1
Lec.1
Pediatrics
6
th
stage
tutorial
د.رؤى
Diabetic ketoacidosis
Diabetes mellitus (DM) is a common, chronic, metabolic
syndromecharacterized by hyperglycemia as a cardinal biochemical
feature. Themajor forms of diabetes are classified according to those
caused byß-cell damage (type 1DM, or T1DM) and those that are a
consequence of insulin resistance occurring at the level of skeletal
muscle, liver, and adipose tissue, with various degree of β-cell
impairment (type 2 DM, or T2DM). T1DM isthe most common
endocrine-metabolic disorder of childhood andadolescence, with
important consequences for physical and emotional
development. Individuals with T1DM confront serious lifestylealterations
that include an absolute daily requirement for exogenousinsulin, the
need to monitor their own glucose level, and the need to payattention
to dietary intake. The acute clinical manifestations are due
tohypoinsulinemic hyperglycemic ketoacidosis. Autoimmune
mechanisms are factors in the genesis of T1DM.
Diabetic Ketoacidosis
DKA is the end result of the metabolic abnormalities resulting from
a severe deficiency of insulin or insulin effectiveness. The latter occurs
during stress as counter-regulatory hormones block insulin action. DKA
occurs in 20-40% of children with new-onset diabetes and in children
with known diabetes who omit insulin doses or who do not successfully
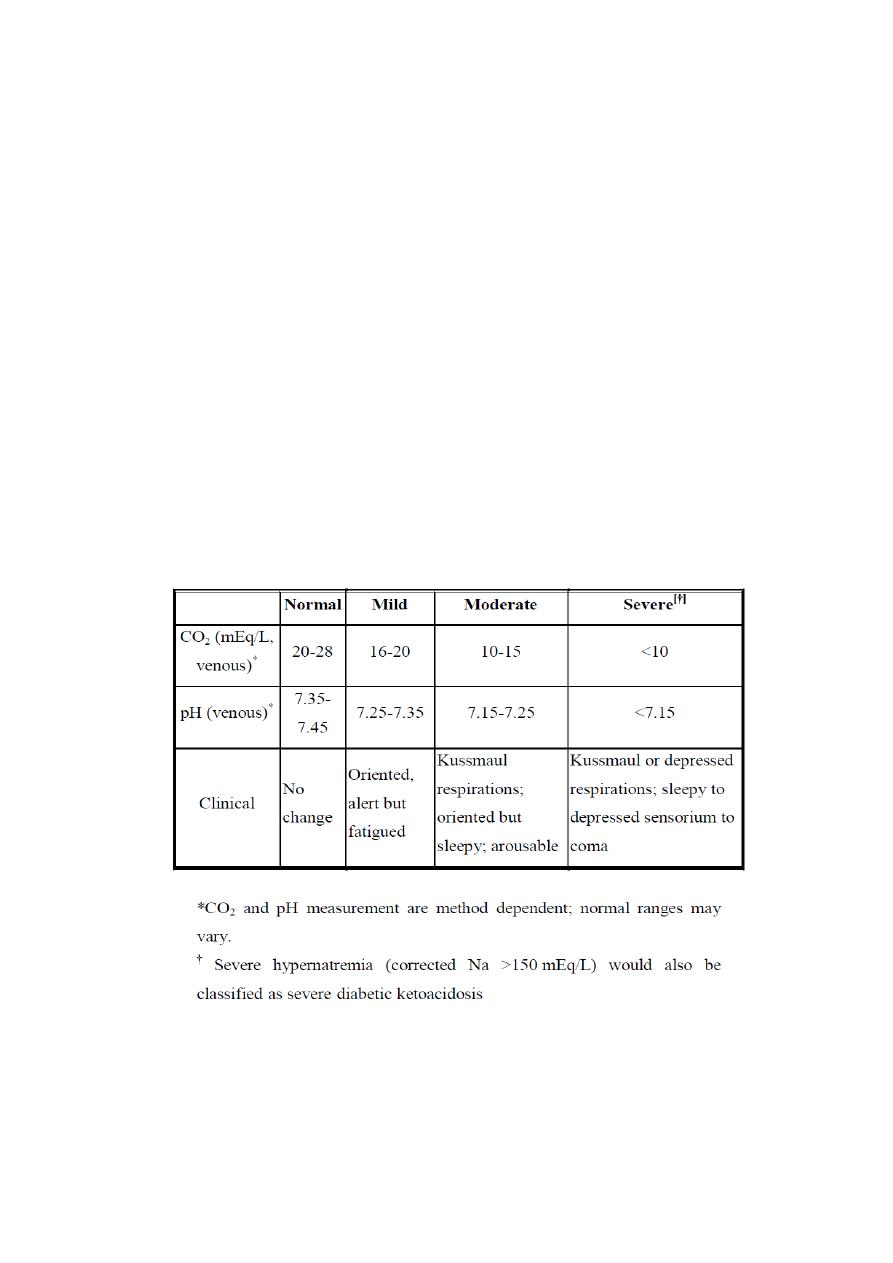
manage an intercurrent illness. DKA may be arbitrarily classified as mild,
2
moderate, or severe (Table 1), and the range of symptoms depends
on the depth of ketoacidosis. There is a large amount of ketonuria, an
increased ion gap, a decreased serum bicarbonate (or total CO2) and pH,
pathophysiology
Table (1): Classification Of Diabetic Ketoacidosis

