Unit 2: Bacteriology
126
Lecture 12+13 - Spirochetes
Spiral motile bacteria, includes 2 families:
1) Spirocheataceae: (free-living bacteria).
2) Treponemataceae include: Treponema, Borrelia &
Leptospira.
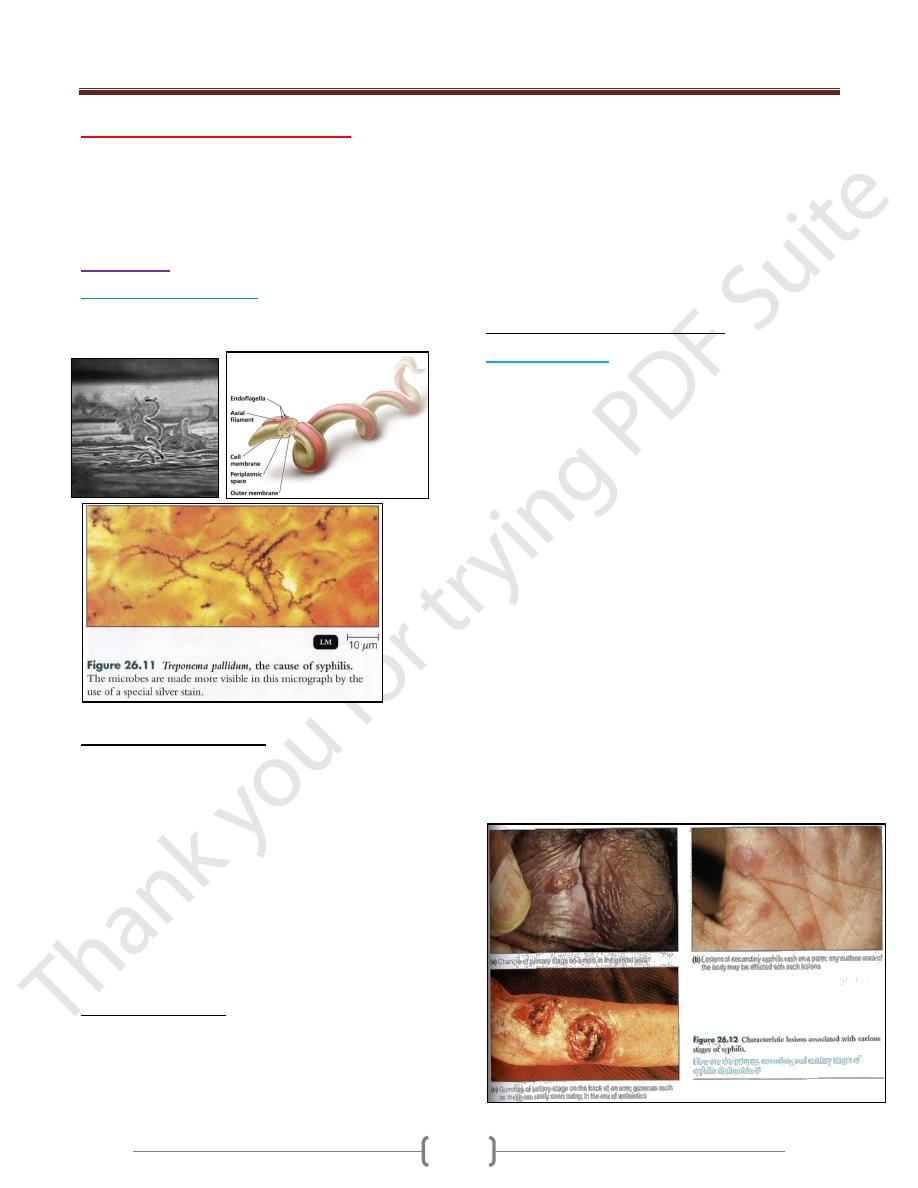
Treponema
T.pallidum subsp. Pallidum
causes syphilis, a long
{0.2X(5-15) mm}, slender, helically coiled, spiral, G-
bacilli
Structural characteristics:
1) Outer sheath (glucosaminoglycan coating).
2) Outer membrane (peptidoglycan).
3) Endoflagella (axial filaments, encapsed by the outer
membrane & wind around the organism).
4) Inner membrane (cytoplasmic membrane).
