BLOOD LIPOPROTEINS
● Lipids absorbed from diet (exogenous) and lipids synthesized in the
body (endogenous) are transported in the blood between the various
tissues for oxidation or storage as lipoproteins .
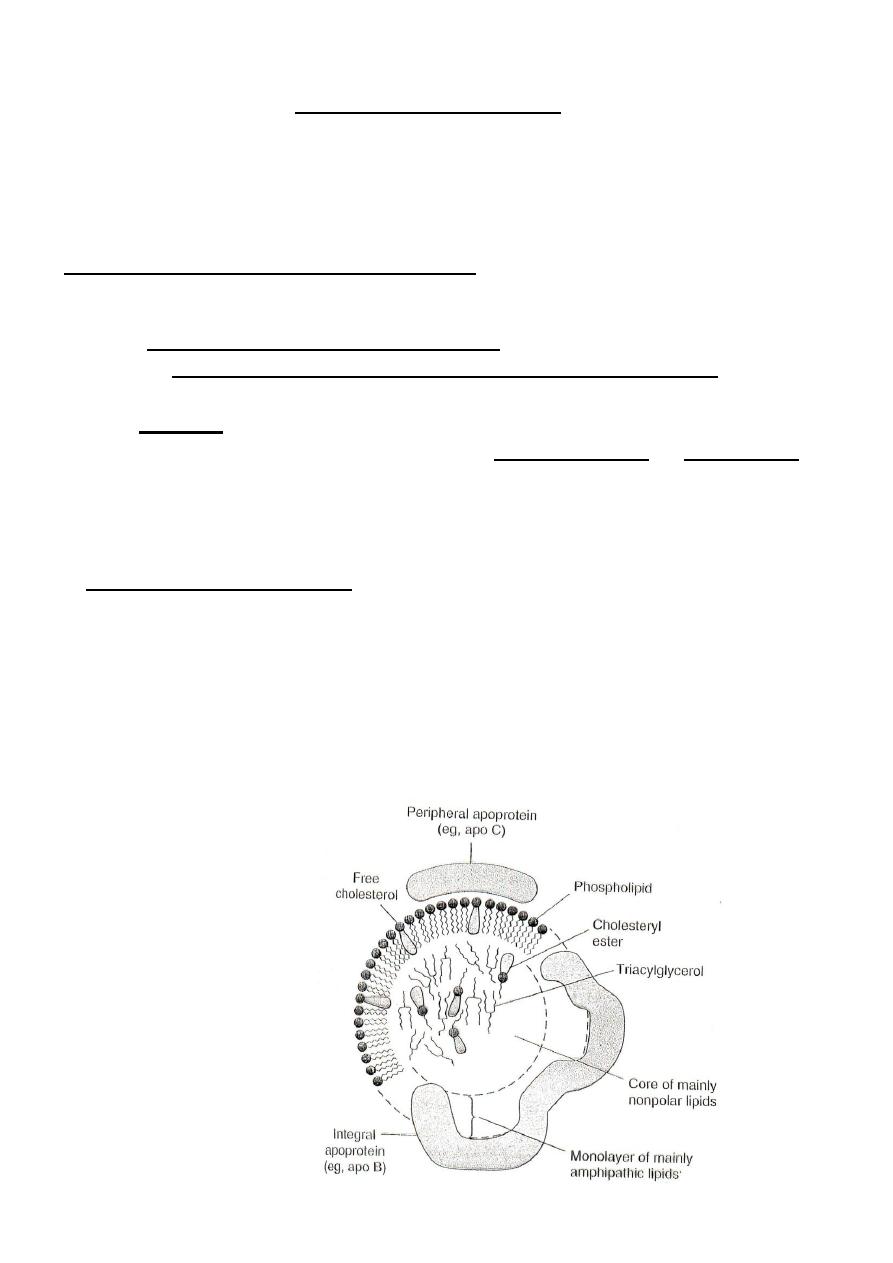
General Structure of Lipoprotein (LP) :
● Lipoprotein molecule in general consists of a non-polar inner core made
up of triglycerides and cholesterol esters surrounded by a single surface
layer of amphipathic phospholipids and cholesterol molecules with their
polar heads facing outward to the aqueous medium and then complexed
with proteins .
● The protein part of lipoprotein is called apolipoprotein or apoprotein .
One or more apoprotein are present in each lipoprotein ; some are
integral and essential for lipoprotein formation while others are
peripheral and free to transfer from one type of lipoprotein into another .
Functions of apoproteins :
1. all apoproteins function in making lipid particles water-soluble .
2. some form integral part of the structure of lipoprotein .
3. some act as activators or inhibitors of enzymes involved in
lipoprotein metabolism .
4. others act as ligand for binding receptors in cell membranes of
tissues mediating the uptake of lipoproteins by tissues .
