Unit 7: Chemotherapeutic Drugs
207
Lecture 5 - Quinolones, Folic Acid
Antagonists, and Urinary Tract
Antiseptics
Inhibitors of microbial growth:
A. Sulfonamides
Are large group of compounds that have similar structures
to p-aminobenzoic acid (PABA).
Sulfonamides are divided into:
1)
Oral absorbable sulphonamides:
a)
Short acting ( t
½
= 6hrs )
sulfamethiazole
and
sulfasoxazole.
b)
Intermediate acting (t
½
= 10-17hrs)
sulfamethoxazole
,
sulfacetamide, sulfadiazine.
c)
Long acting (t
½
= 7-9days)
sulfadioxin.
2)
Oral non-absorbable sulfonamide as sulfasalazine.
3)
Topical sulfonamide:
mafenide, silver sulfadiazine , sulfacetamide
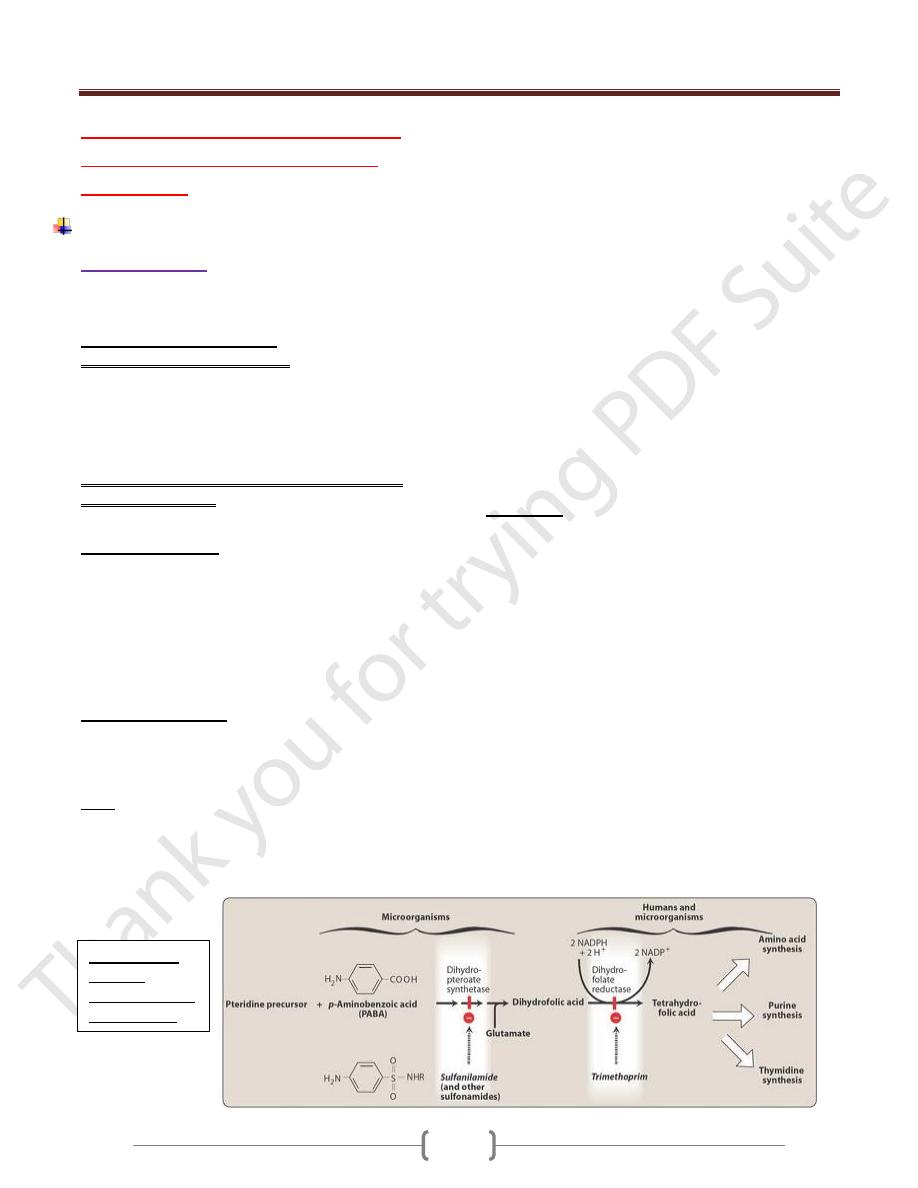
Mechanism of action:
Sulfonamides interfere with microbial growth by
competitively inhibiting incorporation of PABA into folic
acid, thereby inhibiting the synthesis of folic acid which is
an essential
compound to bacterial growth. Humans acquire folic acid
from diet as they cannot synthesis folic acid thus
sulfonamides selectively inhibit microbial growth.
