Unit 4: Virology
211
Lecture 11+12 - DNA enveloped
viruses
Herpesviruses
The herpesvirus family contain six important human
pathogens
1) Herpessimplex virus type 1
2) herpessimoplexvirus type 2
3) varicella zoster virus
4) cytomegalovirus
5) Epstein-Barr virus
6) Human herpes virus 8 (the cause of kaposi´s sarcoma).
All herpesviruses are structurally similar:
1) Enveloped with icosahedral symmetry.
2) Linear DS-DNA.
3) No virion polymerase.
4) They are large in size second in size to pox virus.
5) Replication in nucleus
6) Tegument (play a role in replication) located between
nucleocapsid and the envelope.
They produce latent asymptomatic infection following the
primary acute infection. Some have symptoms of the
latent similar to that of the primary while the other the
symptoms of the latent infection are differ from that of
primary one.
Three of herpesvirus (HSV-1,2 .VZV) cause a vesicular
rash both in primary and in reactivation.
Four herpesvirus induce formation of multinucleated giant
cells ( HSV1,2,VZV,and CMV).
Certain herpes virus cause cancer in man ( e.g: Epestein
Barre virus).
The herpesvirus family can be subdivided into three
categories base on the type of cell most infected and the
site of latency.
Alpha herpesvirus: HSV1,2 VZV) infect epithelial
cells and cause latency in neurons.
Beta herpesviruses: ( CMA,HH6) infect and become
latent in a variety of tissue.
Gamma herpesviruses: Epestein_Barr virus and
HHV8) infect and become latent in lymphoid cells.
Herpesvirus 1&2
They are structurally and morphologically
indistinguishable. They can be distinguished by their
antigenicity and location of lesions.
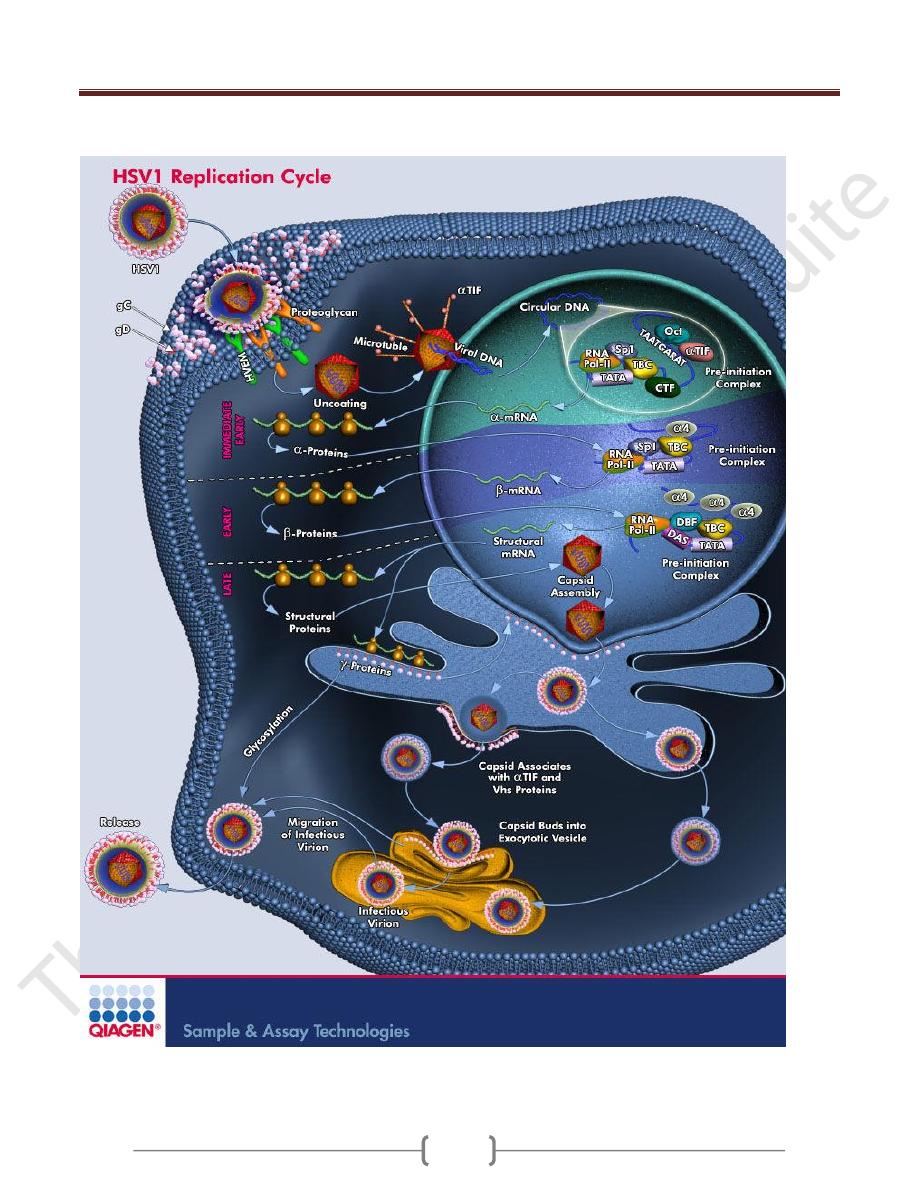
Replicative cycle (as shown in the figure below)
1) HSV-1 binds first to heparin sulfate on the cell surface
and then to second receptor, nectin.