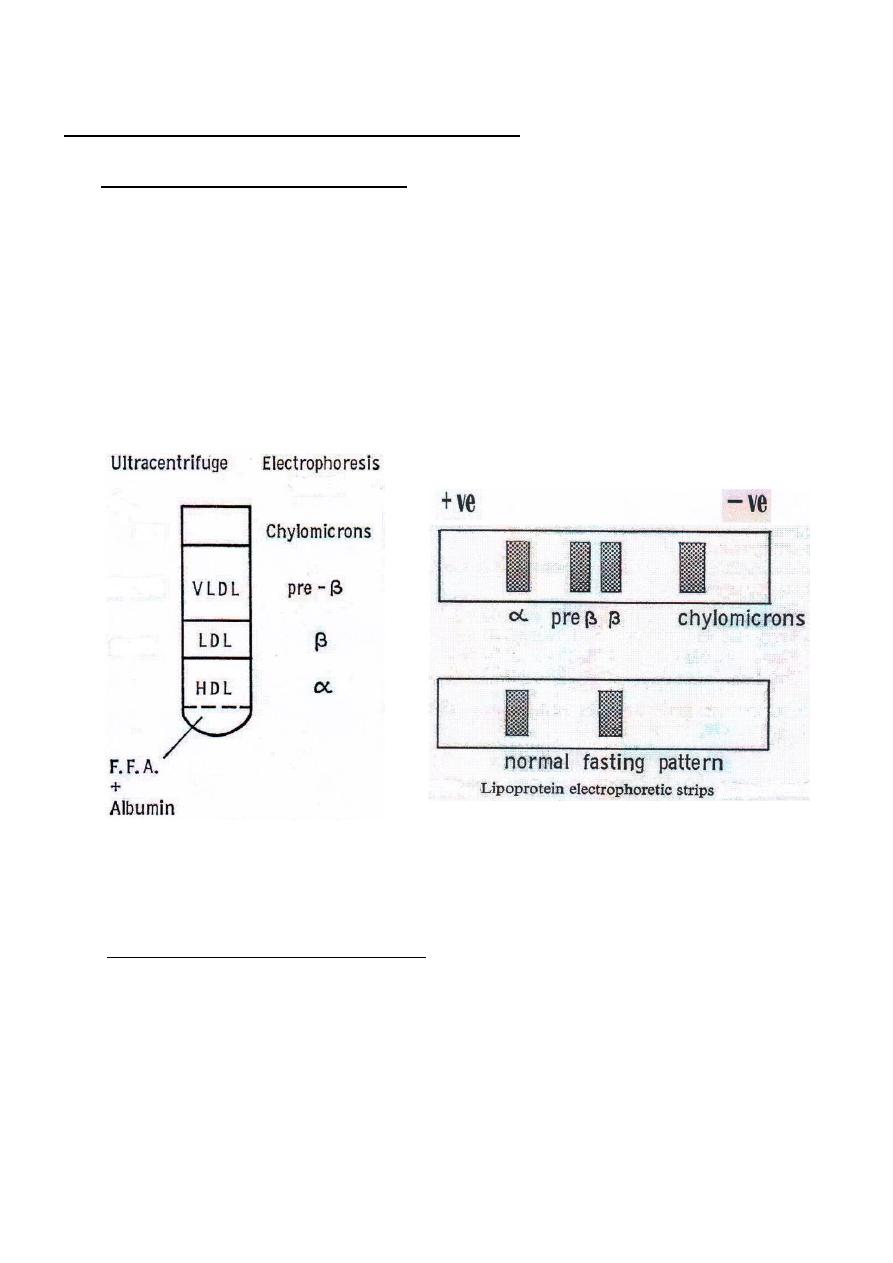
Separation & Classification of Lipoproteins :
A
–
Separation by Centrifugation :
● plasma lipoproteins are separated depending on their density by
high-speed centrifugation into four major classes :
I - Chylomicrons .
II - Very low density lipoprotein (VLDL)
III - Low density lipoprotein (LDL) .
IV - High density lipoprotein ( HDL ) .
●
lipoproteins with high lipid content have low density and float on
centrifugation whereas lipoproteins with high protein content have
high density and sediment easily .
● Free fatty acids ( FFA ) are transported in plasma combined to
albumin ; is not classified as lipoprotein but is metabolically most
active .
B – Separation by Electrophoresis:
Apoproteins are charged particles and therefore lipoproteins can be
separated by electrophoresis into 4 major classes depending on the
amount and nature of apoproteins:
I-
Chylomicrons .
II-
β –lipoprotein : corresponds to LDL .
III-
pre-
β-lipoprotein : corresponds to VLDL .
IV-
α –lipoprotein : corresponds to HDL .
● Free fatty acids move faster towards the anode .
LIPOPROTEIN METABOLISM
Chylomicron metabolism ( exogenous lipid cycle )
:
● Chylomicrons are synthesized by the intestinal cells from exogenous
lipids ; are secreted into the chyle of the lymphatic system and enter the
blood via the thoracic duct .
● Chylomicron metabolism represent exogenous lipid cycle and function
in the transport of the exogenous lipids (mainly triglycerides) into
tissues for metabolism .
● Chylomicrons begin to enter the blood within 1-2 hours after the start of
a meal and continue to enter the blood for many hours .
● Newly formed chylomicrons are called nascent chylomicrons and are
rich in exogenous triglycerides ( 90% ) , therefore are the least dense of
the lipoproteins , and contain only the apoproteins apo B & apo-A ;
both synthesized by the intestinal cells .
● Nascent chylomicrons accepts apoproteins particularly apo-E & apo-C
from lipoprotein- HDL within the lymph and blood and they become
"mature" chylomicrons .
● The main sites of chylomicron metabolism are adipose tissue and
muscles ( skeletal & cardiac ) . The triglycerides of chylomicrons are
hydrolyzed into fatty acids and glycerol by the enzyme lipoprotein
lipase (LpL) located in the membranes of the capillary endothelial cells
in these tissues .
- In adipose tissue , the fatty acids released are re-esterified and
stored as triglycerides .
- In muscles and other tissues , the fatty acids are oxidized for energy .
