Unit 8: Anti-inflammatory Drugs and Autacoids
832
Lecture 1+2 - Anti-
inflammatory Drugs
Prostaglandins
Non-steroidal anti-inflammatory drugs
(NSAIDs)
Inflammation is due to the release of chemical mediators
from injured tissues and migrating cells. The specific
mediators vary with the type of inflammation. They
include:
Histamine, 5HT, PG
s
, bradykinin and IL-1. NSAID
s
are
group of chemically dissimilar agents, they differ in the
following activities antipyretic effect, analgesic effect in
the following activities antipyretic effect, analgesic effect
and anti-inflammatory effect.
Classification according to their therapeutic
uses:
1. Drugs with analgesic activity and weak
antiinflammatory action.
Para-aminophenol:
* Acetaminophen (paracetamol)
* Phenacetin * Glafenin (Glifenan)
2. Drugs with analgesic activity and mild to
moderate antiinflammatory action.
a) Propionic acid derivatives
* Ibuprofen (brufen) * Ketoprofen
* Fenoprofen * Naproxen
b) Fenamic acid derivatives
* Mefenamic acid (ponstan) * Flufenamic acid
3. Drugs with analgesic activity and strong
antiinflammatory actions.
a) Salicylic acid derivatives
* Aspirin (Acetylsalicylic acid) * Benorylate
* Diflunisal * Methylsalicylate
b) Acetic acid derivatives
* Diclofenac (voltaren) * Indomthacine (Indocid)
* Tolmetin * Etodolac * Sulindac
c) Enolic acid derivatives.
* piroxicam (feldene) * Tenoxicam
* Azapropazone * Phenylbutazone
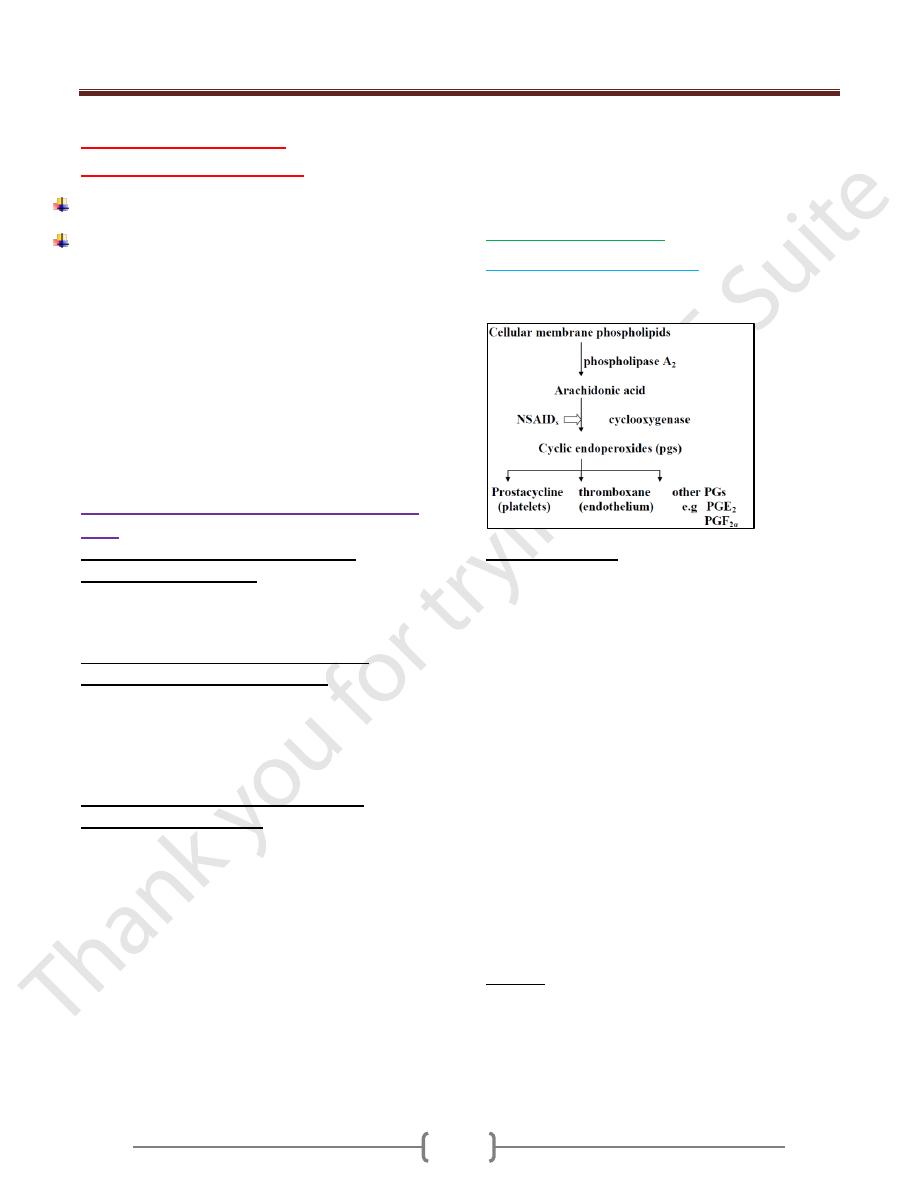
NSAID
s
act by inhibiting the enzyme cyclo-oxygenase
(COX), the prototype of this group is aspirin, to which all
other anti-inflammatory agents are compared with aspirin.
Some of the newer NSAID
s
are better than aspirin in
certain patients because of less gastric irritation but these
drugs still more expensive than aspirin and some are more
expensive.
Salicylic acid derivatives:
Aspirin and other salicylate:
The figure represents the acetylation of cyclooxygenase
by aspirin.
Pharmacokinetics:
Well absorbed from stomach and upper part of the small
intestine yielding a peak plasma concentration 1-2 hrs.
At the acid gastric pH keeps large fraction of salicylate in