Antimicrobial activity:
Effective against G+ve, some G-ve bacteria and
Chlamydia, as well as Nocardia asteroids, some enteric
bacteria as E.coli, klebseilla, salmonella and shigella.
Uses:
1) Oral absorbable sulphonamides The short acting
sulfonamides are used in treating acute uncomplicated
UTI
s
caused by E.coli, meningococcal meningitis and
shigellosis.
Sulfadiazine and sulfasoxazole are useful in the
prevention of streptococcal infection in patients with
rheumatoid arthritis who are allergic to penicillins, but not
against established streptococcal pharyngitis.
Sulfadiazine is combined with pyrimethamine
(antiprotozol) as a first line in the treatment of
toxoplasmosis.
Sulfadoxine is combined with pyrimethamine in the
treatment falciparum malaria.
2) Oral non-absorbable as sulfasalazine is used for the
treatment of ulcerative colitis.
3) Topical agents:
Silver sulfadiazine cream is widely used in preventing
infection in burn.
Sulfacetamide is used topically for treating ocular infection.
Haemophilus vaginalis infections are treated
intravaginally with triple sulfa preparation (sulfathiazole,
sufacetamide and sulfabenzamide).
Side effects:
1) Hypersensitivity: as rash, angioedema and Stevens-
syndrome (characterized by fever, malaise, erythema,
ulceration of mucous membranes of mouth and genitalia)
the latter occurs more with longer acting agents.
2) Crystalluria: high urine concentration of sulfonamides or
its metabolites may form crystals causing bleeding or
complete kidneys obstruction. Adequate hydration and
alkalinization of urine prevent the problem. With the
newer water soluble agents such as sulfasoxazole and
sulfamethoxazole are more soluble at urinary pH than the
older sulfonamides for e.g sulfadiazine.
3) Hemopoietic disturbances: Hemolytic anemia occurs
with genetic deficiency of RBC
s
and G-6PD.
4) Sulfonamides displace bilirubin from binding sites on
serum albumin in newborns causing kernicterus which is
a toxic encephalopathy so sulfonamides should not to be
administered to newborns or to women during the last 2
months pregnancy.
Mechanism of
action of
sulfonamide and
trimethoprim
Unit 7: Chemotherapeutic Drugs
208
5) Drug potentiation: transient potentiation of
hypoglycemic effect of tolbutamide or the anticoagulant
effect of warfarin.
B.Trimethoprim:
Mechanism of action:
It competitively inhibits dihydrofolate reductase enzyme
that catalyze the reduction of folic acid to tetrahydrofolic
acid (as we see in the figure), leading to a decrease in the
folate coenzymes for purine, pyrimidine and amino acid
biosynthesis. Bacterial reductase has a much stronger
affinity for trimethoprim than does the mammalian
enzyme.
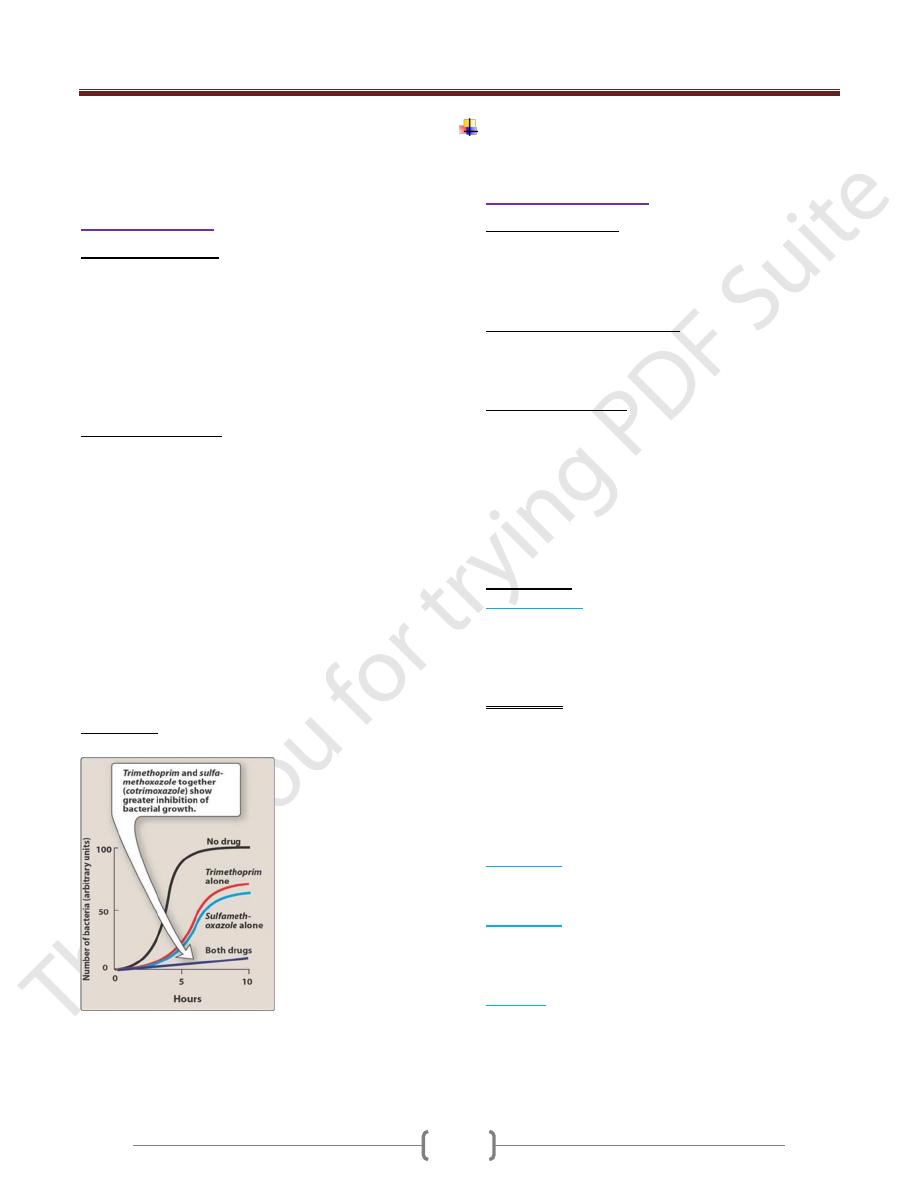
Antibacterial activity:
Trimethoprim is 20 to 50 times more potent than the
sulfonamide.Trimethoprim may be used alone in a cute
urinary tract infections and in the treatment of bacterial
prostitise. It’s commonly used with sulfamethoxazole
(called Co-trimoxazole), shows greater antimicrobial
activity than equivalent quantities of either drug used
alone.
Co-trimoxazole has activity against most aerobic and
facultative G+ve and G-ve. It has not active against
anaerobic and P.aeruginosa. It may be taken for
pneumocystic carinii, genital infections, prostate and
urinary tract infections, gastrointestinal infections,
respiratory infections.
Side effects: the same as sulfonamides.
Synergism between trimethoprim and sulfamethoxazole
on the inhibition of growth of Escherichia coli.
Inhibitors of nucleic acid function or
synthesis.
A. Fluoroquinolones:
Mechanism of action: they block the DNA synthesis by
inhibiting the replication of bacterial DNA gyrase
(topoisomerase II) during bacterial growth and
reproduction.
Members of fluoroquinolones:
Ciprofloxacin, Norfloxacin, Ofloxacin, Enoxacin and
Lomefloxacin
Antibacterial activity:
They are bactericidal, effective against G-ve organisms
such as enterobacteria, pseudomonas organisms,
Haemophilus influenzae, Moraxella catarrhalis,
Legionella, Chlamydia, Gonorrhea and Mycobacteria, not
effective against anaerobic bacteria. They have less
activity against G+ve bacteria; they should be avoided in
the treatment of pneumoccal or enterococcal infections.
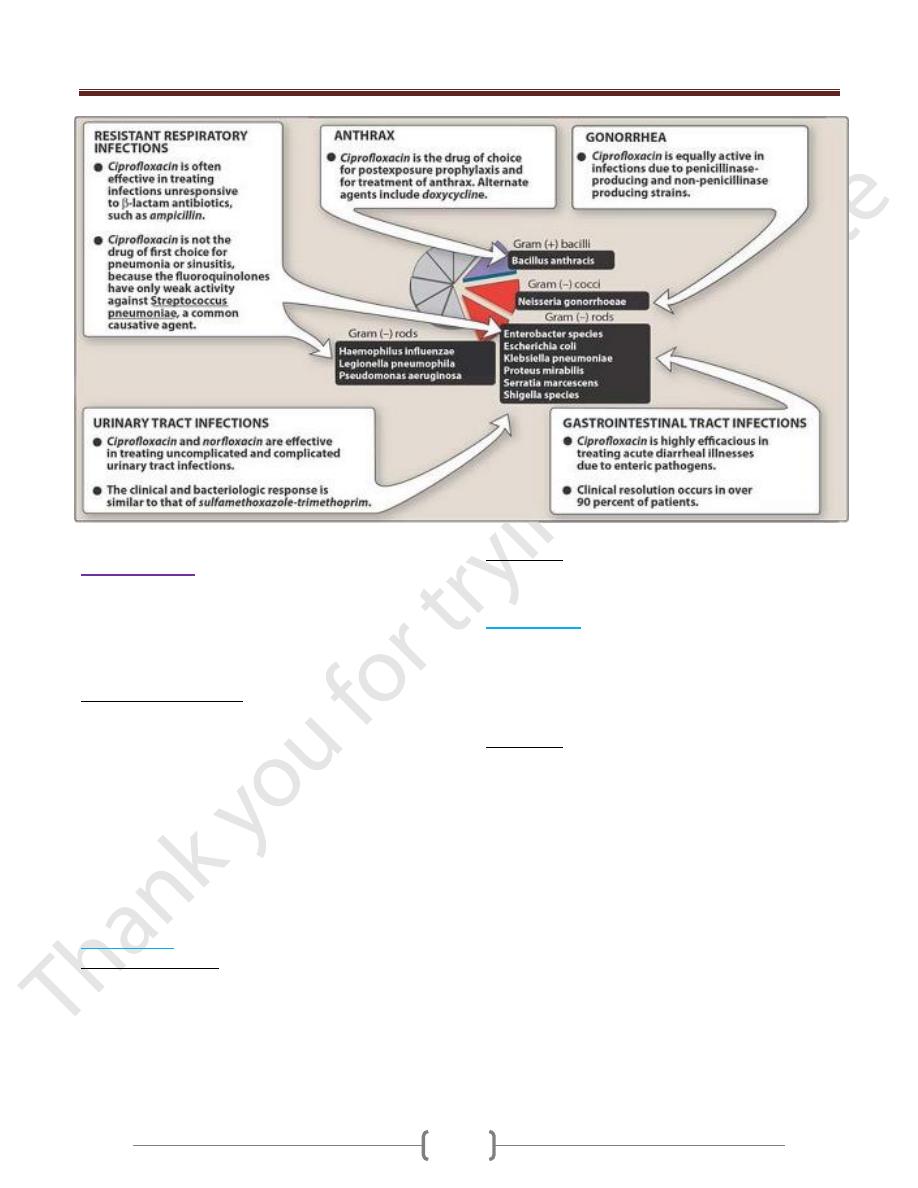
Clinical uses:
1) Ciprofloxacin :
has good activity in treating UTI
s
, intra-
abdominal biliary infections, respiratory tract infection,
cystic fibrosis complicated by P. aeruginosa infections of
the lung, Osteomylitis, bowel infections and all form of
gonorrhea.
Side effects:
1) GI upset (nausea, vomiting, diarrhea, abdominal pain).