● Normally , half-life of chylomicrons in blood is about one hour ; about
90% of triglycerides in chylomicrons are metabolized by extrahepatic
tissues and so they shrink in size and the portion of a chylomicron that
remains in the blood after LpL action is known as chylomicron
remnants which are rich in cholesterol ( free + esterified ) and contain
only apo B and apo-E . The other apoproteins ( apo-A & apo-C ) are
transferred to HDL .
● Chylomicron remnants bind to receptors on hepatocytes (mediated by
apo-E ) and the remnants are taken up by the process of endocytosis .
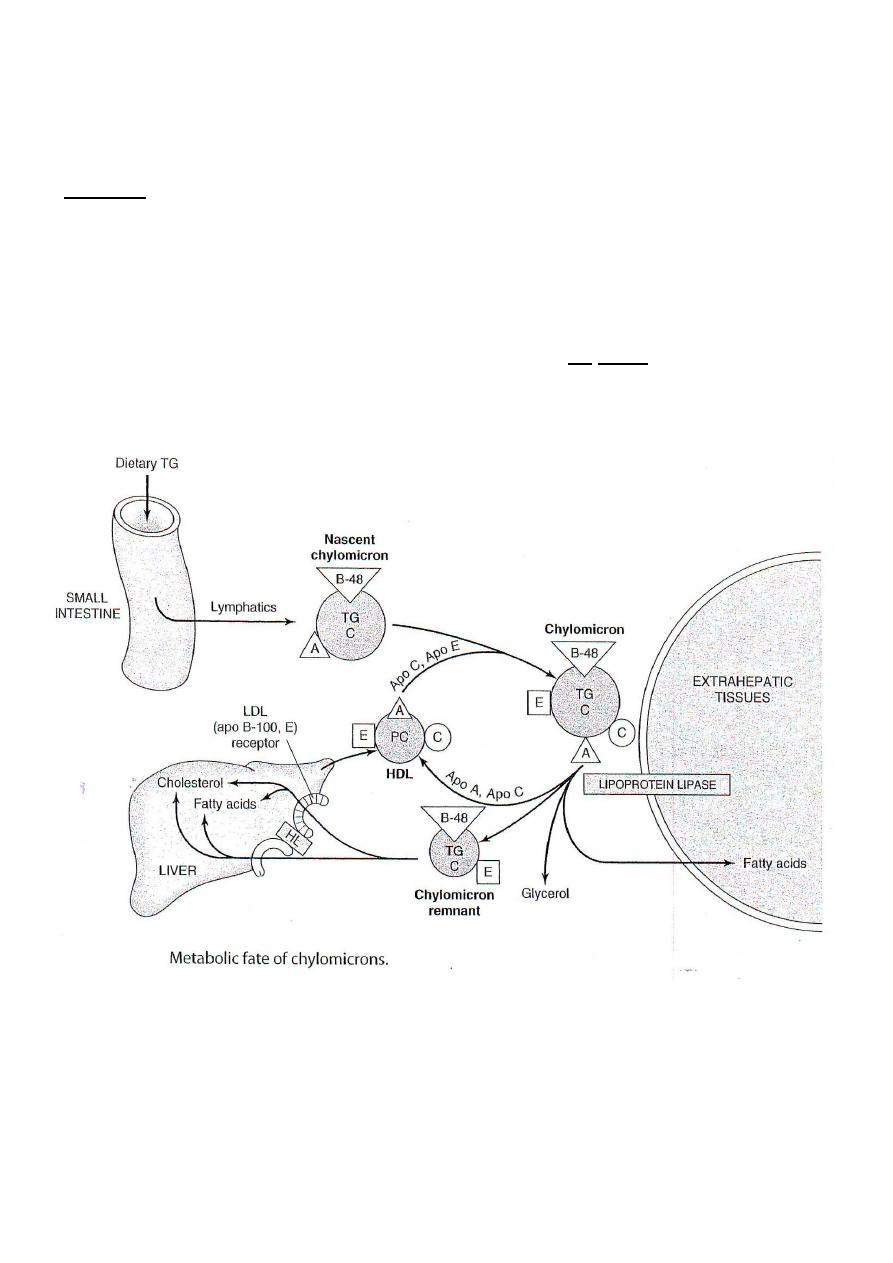
The proteins and lipids of the remnants are degraded by lysosomal
enzymes .
Notes :
1. Apo-C activates LpL ; lack of apo-C results in slow clearance of
chylomicrons from circulation .
2. The enzyme LpL is absent from liver so mature chylomicrons are not
metabolized by liver .
3. Chylomicron cholesterol is mostly delivered to liver . The resultant
increase of the free cholesterol pool inhibits de novo synthesis of
cholesterol .
