THE OEDEMATOUS CHILD
Oedema is a common presenting problem in paediatrics. It is defined as accumulation of excess interstitial fluid and could be localised or generalised. Oedema results from either excess salt and water retention of from increased transfer of fluid across the capillary membranes. As such, it could be a presentation of mild conditions such as insect bite reaction to more serious conditions such as glomerulonephritis, hepatic and cardiac disease. Understanding the pathophysiology of oedema is important in the clinical approach and management of this condition in children.Contents
Causes of oedemaClinical approach
Investigations
Management
CAUSES OF OEDEMA
Oedema results when there is:1) Increased hydrostatic pressure
• acute nephritic syndrome, acute tubular necrosis, cardiac failure
2) Decreased plasma oncotic pressure (hypoproteinaemic states)
• nephrotic syndrome, chronic liver failure, protein losing enteropathy, protein
• caloric malnutrition
3) Increased capillary leakage
• insect bite, trauma, allergy, sepsis, angio-oedema
4) Impaired lymphatic flow
• lymphatic obstruction (tumour), congenital lymphoedema
5) Impaired venous flow
• hepatic venous outflow obstruction, superior/inferior vena cava obstruction
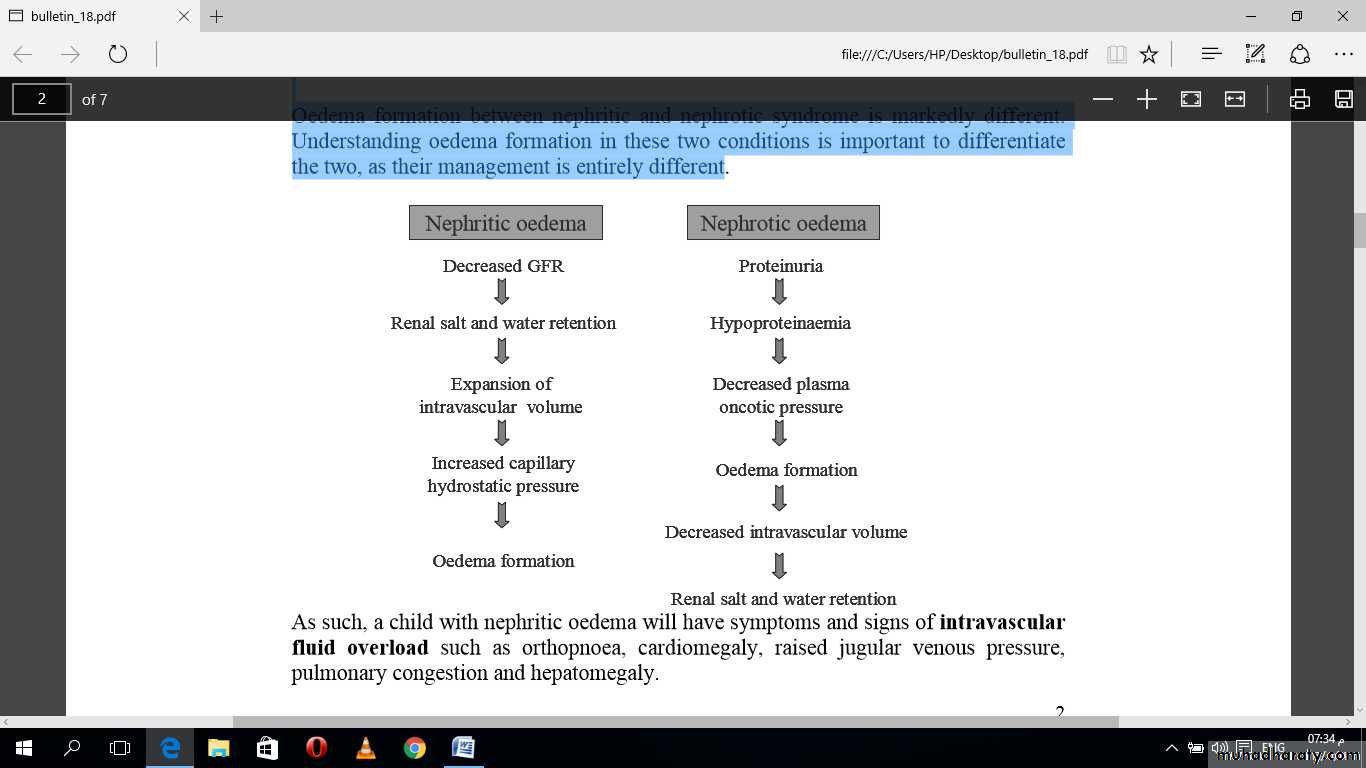
Mechanism of oedema formation in renal disease
Oedema formation between nephritic and nephrotic syndrome is markedly different. Understanding oedema formation in these two conditions is important to differentiate the two, as their management is entirely different
As such, a child with nephritic oedema will have symptoms and signs of intravascular fluid overload such as orthopnoea, cardiomegaly, raised jugular venous pressure, pulmonary congestion and hepatomegaly.