non-ionized form (lipid soluble) so it diffuses easily and
absorption is promoted.
When high conc. of salicylates enter the muocosal cells,
the drug may damage the mucosal barrier and result in
gastric ulcer. If gastric PH is raised by suitable buffer to
3.5 or higher gastric irritation will be minimized (less
absorption but less irritation).
Aspirin in tissues is hydrolyzed to acetic acid +salicylate.
Alkalization of urine increases the rate of excretion of free
salicylate.
If it is desired to get salicylate out of the body quickly an
alkaline diuresis will be useful.
When aspirin is used in low doses up to 600 mg/daily (t½
is 3-5hrs) elimination is first order kinetic.
With higher doses nearly 4g/daily (t½ 15hrs or more)
elimination is zero-order kinetic.
Actions:
Anti-inflammatory, analgesic (mild to moderate intensity
but not severe pain), antipyretic effects (is relate to
dissipation of heat caused by vasodilation of the
superficial blood vessels). It has no any sedative,
tolerance or dependence effects.
Unit 8: Anti-inflammatory Drugs and Autacoids
832
Cellular metabolism increases when the plasma salicylate
concentration increases, so it will increase the heat
production.
Hypoglycemia.
Inhibition of platelets aggregation so aspirin is used in
transient ischemic attacks and unstable angina.
Respiratory effect. Causing hyperventilation and
respiratory alkalosis
Acid-base and electrolyte balance (increase water loss
in urine)
.
CVS: Large doses induce vasodilatation, fall in B.P.
G.I.T: Irritates gastric mucosa, produce focal necrosis,
increased blood loss(4ml/day).
Enteric coated aspirin tablets are less G.I.T problem.
Urate excretion: at higher doses (5-8gm/day). The effect
is greater and more in an alkaline urine. Low doses of
aspirin less than 2gm/day-cause urate retention.
Clinical uses of aspirin:
1. Analgesic, anti-inflammatory and antipyretic.
2. Inhibition of platelet aggregation.
3. External application for Corns and wart.
Adverse effects:
1) GIT:
Heart burn, vomiting, fecal blood loss and gastritis is due
to undissolved tablets, stomach absorption of non-ionized
salicylate and inhibition of protective PG
s
(I
2
and E
2
).
