Unit 12: Lung (Diseases of respiratory system)
071
Atelectasis (collapse)
It is loss of lung volume caused by inadequate expansion
of airspaces. It results in shunting of inadequately
oxygenated blood from pulmonary arteries into veins,
thus giving rise to a ventilation-perfusion imbalance &
hypoxia.
Atelectasis is classified into three forms:-
1) Resorption Atelectasis
Resorption atelectasis occurs when an obstruction
prevents air from reaching distal airways. Depending on
the level of airway obstruction, an entire lung, a complete
lobe, or one or more segments may be involved.
Causes of resorption collapse is obstruction of a bronchus
by a mucous or mucopurulent plug. This frequently
occurs postoperatively, also complicate bronchial asthma,
bronchiectasis, chronic bronchitis, or the aspiration of
foreign bodies.
2) Compression Atelectasis
This usually associated with accumulations of fluid,
blood, or air within the pleural cavity, which
mechanically collapse the adjacent lung. This is a frequent
occurrence with pleural effusions, caused most commonly
by congestive heart failure (CHF). Leakage of air into the
pleural cavity (pneumothorax) also leads to compression
atelectasis.
Basal atelectasis resulting from the elevated position of
the diaphragm commonly occurs in
1- bedridden patients
2- patients with ascites,
3- patients during and after surgery.
3) Contraction Atelectasis
Occurs when either local or generalized fibrotic changes
in the lung or pleura hamper expansion and increase
elastic recoil during expiration.
Acute lung injury
Acute Respiratory Distress Syndrome (ARDS)
ARDS is a clinical syndrome caused by diffuse alveolar
capillary and epithelial damage. There is usually rapid
onset of life-threatening respiratory insufficiency,
cyanosis, and severe arterial hypoxemia that is refractory
to oxygen therapy and that may progress to multisystem
organ failure. The histologic manifestation of ARDS in
the lungs is known as diffuse alveolar damage. ARDS is
associated with either direct injury to the lung or indirect
injury in the setting of a systemic process.
Pathogenesis
The alveolar capillary membrane is formed by 2 separate
barriers: the microvascular endothelium and the alveolar
epithelium. In ARDS the integrity of this barrier is
compromised by either endothelial or epithelial injury, or both.
The acute consequences of damage to the alveolar
capillary membrane include
1- Creased vascular permeability →alveolar flooding,
2- Loss of diffusion capacity
3- Widespread surfactant abnormalities caused by damage
to type II pneumocytes recent work suggests that in
ARDS, lung injury is caused by an imbalance of pro-
inflammatory and anti-inflammatory mediators. Nuclear
factor κB (NF-κB), whose activation is tightly regulated
under normal conditions shifting the balance in favor of
pro-inflammatory state. As early as 30 minutes after an
acute insult, there is increased synthesis of interleukin 8
(IL-8), a potent neutrophil chemotactic and activating
agent, by pulmonary macrophages as well asIL-1 &
(TNF), leads to endothelial activation, and pulmonary
microvascular sequestration and activation of neutrophils.
Activated neutrophils release a variety of products (e.g.,
oxidants, proteases, platelet-activating factor, &
leukotrienes) that cause damage to the alveolar epithelium
and maintain the inflammatory cascade. Combined assault
on the endothelium and epithelium perpetuate vascular
leakiness and loss of surfactant that render the alveolar unit
unable to expand. It should be noted that the destructive
forces unleashed by neutrophils can be counteracted by an
array of endogenous antiproteases, antioxidants, and anti-
inflammatory cytokines (e.g. IL-10) that are upregulated by
pro-inflammatory cytokines. In the end, it is the balance
between the destructive & protective factors that determines
the degree of tissue injury and clinical severily of ARDS.
Causes of ARDS
Direct Lung Injury
Indirect Lung Injury
Pneumonia
Sepsis
Aspiration of gastric contents
Severe trauma with shock
Uncommon Causes
Pulmonary contusion
Cardiopulmonary bypass
Fat embolism
Acute pancreatitis
Near-drowning
Drug overdose
Inhalational injury
Transfusion of blood products
Uremia
Morphology
In the acute phase of ARDS the lungs are dark red, firm,
airless, and heavy. Microscopically, there is capillary
congestion, necrosis of alveolar epithelial cells, interstitial
and intra-alveolar edema and hemorrhage, collections of
Unit 12: Lung (Diseases of respiratory system)
070
neutrophils in capillaries. The most characteristic finding
is the presence of hyaline membranes, particularly lining
the distended alveolar ducts. consist of fibrin-rich edema
fluid admixed with remnants of necrotic epithelial cells.
Overall, the picture is remarkably similar to that seen in
respiratory distress syndrome in the newborn.
In the organizing stage there is marked proliferation of
type II pneumocytes in an attempt to regenerate the
alveolar lining. Resolution is unusual; more commonly
there is organization of the fibrin exudates, with resultant
intra-alveolar fibrosis. Marked thickening of the alveolar
septa caused by proliferation of interstitial cells and
deposition of collagen.