CLINICAL APPROACH TO AN OEDEMATOUS CHILD
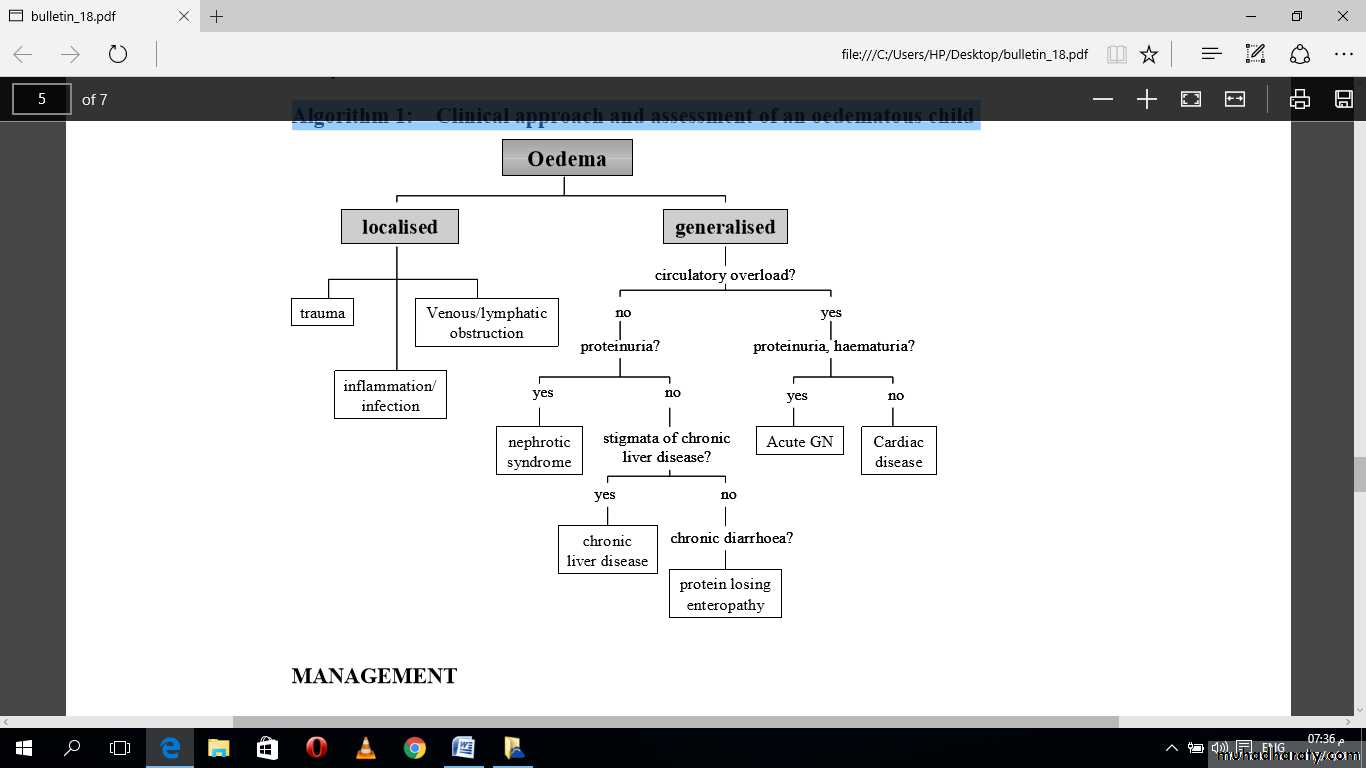
1. Confirm oedema.2. Assess distribution of oedema: Localised versus generalised. In generalised oedema, look for dependent areas such as pretibial, sacral, scrotal, vulval oedema other than peri-orbital oedema and ascites.