2) CNS:
higher doses cause salicylism: hearing difficulty,
dizziness, headache and confusion.
large doses cause hyperapnea by direct effect on medulla.
toxic doses causes respiratory alkalosis which cause
increased ventilation then acidosis due to accumulation of
salicylic acid derivatives and then depression of
respiratory centre.
3) Other side effects:
Allergy more susceptible
Reyes syndrome: Aspirin gives during viral infection
increased incidence of Reyes syndrome (fatal hepatitis
with cerebral oedema) in children.
Treatment of acute salicylate poisoning:
Gastric lavage, or therapeutic emesis with syrup
Ipecacuanha.
Correction of dehydration due to sweating, vomiting and
over breathing (dextrose 5%).
Na-bicarbonate is used to correct metabolic acidosis
(blood pH<7.2) and to alkalinize the urine to remove
salicylate.
Removal of salicylate from the body by activated charcoal.
Haemodialysis can be used especially when there is renal
failure.
Drug interaction:
Drug enhance Salicylate intoxication include
Acetazolamide and ammonium chloride.
Alcohol increases G.I.T bleeding produced by salicylate.
Aspirin displaces number of drugs from protein binding
sites include: Tolbutamide, Chloropropamide,
Methotrexate and Probencid.
Corticosteroides may decrease Salicylate concentration.
Aspirin reduces pharmacological activity of some drug
e.g Spironolactone.
Antagonise heparin.
Competes with pencillin G for renal tubular secretion.
Other Salicylic acid derivatives:
2) Diflunisal:
similar to aspirin with analgesic and anti-
inflammatory action. It may cause less gastric adverse
effect. The diarrhea is more common. It causes cross
allergy with aspirin.
3) Benorylate:
Is an ester of aspirin and paracetamol which
is non-ionic and so lipid soluble.
-Is well absorbed from G.I.T. It is less irritant to stomach.
-Causes less blood loss than dose Aspirin.
4) Methyl salicylate
: is too irritant to be used internally. It is
used as counter irritant as liniments.
5) Salicylic acid
: Topical use for wart and corn removal.
Para-aminophenol:
Paracetamol (acetaminophen):
This agent unlike NSAID
s
has little or no anti-
inflammatory activity.
Used as analgesic and antipyretic agent instead of aspirin
in patients with gastric problems and with problems
arising from prolonging bleeding clot time and also used
in patients don’t require anti-inflammatory effects.
Its efficacy about equivalent to that of aspirin. It is
effective in mild to moderate pain such as of headache or
dysmenorrhea.
Kinetics:
It is rapidly absorbed from alimentary canal
with significant first pass elimination. It is inactivated in
liver by conjugation as glucuronide and sulphate.
Minor metabolites are formed. One of this metabolite is
called N-acetyl-p-benzoquinoneminie. Is highly reactive
chemically and dangerous metabolite.
At normal doses this substance reacts with (-SH) group of
Glutathione in the body forming a non-toxic substance
Unit 8: Anti-inflammatory Drugs and Autacoids
842
With large doses: the metabolite product will react with
hepatic proteins forming covalent bounds, so hepatic
necrosis will result, also renal tubular necrosis can occur.
Side effects:
Nearly without S.E at normal therapeutic doses. skin rash
and minor allergic reaction occur rarely.
But heavy long-term daily use may predispose to
hepatotoxicity (damage to the liver), urticaria, hemolytic
anemia, hypoglycemia, jaundice(yellow discoloration of
the skin), and hepatic failure (seen in chronic alcoholics
taking the drug).
Acute paracetamol poisoning (over dose).
Sever
hepatic and renal damage can occur after a single 10-
15gm dose of paracetamol. Dosages of 20 to 25gm may
be fatal. With excessive dosage the liver cells will cause
necrosis or die. Death can occur due to liver failure. The
risk of liver failure increases in patients who are chronic
alcoholics.
