RBC Anemia and polycythemia
Red Blood Cells (Erythrocytes):
Functions of RBC:
The major function of red blood cells, also known as
erythrocytes,
is to transport
hemoglobin,
which in turn
carries oxygen
from the
lungs to the tissues.
The red blood cells contain a large quantity of
carbonic anhydrase
,
an enzyme that catalyzes the reversible reaction between carbon
dioxide (CO2) and water to form carbonic acid (H2CO3),
. The rapidity of this reaction makes it possible for the water of the
blood to
transport enormous quantities of CO2
in the form of
bicarbonate ion (HCO3–) from the tissues to the lungs, where it is
reconverted to CO2 and expelled into the atmosphere as a body
waste product.
The hemoglobin in the cells is an excellent
acid-base buffer
(as is
true of most proteins), so that the red blood cells are responsible
for most of the acid-base buffering power of whole blood.
Shape and Size of Red Blood Cells:
Normal red blood cells, are
biconcave
discs having a mean
diameter of about 7.8 micrometers
The red blood cell is a “bag” that can be deformed into almost any
shape.
Concentration of Red Blood Cells in the Blood:
In normal
men
, the average number of red blood cells per cubic
millimeter is 5,200,000;
in normal
women
, it is 4,700,000.
Persons living at high altitudes have greater numbers of red blood
cells.
Quantity of Hemoglobin in the Cells:-
When the hematocrit and the quantity of hemoglobin in each
respective cell are normal, the whole blood of men contains an
average of
15
grams of hemoglobin per 100 milliliters of cells (dl);
for women, it contains an average of
14
grams per 100 milliliters
(dl).
Each gram of pure hemoglobin is capable of combining with
1.34
milliliters of oxygen.
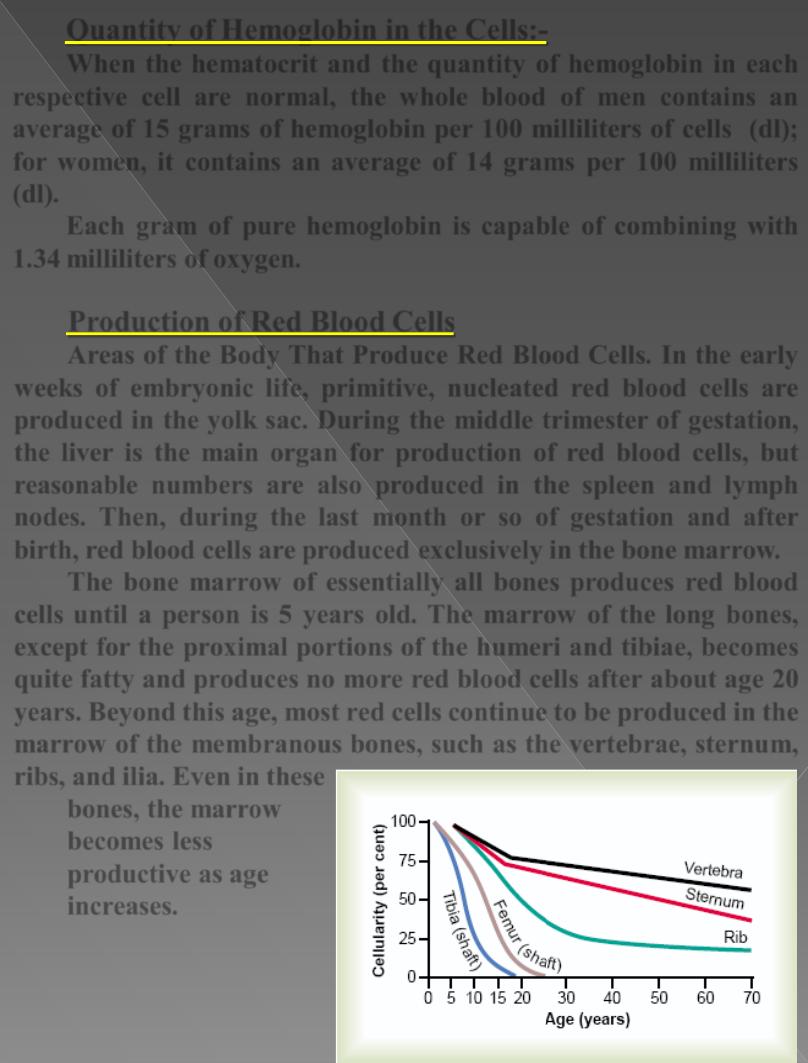
Production of Red Blood Cells
Areas of the Body That Produce Red Blood Cells.