2) Following fusion of the viral envelope with the cell
membrane, the nucleocapsid and the tegument proteins
are released into the cytoplasm.
3) Viral NC is transported to the nucleus, where it docks to a
nuclear pore and the genome DNA enters the nucleus
along with tegument protein VP 16. the linear genome
DNA now becomes circular.
4) VP 16 interacts with cellular transcription factors to
activatew transcription of viral immediate early (IE) genes
by host cell RNA polymerase.
5) IE mRNA is translated into IE proteins that regulate the
synthesis of early proteins such as DNA polymerase
(repilicate the genome) and thymidine Kinase .
6) Viral DNA polymerase replicate the genome DNA at
which early protein synthesis is shut off and late protein
synthesis begin.
7) The late, structural protein are transported to the nucleus
where virion assembly occurs by budding through nuclear
membrane.
Note: immediate early proteins are proteins whose mRNA
synthesis is activated by a protein brought in by incoming
parental virion whilt early protein do require the synthesis
of new viral regulatory proteins to activate the
transcription of their mRNAs.
Transmission and epidemiology
HSV-1 is transmitted primarily by saliva.
HSV-2 is transmitted by sexual contact.
Pathogenesis and Immunity:
1) Virus replicate in the skin or mucous membrane at the
initial site of infection, then migrates up the neurons by
retrograde axonal flow and becomes latent in the sensory
ganglion cell.
2) HSV-1 becomes latent in trigeminal ganglia
3) HSV-2 becomes latent in the lumbar and sacral ganglia.
4) During latency, most- if not all-viral DNA is located in
the cytoplasm rather than integrated into nuclear DNA.
5) The typical lesion is a vesicle and when vesicle rupture,
virus is librated and can be transmitted to other individual.
6) Multinucleated giant cells are typically found at the base
of herpevirus lesion.
7) Immunity is type specific and incomplete and both
reinfection and reactivation occur in the presence of
circulating IgG.
8) There is viremia in HSV-2 with no viremia in HSV-1.
Unit 4: Virology
211
Unit 4: Virology
211
Clinical findings:
HSV-1 cause the following diseases.
1) Gingivostomatitis (vesicles in the mouth) mainly in
children.
2) Herpes labialis
3) Keratoconjuctivitis.
4) Encephalitis.
5) Herpetic whitlow ( pustular lesion of the skin of the finger
or hanbds) senn in dentists and hospital peresonale.
6) Herpetic gladiatorum (vesicular lesion on the head, neck,
and trunk). Seen on wrestlers bodies.
7) Disseminated infection (oesophagitis and pneumonia).
HSV-2 causes the following:
1) genital herpes
2) Neonatal herpes
3) Aseptic meningitis.
Both HSV-1 and HSV-2 are associated with erythema
multiforme.
Laboratory diagnosis:
1) Isolation of the virus by cell culture
2) A rapid diagnosis from skin lesions can be made by using
the Tzanck smear, in which cells from the base of the
vesicle are stained with Giemsa stain. The presence of
MNG cells suggest herpesvirus infection.
3) Encephalitis diagnosed by PCR for HSV-1 DNA.
4) Serological test such as neutralization test can be used in
the diagnosis of primary infection because of significant
increase in Ab titer, but it is of no benefit in recurrence.
Treatment
1) Acyclovir is the treatment of choice for encephalitis and
systemic disease caused by HSV-1, and treatment of the
primary and recurrent genital herpes; it shortens the
duration of the lesion and reduces the extent of shedding.