Antidote for paracetamol poisoning:
Glutathione itself cannot be used as it is, because it
penetrates to the cells poorly: N-acetylcystein (NAC) and
Methionine are effective. These two agents are the
precursors for the synthesis of Glutathione.
Propionic acids:
Ibuprofen (Brufen):
It can be regarded as a typical of the group.
It is well absorbed after an oral dose to give maximum
plasma concentration in one hour. Other of this group
include: ketoprofen, fenoprofen and naproxen.
They all have similar properties and are most useful in
painful conditions not accompanied by prominent
inflammation. Painful conditions such as mild rheumatoid
disease and musculoskeletal disorders.
Their main advantage over aspirin is a low incidence of
adverse effects particularly in G.I.T.
Side effects:
Nausea, vomiting, diarrhea, constipation, gastric or
duodenal ulcer bleeding (but less sever and less frequent
than of aspirin), headache, dizziness, fever and rash.
Fenamic acids
Mefenamic acids (Ponstan)
Is slowly absorbed from the small intestine and is
eliminated mainly as metabolites in the urine and faeces.
It is used for mild to moderate pain where inflammation
is not marked e.g: muscular dental and traumatic pain and
headache, and also for dysmenorrhoea and menorrhagia
due to uterine dysfunction.
The principal side effects: Diarrhoea, upper abdominal
discomfort, peptic ulcer and haemolytic anaemia. Elderly
patients who take mefenamic acid may develop
nonoliguric renal failure especially if they become
dehydrated e.g. by diarrhoea; the drug should be avoided
or used with close supervision in the elderly.
Acetic acids
Diclofenac (Voltarin)
is used for moderate pain and
inflammation due to rheumatoid disease, musculoskeltal
disorders, renal colic and postoperative pain.
The principal side effects: CNS (headache, dizziness,
insomnia and fatigue), GI (nausea, GI pain, and diarrhea)
and others (rash and peripheral edema).
Indomethacin (indocid)
is highly effective anti-
inflammatory, analgesic and antipyretic agent. Absorption
from the gut is rapid and almost complete. It is used to
relieve moderate to severe pain and inflammation of
rheumatoid disease and gout.
Side effects of indomethacin include gastric irritation
with ulcer formation, bleeding and perforation. it reduces
the effectiveness of diuretic drugs. Headache is common,
vomiting, dizziness and ataxia occur. Allergic reactions
occur and there is cross-reactivity with aspirin.
Enolic acids
Piroxicam (Feldene)
Is completely absorbed from the gastrointestinal tract. It is
with long half-life. It is used as one dose daily.
Uses: Rheumatoid disease, musculoskeletal disordes and
gout.
Side effects are those to be expected with NSAID
s
. CNS
and GI are the commonest.
Topical use of NSAID
s
Salicylates, diclofenac, piroxicam, ketoprofen and
ibuprofen
are available as gels and cream for topical use
on the skin for relief of symptoms caused by soft tissue
trauma. The objective is to produce therapeutic local
concentration without (undesirable) systemic effects.
They have less therapeutic efficacy.
Unit 8: Anti-inflammatory Drugs and Autacoids
842
Rheumatoid arthritis (RA)
Is the most common form of chronic inflammatory
destructive disease of the joint.
Drug therapy for this disease:
1.
Simple analgesics
To relieve pain but without appreciable anti-inflammatory
action. These include peripherally acting agents such as
paracetamol
and centrally acting such as
dihydrocodine
and
dextropropoxyphene.
2.
NSAID
s
Are very effective in relieving pain and stiffness, but they
don’t alter the course of the disease. The major action is
inhibition of cyclooxygenase and thus inhibition of the
production of prostaglandins and thromboxane.
There are two forms of cyclooxygenase (cox): cox
1
and
cox.
2.
Cox
1
: is an enzyme expressed in most tissues
including: blood platelets, kidney, stomach and in tissue
homeostasis.Cox
2
: is induced in inflammatory cells.
Most NSAID
s
in current use are inhibitors of both
isoenzymes. They vary in the degree of inhibition of each.
Clearly the anti-inflammatory action of NSAID
s
is mainly
related to their inhibition of cox
2
.