5) Cytoplasm contains body fibrils (cytoplasmic tubules).
Actively motile & so thin-→cannot be seen unless
immunofluorescin stain or dark-field microscope is
employed.
Never been cultured on artificial media or in fertile eggs
or in tissue culture.
Antigenic Structure:
1) Does not contain LPS.
2) The endoflagella: similar to bacterial flagellin protein.
3) Cardiolipin (an important treponemal antigens).
4) Hyaluronidase (breaks down the hyaluronic acid in tissue
& enhances the invasiveness of this organism, so it is
Virulence Factor).
Human with syphilis develops antibodies (can be used for
staining T.pallidum by direct IF test or complement
fixation test.
Also develops Ab-like substances or non-specific Abs.
called reagin, directed against some Ags. distributed in
normal tissues.
Pathogenesis & Clinical Findings:
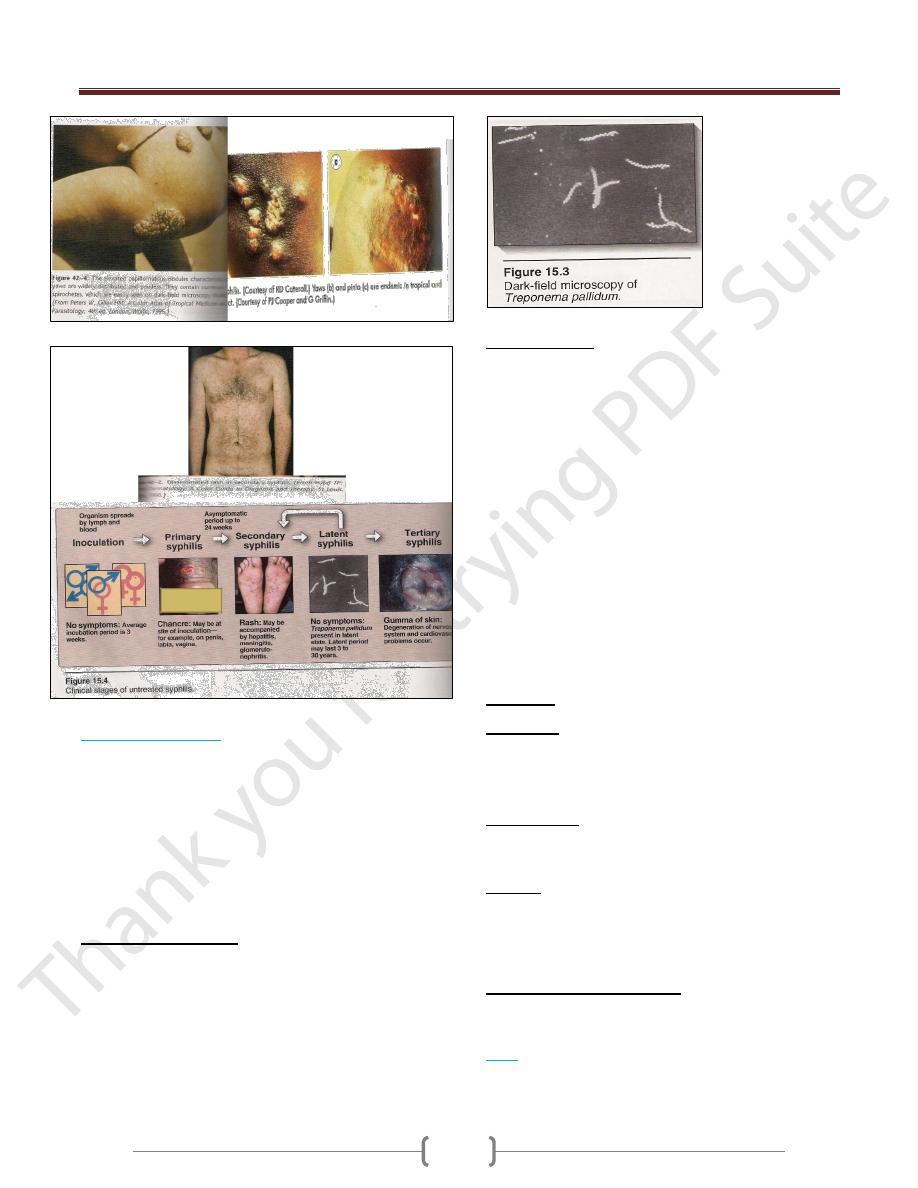
1) Acquired syphilis:
T.pallidum transmitted by sexual
contact (the infectious lesion is on the skin or mucous
membrane of genitalia & only 10-20% on intrarectal,
perianal & oral lesions).
