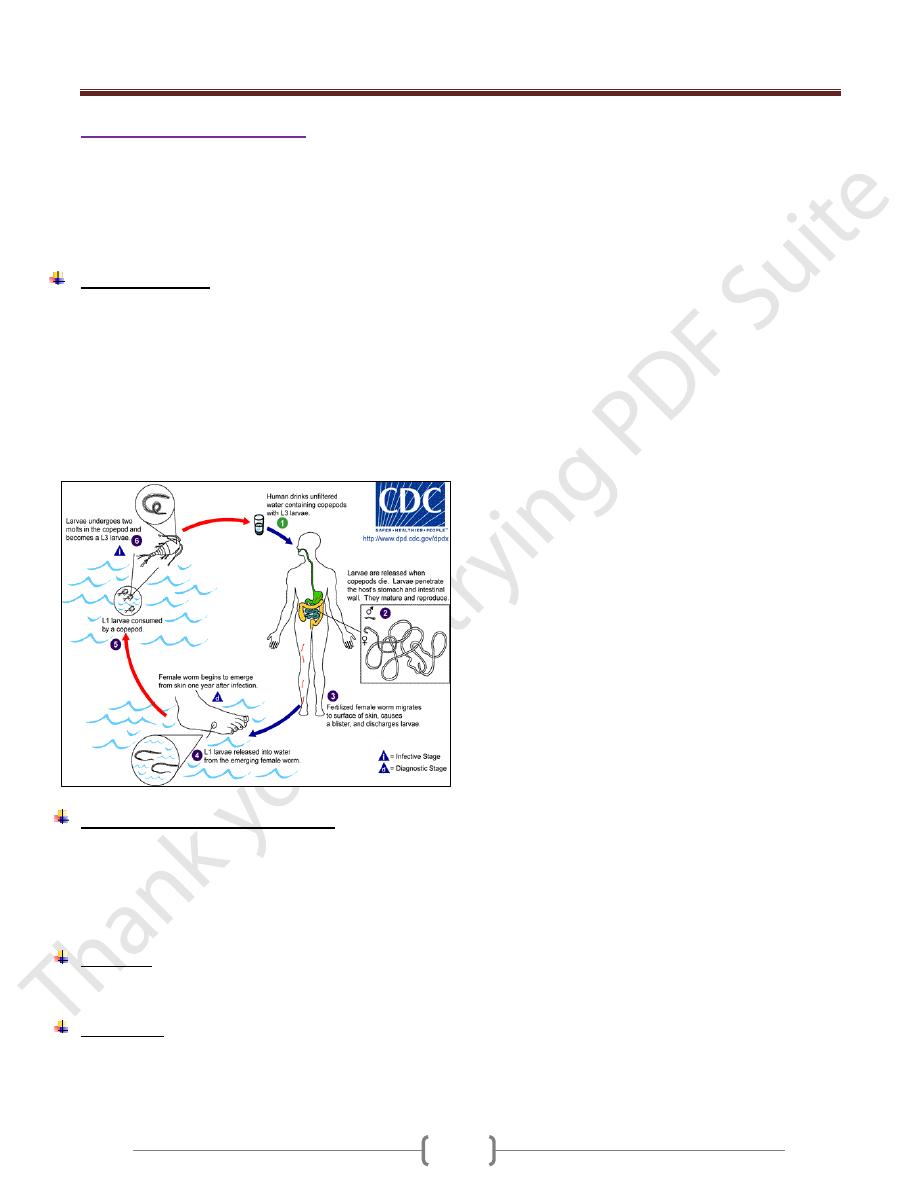
Life cycle:(Fig.1)
Humans are infected when tiny crustaceans (copepods)
containing infective larvae are swallowed in drinking
water. The larvae are released in the small intestine and
migrate through the intestinal wall into deep somatic
tissue, where they develop into adults. Meter –long adult
females cause the skin to ulcerate and then release motile
larvae into fresh water. Copepods eat larvae, which molt
to form infective larvae .The cycle is completed when
these are ingested in the water.
Pathogenesis and clinical finding:
The adult female produces a substance that causes an
inflammation, blistering, and ulceration of the skin,
usually of the lower extremities. The inflamed papule
burns and itches, and the ulcer can become secondarily
infected.
Diagnosis
Is usually made clinically by finding the head of the worm
in the skin ulcer.
Treatment:
Gradually extracting the worm by winding it up on a stick
over a period of days.Thiabendazole or metronidazole
makes the worm easier to extract.
