Unit 7: Chemotherapeutic Drugs
193
Lecture 1 - Principles of
Antimicrobial Therapy
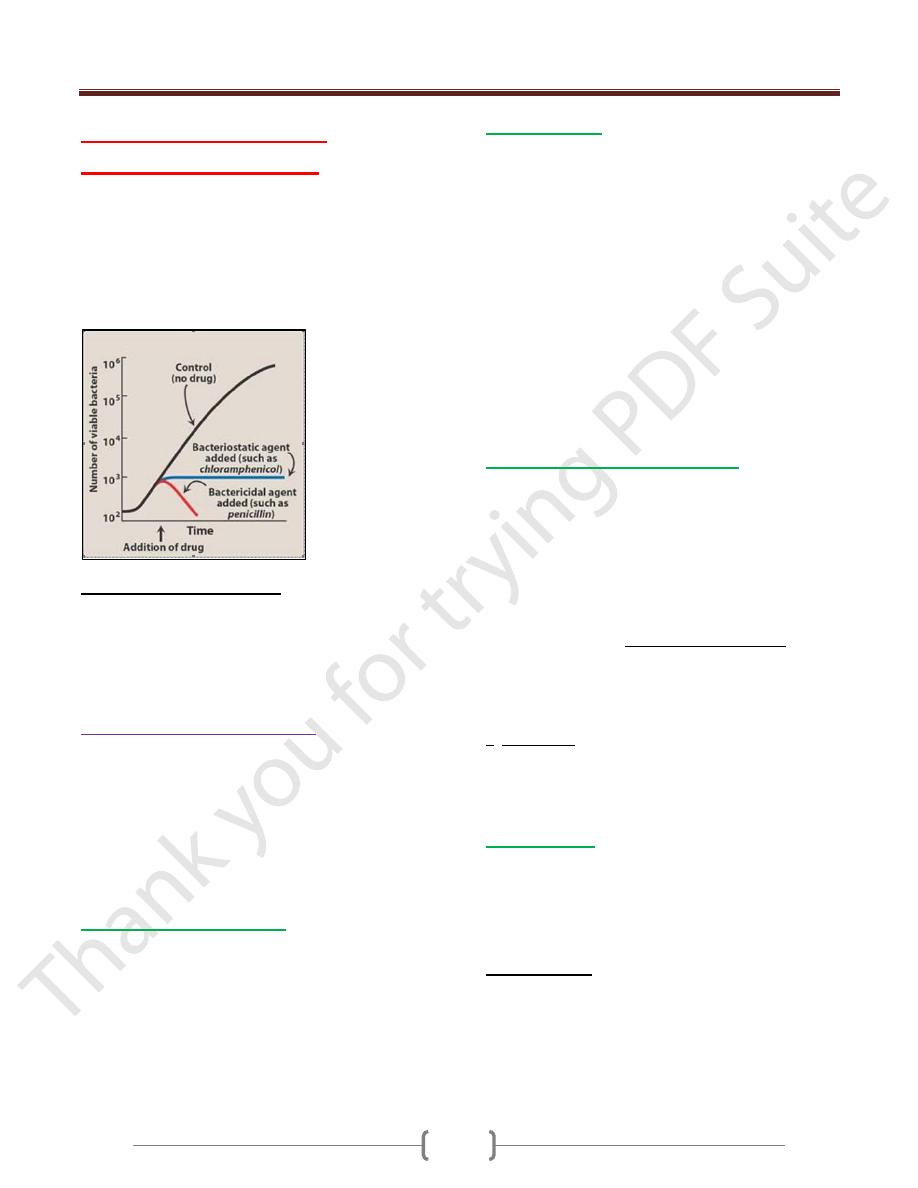
They are drugs used in case of infections. They inhibit the
growth (bacteriostatic) or kill (bactericidal)
microorganism without causing harm to the cell of the
host. The concentration of the drug must be carefully
controlled to attack the microorganism while still being
tolerated by the host.
Source of antimicrobial agents:
1) Natural from living organism mostly fungus and
sometimes bacteria. These are called antibiotics.
2) Synthetic: obtained manufacturely.
3) Semi-synthetic: taken from the living organism and
modified manufacturely.