• It is penetrate through mucous membrane or a break in the
epidermis, multiply locally-→ spread to lymph nodes-→
bloodstream.
• In 2-10 weeks after infection: primary syphilis or primary
lesion (a papule develops at the site of infection breaks
down to form an ulcer with clean, hard base called
hardchancre), heals spontaneously.
• 2-10 weeks later: secondary syphilis or secondary lesions
(a red maculopapular rash anywhere of the body) &
condylomas (a moist, pale papules in the anogenital
region, axilles & mouth). Also may be appear syphilitic
meningitis, chorioretinitis, hepatitis or periostitis → heals
spontaneously.
• Both primary & secondary lesions are rich in spirochetes
& highly infectious.
• 40% progresses to the tertiary stage (latent syphilis)-→
gummas (a granulomatous lesion in skin, bones, liver &
degenerative changes in CNS or cardiovascular lesions.
This lesion due to hypersensitivity to the organisms).
Unit 2: Bacteriology
127
2) Congenital syphilis:
Pregnant syphilitic women can transmit T.pallidum to the
fetus through the placenta in 10
th
-15
th
weeks of gestation.
Some infected fetus die, others are borne live with sings
of congenital syphilis in childhood (keratitis,
Hutchinson’s teeth, saddlenose, periostitis & variety of
CNS anomalies).
Treatment mother during pregnancy prevents congenital
syphilis.
Diagnostic Lab. Tests:
Specimens: Tissue fluids (lesions) & serum (serological
tests).
Dark-field examination: drop of tissue fluid examined
by dark-field microscope-→ motile spirochetes.
Immunofluorescence test: Tissue fluid stained with a
fluorescein-labeled antitreponemal serum examined by
fluorescent microscope-→ fluorescent spirochetes.
Serological tests:
1) Nontreponemal Ag tests: using cardiolipin (extracted from
normal mammalian tissue) + patient’sserum (reagin).
Reagin appears in serum after 2-3 weeks or in CSF after
4-8 weeks of infection. 2 types:
A. Complement fixation (CF) test or Wassermann-
Kolmer test: rarely used.
B. Flocculation test: VDRL (Venereal Disease Research
Lab.) or RPR (Rapid Plasma Reagin). Cardiolipin
form visible clumps with reagin containing sera.
2) Treponemal Ab tests: 2 types:
A. Fluorescent treponemal Ab-Absorbance (FTA-ABS) test:
Killed T.pallidum Reiter strain + patient’s serum +labeled
antihuman gamma globulin (very specific& sensitive test)
B. T.pallidum hemagglutination (TPHA) test:
-Red blood cells treated to adsorb treponemes on their
surface + patient’sserum-→ red cells clumped
Immunity: after cure-→ patient become susceptible.
Treatment:
Syphilis less than 1 year-→ benzathine penicillin (IM).
Older (latent syphilis) -→ = = (3 times weekly intervals).
Neurosyphilis-→ penicillin (large amount, IV).
Epidemiology:
Transmitted sexually.
An infected person may remain contagious for 3-5 years.
Control:
1) Treatment of all discovered cases.
2) Follow-up on sources of infection & contacts.
3) Safe sex.
Diseases Related to Syphilis
None are sexually transmitted diseases but by direct
contact. Diagnosis & therapy similar to syphilis.
1) Bejel
(T.pallidum subsp. endemicum)
→produces highly
infectious skin lesions. Penicillin the drug of choice.
Among children, in Africa, Middle East & Southeast Asia.
Unit 2: Bacteriology
128
2) Yaws
(T.pallidum subsp. pertenue)
→ Ulceration
papule usually on arms & legs-→ Scar formation of skin
lesions & bone destruction are common.
Among children, in humid, hot tropical countries.
3) Pinta
(T.carateum)
→ Lesions on skin, depigmentation
& hyperkeratosis take years afterward.
In all ages (dark-skinned races), in Mexico, American,
Pacific areas & Philippines.