In the
early
weeks
of embryonic life, primitive, nucleated red blood cells are
produced in the
yolk sac
. During the
middle
trimester
of gestation,
the
liver
is the main organ for production of red blood cells, but
reasonable numbers are also produced in the
spleen
and
lymph
nodes
. Then, during the
last
month
or so of gestation and after
birth, red blood cells are produced exclusively in the
bone marrow
.
The bone marrow of essentially all bones produces red blood
cells until a person is
5
years old
. The marrow of the long bones,
except for the proximal portions of the humeri and tibiae, becomes
quite fatty and produces no more red blood cells after about age
20
years
. Beyond this age, most red cells continue to be produced in the
marrow of the membranous bones, such as the
vertebrae,
sternum,
ribs
,
and
ilia
. Even in these
bones, the marrow
becomes less
productive as age
increases.
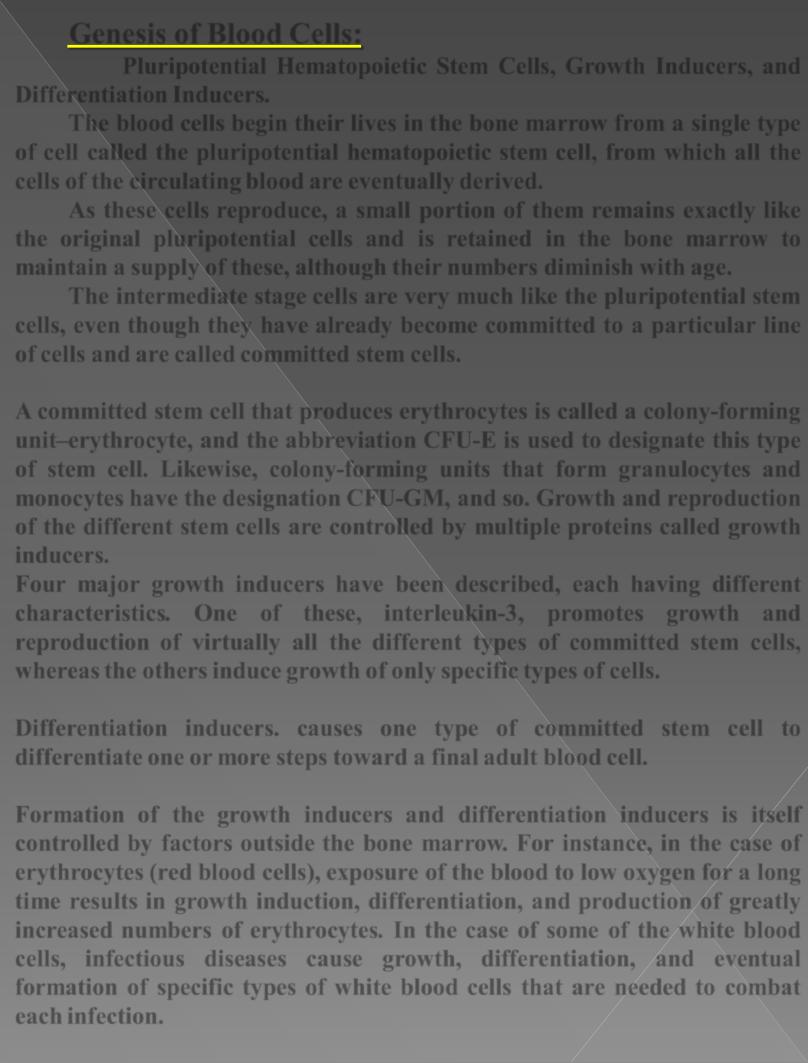
Genesis of Blood Cells:
Pluripotential Hematopoietic Stem Cells, Growth Inducers, and
Differentiation Inducers.