***************************************
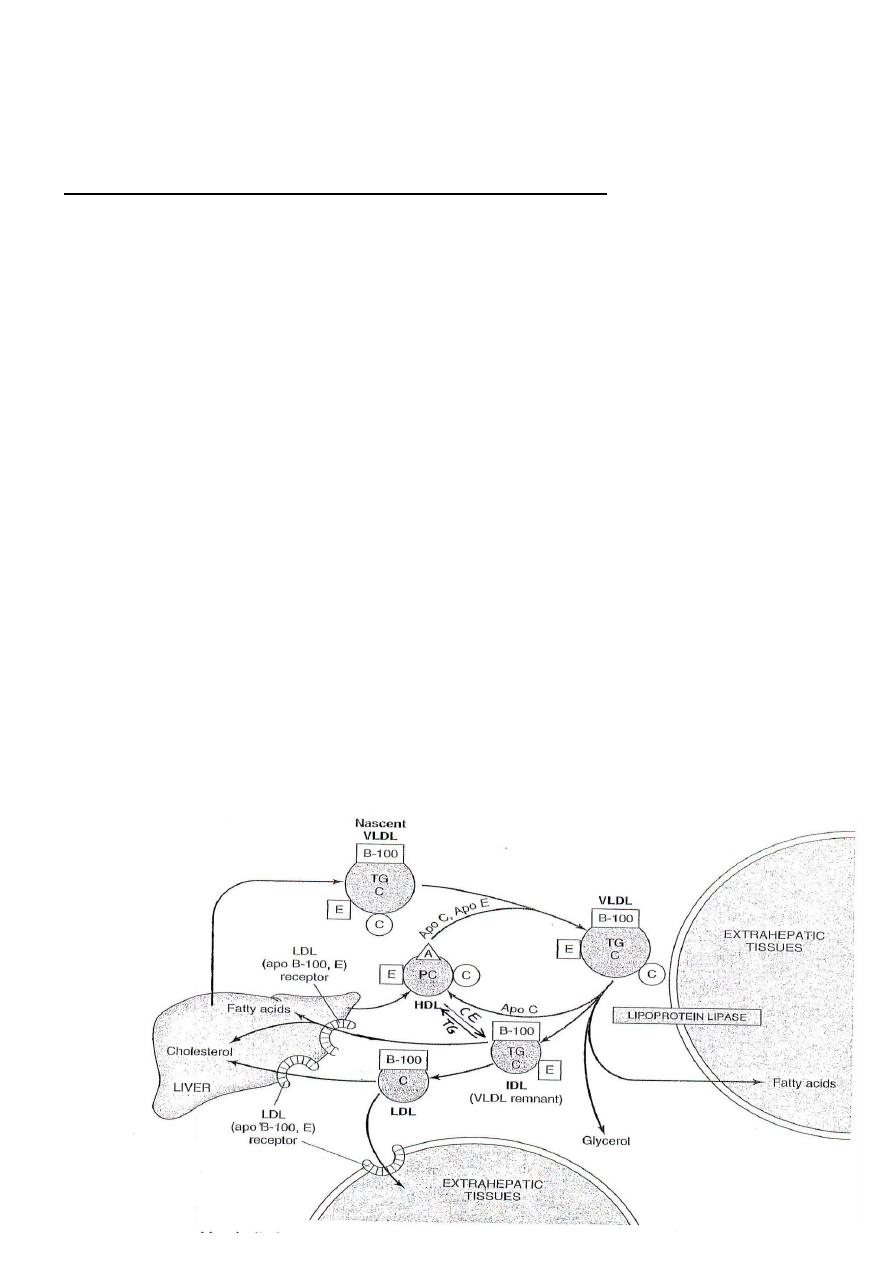
Metabolism of VLDL( Endogenous lipid cycle ) :
● Endogenous triglycerides synthesized in the liver are packaged with
cholesterol , phospholipids , and proteins to form VLDL .
● The major apoprotein of VLDL is apo B-100 (also synthesized in the
liver) ; there is one long apo B-100 molecule for each VLDL particle .
● VLDL are secreted by the liver into circulation and function in the
transport of endogenous triglycerides into peripheral tissues ( mainly
adipose & muscle ) .
● VLDL accepts apo-C and apo-E from HDL in the blood .
● In peripheral tissues , the enzyme LpL hydrolyzes the triglycerides in
VLDL and the fatty acids released to be stored or oxidized for energy .
fatty acids of VLDL are mainly esterified and stored in adipose tissue.
● As the triglyceride content of VLDL decreases by LpL digestion , apo-C
returns to HDL and the VLDL is converted to intermediate density
lipoprotein (IDL) . There are two possible fates for IDL:
(a) - may return to the liver and degraded by lysosomal enzymes .
(b) - major fraction of IDL transfers apo-E and triglycerides to HDL
in exchange for cholesterol ( esterified ) and in this way IDL is
converted to low density lipoprotein ( LDL ) .
● Most of the cholesterol secreted by liver in VLDL is retained in IDL and
ultimately in LDL .

( Metabolism of VLDL and production of LDL )
Notes :
1. The LpL in the capillaries of muscle cells has higher affinity for
triglycerides thus muscle cells can obtain fatty acids from the blood
lipoproteins, chylomicrons and VLDL , as a source of energy even
when the blood concentrations of these lipoproteins are low .
2. The LpL in adipose tissue has low affinity for triglycerides and is
most active only following a meal when blood levels of chylomicrons
& VLDL are elevated .
*******************************************
Metabolism of low density lipoproteins ( LDL ) :
● LDL are cholesterol rich lipoproteins containing only apo B-100 and
derived mostly from VLDL .
● LDL function in the transport of cholesterol mainly from liver into
peripheral tissues .
* About 75% of plasma cholesterol ( mostly esterified ) is present in LDL
and is of two origins :
a - cholesterol ( free & esterified ) secreted by liver in VLDL and
retained during formation of LDL .
b - cholesterol ( esterified ) obtained from HDL in exchange for
triglycerides .