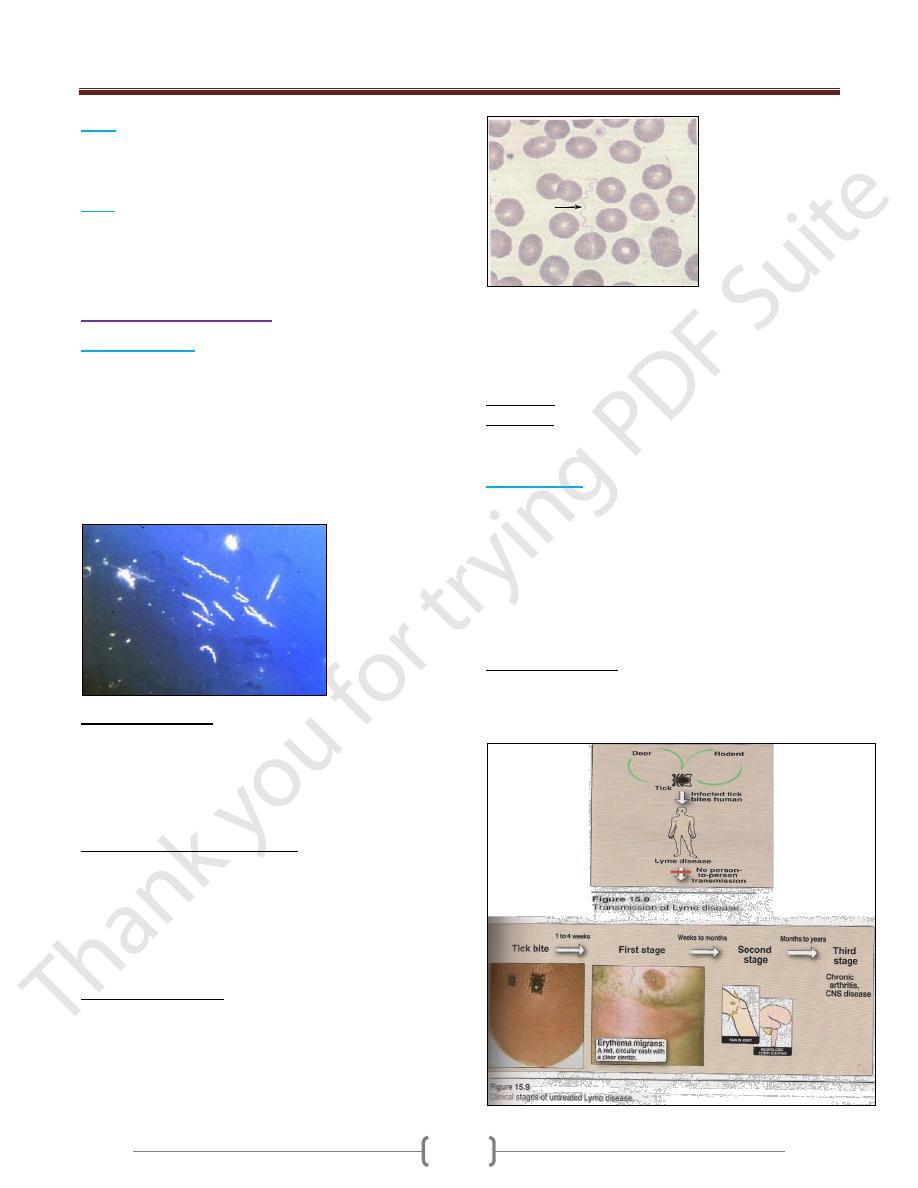
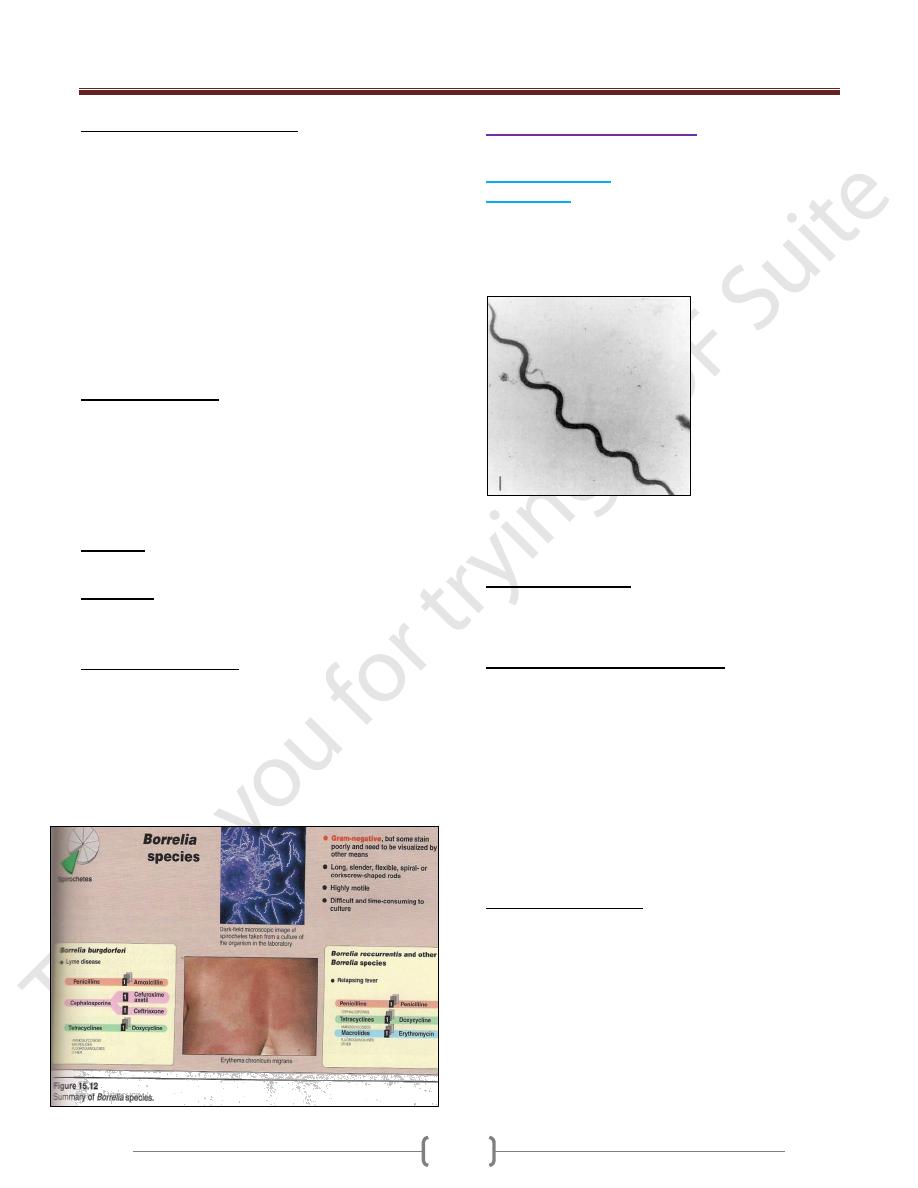
Borreliae (Borrelia SPP.)
1) Relapsing Fever
(Borrelia recurrentis)
transmitted by the human body
louse. Endemic relapsing fever in western USA
(B.hermsii)
transmitted by ticks (Orinthodoros hermsii).
Irregular spiral {0.3 X (10-30)μm}, flexible motile has
many endoflagella. Stained by bacteriological dyes &
blood stains (Giemsa’sor Wright’sstains).
Can be cultured in fluid media containing blood, serum or
tissue or in chick embryos.
Antigenic Structure:
Have antigenic variation-→ relapsing course due to the
multiplication of antigenic variants against which the host
must then develop new Abs. After 3-10 relapses-→
Ultimate recovery (associated with the presence of Abs
against antigenic variants).
Pathogenesis & Clinical Findings:
After incubation period (3-10 days), sudden chills & fever
(spirochetes found in blood). The fever persists for (3-5
days, febrile period). Then declines leaving the patient
weak but not ill (afebrile period), followed by a 2
nd
attack
of chills, fever,headache & malaise(3-10 such
recurrences)-→ recovery
Diagnostic Lab. Tests:
Specimens: Blood (during fever) for smear & animal
inoculation.
Smear: Thin or thick blood smear stained with Giemsa’s
or Wright’s→ Large, loosely coiled spirochetes among
the red cells.
Animal inoculation: White mice or rats inoculated (I.P),
after 2-4 days-→stained blood film for examined of
spirochetes.