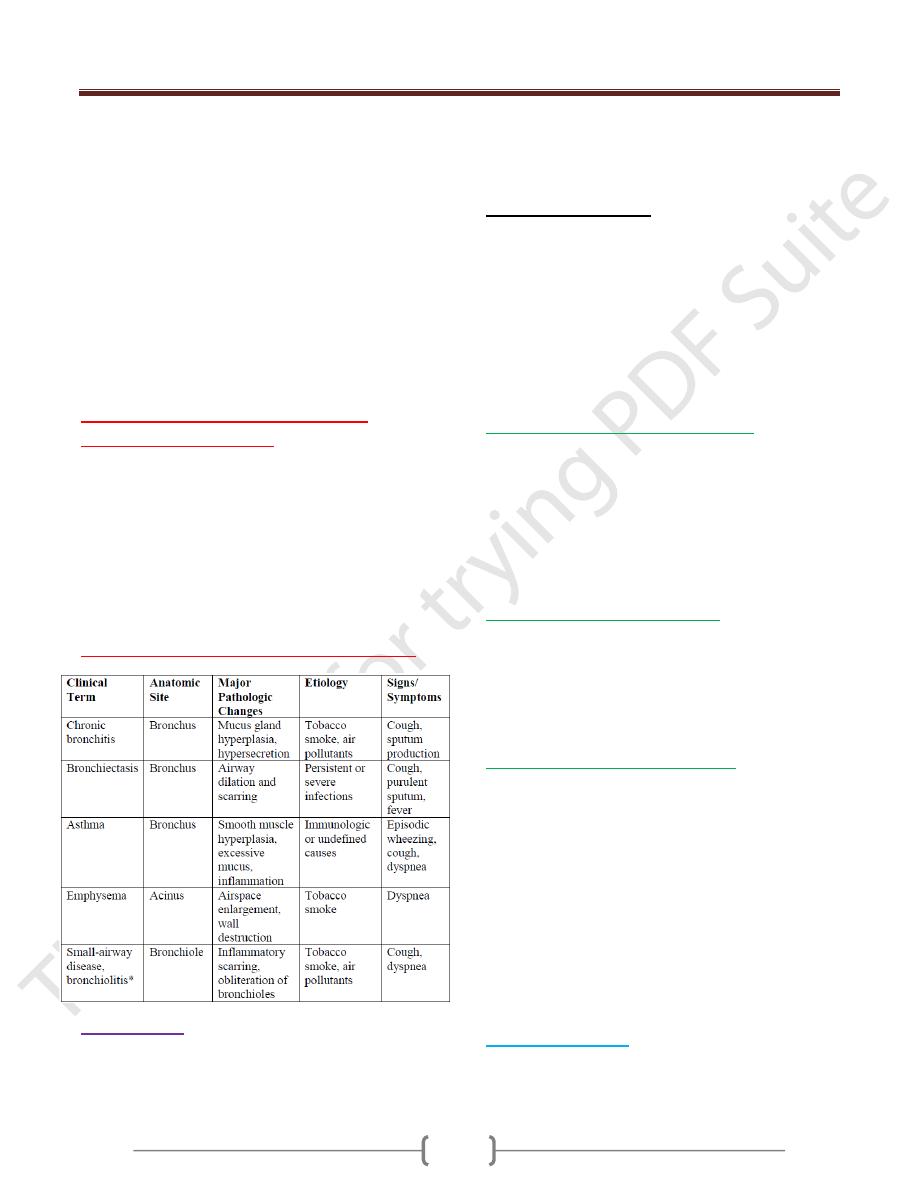
Obstructive versus restrictive
pulmonary diseases
Diffuse pulmonary diseases can be classified in 2 categories
(1) Obstructive disease (airway disease), characterized by
limitation of airflow usually resulting from an increase in
resistance caused by partial or complete obstruction at any
level, (2) Restrictive disease, characterized by reduced
expansion of lung parenchyma accompanied by decreased
total lung capacity.
Obstructive lung (airway) diseases
Emphysema
It characterized by abnormal permanent enlargement of the
airspaces distal to the terminal bronchioles, accompanied
by destruction of their walls without obvious fibrosis.
overinflation conditions in which enlargement of airspaces is
not accompanied by destruction e.g.the distention of airspaces
in the opposite lung after unilateral pneumonectomy
Types of Emphysema
Emphysema is classified according to its anatomic
distribution within the lobule; recall that the acinus is the
structure distal to terminal bronchioles, and a cluster of
three to five acini is called a lobule.
There are four major types of emphysema: (1)
centriacinar, (2) panacinar, (3) distal acinar, and (4)
irregular. Only the first two cause clinically significant
airway obstruction, with centriacinar emphysema being
about 20-times more common than panacinar disease.
1) Centriacinar (Centrilobular) Emphysema
In which the central or proximal parts of the acini, formed
by respiratory bronchioles, are affected, while distal
alveoli are spared. Thus, both emphysematous and normal
airspaces exist within the same acinus and lobule. The
lesions are more common and severe in the upper lobes,
particularly in the apical segments. commonly seen as a
consequence of cigarette smoking in people who do not
have congenital deficiency of α
1
-antitrypsin
2) Panacinar (Panlobular) Emphysema
In this type of emphysema, the acini are uniformly
enlarged from the level of the respiratory bronchiole to
the terminal blind alveoli. In contrast to centriacinar
emphysema, panacinar emphysema tends to occur more
commonly in the lower lung zones and is the type of
emphysema that occurs in α
1
-antitrypsin deficiency.
3) Distal Acinar (Paraseptal) Emphysema
In this form, the proximal portion of the acinus is normal
but the distal part is primarily involved. The emphysema
is more striking adjacent to the pleura, along the lobular
connective tissue septa, and at the margins of the lobules.
It occurs adjacent to areas of fibrosis, scarring, or
atelectasis and is usually more severe in the upper half of
the lungs. The characteristic findings are the presence of
multiple, contiguous, enlarged airspaces that range in
diameter from less than 0.5 mm to more than 2.0 cm,
sometimes forming cystlike structures that with
progressive enlargement are referred to as bullae. This
type of emphysema probably underlies many of the cases
of spontaneous pneumothorax in young adults.
4) Irregular Emphysema
Irregular emphysema, so named because the acinus is
irregularly involved, is almost invariably associated with
scarring, such as resulting from healed inflammatory
Unit 12: Lung (Diseases of respiratory system)
071
diseases. Although clinically asymptomatic, this may be
the most common form of emphysema.