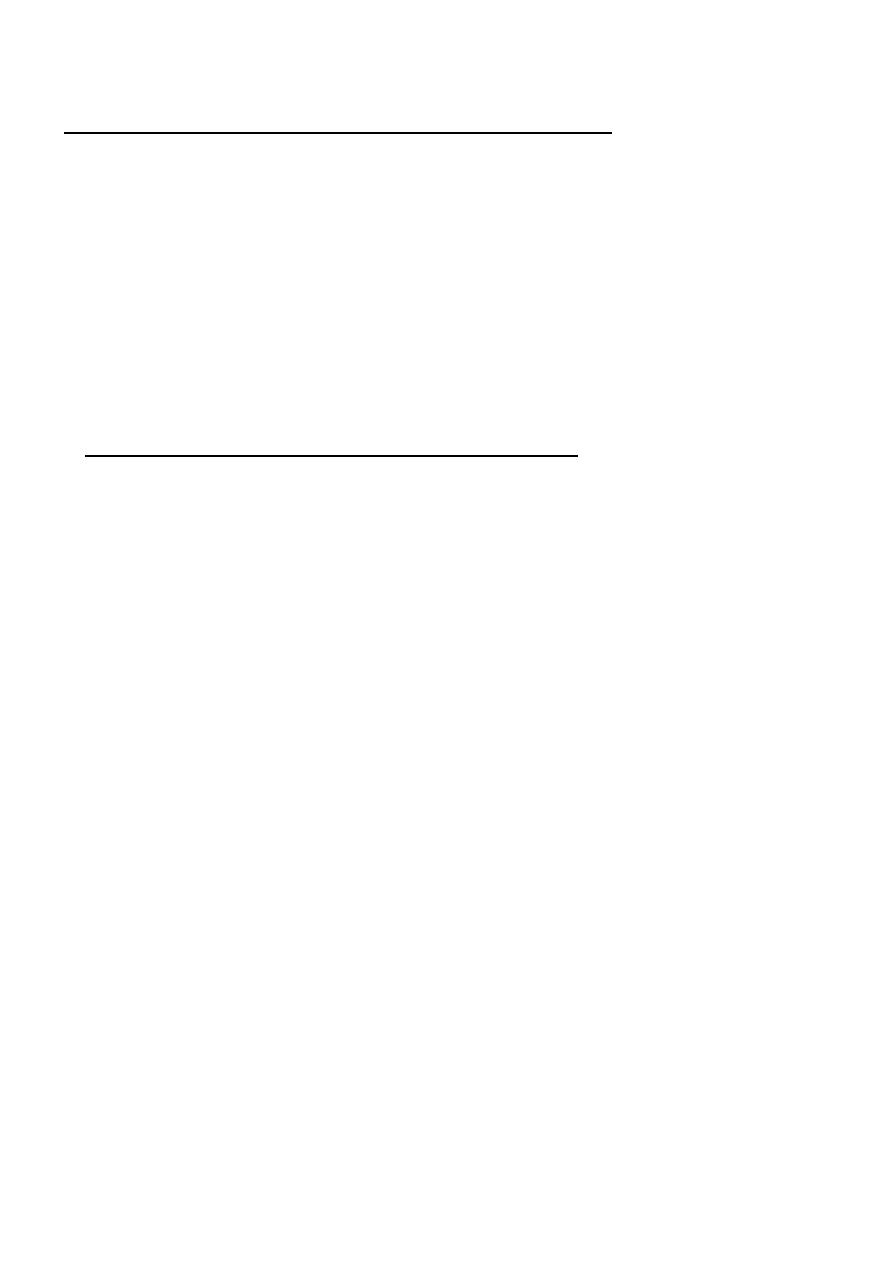
LDL internalization into cells by LDL receptors :
●
LDL
particles are taken up by tissues by the process of endocytosis
mediated by LDL receptors located on the cell membranes which bind
the apoproteins of LDL ( apo B-100 & apo-E ) .
* hepatic cells and the cells of adrenal cortex contain the highest number
of LDL receptors .
● Inside the cells , LDL particles are digested by lysosomal enzymes and
the free cholesterol released within the cells has the following fates :
1. incorporated into cell membrane to maintain stability .
2. used in the synthesis of steroid hormones specially in adrenal cortex
and gonads .
3. re-esterified , for storage in the cell , catalyzed by the enzyme
Acyl CoA-Cholesterol Acyl Transferase
(
ACAT
)
which uses
monounsaturated or saturated fatty acids for esterification .
4. removed from the cell and esterified by the enzyme
Lecithin-Cholesterol- Acyl Transferase ( LCAT ) and transported to
liver and excreted .
● high intracellular free cholesterol level depress synthesis of LDL
receptor protein . This mechanism is called down-regulation of receptor
synthesis .
● Liver controls the plasma levels of LDL cholesterol since :
a- LDL receptors are present in highest concentration in hepatic cells ;
70% of LDL is degraded in liver and 30% in extrahepatic tissues .
b- the liver is the only organ that can excrete cholesterol through bile
and also converts cholesterol to bile acids .
[ LDL internalization and fate of cholesterol within the cell ]
Mechanism of action of Statin drugs :
Statin drugs inhibit the enzyme HMG-CoA reductase and decreases
the rate of synthesis of cholesterol in cells . As cellular cholesterol level
decrease , the synthesis of LDL receptors increase and thus the uptake of
LDL by cells is increased and consequently the blood cholesterol level
decreases .