Serology: + ve VDRL or CF tests.
Immunity: Short duration.
Treatment: Tetracycline or erythromycin & penicillin for
single day may be sufficient.
2)
Lyme Disease
(B.burgdorferi)
transmitted by tick
called Ixodes.
Spiral, highly motile, stained with acid & aniline dyes &
by silver impregnation techniques.
Isolated from erythema migrans skin lesions & ticks.
Grows in a complex medium (BSKII medium), seldom
used because it takes 6-8 weeks to grow & lacks
sensitivity with low diagnostic yield.
Antigenic Structure:
Have large No. of lipoproteins (Outer Surface Proteins;
Osp A-F) → help this organism live in the very different
tick & mammalian hosts.
Unit 2: Bacteriology
129
Pathogenesis & Clinical Findings:
Transmitted to human by injection of the organisms in
tick saliva, migrates (from the bite site) → skin lesions
called erythema migrans (a flat reddened area near the
tick bite slowly expands with central clearing, begins 3
days to 4 weeks after bite) →flu-like illness with fever,
chills, myalgia & headache (the initial stage) →
dissemination by lymphatics or blood to the other skin
area & organs (the second stage) occurs weeks to months
later (arthralgia & arithritis, meningitis, cardiac disease).
The third stage begins years later with chronic skin,
nervous system or joint involvement (the organism can be
isolated from all these sites).
Diagnostic Lab. Tests
Can be established clinically by observing the erythema
migrans, if not present→diagnostic lab.T.
Specimens: Blood (serological tests) & biopsy (smear). -
Serology: IFA, EIA or ELISA, Western blot.
Molecular probes: PCR (detection of B.burgdorferi
DNA in body fluids).
Immunity:
4-6 weeks after infection IgG to OspA & OspB.
Treatment:
Amoxicillin or doxycycline (20-30 days).
Arithritis: penicillin + probencide (30 days or longer).
Epidemiology & Control:
In USA, Europe & other areas.
Mice & deer (the main reservoirs), rodents & birds also
infected.
Prevention by avoidance ticks (using insecticides for
control)
OspA vaccine efficient 66-76 % for how lives or works in
endemic areas.
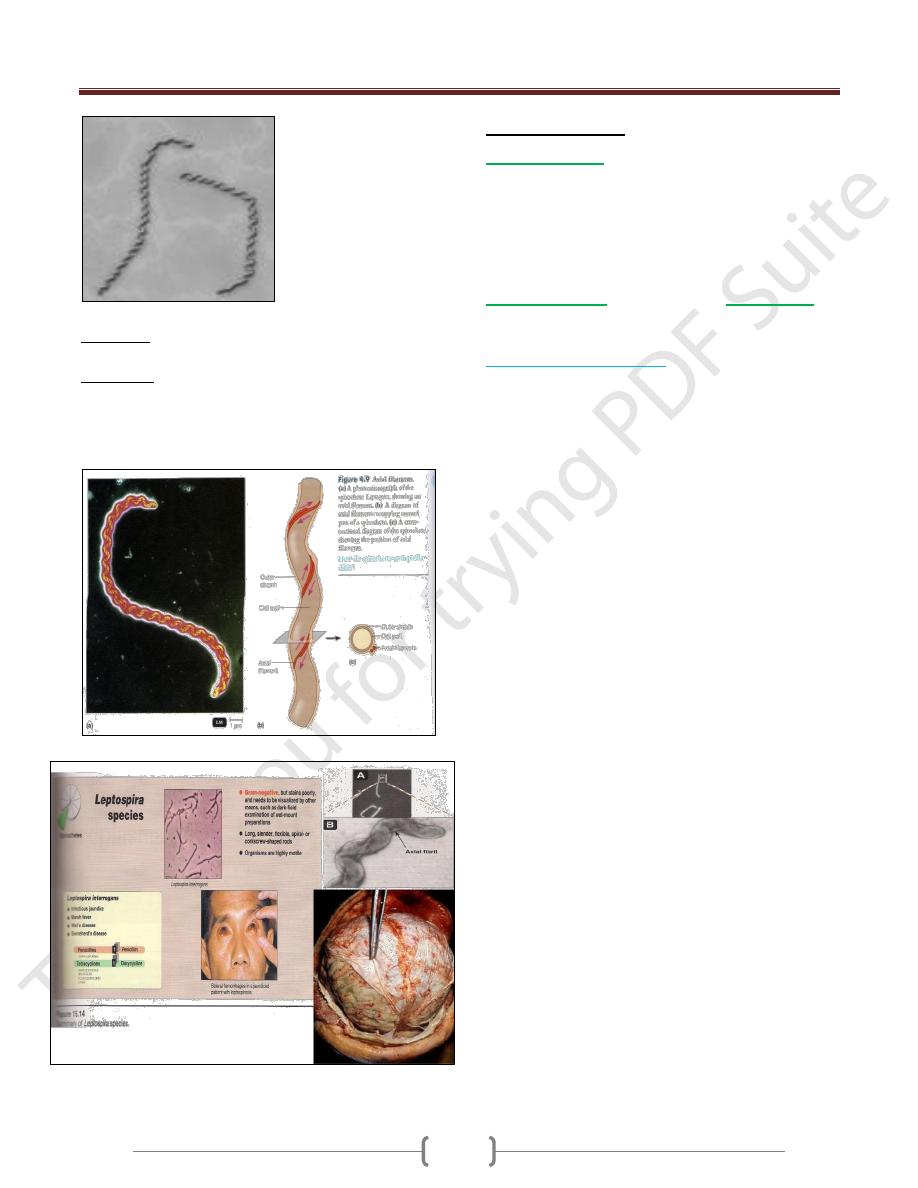
Leptospira & Leptospirosis
Leptospirosis includes 2 worldwide diseases:
1) Infectious jaundice
(L.interrogans serovar. canicola)
(dogs)
2) Weil’sdisease
(L.interrogans serovar.
icetrohaemorrhagia)(rats).