Selection of antimicrobial agents:
Selection of the most appropriate antimicrobial agent
requires knowledge of:
1) Diagnosis of infection
2) Site of infection
3) Ideal therapy used to treat infection
4) Patient factors
5) Safety of the agent
6) Cost of therapy
1) Make a diagnosis of infection
. This is either:
a) Clinical diagnosis might enable us to initiate therapy such
as in syphilis we use penicilline.
b) Microbiological either:
Direct smear: take a sample for culture in special Lab
to estimate the type of bacteria before starting the
prescribe of drugs, as in case of urinary tract infection
Indirect method as for e.g to find the Abs in plasma by
widal test.
2) Site of infection:
for a drug to be effective, it must be
capable of reaching the site of infection in adequate
amounts and the site of infection might determine the
choice o\f the antibiotic and this depend on the
pharmacokinetic properties of the drug.
e.g ampicilline, amoxycillin, cephalosporine and
rifampicin tend to achieve high conc. in the bile so they
are suitable for biliary infections. The site of infection
may also determine the dose of the drug for example the
eye, prostate and bones are poorly penetrated by drugs
and infection to them requires higher dosages. Higher
dose is also needed in case of infection to vascular tissues
as in case of bacterial endocarditis. Also the site of
infection will determine the route of administration of the
drug as in case meningitis we may give the drug
intrathecally i.e. into the CSF.
3) Ideal therapy used to treat infection
: The
antimicrobial agent used to treat an infection is selected
after the organism has been identified. In the critical ill
patient, such a delay could prove fatal, and immediate
empiric therapy is indicated. Symptoms characteristic of
meningitis require immediate treatment. Therapy is
initiated after specimens for laboratory analysis have been
obtained but before the results of the culture are available.
A gram-positive coccus in the spinal fluid of a newborn
infant is unlikely to be Streptococcus pneumoniae
(pneumococcus) but most likely to be Streptococcus
agalactiae (Group B). This organism is sensitive to
penicillin G. By contrast, a gram-positive coccus in the
spinal fluid of a forty year old patient is most likely to be
S. pneumoniae. This organism is frequently resistance to
penicillin G, and often requires treatment with a third-
generation cephalosporin (such as cefotaxime or
ceftriaxone) or vancomycin.
4) Patient factors:
In selecting an antibiotic, attention must be taken in
consideration. For example, the status of the patients
immune system, kidneys, and liver must be considered. In
women, pregnancy or breast-feeding an infant also affect
the selection of the antimicrobial agent.
a) Immune system: Elimination of infecting organism from
the body depends on an intact immune system.
Antibacterial drugs decrease the microbial population
(bactericidal), or inhibit further bacterial growth
(bacteriostatic), but the host defense system must
ultimately eliminate the invading organisms. Alcoholism,
diabetes, infection with the human immunodeficiency
Unit 7: Chemotherapeutic Drugs
194
virus, malnutrition, or advanced age can affect on the
patients. Higher than usual doses of bactericidal agents or
longer treatment are required to eliminate the infective
organisms in these individuals.
b) Renal dysfunction: Poor kidney function (10% or less of
normal) leads to accumulation of the drugs that are
eliminated through this route and this will lead to adverse
effects unless controlled by adjusting the dose of the
antibiotic. Although serum creatinine levels are
sometimes used as an index of renal function for adjusting
of drug regimens. However, direct monitoring of serum
levels of some antibiotics (for example aminoglycosides)
is preferred to identify maximum and minimum values.
Drugs contra-indicated in renal disease. Cephalothin,
Cephaloridine, nitrofurantoin, tetracycline (except
doxycycline).
Dose reduction required in renal failure.
Aminoglycoside, amphotericin-B, vancomycin and
ethambutol.
Note: penicillin and rifampicin do not require dose
adjustment in renal disease.
c) Hepatic function: Antibiotics that are concentrated or
eliminated by the liver (for example, erythromycin, and
tetracycline) are contraindicated in treating patients with
liver disease.
d) Poor perfusion: Decreased circulation to an anatomic
area as in the lower limbs of the diabetic reduces the
amount of antibiotic that reaches that site.
e) Pregnancy: All antibiotics cross the placenta. adverse
effects to the fetus are rare, except for tooth dysplasia and
inhibition of bone growth occur in case of tetracycline.