2) Foscarnet in mutant strain of HSV-1
3) Trifluridine used in the treatment of eye infection
topically.
4) Penciclovir in the treatment of recurrent orolabial HSV-1.
5) Valacyclovir and famiciclovir in the treatment of genetal
herpes.
Note:
1) Drug is effective in preventing the recurrence after
primary infection.
2) Drugs have no effects on latent state.
Varicella- zoster virus (VZV) Disease
Varicella – chicken pox (primary disease)
Zoster - shingles is the recurrent form.
VZV has a single serotype
Immunity following varicella is lifelong but zoster can
ocurr despite immunity to varicella.
The virus is transmitted by respiratory droplets and by
direct contact with the lesion. Varicella is highly
contagious disease of childhood. It is a mild disease in
children and severe in adult.
VZV infects the mucosa of the URT then spread via the
blood to the skin. The virus infects sensory neurons and is
carried by retrograde axonal flow into the cells of the
dorsal root ganglia where the virus become latent.
Clinical findings:
Varicella:
Incubation period = 14-21 days.
A brief prodromal symptoms of fever, malaise occur
followed by papulovesicular rash in crops on the trunk
and spreads to the head and extremities. The rash evolves
from papules, vesicle pustules and finally crusts.
Zoster
The occurrence of painful vesicles along the course of a
sensory nerve of the head or trunk.
Laboratory diagnosis
It is mainly clinical.
Treatment
No antiviral therapy is required in immunocompetent
patient.
Therapy by acyclovir is indicated in immunocompetent
patient with moderate to severe infection and in
immunocompromised children and adults.
Prevention
There are two live attenuated VZV vaccine:
Varivax against varicella (recommended for children
between 1-12 years)
Zostavax against zoster but does not eradicate the latent
state of VZV (recommended for people older than 60
years and who have had varicella).
In immunocompromised patients prevention is by
acyclovir or Varicella zoster immunoglobulin (VZIG).
Unit 4: Virology
211
Cytomegalovirus (CMV)
Diseases:
Cytomegalic inclusion bodies in neonates. CMV is a very
important of pneumonia and other diseases in
immunocompromised patient. It also causes a heterophil
negative infectious mononucleosis like syndrome.
It has a single serotype.
Replicative cycle:
It is similar to that of HSV but in CMV, some of its
immediate early proteins are translated from mRNA
brought into the infected cell by parental virion rather
than being translated from mRNAs synthesized in the
newly infected cell.
Transmission
Early in life= transplacental, from birth canal, and in
breast milk.
In young children = mainly via saliva
Later in life = sexually; it is present in both semen and
cervical secretions. It can also transmitted by blood
transfusion, and organs transplantation.
About 80% of adults have antibody against the virus.
Pathogenesis
CMV causes cytomegalic inclusion diseases in infants
characterized by MNG cell with prominent intranuclear
inclusions. Many organs are affected. The infection is
acquired if the mother infected during pregnancy and
congenital abnormalities are more common if the
infection is acquired during the first trimester.
Infections of children and adults are usually asymptomatic
and the virus enter a latent state primarily in the
monocytes and can be reactivated when cell mediated
immunity is decreased.
Reactivation of CMV from the latent state in cervical cells
can result in infection of the new born during passage
through the birth canal.
How the virus escape the immune system?
1) In viral infected cell, assembly of the MHC class I viral
peptide complex is unstable, so viral antigens are not
displayed on the cell surface and killing by Tc does not
occur.
2) CMV encodes several microRNAs, one of which binds to
and prevents the translation of the cells mRNA for the
Class I- MHC proteins.
Clinical findings
1) About 20% of infants infected with CMV during gestation
show clinically apparent manifestations of cytomegalic
inclusion disease such as microcephaly, seizure, deafness,
jaundice, & purpura. Hepatosplenomegaly is very common
2) In immunocompetent adults, CMV causes heterophil
negative mononucleosis which is characterized by fever,
lethargy and the presence of abnormal lymphocytes in
peripheral blood smears.
3) In immunocompromised patients, it causes systemic
infection like pneumonitis and hepatitis.it is a common
cause of retinitis in AIDS patient which lead to blindness.
Laboratory diagnosis
1) Culture in shell vial culture coupled with the use of
immunoflourescent antibody which make Diagnosis
within 72 hours.
2) Fluorescent antibody and histologic staining of inclusion
bodies in giant cells in urine and tissue. The inclusion
bodies are intranuclear and have an oval owls-eye shape.