New compounds with a selective action on cox
2
:
Meloxicam (Mobic)
Rofecoxib (Dioxx)
3. SAARD
s
(slow acting anti-rheumatic drugs) or
called (2
nd
line treatment for RA).
These agents don’t involve inhibition of cyclooxygenase
enzyme or possess immediate anti-inflammatory effects,
but will improve joint pain, stiffens and swelling.
These agents slow the course of the disease (i.e. retard
structural damage to the joints.
Their onset of action may take 3-4 months: Drugs as
a) Gold salts:
They can’t repair the existing damage, but prevent further
injury or joint destruction as
Sodium aurothiomalate
I.M
Auranofin
as tab
These are effective but their side effects are too high in
addition they are expensive.
The plane of therapy is to gradually build up the amount
of gold in the body to an effective concentration. The gold
salts are concentrated in collagen and synovial membrane
to prevent joint destruction.
Side effects: mostly with parenteral administration of the
drug. Dermatitis, mouth ulcers, enterocolitis, proteinuria,
nephrotic syndrome, thromocytopenia, agranulocytosis
and a plastic anemia. Oral gold therapy has less S.E but
with severe diarrhea.
b)
Pencillamine
It is produced by hydrolysis of penicillin. It is used in-
patients with active progressive disease (development of
deformities or radiological bone changes).
Mechanism of action: Is thought to modify rheumatoid
disease partly by decreasing interleukin-1 generation and
or parrtly by an effect on collagen synthesis, preventing
maturation of newly synthesized collagen.
Side effects: Anoraxia, nausea and vomiting, losse of
taste, proteinuria, thrombocytopenia and rarely
myasthenia gravis. Pencillamine is a metal chelator and so
should not be given with gold compounds.
c)
Captopril
(an angiotensine converting enzyme
inhibitor). Has structurally similar to pencillamine and is
evaluated in rheumatoid disease.
d) Antimalarial agent
(Chloroquine).
It is an effective drug and 65% of patients may improve
and their effect will be seen in 3-6 months. The drug
should be discontinued if there is no effect within 6
months.
On long term use, it accumulates in many organs
including the eye, which may cause retinal damage, so the
patients should have an ophthalmic examination before
and after treatment.
Side effects: Nausea, diarrhea, rashes, hemolytic anemia,
ototoxicity and neuromyopathy. Its major side effect the
retinopathy, which may produce blindness.
e)
Sulphasalazine (salazopyrine).
Is a first choice in rheumatoid disease, produces remission
in active rheumatoid arthritis. It is also used for chronic
inflammatory bowel disease.
Side effects: Gastrointestinal disturbance, Malaise,
headache, megaloblastic anemia and rashes.
f) Immunosuppressive drugs
.
Include
Methotrexate, Azothioprine, Cyclosporin
and
cyclophosphamide.
These are selectively suppressing immune response. They
have an effect on preventing progression RA.
g)
Levamisol
Is RA. used as an antihelmenthic agent. It has been found
to be benefit in
Unit 8: Anti-inflammatory Drugs and Autacoids
848
Gout and drugs
Gout is characterized by a recurrent episode of acute
arthritis due to deposition of urate in joints (bones and
cartilage) and in the kidney.
Urate deposit may form renal calculus or cause other
damage. Urate deposits produces periodic episodes of
severe pain. Gout is associated with hyperuricemia with
poorly soluble substances.
Hyperuricemia and gout from whatever cause (e.g
metabolic, renal disease, neoplasia) depend on 2
processes.
1) Overproduction of urate due to excessive cells
destruction.
2) Underexcretion of urate. Is caused by all diuretics (except
spironolactone), aspirin in low doses, ethambutol,
pyrazinamide, nicotinic acid and alcohol (which increases
urate synthesis and also causes a rise in blood lactic acid
that inhibits tubular secretion of urate.
Drug management: aims are to
Suppress the symptoms (by anti-inflammatory drugs) as
by indomethacine, dichlofenac, naproxen, piroxicam,
colchicine and adrenal steroids.