The blood cells
begin
their lives in the bone marrow from a single type
of cell called the
pluripotential hematopoietic
stem cell, from which all the
cells of the circulating blood are eventually derived.
As these cells reproduce, a small portion of them
remains exactly
like
the original pluripotential cells and is retained in the bone marrow to
maintain a supply of these, although their numbers diminish with age.
The intermediate stage cells are very much like the pluripotential stem
cells, even though they have already become committed to a particular line
of cells and are called
committed stem cells.
A committed stem cell that produces erythrocytes is called a colony-forming
unit–erythrocyte, and the abbreviation
CFU-E
is used to designate this type
of stem cell. Likewise, colony-forming units that form granulocytes and
monocytes have the designation
CFU-GM
, and so. Growth and reproduction
of the different stem cells are controlled by multiple proteins called
growth
inducers
.
Four major growth inducers have been described, each having different
characteristics. One of these,
interleukin-3
, promotes growth and
reproduction of virtually all the different types of committed stem cells,
whereas the others induce growth of only specific types of cells.
Differentiation
inducers
. causes one type of committed stem cell to
differentiate one or more steps toward a final adult blood cell.
Formation of the growth inducers and differentiation inducers is itself
controlled
by
factors
outside
the bone marrow. For instance, in the case of
erythrocytes
(red
blood
cells),
exposure of the blood to low oxygen for a long
time results in growth induction, differentiation, and production of greatly
increased numbers of erythrocytes. In the case of some of the
white
blood
cells, infectious diseases cause growth, differentiation, and eventual
formation of specific types of white blood cells that are needed to combat
each infection.
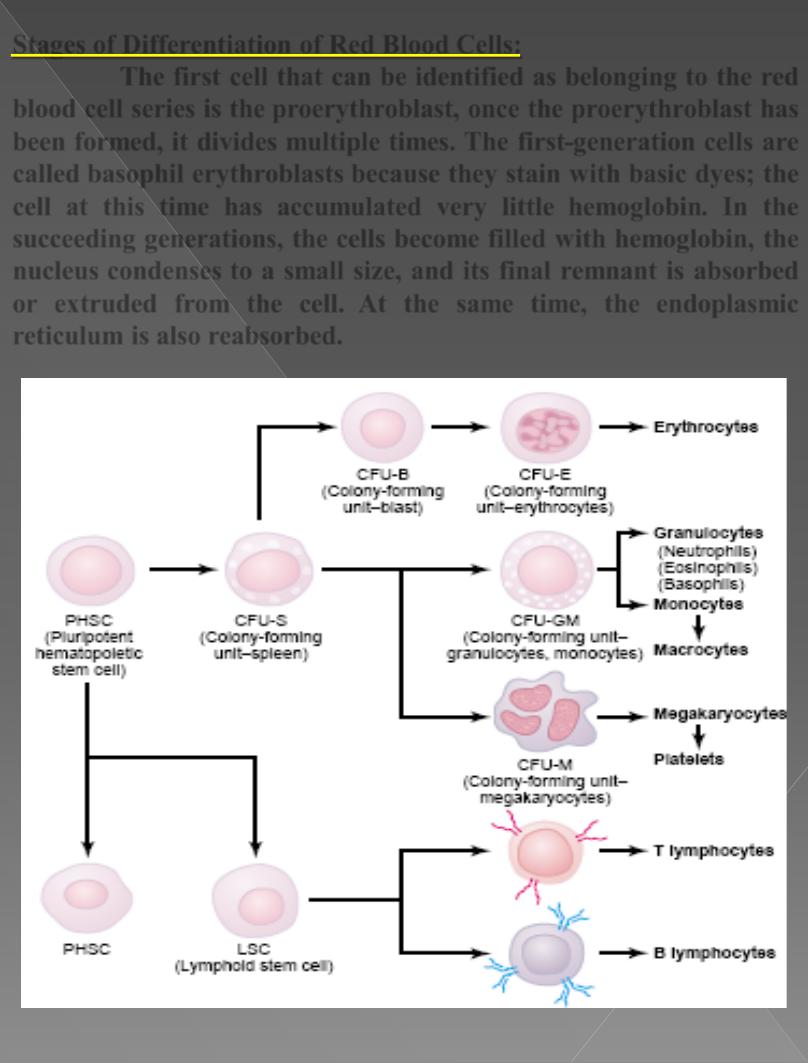
Stages of Differentiation of Red Blood Cells:
The first cell that can be identified as belonging to the red
blood cell series is the
proerythroblast
, once the proerythroblast has
been formed, it divides multiple times. The first-generation cells are
called
basophil
erythroblasts
because they stain with basic dyes; the
cell at this time has accumulated very little
hemoglobin
. In the
succeeding generations, the cells become filled with hemoglobin, the
nucleus
condenses
to a small size, and its final remnant is absorbed
or extruded from the cell. At the same time, the
endoplasmic
reticulum is also reabsorbed.
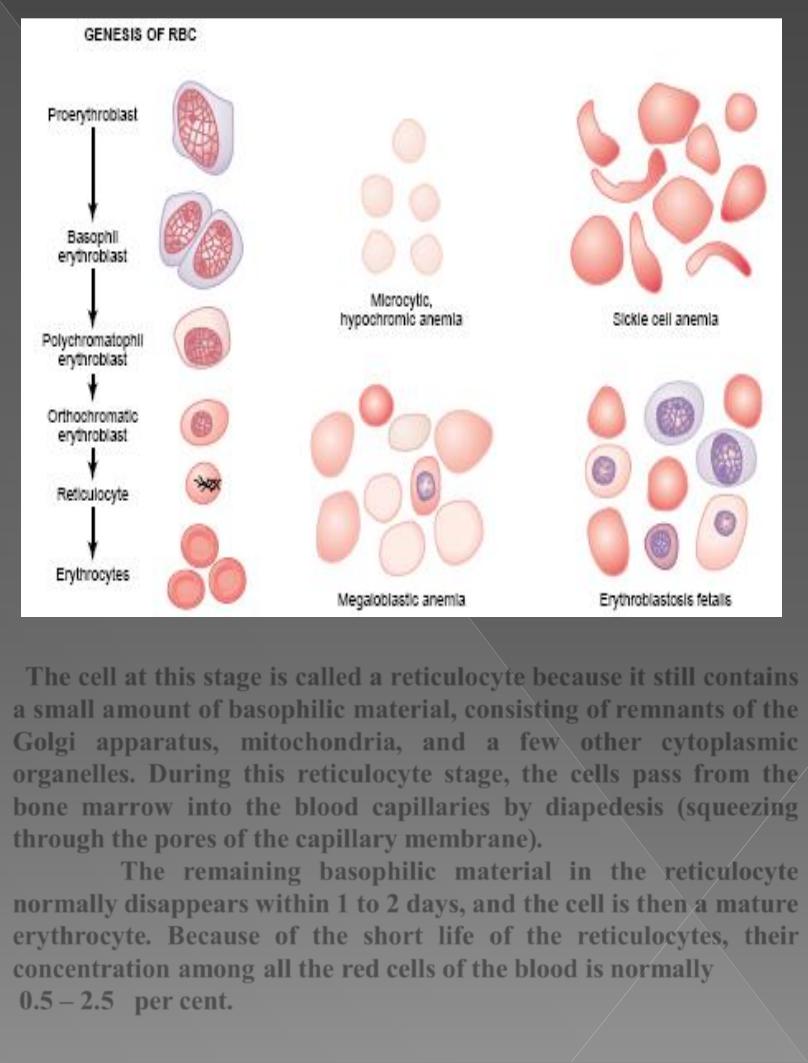
The cell at this stage is called a
reticulocyte
because it still contains
a small amount of basophilic material, consisting of remnants of the
Golgi
apparatus,
mitochondria
, and a few other cytoplasmic
organelles
. During this reticulocyte stage, the cells pass from the
bone marrow into the blood capillaries by diapedesis (squeezing
through the pores of the capillary membrane).