3
DKA is the end result of metabolic abnormalities resulting from a severe
deficiency of insulin→3 physiologic processes:
1. increased glucose production coupled with decreased glucose
utilization raises serum glucose→increased serum osmolality
→hypertonic dehydration.
2. increased release of free fatty acids from peripheral fat stores supplies
substrate for hepatic ketoacid production→ accumulation of large
amounts of ketoacids→ ketonuria, increase ion gap, decrease serum
bicarbonate,and decrease PH.
3. Metabolic acidosis→ cellular losses of potassium, phosphorus and
sodium.
Clinical features
Insidious increased thirst (ie, polydipsia) and urination (ie, polyuria)
are the most common early symptoms of diabetic ketoacidosis (DKA).
Malaise, generalized weakness, and fatigability also can present as
symptoms of DKA.
Nausea and vomiting usually occur and may be associated with
diffuse abdominal pain, decreased appetite, and anorexia. A history of
rapid weight loss is a symptom in patients who are newly diagnosed with
type 1 diabetes.
Patients may present with a history of failure to comply with insulin
therapy or missed insulin injections due to vomiting or psychological
reasons. Decreased perspiration is another possible symptom of DKA.
Altered consciousness in the form of mild disorientation or
confusion can occur. Although frank coma is uncommon, it may occur
when the condition is neglected or if dehydration or acidosis is severe.

4
Among the symptoms of DKA associated with possible intercurrent
infection are fever, dysuria, coughing, malaise, chills, chest pain,
shortness of breath, and arthralgia.
Physical Examination
General signs of diabetic ketoacidosis (DKA) may include the
followin:
٭
Ill appearance
٭
Dry skin
٭
Labored respiration
٭
Dry mucous membranes
٭
Decreased skin turgor
٭
Decreased reflexes
٭
Characteristic acetone (ketotic) breath odor
٭
Effects on vital signs that are related to DKA may include the following:
Tachycardia
Hypotension
Tachypnea
Hypothermia
Fever, if infection is present
٭
Specific signs of DKA may include the following:
Confusion
Coma

5
Abdominal tenderness
The physical examination should also include detection of the signs
of possible intercurrent illnesses such as urinary tract infection,
pneumonia, and perinephric abscess. Search for signs of
infection is mandatory in all cases.
Laboratory Finding
Diabetic ketoacidosis is typically characterized by hyperglycemia
over 300 mg/dL, a bicarbonate level less than 15 mEq/L, and a pH less
than 7.30, with ketonemia and ketonuria.
Laboratory studies for diabetic ketoacidosis (DKA) should be scheduled
as follows:
Blood tests for glucose every 1-2 h until patient is stable, then
every 6 h.
Serum electrolyte determinations every 1-2 h until patient is stable,
then every 4-6 h.
Initial blood urea nitrogen (BUN).
Initial arterial blood gas (ABG) measurements, followed with
bicarbonate as necessary.
Repeat laboratory tests are critical, including potassium,
glucose,electrolytes, and, if necessary, phosphorus.
Serum Glucose Study
The blood glucose level for patients with DKA usually exceeds 250