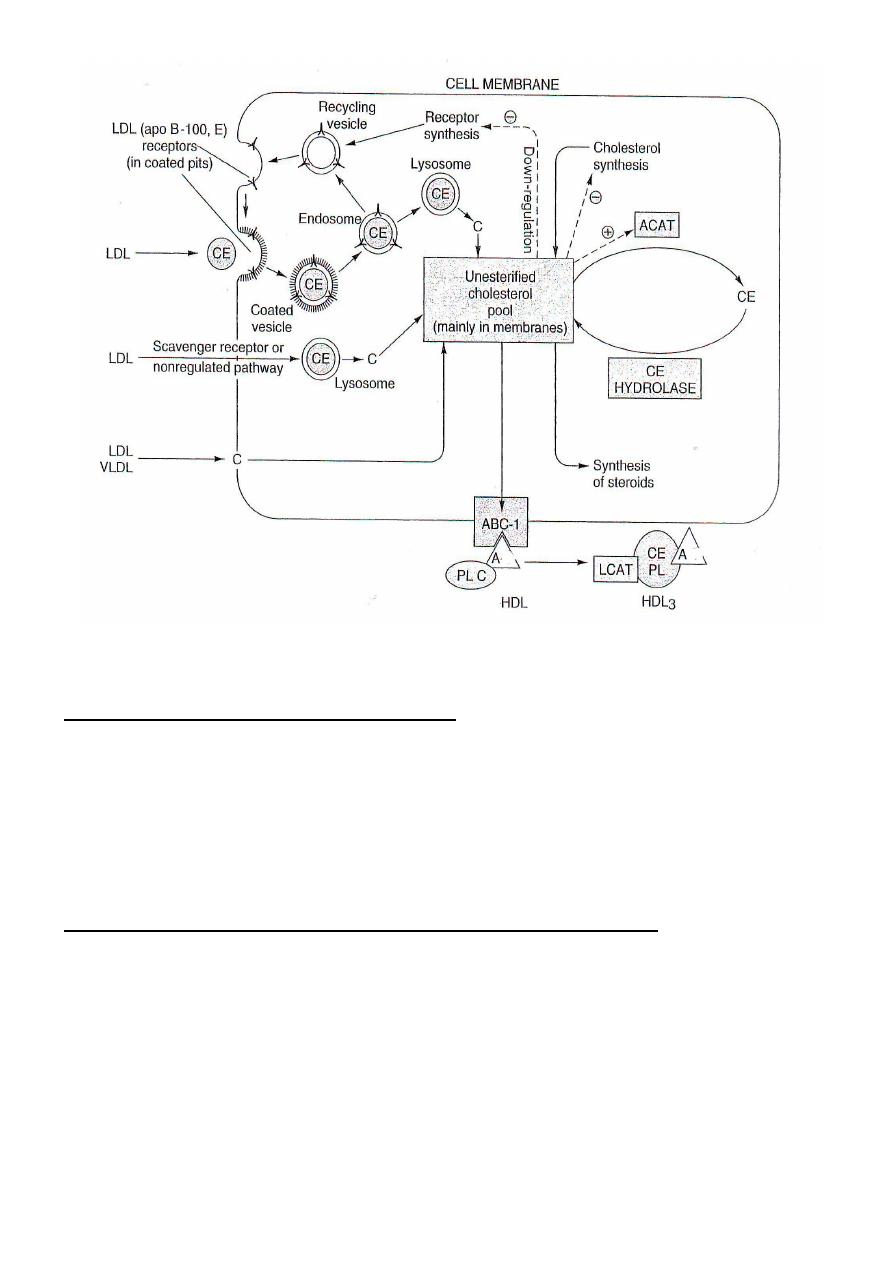
Macrophage Scavenger Receptor for LDL internalization :
●Macrophages have nonspecific receptors called ″scavenger receptors″
that bind various types of molecules including oxidized LDL particles .
* LDL particles are oxidized by reactive oxygen species ( O
2
•
, NO
•
, &
H
2
O
2
) ; percentage of oxidized LDL increases as the concentration of
LDL in blood rises .
●Scavenger receptors are not subject to down regulation ; this allows
macrophages to take up oxidized LDL continuously .
● As macrophages become filled with lipid ( LDL ) they are called foam
cells .
● When the endothelial cells of the artery wall are injured , foam cells
accumulate in the subendothelial space of blood vessels . This forms
the earliest sign of a developing atherosclerotic plaque known as a
fatty streak ; this is the basis of atheroseclorosis which is the major
cause of cardiovascular pathologies like hypertension and ischaemic heart
disease .