Pathogenesis
Emphysema arising as a consequence of the protease-
antiprotease imbalance
The protease-antiprotease imbalance hypothesis is based
on the observation that patients with a genetic deficiency
of the antiprotease α
1
-antitrypsin have a markedly
enhanced tendency to develop pulmonary emphysema,
which is compounded by smoking. About 1% of all
patients with emphysema have this defect. α
1
-Antitrypsin,
normally present in serum, which is a major inhibitor of
proteases (particularly elastase) secreted by neutrophils
during inflammation.
α
1
-Antitrypsin is encoded by (Pi) locus on chromosome 14.
The following sequence is postulated:
1) 1-Neutrophils (the principal source of cellular proteases)
are normally sequestered in peripheral capillaries,
including those in the lung, and a few gain access to the
alveolar spaces.
2) 2-Any stimulus that increases either the number of
leukocytes (neutrophils and macrophages) in the lung or
the release of their protease-containing granules increases
proteolytic activity.
3) 3-With low levels of serum α
1
-antitrypsin, elastic tissue
destruction is unchecked and emphysema results.
In smokers, neutrophils and macrophages accumulate in
alveoli. The mechanism of inflammation is not entirely
clear, but possibly involves the direct chemo attractant
effects of nicotin , these activate the transcription factor
NF-κB, which switches on genes that encode TNF and
chemokines, including IL-8. These, in turn, attract and
activate neutrophils. Accumulated neutrophils are
activated and release their granules, rich in a variety of
cellular proteases (neutrophil elastase, proteinase 3, and
cathepsin G), resulting in tissue damage.
Smoking also enhances elastase activity in macrophages;
macrophage elastase is not inhibited by α
1
-antitrypsin and,
indeed, can proteolytically digest this antiprotease. There
is increasing evidence that in addition to elastase, matrix
metalloproteinases derived from macrophages and
neutrophils have a role in tissue destruction.
Morphology
The diagnosis and classification of emphysema depend
largely on the macroscopic appearance of the lung.
Panacinar emphysema, when well developed, produces
pale, voluminous lungs that often obscure the heart when
the anterior chest wall is removed at autopsy.
In centriacinar emphysema the lungs are a deeper pink
than in panacinar emphysema and less voluminous, unless
the disease is well advanced.
Generally, in centriacinar emphysema the upper two-
thirds of the lungs is more severely affected than the
lower lungs.
Histologically there is thinning and destruction of
alveolar walls. With advanced disease, adjacent alveoli
become confluent, creating large airspaces. Terminal and
respiratory bronchioles may be deformed because of the
loss of septa that help tether these structures in the
parenchyma. With the loss of elastic tissue in the
surrounding alveolar septa, there is reduced radial traction
on the small airways. As a result, they tend to collapse
during expiration-an important cause of chronic airflow
obstruction in severe emphysema. In addition to alveolar
loss, the number of alveolar capillaries is diminished.
Chronic Bronchitis
Is defined as a persistent productive cough for at least
3 consecutive months in at least 2 consecutive years. It
is common among cigarette smokers and urban dwellers
in smog-ridden cities; about 20% - 25% of men in the 40-
to 65-year age have the disease. Recurrent infections and
respiratory failure are constant threats & diagnosis is
made on clinical grounds.
Pathogenesis
Environmental irritants mainly cigarette smoking &
other air pollutants, induce:-
1) Hypertrophy of mucous glands in the trachea & main-
stem bronchi and lead to a marked increase in mucin-
secreting goblet cells in the surface epithelium of smaller
bronchi and bronchioles lead to hypersecretion of mucus
2) Inflammation with infiltration of CD8+ T cells,
macrophages, and neutrophils.
The morphologic basis of airflow obstruction in
chronic bronchitis is more peripheral and results from
1) "Small airway disease," induced by goblet cell
metaplasia with mucus plugging of the bronchiolar
lumen, inflammation, and bronchiolar wall fibrosis.
2) Coexistent emphysema: chronic bronchitis with
significant airflow obstruction is almost always
complicated by emphysema.
Morphology
Grossly, the mucosal lining of the larger airways is
usually hyperemic and swollen due to edema. It is often
covered by a layer of mucinous or mucopurulent
Unit 12: Lung (Diseases of respiratory system)
071
secretions. The smaller bronchi and bronchioles may also
be filled with similar secretions.
Histologically,
(1) In the trachea and larger bronchi is enlargement of
the mucus-secreting glands. (2) Mixed inflammatory
cells, largely mononuclear but sometimes admixed with
neutrophils in the bronchial mucosa.
Chronic bronchiolitis (small airway disease),
characterized by goblet cell metaplasia, mucus plugging,
inflammation, and fibrosis, is also present. In the most
severe cases, there may be complete obliteration of the
lumen due to fibrosis (bronchiolitis obliterans). It is the
peribronchiolar fibrosis and luminal narrowing that results
in airway obstruction.
Asthma
Asthma is a chronic inflammatory airways disorder that
causes recurrent episodes of wheezing, breathlessness,
chest tightness, and cough, particularly at night and/or
early in the morning.
This clinical picture is caused by repeated immediate
hypersensitivity and late-phase reactions in the lung that
give rise
1) intermittent and reversible airway obstruction,
2) chronic bronchial inflammation with eosinophils,
3) Bronchial smooth muscle cell hypertrophy and
hyperreactivity. It is thought that inflammation causes
an increase in (bronchospasm) to a variety of stimuli.
About 70% of cases are said to be "extrinsic" or "atopic"
and are due to IgE and T
H
2-mediated immune responses
to environmental Ags. While in 30% asthma is said to be
"intrinsic" or "non-atopic" & is triggered by non-immune
stimuli such as aspirin; pulmonary infections,(viruses);
cold; psychological stress; exercise; and inhaled irritants.
Pathogenesis
The major etiologic factors of asthma are genetic
predisposition to type I hypersensitivity ("atopy"), acute
and chronic airway inflammation, and bronchial hyper-
responsiveness to a variety of stimuli.