6
mg/dL. The clinician can perform a fingerstick glucose test while waiting
for the serum chemistry panel.
Urine Dipstick Testing
For patients with DKA, the urine dipstick test is highly positive for
glucose and ketones.
Arterial Blood Gases
In patients with DKA, arterial blood gases (ABGs) frequently show
typical manifestations of metabolic acidosis, low bicarbonate, and low
pH
(< 7.2).
Serum Electrolyte Panel
Serum potassium levels initially are high or within the reference
range in patients with DKA. This is due to the extracellular shift of
potassium in exchange of hydrogen, which is accumulated in acidosis, in
spite of severely depleted total body potassium. This needs to be
checked
frequently, as values drop very rapidly with treatment.
An ECG may beused to assess the cardiac effects of extremes in
potassium levels.
The serum sodium level usually is low in affected patients. The
osmotic effect of hyperglycemia moves extravascular water to the
intravascular space. For each 100 mg/dL of glucose over 100 mg/dL,
theserum sodium level is lowered by approximately 1.6 mEq/L. When
glucose levels fall, the serum sodium level rises by a corresponding
amount.

7
Additionally, serum chloride levels and phosphorus levels always are
lowin these patients.
Bicarbonate
Use bicarbonate levels in conjunction with the anion gap to assess the
degree of acidosis that is present.
Anion Gap
In patients with diabetic ketoacidosis, the anion gap is elevated ([Na
+ K] - [Cl + HCO3] >13 mEq/L).
CBC Count
Even in the absence of infection, the CBC count shows an increased
white blood cell (WBC) count in patients with diabetic ketoacidosis. High
WBC counts (>15 X 109/L) or marked left shift may suggest underlying
infection.
Renal Function Studies
BUN frequently is increased in patients with diabetic ketoacidosis.
Osmolarity
Plasma osmolarity usually is increased (>290 mosm/L) in patients
with diabetic ketoacidosis.
Patients with diabetic ketoacidosis who are in a coma typically have
osmolalities greater than 330 mosm/kg..
Cultures
Urine and blood culture findings help to identify any possible
infecting organisms in patients with diabetic ketoacidosis.