********************************************

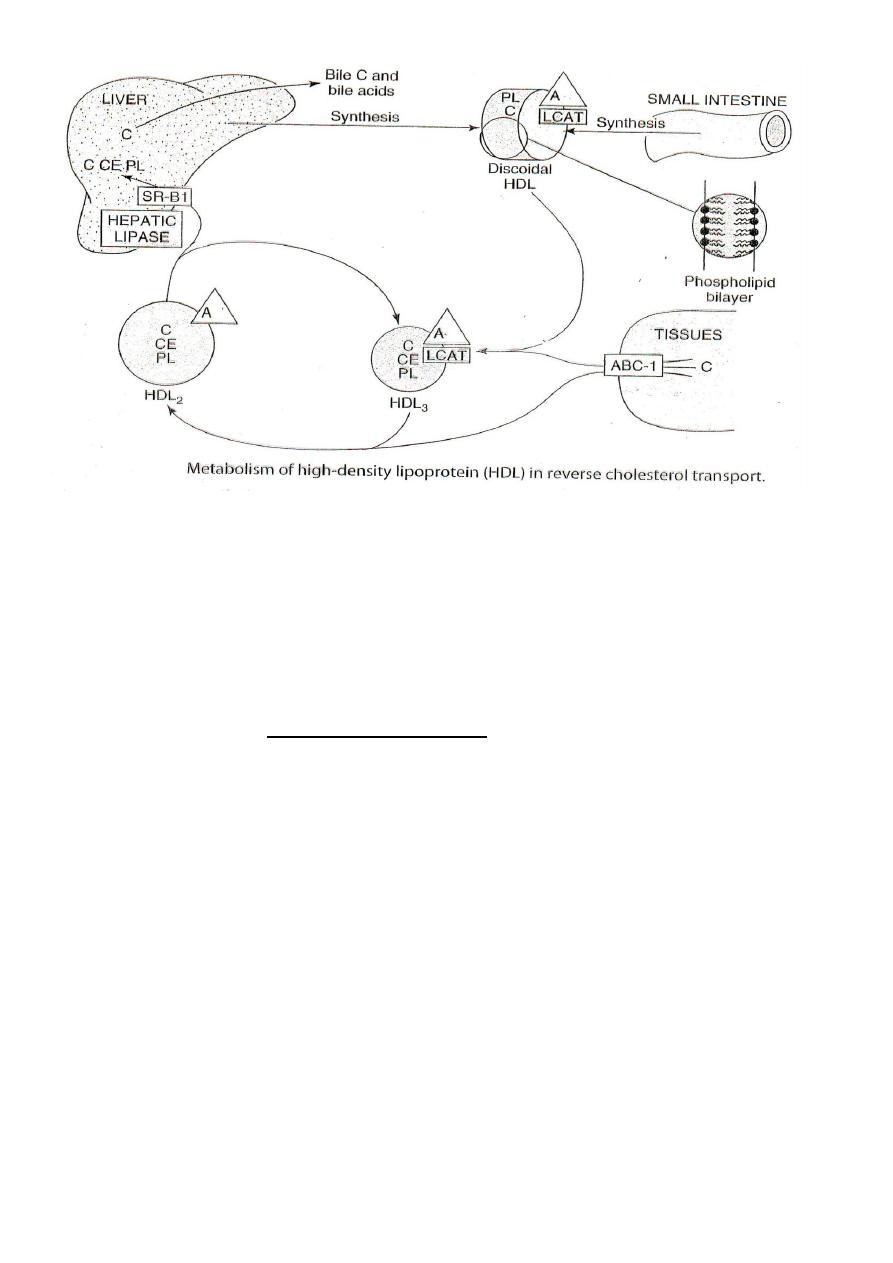
Metabolism of High Density Lipoprotein ( HDL ) :
● HDL is synthesized in the liver and gut .
● Nascent HDL particles are small and consists of phospholipid
bilayers containing apo-A , apo-C , apo-E and free cholesterol .
● HDL contains a much higher percentage of its weight as protein and a
much lower percentage as triglycerides than other lipoproteins and
therefore is the most dense .
● HDL function is the transport of free cholesterol from peripheral tissues
and other lipoproteins to liver to be excreted in the bile . Therefore ,
HDL is known as " Good Cholesterol " and HDL is considered anti-
atherogenic and also termed as " Highly Desirable Lipoprotein " .
● HDL particles pick up free cholesterol from cell membranes and other
lipoproteins and converts it to cholesterol esters by a reaction catalyzed
by the enzyme Lecithin Cholesterol Acyl Transferase ( LCAT ) . This
enzyme is present in plasma and is activated by the apo-A of HDL .
● As HDL particles fill with cholesterol esters , they become large and
spherical in shape known as HDL
3
.
● HDL
3
exchange cholesterol esters with lipoproteins VLDL ,IDL & LDL
in exchange for triglycerides . This process is mediated by Cholesterol
Ester Transfer Protein (CETP) .
●
As a result of the transfer of lipids and apoproteins between HDL
3
and
other lipoproteins , the HDL
3
particles become mature and termed
HDL
2
.
● Mature HDL particles (HDL
2
) has two fates :
(a) are taken up by the liver cells by apo-A mediated receptors and fully
degraded .
(b) binds to scavenger receptor and cholesterol ester is
selectively delivered to the liver cells to be excreted .
● The transfer of cholesterol from tissues to the liver is known as reverse
cholesterol transport .
**********************************
LIPID DISORDERS
●Lipid disorders are the commonest metabolic disease in clinical practice ;
some hyperlipidemia ( hyperlipemia ) are associated with coronary heart
disease ( CHD ) .
● Classification of lipid diseases based on lipoprotein analysis is of more
value in understanding abnormalities of lipid metabolism than one
based on chemical analysis only ( i.e. estimation of triglycerides &
cholesterol ) because all lipoproteins contain cholesterol and
triglycerides in different proportions .
● Lipoprotein disorders are best detected by electrophoresis . Once the
type of lipoprotein disorder is identified by electrophoresis , the next
step is to decide if it is a primary or secondary phenomenon .
Hypolipoproteinemia : Primary lipoprotein disorders due to inherited
defect :
1 . Abetalipoproteinemia :
Defect in loading apo-B with lipid . No chylomicron , VLDL & LDL are
formed . Lipid accumulate in intestine and liver . Fat-soluble vitamins
are not absorbed causing mental and physical retardation and may be
blindness . Serum TG , Cholesterol and Phospholipids are all very low .