1) Atopic asthma is associated with an excessive T
H
2
reaction against environmental antigens. Cytokines”IL-4”
produced by T
H
2 cells account for most of the features of
asthma- stimulates IgE production, IL-5 activates
eosinophils, and IL-13 stimulates mucus production. All
of these cytokines are produced by T
H
2 cells.
In addition, epithelial cells are activated to produce
chemokines that promote recruitment of more T
H
2 cells
and eosinophils & other leukocytes.
2) "airway remodeling." These changes include
hypertrophy of bronchial smooth muscle and deposition
of subepithelial collagen, it may occur over several years
before initiation of symptoms& its etiologic basis may be
an inherited predisposition associated with accelerated
proliferation of bronchial smooth muscle cells and
fibroblasts. The gene that implicated called ADAM33, .
Mast cells, are also thought to contribute to airway
remodeling by secreting growth factors that stimulate
smooth muscle proliferation.
Atopic Asthma
This most common type of asthma usually begins in
childhood. A positive family history of atopy is common,
and asthmatic attacks are often preceded by allergic
rhinitis, urticaria, or eczema. The disease is triggered by
environmental antigens, such as dusts, pollen, animal
dander, and foods…etc.
In the airways there is an initial sensitization to the
inhaled antigens, which stimulates induction of T
H
2-type
cells and release of interleukins IL-4 and IL-5. This leads
to synthesis of IgE that binds to mucosal mast cells.
Exposure of IgE-coated mast cells to the same antigen
causes cross-linking of IgE and the release of chemical
mediators. Mast cells on the respiratory mucosal surface
are initially activated; the resultant mediator release opens
mucosal intercellular junctions, allowing penetration of
the antigen to more numerous mucosal mast cells. In
addition, direct stimulation of subepithelial vagal
(parasympathetic) receptors provokes reflex
bronchoconstriction through both central and local
reflexes. This occurs within minutes after stimulation and
is therefore called the acute, or immediate, response,
which consists of bronchoconstriction, edema (due to
increased vascular permeability), and mucus secretion. A
variety of inflammatory mediators have been implicated
in the acute-phase response, includes: Leukotrienes C
4
,
D
4
, and E
4
, Acetylcholine, histamine. Prostaglandin
D
2
,.Platelet-activating factor.
Mast cells also release additional cytokines that cause the
influx of other leukocytes, including neutrophils &
mononuclear cells, & eosinophils. These inflammatory
cells set the stage for the late-phase reaction, which starts
4 to 8 hours later & may persist for 12 to 24 hours or more
Non- Atopic Asthma
Viral infections of the respiratory tract (most common)
and inhaled air pollutants such as sulfur dioxide, ozone,
and nitrogen dioxide. These agents increase airway hyper-
reactivity in both normal and asthmatic subjects. In the
Unit 12: Lung (Diseases of respiratory system)
071
latter, however, the bronchial response, manifested as
spasm, is much more severe and sustained. A positive
family history is uncommon, serum IgE levels are normal,
and there are no associated allergies.
Drug-Induced Asthma
Several pharmacologic agents provoke asthma, aspirin
being the most striking example. Individuals with aspirin
sensitivity present with recurrent rhinitis and nasal polyps,
urticaria, and bronchospasm. The precise mechanism
remains unknown.
Occupational Asthma
This form of asthma is stimulated by fumes (epoxy resins,
plastics), organic and chemical dusts (wood, cotton,
platinum), gases (toluene), and other chemicals. Asthma
attacks usually develop after repeated exposure to the
inciting antigen(s).
Morphology
In fatal cases, grossly, the lungs are overdistended because
of overinflation, and there may be small areas of
atelectasis. The most striking macroscopic finding is
occlusion of bronchi and bronchioles by thick, tenacious
mucus plugs. Histologically, the mucus plugs contain
whorls of shed epithelium (Curschmann spirals).
Numerous eosinophils and Charcot-Leyden crystals
(collections of crystalloids made up of eosinophil proteins)
are also present. The other characteristic findings of
asthma, collectively called "airway remodeling"
Thickening of the basement membrane of the bronchial
epithelium.Edema and an inflammatory infiltrate in the
bronchial walls, with a prominence of eosinophils and
mast cells.An increase in the size of the submucosal
glands.Hypertrophy of the bronchial muscle walls.
Bronchiectasis
Bronchiectasis is the permanent dilation of bronchi and
bronchioles caused by destruction of the muscle and
elastic supporting tissue, resulting from or associated with
chronic necrotizing infections. It is not a primary disease
but rather is secondary to persisting infection or
obstruction caused by a variety of conditions.
Predisposing Factors
Bronchial obstruction. by tumors, foreign bodies, and
occasionally impaction of mucus. Under these conditions,
the bronchiectasis is localized to the obstructed lung
segment. Bronchiectasis can also complicate atopic
asthma and chronic bronchitis.
Congenital or hereditary conditions. Like
In cystic fibrosis, widespread severe bronchiectasis
results from obstruction and infection caused by the
secretion of abnormally viscid mucus.
In immunodeficiency states, particularly
immunoglobulin deficiencies, bronchiectasis is likely to
develop because of an increased susceptibility to repeated
bacterial infections.
Kartagener syndrome, an autosomal recessive disorder,
is frequently associated with bronchiectasis and with
sterility in males. Structural abnormalities of the cilia
impair mucociliary clearance in the airways, leading to
persistent infections, and reduce the mobility of
spermatozoa.
Suppurative, pneumonia, due to Staphylococcus aureus
or Klebsiella spp., may predispose to bronchiectasis.
