Unit 2: Bacteriology
112
Lecture 5 - Vibrios (vibrio spp.) &
associated bacteria
Found in marine & surface water, curved aerobic rods &
motile with polar flagellum. The medically important
vibrios are:
Vibrio spp.
1. Vibrio cholerae
Causes cholera (profuse watery diarrhea that can lead to
death)
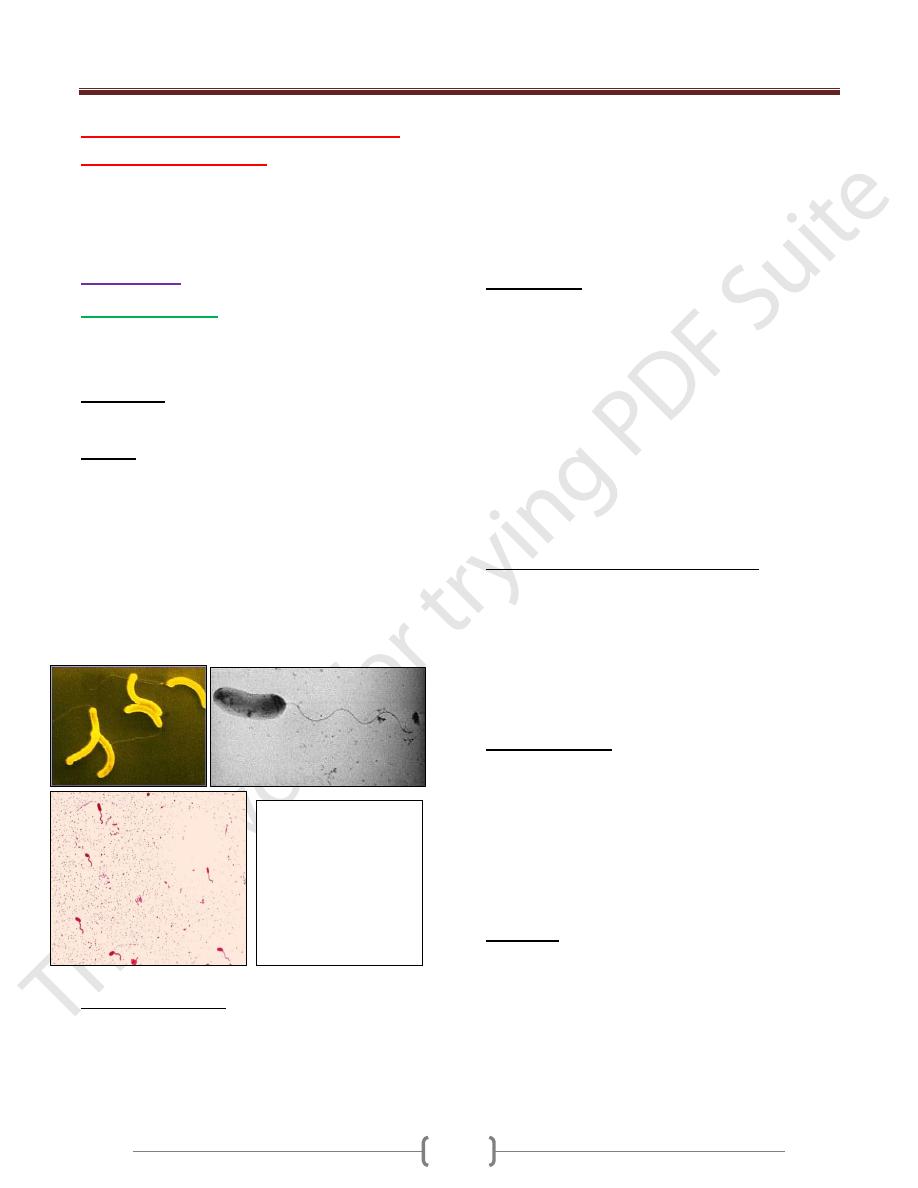
Morphology:
Comma-shaped, curved rod, motile with polar flagellum.
Culture:
Convex, smooth, round colonies, grows at 37C˚ on many
kinds of media. On TCBS (Thiosulfate-Citrate-Bile-
Sucrose) agar→Yellow colonies, Oxidase +, grow at very
high pH (8.5-9.5).
Some vibrios are halophilic (requiring NaCl to grow).
Others are halotolerant (NaCl stimulate their growth).
Vibrios grow on media containing 6% NaCl & susceptible
to compound O/129 (2,4-diamino-6,7-diisopropyl
pteridine phosphate).
Antigenic Structure:
1) H (flagellar) Ag.
2) O Ag of LPS (139 O Ag groups).
V.cholerae strains O group 1& O group 139 causes classic
(epidemic & pandemic) cholera.
Serogroup O1 Ag (including Ogawa & Inaba serotypes).
Non O1/non O139 V.cholerae causes cholera like-disease
(mild diarrhea), rarely extraintestinal infections.
For epidemiological studies, 2 biotypes of epidemic
V.cholerae Classic & ElTor (ElTor biotype cause mild
diarrhea than Classic biotype).
3) Capsule (polysaccharide) Ag: in O139 & non O1
V.cholerae (serogroup O1 dose not).