2) Allergic reactions (rashes, urticaria).
3) CNS reactions (headache, visual disturbances, depression
and dizziness).
4) Hypoglycemia and may cause damage to the growing
cartilage this occur especially in children.
2) Norfloxacin
is useful in treating uncomplicated UTI
s
including those caused by G-ve rods and G+ve cocci.
3) Ofloxacin is
similar to ciprofloxacin, effective in treating
lower respiratory infections and acute urethral and
cervical gonorrhea, but its not suitable for P.aeruginosa
infections.
4) Enoxacin
is used in the treatment of gonorrhea, UTI
s,
and
chronic bronchitis.
Typical therapeutic application of ciprofloxacine in figure
below
Unit 7: Chemotherapeutic Drugs
209
B. Quinolones:
Nalidxic acid is a quinolone with the same mechanism of
action as that of fluoroquinolones. It is effective against
most of the G-ve bacteria that commonly causes UTI
s
but
G+ve organism are resistance.
Urinary tract antiseptics:
Urinary tracts infections are the most common problems
in women of child bearing age, and in elderly. E. coli,
Staphylococcus saprophyticus, Klebsiella pneumoniae
and Proteus mirabilis are the most common bacterial
pathogen causing infection the upper and lower UTI.
These types of infections may be treated by group of
agents called urinary tract antiseptics, including
methenamine and nitrofurantoin. These drugs do not
achieve antibacterial levels in the circulation, but because
they are concentrated in the urine, microorganisms at that
site can be effectively eradicated.
1) Methenamine:
Mechanism of action:
It metabolizes at an acidic pH of 5.5 or less in the urine to
formaldehyde, which is toxic to most bacteria.
Methenamine is frequently formulated with a weak acid
as mandelic acid, which lowers the pH of the urine thus
aiding decomposition of the drug.
Side effects:
Gastrointestinal distress, albuminuria, hematuria and
rashes may develop.
2) Nitrofurantoin
: the drug is bacteriostatic. It is useful
against E.coli but other common urinary tract G-ve
bacteria may be resistance. The drug is rapidly excreted
by glomerular filtration. The presence of the drug turns
the urine brown, a surprise for unsuspecting patients.
Side effects:
GIT disturbances (nausea, vomiting and diarrhea),
Neuropathies and hemolytic anemia in G-6-phospate
dehyd- rogenase deficiency.