Aminoglycosides should be avoided in pregnancy because
of their ototoxic effect in the fetus.
f) Lactation: Drugs administered to a lactating mother may
enter the nursing infant via the breast milk. Although The
concentration of an antibiotic in breast milk is usually
low; the total dose to the infant may be enough to cause
problems.
g) Age: In very young infant, the renal and hepatic
elimination processes are poorly developed making them
susceptible to the toxic effects of certain antibiotics such
as chloromphenicol and the sulfonamides. Young children
should not be treated with tetracycline which affect bone
growth or fluoroquinolones which interfere with cartilage
growth.
5) Safety of the agent:
many of the antibiotics, such as
the penicillins, are among the least toxic of all drugs
because they interfere with a site unique to the growth of
microorganism. Other antimicrobial agent as with
chloromphenicol may cause serious toxicity.
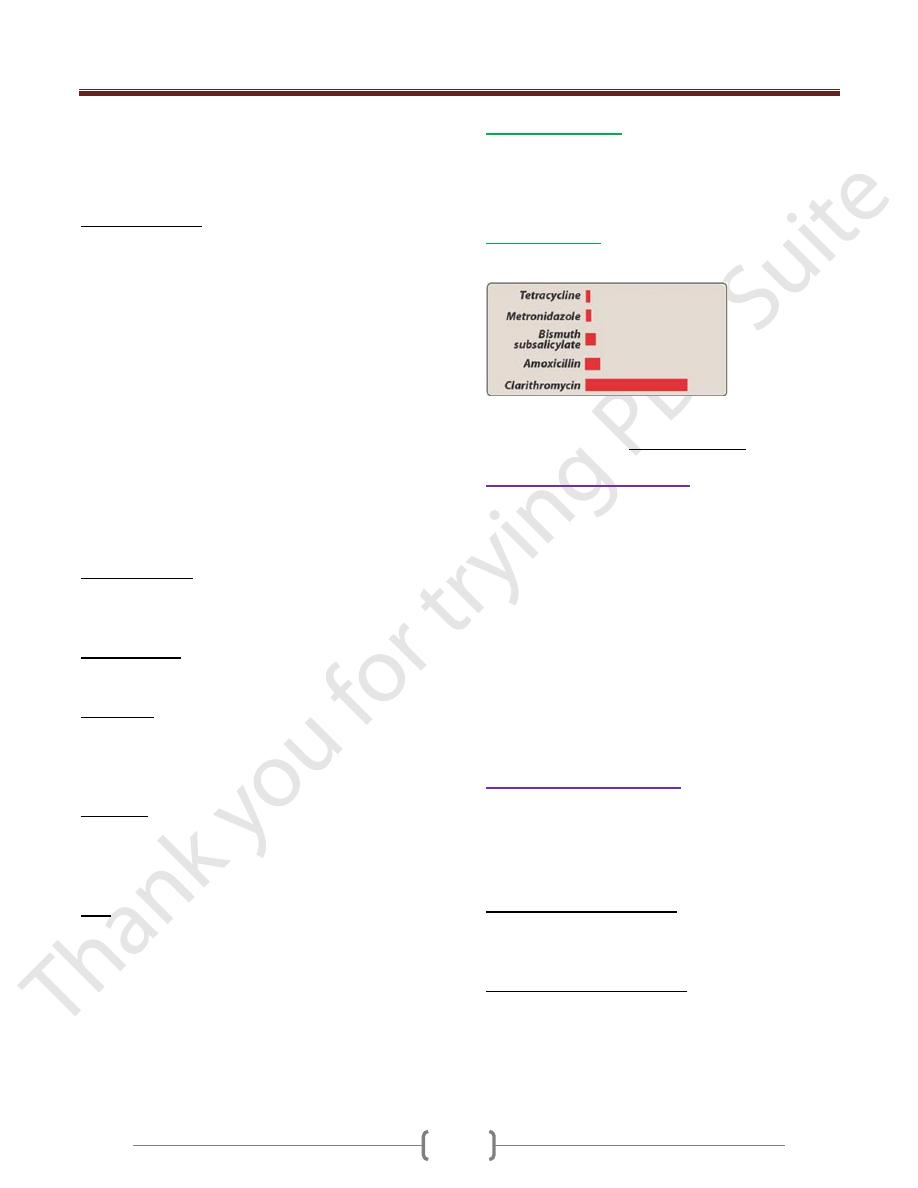
6) Cost of therapy:
several drugs may show similar
efficacy in treating an infection, but vary widely in cost.