The remaining basophilic material in the reticulocyte
normally disappears within 1 to 2 days, and the cell is then a
mature
erythrocyte
. Because of the short life of the reticulocytes, their
concentration among all the red cells of the blood is normally
0.5
–
2.5
per
cent
.
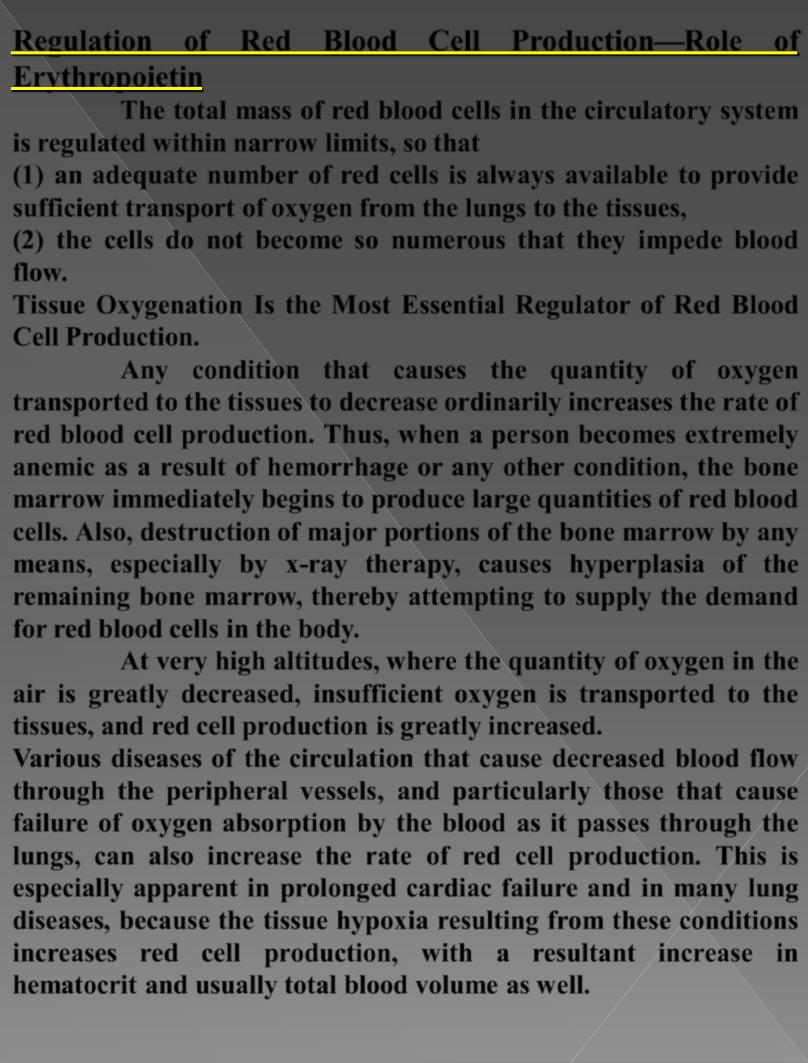
Regulation of Red Blood Cell Production—Role of
Erythropoietin
The total mass of red blood cells in the circulatory system
is regulated within narrow limits, so that
(1) an
adequate
number of red cells is always available to provide
sufficient transport of oxygen from the lungs to the tissues,
(2) the cells do not become so numerous that they
impede
blood
flow.