8
Chest Radiography
Chest radiography should be used to rule out pulmonary infection
such as pneumonia.
MRI
An MRI is helpful in detecting early cerebral edema; it should be ordered
only if altered consciousness is present.
CT Scanning
The threshold should be low for obtaining a head CT scan in
children with diabetic ketoacidosis who have altered mental status, as
this
may be caused by cerebral edema.
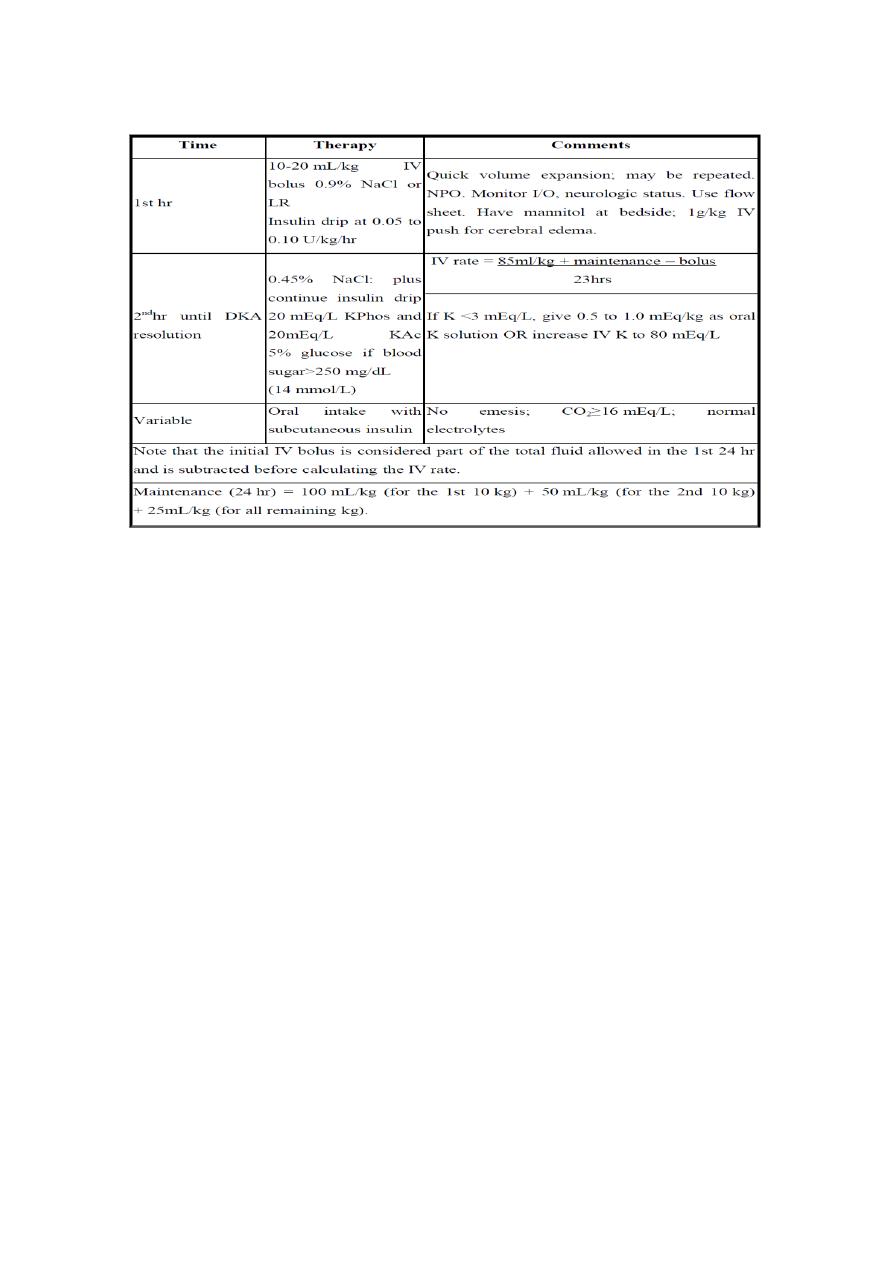
potassium should be added as soon as it has been
established that the patient has urine output , even if K is on the high
side
of normal , to anticipate the massive intracellular shift as insulin reverse
the catabolic state. Because the patient will receive an excess of chloride
,which may aggravate acidosis , it is prudent to use potassium phosphate
rather than potassium chloride as a potassium source
9
Complications
1
. Cerebral edema
*Cerebral edema occurs in 0.7-1% of children with diabetic
ketoacidosis
* Causes are multifactorial but may include too-rapid infusion
of fluids and electrolytes, overhydration, and overly
aggressive correction of acidosis or hyperglycemia.
* Treatment includes intubation, hyperventilation, and
mannitol 0.25-1 g/kg intravenously.
2. Hypoglycemia
* Causes include increased sensitivity to exogenous insulin
and insufficient serum glucose for insulin to metabolize.
* Treatment includes adding 5-10% dextrose to intravenous
Diabetic Ketoacidosis (DKA) Treatment Protocol:
11
fluids when serum glucose level is 250-300 mg/Dl.
3. Hypokalemia
* Serum potassium begins to reflect actual total body
potassium depletion as volume depletion and acidosis
resolve.
* Add potassium to intravenous fluids when urine output is present and
results ofserum potassium level are available.
4. Cardiac dysrhythmia
5. Pulmonary edema
Morbidity and mortality
Diabetic ketoacidosis is the most common cause of diabetes-related
death in childhood. Without insulin therapy, the mortality rate is 100%,
but current mortality rates are around.
Treatment for diabetic ketoacidosis may cause life-threatening,
predictable, and avoidable acute complications such as hypokalemia,
hypoglycemia, hyponatremia, and fluid overload. Other complications,
such as cerebral edema, are not as predictable but are very important.
Indeed,Cerebral edema complicating DKA remains the major cause of
morbidity and mortality in children and adolescents with T1DM.
However, its etiology remains unknown.
Prognosis
The overall mortality rate for DKA is 2% or less. The presence of deep
coma at the time of diagnosis, hypothermia, and oliguria are signs of
poor

11
prognosis.
The prognosis of properly treated patients with diabetic ketoacidosis
is excellent, especially in younger patients if intercurrent infections are
absent. The worst prognosis usually is observed in older patients with
severe intercurrent illnesses (eg, myocardial infarction, sepsis, or
pneumonia), especially when these patients are treated outside an
intensive care unit.