Relative cost of some drugs used for the treatment of
peptic ulcers caused by Helicobacter pylori
Administration of antibiotics
Must administer the drug in optimum dose and by the
most appropriate route.
Inadequate dose may lead to the development microbial
resistance.
We have to continue the therapy until apparent cure is
achieved, for most acute infection, it is usually required 5-
10 days except in some conditions as typhoid fever, T.B,
brucellosis and infective endocarditis in which relapse
may occur and we must continue the prescription for
longer period of time.
In certain infection we must do test for cure as in case of
UTI where microbiological examination must be done
after withdrawal of the antibiotic.
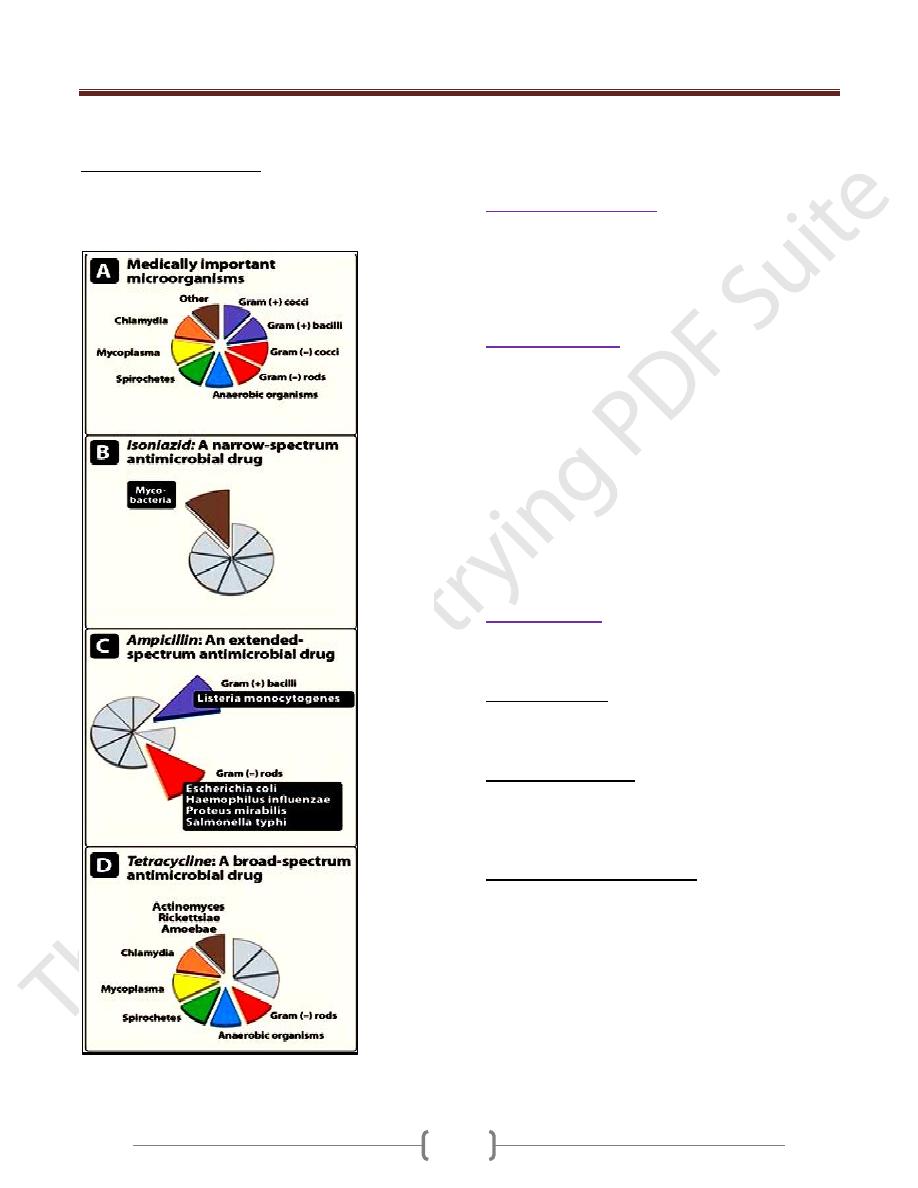
Chemotherapeutic Spectra:
The clinically important bacteria have been organized into
eight groups based on Gram stain, morphology, and
biochemical or other characteristics (figure A). Figure
below illustrates the spectra of bacteria for which a
particular class of antibiotics is therapeutically effective.