Pathogenesis
Two processes in the pathogenesis of bronchiectasis:
Obstruction and chronic persistent infection. Either of
these two processes may come first. Normal clearance
mechanisms are hampered by obstruction (by a
bronchogenic carcinoma or a foreign body), so secondary
infection soon follows; conversely, chronic infection in
time causes damage to bronchial walls, leading to
weakening and dilation.
Morphology
Bronchiectatic involvement of the lungs usually affects
the lower lobes bilaterally, When tumors or aspiration of
foreign bodies lead to bronchiectasis, involvement may be
sharply localized to a single segment of the lungs.
Usually, the most severe involvement is found in the more
distal bronchi and bronchioles. The airways may be
dilated to as much as four times their usual diameter.
The histologic findings vary with the activity and
chronicity of the disease. In the full-blown active case, an
intense acute and chronic inflammatory exudate
within the walls of the bronchi and bronchioles and the
desquamation of lining epithelium cause extensive areas
of ulceration.
In the usual case, a mixed flora can be cultured from the
involved bronchi, including staphylococci, streptococci,
pneumococci, .When healing occurs, the lining epithelium
may regenerate completely; however, usually so much injury
has occurred that abnormal dilation and scarring persist.
Fibrosis of the bronchial and bronchiolar walls and
peribronchiolar fibrosis develop in more chronic cases.
In some instances, the necrosis destroys the bronchial or
bronchiolar walls and forms a lung abscess
Unit 12: Lung (Diseases of respiratory system)
071
Pulmonary infections
Pneumonia defined as any infection in the lung. It may be
acute or chronic disease with a more protracted course.
Causes
Bacterial, viral, fungal, chemical…. .
Acute bacterial pneumonias can present as
bronchopneumonia or lobar pneumonia.
1) Bronchopneumonia implies a patchy distribution of
inflammation that generally involves more than one lobe,
results from an initial infection of the bronchi and
bronchioles with extension into the adjacent alveoli.
2) Lobar pneumonia the contiguous airspaces of part or all of
a lobe are homogeneously filled with an exudate that can
be visualized on radiographs as a lobar or segmental
consolidation. Streptococcus pneumoniae is responsible
for more than 90% of lobar pneumonias. Other
classification of pneumonias
1-base on specific etiologic agent
2-clinical setting if no pathogen can be isolated.
Community-Acquired Acute Pneumonias
Most community-acquired acute pneumonias are bacterial
in origin. Usually the infection follows a viral upper
respiratory tract infection. The onset is usually abrupt, with
high fever, chills, pleuritic chest pain, & a productive
mucopurulent cough; S. pneumoniae is the most common
cause of community-acquired acute pneumonia.
I-Streptococcus pneumoniae
Pneumococcal infections occur with increased frequency
in three groups of individuals:
1) Those with underlying chronic diseases such as CHF,
COPD, or diabetes.
2) Those with either congenital or acquired immunoglobulin
defects (e.g., the acquired immune deficiency syndrome).
3) Those with decreased or absent splenic function (e.g.,
sickle cell disease or after splenectomy). because the
spleen contains the largest collection of phagocytes & thus
responsible for removing pneumococci from the blood.
Morphology
With pneumococcal lung infection, it could be lobar or
bronchopneumonia, the latter is more prevalent at the
extremes of age. Regardless of the distribution of the
pneumonia, because pneumococcal lung infections usually
originate by aspiration of pharyngeal flora (20% of adults
harbor S. pneumoniae in their throats), the lower lobes or
the right middle lobe are most frequently involved.
In the era before antibiotics, pneumococcal pneumonia
involved entire or almost entire lobes and evolved through
four stages: congestion, red hepatization, gray
hepatization, and resolution. Early antibiotic therapy
alters this typical progression.
1) Congestion stage: in which the affected lobe heavy &
red. Histologically, vascular congestion can be seen, with
proteinaceous fluid, scattered neutrophils, and many
bacteria in the alveoli.
2) Red hepatization stage in which the lung lobe has a
liver-like consistency; the alveolar spaces are packed with
neutrophils, red cells, and fibrin.
3) Gray hepatization in this stage the lung is dry, gray, and
firm, because RBC are lysed, while the fibrinosuppurative
exudate persists within the alveoli.
4) Stage of Resolution follows in uncomplicated cases, as
exudates within the alveoli are enzymatically digested to
produce granular, semifluid debris that is resorbed,
ingested by macrophages, coughed up, or organized by
fibroblasts growing into it.
The pleural involvment (pleuritis) may resolve or
undergo organization, leaving fibrous thickening or
permanent adhesions
In the bronchopneumonic pattern, foci of inflammatory
consolidation are distributed in patches throughout one or
more lobes, most frequently bilateral and basal. Well-
developed lesions up to 3 - 4 cm in diameter are slightly
elevated and are gray-red to yellow. The lung tissues
surrounding areas of consolidation is usually hyperemic
and edematous& Pleural involvement is less common
than in lobar pneumonia.
Histologically, the lesion consists of focal suppurative
exudate that fills the bronchi, bronchioles, and adjacent
alveolar spaces.
Complications:
1) Abscess due to tissue destruction and necrosis .
2) Empyema when pus accumulate in the pleural cavity.
3) Organization of the intra-alveolar exudate may convert
areas of the lung into solid fibrous tissue;
4) bacteremic dissemination may lead to meningitis,
arthritis, or infective endocarditis. Complications are
much more likely with serotype 3 pneumococci
Diagnosis
1) Gram-stained sputum is an important step in the diagnosis
of acute pneumonia. Looking for neutrophils containing
the typical gram-positive diplococci is good evidence of
pneumococcal pneumonia, but as S. pneumoniae is an
endogenous flora and therefore false-positive results may
be obtained by this method.
Unit 12: Lung (Diseases of respiratory system)
071
2) Blood cultures is more specific. During early phases of
illness, blood cultures may be positive in 20% to 30% of
persons with pneumonia.