3) A fourfold increase in antibody titer
4) PCR for CMV DNA in tissue or body fluids (spinal or
amniotic).
5) CMV antigenaemia can be measured by detecting pp65
within blood leukocytes using an IF assay. Pp65 is a
protein located in the nucleocapsid of CMV.
Treatment
Ganciclovir is moderately effective in the treatment of
CMV retinitis and pneumonia in AIDS patient.
Valganciclovir is also used for retinitis
Foscarnet
Cidofovir is also useful in the treatment of retinitis.
Fomivirsen is an antisense DNA approved for intraocular
treatment of retinitis.
Prevention
There is no vaccine against CMV
Ganciclovir can suppress retinitis in AIDS patient.
Infants with Cytomegalic inclusion disease who are
shedding virus in their urine should be kept isolated from
other infants.
A high titer of immunoglobulin preparation is used to
prevent disseminated CMV infections in organ transplant
patients.
Unit 4: Virology
211
Epstein-Barr virus (EBV)
Diseases:
EBV causes infectious mononucleosis. It is associated
withy Burkitt's lymphoma, other B-cell lymphomas and
nasopharyngeal carcinoma.
EBV causes hairy leukoplakia.
Properties
Antigens of EBV
1) Viral capsid antigen (VCA) is mostly used in the
diagnosis.
2) Early antigen (EA) are produced prior to viral DNA
synthesis.
3) Nuclear antigen (EBNA)
4) Lymphocyte determined membrane antigen.
5) Viral membrane antigen.
Neutralizing activity is directed against the viral
membrane antigen.
EBV infects mainly lymphoid cells, primarily B-
lymphocytes. It also infects the epithelial cells of the
pharynx.
Transmission and epidemiology
It is transmitted primarily by saliva
Not transmitted by blood transfusion.
Infection in the first few years of life is asymptomatic.
The frequency of clinically apparent IM is highest in
those who are exposed to the virus later in life (e.g.,
college students).
Pathogenesis
The infection first occurs in nasopharynx and then spread
to blood, where it infects B lymphocytes. Cytotoxic T cell
react against the infected B cell. The T cells are the
"Atypical lymphocytes" seen in bloods. The virus
becomes latent within B- lymphocytes.
Immunity
1) First Antibody response is IgM against VCA followed by
IgG and persist for life.
2) Lifetime immunity against second episodes of IM is based
on antibody to the viral membrane antigen.
3) Nonspecific heterophil antibodies are also found.
Heterophil refers to antibodies that are detected by tests
using antigens different from the antigens that induced
them. The heterophil antibodies formed in infectious
mononucleosis agglutinate sheep or horse red blood cells
in laboratory.
Note that these antibodies don’t reacts with any
components of EB!. How?
The answer is that EBV likely modifies a cell membrane
constituent such that it becomes antigenic and induces the
heterophil antibody. These antibodies disappear 6 months
after recovery. These antibodies are not specific for EBV
infection and are also seen in individuals with hepatitis B
and serum sickness.
Clinical findings
Infectious mononucleosis is characterized primarily by
fever, sore throat, lymphadenopathy, and splenomegaly.
Anorexia and lethargy is prominent.
Hepatitis is frequent. Encephalitis could occur.
Spontaneous recovery usually occurs 2-3 weeks. Splenic
rupture is associated with sport activities such as football.
Laboratory diagnosis:
1) Haematologic approach absolute lymphocytosis occurs as
many as 30 % abnormal lymphocytes. These atypical
lymphocytes are enlarged with expanded nucleus and an
abundant often vacuolated cytoplasm. They are cytotoxic
T-cells that are reacting against the EBV-infected B-cell.
2) Immunologic
A. Monospot test for heterophil antibody test.
B. The EBV –specific antibody test are user primarily in
the diagnosis. (VCA,EA,and EBNA).
Treatments
No antiviral test is necessary for uncomplicated IM.
Acyclovir has little activity against EBV, but high doses
may be useful in life threatening EBV infections.
Prevention
There is no EBV vaccine.
Human herpesvirus-8 (Kaposi's sarcoma
associated Herpes virus)
The virus is transmitted sexually and also may be by
organ transplantation.
It causes kaposi's sarcoma by malignant transformation by
the mechanism of inactivation of tumor suppressor gene.
Poxviruses
It includes three viruses:
1) Small pox virus.
2) Vaccine virus.
3)
Mollescum contagiosum virus
.