3. Detailed history and physical examination to assess severity, associated complications and underlying cause of the oedema (algorithm . A) Localised oedema
i. History of trauma, insect bite or infection ii. Peripheral lymphoedema in newborn – to exclude Turner’s syndrome iii. Acute oedema of the face and neck – to exclude superior vena cava obstruction syndrome
B) Generalised oedema
i. Renal disease (most common cause in children) - gross haematuria, oliguria, hypertension, cardiomegaly, pulmonary oedema to suggest acute glomerulonephritis. Frothy urine suggests nephrotic syndrome. Absence of circulatory congestion differentiates nephrotic syndrome from nephritic syndrome. - signs and symptoms of chronic renal insufficiency such as anaemia, growth retardation and uraemic symptoms such as nausea and vomiting - exclude secondary causes such as post-infectious glomerulonephritis, systemic lupus erythematosus, Henoch Schonlein purpura nephritis.
ii. Liver disease - stigmata of chronic liver disease such as jaundice, palmar erythema, clubbing, pruritic rash - hepatosplenomegaly with gross ascites in the absence of jaundice to exclude portal vein thrombosis - previous operation scar such as Kasai porto-enterostomy
iii. Allergic reactions - oedema usually mild, commonly periorbital - history of allergen exposure such as medications, animal dander, food preservatives and colouring - associated rashes such as urticaria - assess for Stevens-Johnson reaction - if recurrent oedema, consider C1 esterase deficiency
iv. Cardiac disease - symptoms of congestive cardiac failure such as decreased effort tolerance, orthopnoea, paroxysmal nocturnal dyspnoea and signs such as cardiomegaly, gallop rhythm, lung crepitations and turgid liver - assess for underlying cause such as structural heart disease, cardiomyopathy and myocarditis Note: oedema in cardiac disease often denotes a late sign in small children
v. Protein losing enteropathy - history of chronic diarrhoea, steatorrhoea and recurrent abdominal pain - detailed dietary history for possible milk allergy and gluten hypersensitivity - consider coeliac disease and inflammatory bowel disease in northern Indians and Caucasians - assess for complications of anaemia, malnutrition and vitamin deficiency states
4. Investigations
Basic investigations could be conducted at the general practice set-up to delineate the major causes of oedema and assess its severity. They include:
a) Urine dipstick and microscopy - proteinuria, haematuria and casts are indicative of renal disease
b) Renal function test - raised serum urea and creatinine are indicative of renal disease
c) Full blood count - normochromic normocytic anaemia suggest chronic disease - hypochromic microcytic anaemia suggest iron deficiency from occult gastrointestinal bleeding i.e. cows milk allergy - megaloblastic anaemia suggest vitamin B12 and folate deficiency from small bowel disease
d) Liver function test - hypoalbuminaemia in the absence of circulatory overload suggests hypoproteinaemic states - hyperbilirubinaemia and transaminitis suggest liver disease
e) Chest X-ray and electrocardiogram - cardiomegaly with prominent perihilar vascular markings/upper lobe diversion and left ventricular hypertrophy confirms intravascular fluid overload
Further investigations are indicated upon specialist referral depending on the most likely cause.