II-Haemophilus influenzae
It can cause a life-threatening form of pneumonia in
children, often following a respiratory viral infection.
Adults at risk are those with chronic pulmonary diseases
such as chronic bronchitis, cystic fibrosis, and
bronchiectasis.
.Encapsulated H. influenzae type b was an important
cause of epiglottitis and suppurative meningitis in
children, & vaccination against this organism in infancy
has significantly reduced the risk.
III-Staphylococcus aureus
It is an important cause of secondary bacterial pneumonia
in children and healthy adults after viral respiratory
illnesses (e.g., measles in children and influenza in both
children & adults).Staphylococcal pneumonia is associated
with a high incidence of complications, such as lung
abscess and empyema.Staphylococcal pneumonia occurring
in association with right-sided staphylococcal endocarditis
is a serious complication of intravenous drug abuse. It is
also an important cause of nosocomial pneumonia
IV-Klebsiella pneumoniae
K. pneumoniae is the most frequent cause of gram-
negative bacterial pneumonia.It frequently Affect
debilitated and malnourished persons, particularly chronic
alcoholics.Thick and gelatinous sputum is characteristic,
because the organism produces an abundant viscid
capsular polysaccharide.
Hospital-Acquired Pneumonias (Nasocomial
pneumonia)
Nosocomial or hospital-acquired, pneumonias are defined as
pulmonary infections acquired in the course of a hospital
stay. Nosocomial infections are common in hospitalized
persons with severe underlying disease, immune
suppression, or prolonged antibiotic therapy. Those on
mechanical ventilation are at high-risk. Gram-negative rods
(Enterobacteriaceae and Pseudomonas spp.) & S. aureus are
the most common isolates; while, S. pneumoniae is not a
major pathogen in nosocomial infections
Aspiration Pneumonia
Aspiration pneumonia occurs in markedly debilitated
patients or those who aspirate gastric contents either while
unconscious (e.g., after a stroke) or during repeated
vomiting. These individuals have abnormal gag and
swallowing reflexes that facilitate aspiration. The
resultant pneumonia is partly chemical, resulting from the
extremely irritating effects of the gastric acid, and partly
bacterial recent studies implicate aerobes more commonly
than anaerobes. This type of pneumonia is often
necrotizing, with a fulminant clinical course, and is a
frequent cause of death in persons predisposed to
aspiration & abscess formation is a common complication
Lung Abscess
Lung abscess refers to a localized area of suppurative
necrosis within the pulmonary parenchyma, resulting in
the formation of large cavity. The term necrotizing
pneumonia has been used for a similar process resulting in
multiple small cavitations; necrotizing pneumonia often
coexists or evolves into lung abscess, The causative
organism may be introduced into the lung by any of the
following mechanisms
1) Aspiration of infective material from carious teeth or
infected sinuses or tonsils, particularly likely during oral
surgery, anesthesia, coma, or alcoholic intoxication and in
debilitated patients with depressed cough reflexes.
2) Aspiration of gastric contents, usually accompanied by
infectious organisms from the oropharynx.
3) As a complication of necrotizing bacterial pneumonias,
particularly those caused by S. aureus, Streptococcus
pyogenes, K. pneumoniae, Pseudomonas spp., and, rarely,
type 3 pneumococci. Mycotic infections and
bronchiectasis may also lead to lung abscesses.
4) Bronchial obstruction, particularly with bronchogenic
carcinoma obstructing a bronchus or bronchiole. Impaired
drainage, distal atelectasis, and aspiration of blood and
tumor fragments all contribute to the development of
abscesses. An abscess may also form within an excavated
necrotic portion of a tumor.
5) Septic embolism, from septic thrombophlebitis or from
infective endocarditis of the right side of the heart.In
addition, lung abscesses may result from hematogenous
spread of bacteria in disseminated pyogenic infection e.g.
staphylococcal bacteremia which results in multiple lung
abscesses.
Anaerobic bacteria are present in almost all lung
abscesses e.g. Bacteroides& microaerophilic streptococci.
Morphology
Abscesses vary in diameter from a few millimeters to large
cavities of 5 to 6 cm. The localization and number of
Unit 12: Lung (Diseases of respiratory system)
077
abscesses depend on their mode of development.
Pulmonary abscesses resulting from aspiration of infective
material are much more common on the right side (more
vertical airways) than on the left, and most are single. On
the right side, they tend to occur in the posterior segment of
the upper lobe and in the apical segments of the lower lobe,
because these locations reflect the probable course of
aspirated material when the patient is recumbent.
Abscesses that develop in the course of pneumonia or
bronchiectasis are commonly multiple, basal, and
diffusely scattered.
abscesses arising from hematogenous seeding or Septic
emboli are commonly multiple and may affect any region
of the lungs.
As the focus of suppuration enlarges, it almost inevitably
ruptures into airways. Thus, the contained exudate may be
partially drained, producing an air-fluid level on
radiographic examination. Occasionally, abscesses
rupture into the pleural cavity and produce bronchopleural
fistulas, the consequence of which is pneumothorax or
empyema. Other complications arise from embolization
of septic material to the brain, giving rise to meningitis or
brain abscess.
Histologically there is suppuration surrounded by variable
amounts of fibrous scarring and mononuclear infiltration
(lymphocytes, plasma cells, macrophages), depending on
the chronicity of the lesion.
Lung tumors
Primary lung cancer is a common disease. Bronchial
epithelium is the site of origin of 95% of primary lung
tumors (carcinomas); the remaining 5% includes
bronchial carcinoids, mesenchymal malignancies (e.g.,
fibrosarcomas, leiomyomas), lymphomas, and a few
benign lesions.
The most common benign lesions are Hamartomas:-
Spherical, small (3-4 cm), discrete that often show up as
"coin" lesions on chest radiographs. They consist mainly
of mature cartilage but are often admixed with fat, fibrous
tissue, and blood vessels in varying proportions.