Tightly coiled, thin, flexible spirochetes {(0.1-0.2) X (5-15)
μm}, one end as a hook & actively motile. Does not stain,
seen by dark-field microscope as a chain of minute cocci.
Grow aerobically at 28-30Cº in serum containing media
(Fletcher’sor Stuart’smedia)-→ diffuse zone of growth.
Antigenic Structure:
Have LPS variable from one strain to another (used for
classification & determines the immune response).
Pathogenesis & Clinical Findings:
Infection results by ingestion of water or food
contaminated with leptospirae from urine of dog, rats,
mice, cattle, swine & others (rare through mucous
membranes or breaks in the skin). After incubation period
(1-2weeks), variable febrile onset, flu-like illness
(spirochetes in blood) → establish in parenchymatous
organs (liver & kidneys) → hemorrhage & necrosis of
tissues & dysfunction of organs (initial phase) →second
phase, when IgM titer rises, aseptic meningitis, nephritis,
hepatitis & may be skin, muscle & eye lesions.
Diagnostic Lab. Tests:
Specimens: Blood, CSF, urine & tissues.
Smear: Dark-field microscope or fluorescein-conjugated
Abs or immunohistochemical techniques.
Culture: Fletcher’ssemisolid medium (8weeks). -Animal
inoculation: hamsters or guinea pigs.
Serology: microscopic slide agglutination test.
Unit 2: Bacteriology
130
Immunity: serovar specific immunity but reinfection
with different serovar may occur.
Treatment:
Mild disease: doxycycline, ampicillin or amoxicillin
(orally)
Sever = : penicillin or ampicillin (I.V).
Other Spirochetes
Spirillum minor
-→ rat-bite fever (Sodoku disease).
Very small spirochetes (3-5 μm) & rigid spiral.
Infection through the bite of rat-→ local lesion, regional
glands swellings skin rash & fever (relapsing type). Can
be isolated from enlarged lymph nodes material or blood-
→ inoculated to mice or guinea pigs.
Borrelia bucallis
in normal mouth &
B.refringens
in
normal genitalia.
Fusospirochetal Diseases:
The normal spirochetes with anaerobic fusiform bacilli
(fusobacteria), not primary pathogens but after other
infection (HSV), mucous membrane injury or nutritional
deficiency-→ disease:
1) Ulcerative gingivostomatitis (trench mouth, poor oral
hygiene).
2) Vincent’s stomatitis (Vincent’s angina) → ulcerative
tonsillitis & massive tissue involvement.
3) Leg (tropical) ulcers (similar to V. angina).