2 . Familial alpha lipoprotein deficiency : Low or absence of HDL :
(a) Tangier disease : absence of protein that transfer cholesterol
to HDL ( absence of ABC-1 ) .
(b) Fish-Eye disease : apo-A deficiency .
Hyperlipoproteinemia:
May be primary or secondary to other diseases:
Type I
( Familial LpL deficiency )
:
there is LpL deficiency or inactive LpL
due to deficiency of apo-C . slow clearance of chylomicrons
& VLDL from plasma . Triglyceride is high and deposits in
tissues causing xanthoma . Cholesterol is normal .
Type II ( Familial hypercholesterolemia)
:
most common . LDL receptor
defect
so LDL level is elevated . Cholesterol level is high
but triglyceride is normal . Xanthomatosis and
cardiovascular disease at an early age .
Type III ( Broad Beta Disease ) : abnormal apo-E . Defective binding
to liver receptors and so deficient clearance of remnant
chylomicron & VLDL . Plasma cholesterol and triglyceride
are both elevated . Xanthomatosis and atherosclerosis .
Type IV ( Familial hypertriglyceridemia ) :
overproduction of VLDL .
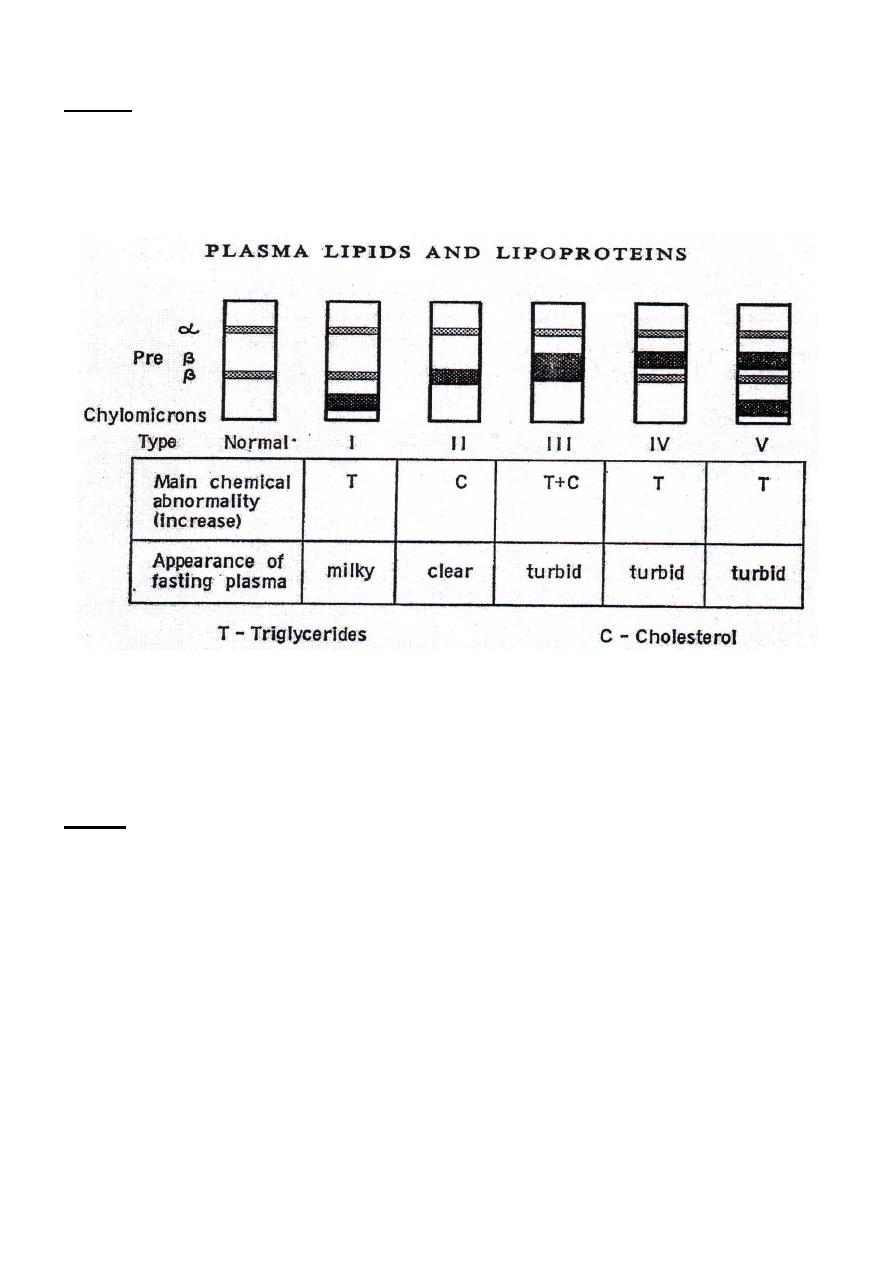
Type V Hypertriglyceridemia :
secondary to other causes . High TG both
endogenous and exogenous origin .
[ Classification of hyperlipoproteinaemia by lipoprotein electrophoresis ]
NOTE
● Blood for lipoprotein electrophoresis is taken after a fast of 14-16 hours
and is centrifuged ; the supernatant plasma or serum is examined .
● Visual turbidity in a fresh serum specimen indicate raised triglyceride .
● Distinction between turbidity due to exogenous TG ( chylomicrons ) and
that due to endogenous TG ( VLDL ) is made by allowing plasma to
stand overnight . Raised exogenous TG form a creamy layer on the
surface whereas endogenous TG remain dispersed .
**********************************************