Prevent urate synthesis (allopurinol).
Promote the elimination of urate by uricosuric drugs as
probencid and sulphinpyrazone.
Colchicine
Is an anti-inflammatory drug used to prevent or treat acute
attacks of gout. In acute attacks, it is the drug of choice
for relieving joint pain and edema. It decreases
inflammation by decreasing the movement of leukocytes
into body tissues containing urate crystals (is an
antimitotic). It has no analgesic or antipyretic effects. It
can relief pain and inflammation by inhibiting the cell
migration to the inflamed area without altering the
metabolism and excretion of urate.
Adverse effects may be sever with abdominal pain,
vomiting, diarrhea which may be bloody. Renal damage
can occur on large doses cause muscular paralysis.
Allopurinol
It decreases the uric acid synthesis by inhibiting the
xanthine oxidase (the enzyme which converts xanthine
and hypoxanthine to uric acid. Allopurinol is metabolized
in the liver to alloxanthine which itself also an inhibitor to
xanthine oxidase and has a long duration of action.
Allopurinol is given once daily.
Indication: Chronic gout, renal stones.
Adverse effects: G.I.T disturbance, nausea, vomiting,
diarrhea, hepatic toxicity, skin rash, arthralgia, fever and
cataract.
Drug interactions:
Potentiation of mercaptopurine (because allopurinol
inhibits the metabolism of mercaptopurine to an
inactive form).
Inhibits the metabolism of probencid and oral
anticoagulants.
Uricosuric agents (include
probenecid
and
sulphinpyrazone)
They are used to decrease body level of urate that means
the reabsorption of uric acid in PCT is decreased and thus
urate excretion is increased in urine. Aspirin in small
doses causes retention of uric acid. So it should not be
used as analgesia for patients with gout. Aspirin can block
the uricosuric effects of probencid and sulphinpyrazone.
Migraine
Is due to variety of factors. Including:
Stress (exertion, excitement, anxiety, fatigue, anger).
Food containing vasoactive amines (chocolate,
cheese).
Food allergy.
Hormonal changes (due to menstruation cycles or
administration of oral contraceptive).
Hypoglycemia.
Classic migraine starts with aura 30mins consists of visual
or sensory disturbances.
These precipitants may initiate release of vasoactive
substances stored in nerve ending and blood platelets.
Vasoactive substances such as histamine, prostaglandin’s
and neuropetides are involved in pain.
Drugs in migraine
Ergotamine
Is a partial agonist acts on α-adrenoceptors
(vasoconstrictor) and also a partial agonist at serotonergic
receptors, due to their partial agonist activity, it will
constrict all peripheral arteries and veins.
Caffeine enhances absorption of ergotamine (both the
speed and peak plasma concentration).
Unit 8: Anti-inflammatory Drugs and Autacoids
843
Sumatriptan
It is selectively stimulates a subtype of serotonin receptors
(5HT like receptor), which are found in cranil blood
vessels causing them to constrict.
Treatment of migraine in general
Acute attack treatment:
Partial agonist at serotonergic receptors and α-
adrenoceptor agonist
(Ergotamine).
Stimulates 5HT
1
like receptor
(sumatriptan).
Inhibition of PG synthesis
(NSAID
s
)
Antiemetic (and/or) activators of Gastric motion
(metoclopramide, prochloperazine, cyclizine).
Sedative
(benzodiazepines compounds)
especially if
attack is triggered by stress.
Corticosteroids (for status migraine i.e. Prolonged
headache for days). By
methyl prednesiolone.
Prophylactic treatment.
NSAID
s
.
β-adrenoceptor block by
propranolol
, other pure
antagonist
atenolol.
Calcium channel blockers (
Verapamil, Nifidepine
)
may provide benefit.
Pizotifen
and
cyproheptadine
block serotonin
receptors as well as having some H
1
-antihistamine
action they can be effective.
Tricyclic antidepressant e.g
amitriptyline
in low dose.
Methysergide
(ergot derivative) blocks serotonin
receptor.