Pathogenesis:
V.cholerae is pathogenic only for humans.
Ingest as many as 10
10
or more organisms (vehicle is water)
or 10
2
-10
4
(vehicle is food) → infection.
Any medication or condition that decreases stomach acidity
makes a person more susceptible to infection with
V.cholerae.
Cholera is not an invasive infection (the organisms do not
reach the bloodstream but remain within the intestinal
tract).
Virulent V.cholerae attach to the microvilli of the brush
border of epithelial cells, multiply & liberate cholera toxin
& mucinases & endotoxin.
V.cholerae enterotoxin (cholera toxin):
a heat-labile, consist of subunits A & B.Ganglioside G
mI
the
receptor for subunit B, which promotes entry of subunit A
into the cell.Activation of subunit A yields increased levels
of cAMP → hypersecretion of water & electrolytes
(increased sodium chloride secretion & inhibit absorption
of sodium & chloride) →diarrhea (20-30 L/day) →
dehydration, shock, acidosis & death.
Clinical Findings:
The incubation period is 1-4 days (depending upon the size
of the inoculum ingested) →sudden onset of nausea,
vomiting and profuse diarrhea with abdominal cramps.
Stool resembles “ rice water” contain mucus, epithelial cells
& large No. of vibrios.
Rapid loss of fluids & electrolytes→dehydration,
circulatory collapse & anuria.If without treatment, 25-50%
mortality.
Diagnosis:
Specimens: mucus flecks from stools (for culture).
Smear: Dark-field or phase contrast microscopy show
rapidly motile vibrios.
Culture: Peptone agar, blood agar (pH 9) or TCBS agar.
Specific Tests: biochemical tests & slide agglutination
(using anti-O group O1 & O139 antiserum).
Vibrio cholerae has a
single polar
flagellum for
swimming
movement. Electron
Micrograph of Vibrio
cholerae
Unit 2: Bacteriology
113
Immunity:
Duration & degree of immunity are not known. Specific
IgA occur in lumen of the intestine.
Gastric acid provides some protection against vibrios.
Treatment:
Water & electrolytes replacement (to correct the sever
dehydration) & oral tetracycline (V.cholerae tetracycline
resistance by transmissible plasmids).
Epidemiology; Prevention & Control:
Africa (millions of people), rare in North America. Cholera
is endemic in India & Southeast Asia. It is carried along
shipping lanes, trade routes & migration routes.
Cholera is spread by person-person contact, water, food &
flies. True chronic carrier is rare (after 3-4 weeks).
Control rests on education & sanitation of food & water.
Patients should be isolated, and their excreta disinfected &
contacts followed up.
Chemoprophylaxis with antimicrobial drugs.
The WHO vaccination for cholera for 6 months only.
Repeated injection of a vaccine containing either LPSs
extracted from vibrios or dense vibrios suspensions (limited
protection).
2. Vibrio parahaemolyticus:
Causes gastroenteritis
Halophilic (required NaCl for growth), grows on blood agar
& TCBS agar (green colonies), oxidase +.
Causes acute gastroenteritis, following ingestion of
contaminated seafood (raw fish or shellfish). After
incubation period (12-24 hrs), nausea, vomiting &
abdominal cramps, fecal leukocytes are observed. Subside
spontaneously in 1-4 days with no treatment.
3. Vibrio vulnificus:
Causes severe wound infections (in immunocompromised
persons), bacteremia (in alcoholism & liver diseases) &
gastroenteritis (oysters, in warm months).
Wound infections may be mild but proceed rapidly (a few
hrs) with development of bullous skin lesions, cellulitis &
myositis with necrosis.
Diagnosis by TCBS agar (green colonies).
Treatment: tetracycline, ciprofloxacin.
Other Vibrios:
V.mimicus
causes diarrhea (uncooked seafood).
V.hollisae
&
V.fluvialis
causes diarrhea.
V.alginolyticus
causes eye, ear, or wound infection after
exposure to seawater.
V.damsela
causes wound infection.
Aeromonads (aeromonas spp.)
3 spp. Are clinical importance:
Aeromonas hydrophila,
A.caviae & A.veronii biovar sorbria.
(Diarrhea).
Rods, motile, their colony morphology is similar to enteric
G – rods but it is oxidase + .Differentiated from vibrios by
resistance to compound O/129 & lack of growth on media
containing 6% NaCl.
Produce hemolysins (large zone of hemolysis on blood
agar) & enterotoxin (some strains), cytotoxin & invade cells
in tissue culture (but non of these characteristics have been
clearly associated with diarrheal disease in humans).
Susceptible to tetracycline, aminoglycosides &
cephalosporines.
Plesiomonas
Exists in both cold- & warm-blooded animals (isolated
from freshwater fish & many animals), cause diarrhea in
tropical & subtropical areas.
P. shigelloides
is a G – rod with polar flagella, isolated
from stool culture of human with diarrhea.
Plesiomonas grows on the same media for Salmonella &
Shigella (but oxidase +). Some strains cross-react with
Shigella antisera.
P. are DNase +, can distinguish it from Aeromonas by
other biochemical tests.