Carcinoma
Lung cancer is the number one cause of cancer-related
deaths in industrialized countries. In either sex. These
statistics are related to the causal relationship of cigarette
smoking and lung cancer.
The peak incidence of lung cancer occurs in persons in
their 50s and 60s. The 5-year survival rate for all stages of
lung cancer combined is about 15%; even those with
disease localized to the lung have a 5-year survival of
approximately 45%.
Histologic types:-
The four major histologic types of carcinomas of the lung
are squamous cell carcinoma, adenocarcinoma, small-cell
carcinoma, and large-cell carcinoma. In some cases there
is a combination of histologic patterns (e.g., combined
small-cell carcinoma, adenosquamous carcinoma).
Adenocarcinoma has replaced squamous cell carcinoma
as the most common primary lung tumor in recent years.
For therapeutic purposes, carcinomas of the lung are
classified into two broad groups:
1-small-cell lung cancer (SCLC)
2-non-small-cell lung cancer (NSCLC) which includes
squamous cell, adenocarcinomas, and large-cell
carcinomas. The reason is that all SCLCs have
metastasized by the time of diagnosis and are not curable
by surgery. Therefore, they are best treated by
chemotherapy, with or without radiation. In contrast,
NSCLCs usually respond poorly to chemotherapy and are
better treated by surgery, there are also genetic differences
between SCLCs and NSCLCs. For example, SCLCs are
characterized by a high frequency of RB gene mutations,
while activating KRAS and EGFR oncogene mutations are
restricted to adenocarcinomas within the NSCLC group
and are rare in SCLCs.
Etiology and Pathogenesis
Carcinomas of the lung arise by accumulation of genetic
abnormalities that result in transformation of benign
bronchial epithelium into neoplastic tissue. The sequence
of molecular changes start by inactivation of the tumor
suppressor genes located on chromosome 3p as an early
event, whereas p53 mutations or activation of the KRAS
oncogene occurs relatively late. Loss of chromosome 3p
material, can be found even in benign bronchial
epithelium of individuals with lung cancer, as well as in
the respiratory epithelium of smokers without lung
cancers, suggesting that large areas of the respiratory
mucosa are mutagenized after exposure to carcinogens.
On this fertile soil, those cells that accumulate additional
mutations ultimately develop into cancer.
Statistically, about 90% of lung cancers occur in active
smokers or those who stopped recently. The increased risk
becomes 60 times greater among habitual heavy smokers
(two packs a day for 20 years) compared with nonsmokers.
Women have a higher susceptibility to carcinogens in
tobacco than men. Cessation of smoking decreases the risk
Unit 12: Lung (Diseases of respiratory system)
071
of developing lung cancer over time but it may never
return to baseline levels. Passive smoking (proximity to
cigarette smokers) increases the risk of developing lung
cancer to approximately twice that of nonsmokers.
The smoking of pipes and cigars also increases the risk,
but only modestly.
It is well known that not all persons exposed to tobacco
smoke develop cancer. It is very likely that the mutagenic
effect of carcinogens is conditioned by hereditary (genetic)
factors. Recall that many chemicals (procarcinogens)
require metabolic activation via the P-450 monooxygenase
enzyme system for conversion into ultimate carcinogens.
There is evidence that persons with specific genetic
polymorphisms involving the P-450 genes have an
increased capacity to metabolize procarcinogens derived
from cigarette smoke and, conceivably, incur the greatest
risk of developing lung cancer.
Morphology
Carcinomas of the lung begin as small mucosal lesions
that are usually firm and gray-white. They may form
intraluminal masses, invade the bronchial mucosa, or
form large bulky masses pushing into adjacent lung
parenchyma. Some large masses undergo cavitation
caused by central necrosis or develop focal areas of
hemorrhage. Finally, these tumors may extend to the
pleura, invade the pleural cavity and chest wall, & spread
to adjacent intrathoracic structures. More distant spread
can occur via the lymphatics or the hematogenous route.
Squamous cell carcinomas
are more common in men
than in women and are closely correlated with a smoking
history; they tend to arise centrally in major bronchi and
eventually spread to local hilar nodes, but they disseminate
outside the thorax later than other histologic types. Large
lesions may undergo central necrosis, giving rise to
cavitation. Squamous cell carcinomas are often preceded
for years by squamous metaplasia or dysplasia in the
bronchial epithelium, which then transforms to carcinoma
in situ, a phase that may last for several years. By this time,
atypical cells may be identified in cytologic smears of
sputum or in bronchial lavage fluids or brushings, although
the lesion is asymptomatic and undetectable on
radiographs. Eventually, the small neoplasm reaches a
symptomatic stage, when a well-defined tumor mass begins
to obstruct the lumen of a major bronchus, often producing
distal atelectasis and infection. Simultaneously, the lesion
invades surrounding pulmonary substance. Histologically,
these tumors range from well-differentiated squamous cell
neoplasms showing keratin pearls and intercellular bridges
to poorly differentiated neoplasms having only minimal
residual squamous cell features.
Adenocarcinomas
are usually more peripherally
located, many arising in relation to peripheral lung scars
(“scar carcinomas”). Adenocarcinomas are the most
common type of lung cancer in women and nonsmokers. It
grow slowly and form smaller masses than do the other
subtypes, but they tend to metastasize widely at an early
stage
Histologically, they assume a variety of forms, including
acinar (gland forming), papillary
, and
solid types
. The
putative precursor of peripheral adenocarcinomas has
been described as atypical adenomatous hyperplasia
(AAH). Microscopically, AAH is recognized as a well-
demarcated focus of epithelial proliferation composed of
cuboidal to low-columnar cells with various degrees of
cytologic atypia (nuclear hyperchromasia, pleomorphism,
prominent nucleoli). Genetic analyses of AAH show
many of the molecular aberrations associated with
adenocarcinomas (e.g., KRAS mutations).