A. Narrow-spectrum antibiotics: Chemotherapeutic agents
acting only on a single or a limited group of microorganisms
are said to have a narrow spectrum. For example, isoniazid is
active only against mycobacteria (Figure B).
B. Extended-spectrum antibiotics: Extended spectrum is
the term applied to antibiotics that are effective against
gram-positive organisms and also against a significant
number of gram-negative bacteria. For example,
ampicillin is considered to have an extended spectrum,
Unit 7: Chemotherapeutic Drugs
195
because it acts against gram-positive and some gram-
negative bacteria (Figure C).
C. Broad-spectrum antibiotics: Drugs such as tetracycline
and chloramphenicol affect a wide variety of microbial
species and are referred to as broad-spectrum antibiotics
(Figure D).
A. Color-coded representation of medically important m.os.
B. Isoniazid a narrow-spectrum antimicrobial agent.
C. Ampicillin an extended-spectrum antimicrobial agent.
D. Tetracycline a broad-spectrum antimicrobial agent.
Combination of antibiotics
a) If there is mixed infection.
b) To obtain Potentiation or synergism.
c) To delay the development of bacterial resistance,
especially in chronic infection.
d) In case of severe infection.
Chemoprophylaxis
To prevent infection usually by one organism rather than
multiple organisms as
1) True prevention of infection
e.g rheumatic fever and recurrent GITI and UTI.
2) Suppression of existing infection before causing the
disease. e.g T.B and malaria
3) Prevention of bacterial endocarditis after dentistry.
4) Prevention of excacerbation of chronic infection e.g
bronchitis and in cystic fibrosis
5) Prevention of spread disease as in an epidemic of
meningitis.
6) In surgery, when risk of infection is high.
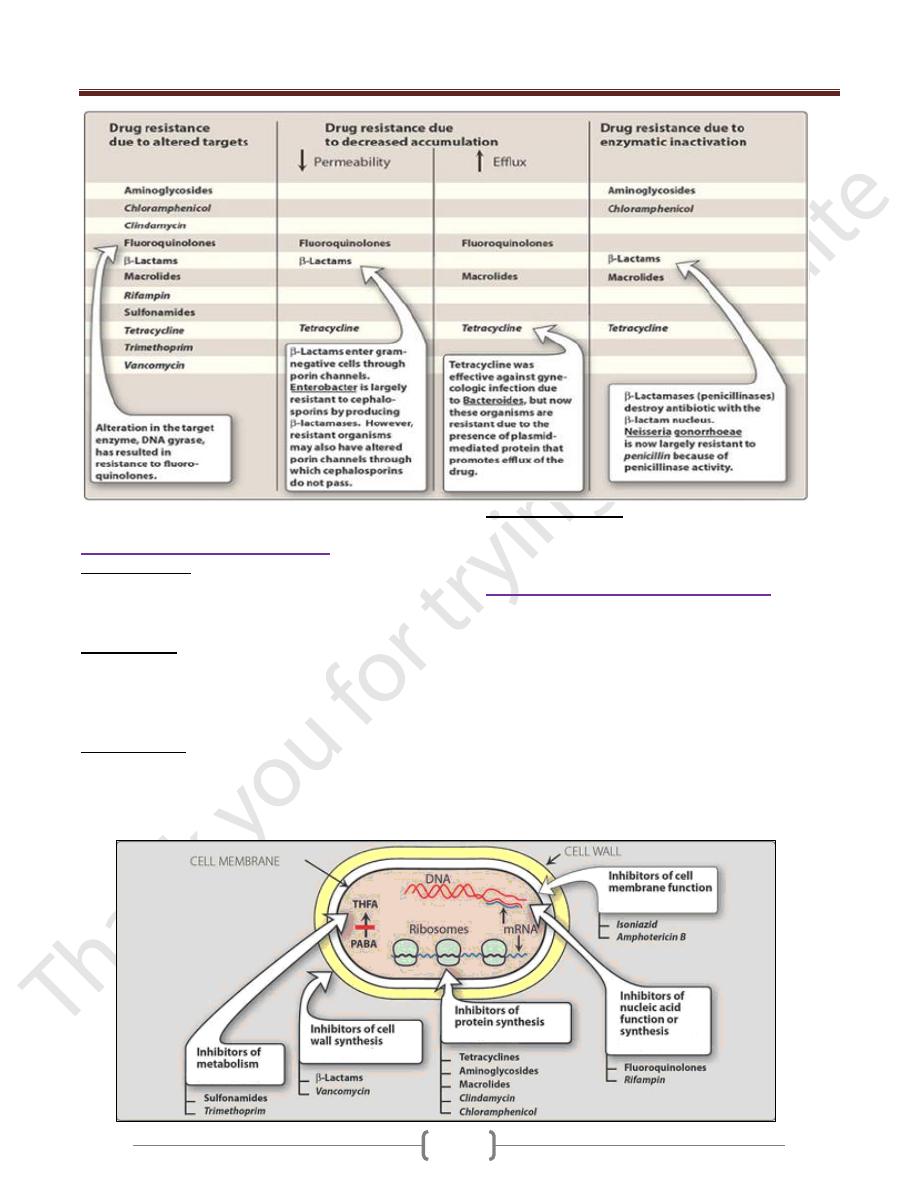
Drug resistance:
Bacteria are said to be resistance if their growth is not
halted by the maximal level of an antibiotic that is
tolerated by the host.
1) Natural resistance: In which the organisms are
inherently resistance to an antibiotic during the course of