Algorithm 1: Clinical approach and assessment of an oedematous child
MANAGEMENT
Subsequent management of oedema is dependent on the primary cause and its severity. What you can doA) Localised oedema
Management
1. Insect bite reaction ------->Anti-histamine, anti-inflammatory (topical steroid)
2. Local infection -------> Incision and drainage, wound dressing, antibiotics
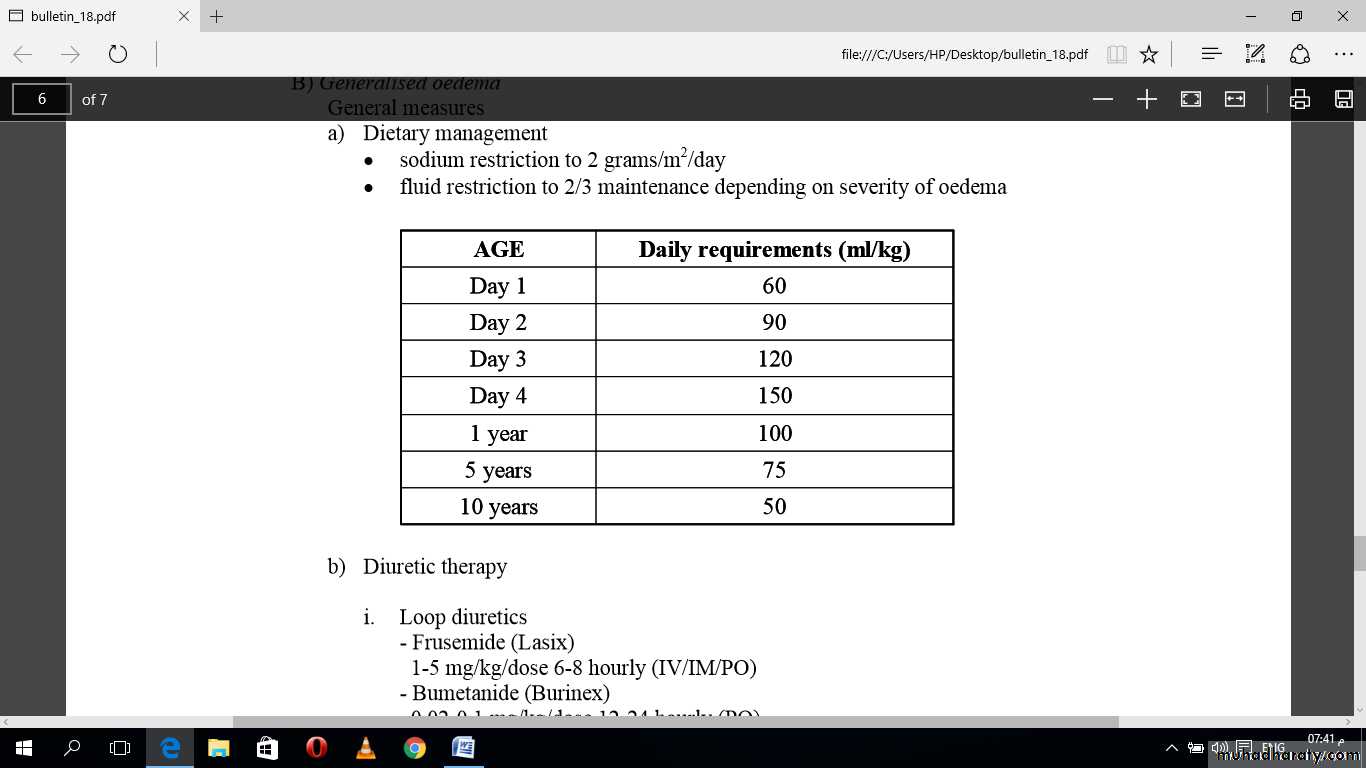
B) Generalised oedema
General measuresa) Dietary management
sodium restriction to 2 grams/m2/day
fluid restriction to 2/3 maintenance depending on severity of oedema
b) Diuretic therapy
i. Loop diuretics- Frusemide (Lasix)
1-5 mg/kg/dose 6-8 hourly (IV/IM/PO)
- Bumetanide (Burinex)
0.02-0.1 mg/kg/dose 12-24 hourly (PO) 0.1-0.2 mg/kg/dose 8-12 hourly (IV/IM)
Note: higher doses are required in acute glomerulonephritis or chronic renal impairment