Bronchioloalveolar carcinomas (BACs)
They
involve peripheral parts of the lung, either as a single
nodule or, more often, as multiple diffuse nodules that
may coalesce to produce pneumonia-like consolidation.
The key feature of BACs is their growth along
preexisting structures and preservation of alveolar
architecture. The two subtypes of BACs are mucinous
and nonmucinous, with the former comprising tall,
columnar cells with prominent cytoplasmic and intra-
alveolar mucin. it is proposed that some invasive
adenocarcinomas of the lung may arise through an
atypical adenomatous hyperplasia-bronchioloalveolar
carcinoma-invasive adenocarcinoma sequence.
Large-cell carcinomas
are undifferentiated malignant
epithelial tumors that lack the cytologic features of small-
cell carcinoma and glandular or squamous differentiation.
The cells typically have large nuclei, prominent nucleoli,
and a moderate amount of cytoplasm. Large-cell
carcinomas probably represent squamous cell or
adenocarcinomas that are so undifferentiated that they can
no longer be recognized by light microscopy.
Ultrastructurally, however, minimal glandular or
squamous differentiation is common
Small-cell lung carcinomas
generally appear as pale
gray, centrally located masses with extension into the
lung parenchyma and early involvement of the hilar and
mediastinal nodes. These cancers are composed of tumor
Unit 12: Lung (Diseases of respiratory system)
071
cells with a round to fusiform shape, scant cytoplasm, and
finely granular chromatin. Mitotic figures are frequently
seen, " the neoplastic cells are usually twice the size of
resting lymphocytes. Necrosis is invariably present and
may be extensive. The tumor cells are markedly fragile
and often show fragmentation and "crush artifact" in
small biopsy specimens. Another feature of small-cell
carcinomas, best appreciated in cytologic specimens, is
nuclear molding resulting from close apposition of tumor
cells that have scant cytoplasm. These tumors are derived
from neuroendocrine cells of the lung, and hence they
express a variety of neuroendocrine markers in addition
to a host of polypeptide hormones that may result in
paraneoplastic syndromes.
Clinical course
Carcinomas of the lung are silent, insidious lesions In
some instances, chronic cough and expectoration call
attention to still localized, resectable disease. By the time
hoarseness, chest pain, superior vena caval syndrome,
pericardial or pleural effusion, or persistent segmental
atelectasis or pneumonitis makes its appearance, the
prognosis is grim. Too often, the tumor presents with
symptoms emanating from metastatic spread to the brain
(mental or neurologic changes), liver (hepatomegaly), or
bones (pain). Although the adrenals may be nearly
obliterated by metastatic disease, adrenal insufficiency
(Addison disease) is uncommon because islands of
cortical cells sufficient to maintain adrenal function
usually persist. Overall, NSCLCs have a better prognosis
than SCLCs. When NSCLCs (squamous cell carcinomas
or adenocarcinomas) are detected before metastasis or
local spread, cure is possible by lobectomy or
pneumonectomy. SCLCs, on the other hand, have
invariably spread by the time they are first detected, even
if the primary tumor appears small and localized. Thus,
surgical resection is not a viable treatment. They are very
sensitive to chemotherapy but invariably recur. Median
survival even with treatment is 1 year. It is variously
estimated that 3% to 10% of all patients with lung cancer
develop clinically overt paraneoplastic syndromes. These
include
1) Hypercalcemia caused by secretion of a parathyroid
hormone-related peptide (osteolytic lesions may also
cause hypercalcemia, but this would not be a
paraneoplastic syndrome;
2) Cushing syndrome (from increased production of
adrenocorticotropic hormone);
3) syndrome of inappropriate secretion of antidiuretic hormone
4) Neuromuscular syndromes, including a myasthenic
syndrome, peripheral neuropathy, and polymyositis;
5) Clubbing of the fingers and hypertrophic pulmonary
osteoarthropathy; and
6) Hematologic manifestations, including migratory
thrombophlebitis, nonbacterial endocarditis, and
disseminated intravascular coagulation. Secretion of
calcitonin and other ectopic hormones has also been
documented. Hypercalcemia is most often encountered
with squamous cell neoplasms, the hematologic
syndromes with adenocarcinomas. The remaining
syndromes are much more common with small-cell
neoplasms, but exceptions abound.
Carcinoids
Bronchial carcinoids are thought to arise from the
Kulchitsky cells (neuroendocrine cells) that line the
bronchial mucosa and resemble intestinal carcinoids. The
neoplastic cells contain dense-core neurosecretory
granules in their cytoplasm and, may secrete hormonally
active polypeptides. They occasionally occur as part of
the multiple endocrine neoplasia syndrome. Bronchial
carcinoids appear at an early age (mean 40 years) and
represent about 5% of all pulmonary neoplasms. In happy
contrast to their more ominous neuroendocrine
counterpart, small-cell carcinomas, carcinoids are often
resectable and curable.
Morphology
Most bronchial carcinoids originate in main-stem bronchi
and grow in one of two patterns: (1) an obstructing
polypoid, spherical, intraluminal mass; or (2) a mucosal
plaque penetrating the bronchial wall.About 5% -15% of
these tumors have metastasized to the hilar nodes at
presentation, distant metastasis is rare.
Histologically, these neoplasms are composed of nests of
uniform cells that have regular round nuclei with "salt-
and-pepper" chromatin, absent or rare mitoses, and little
pleomorphism.
Atypical carcinoid tumors display a higher mitotic rate,
increased cytologic variability, and focal necrosis. & have
a higher incidence of lymph node and distant metastasis
than "typical" carcinoids, and understandably persons
with atypical carcinoids fare worse in the long run with
p53 mutations in 20% to 40% of cases.