therapy. For example gram-negative organisms are
resistance to vancomycin.
2) Spontaneous mutation: Resistance may be cause by a
change in the affinity of the DNA-dependant RNA
polymerase for the drug. An example is the emergence of
rifampin-resistance Mycobacterium tuberculosis when
rifampin is used as a single antibiotic.
3) DNA transfer of drug resistance: Is resistance acquired
due to DNA transfer from one organism to another, and
the most important way of transmission is in the form of
plasmids which will encode for the production of BETA-
lactamase against penicillin.
Unit 7: Chemotherapeutic Drugs
196
Some mechanism of resistance to antibiotics
Complication of antibiotic therapy:
1) Hypersensitivity: hypersensitivity reactions against the
antibiotic or its metabolites. For example, the penicillins
can cause serious hypersensitivity problems ranging from
urticaria to anaphylactic shock.
2) Direct toxicity: high serum levels of certain antibiotics
may cause toxicity by affecting cellular processes in the
host directly. For example aminoglycosides can cause
ototoxicity by interfering with membrane function in the
hair cells of the organ of Corti.
3) Superinfections: may be caused by the antibiotic due to
alteration of the normal microbial flora of the body
permitting the overgrowth of the opportunistic organisms,
especially fungi or resistance bacteria. These infections
are often difficult to treat.
4) Masking of infection: some times, an antibiotic given for
certain disease may mask anathor one, e.g penicillin given
for gonorrhea may mask the 1
st
and 2
nd
stages of syphilis.
Classification of antibacterial agents:
Antibacterial agents can be classified in a number of ways
these include:
1) Inhibitors of cell wall synthesis.
2) Protein synthesis inhibitors.
3) Inhibitors of metabolism.
4) Inhibitors of nucleic acid function or synthesis.
5) Inhibitors of cell membrane function.
The following figure shows the classification of some
antibacterial agents by their sites of action (THFA =
tetrahydrofolic acid; PABA = para-aminobenzoic acid).