Side effects- hyponatremia, hypokalemia, metabolic alkalosis
ii. Hydrochlorothiazide
- 1 mg/kg/dose 12-24 hourly (PO)
iii. Spironolactone
- used in combination with loop diuretics/ thiazides for potassium sparing effects
0-10 kg: 6.25 mg/dose 12 hourly (PO)
11-20 kg: 12.5 mg/dose 12 hourly (PO)
21-40 kg: 25 mg/dose 12 hourly (PO)
> 40 kg: 25 mg/dose 8 hourly (PO)
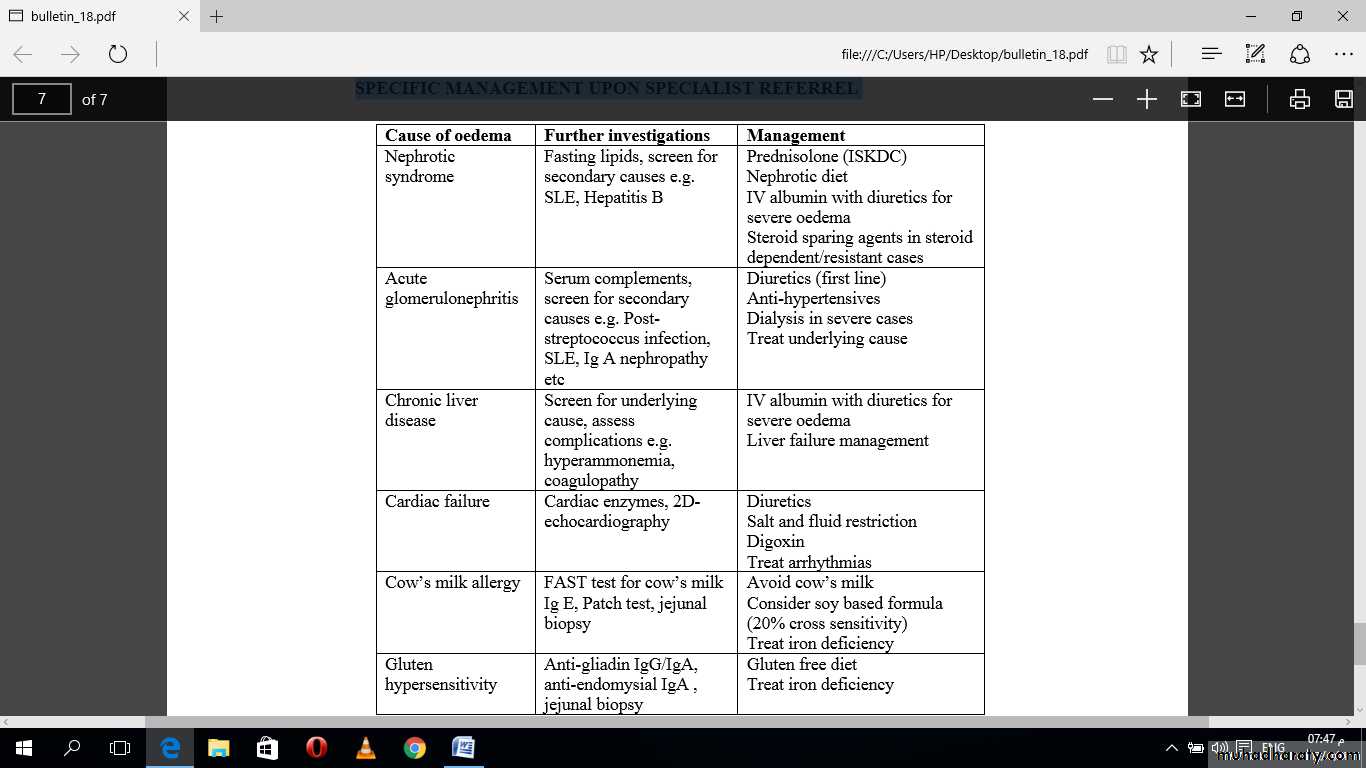
SPECIFIC MANAGEMENT UPON SPECIALIST REFERREL
CONCLUSION
Oedema can be due toincreased hydrostatic pressure
decreased plasma oncotic pressure
increased capillary leakage
impaired lymphatic flow
impaired venous flow
This could be a manifestation of a mild or a serious medical conditions such as renal, hepatic or cardiac diseases. Early recognition of oedema and prompt diagnosis of the underlying cause is important. Initial assessment and stabilisation of patient should be instituted prior to specialist referral.