Tissue
Oxygenation
Is the Most Essential Regulator of Red Blood
Cell Production.
Any condition that causes the quantity of oxygen
transported to the tissues to decrease ordinarily increases the rate of
red blood cell production. Thus, when a person becomes extremely
anemic
as a result of hemorrhage or any other condition, the bone
marrow immediately begins to produce large quantities of red blood
cells. Also, destruction of major portions of the bone marrow by any
means, especially by x-ray therapy, causes hyperplasia of the
remaining bone marrow, thereby attempting to supply the demand
for red blood cells in the body.
At very high altitudes, where the
quantity
of
oxygen
in the
air is greatly decreased, insufficient oxygen is transported to the
tissues, and red cell production is greatly increased.
Various diseases of the
circulation
that cause decreased blood flow
through the peripheral vessels, and particularly those that cause
failure
of
oxygen
absorption
by the blood as it passes through the
lungs, can also increase the rate of red cell production. This is
especially apparent in prolonged
cardiac failure
and in many
lung
diseases
, because the tissue hypoxia resulting from these conditions
increases red cell production, with a resultant increase in
hematocrit and usually total blood volume as well.
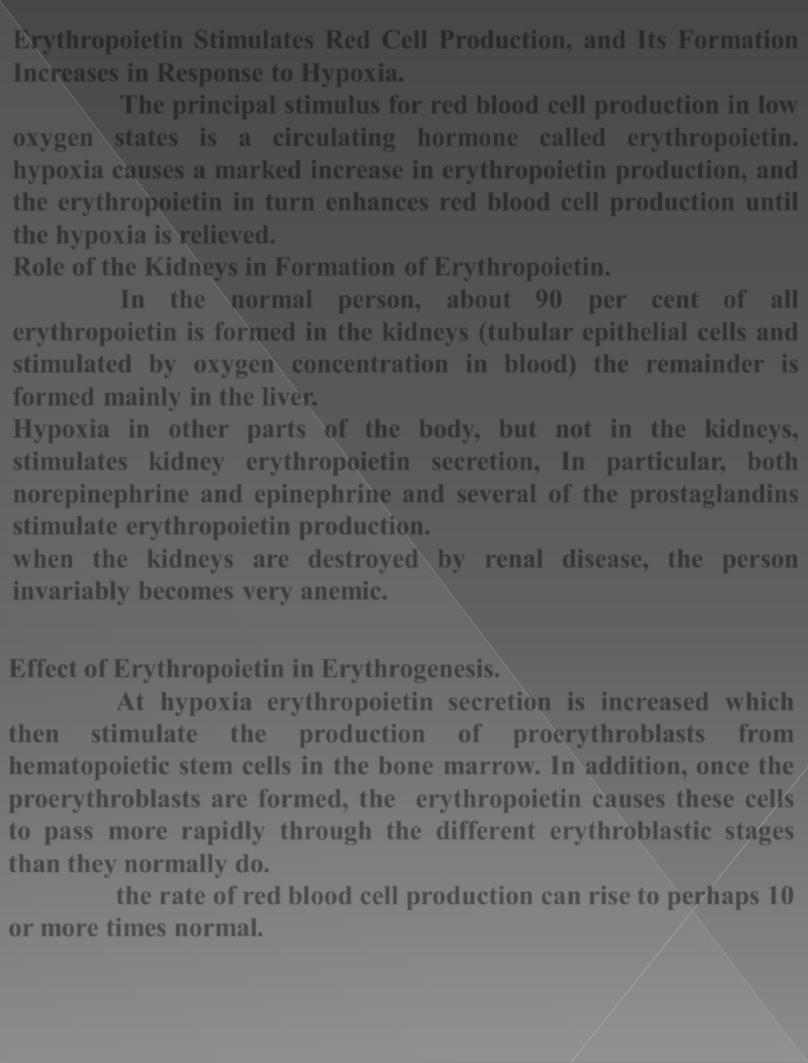
Erythropoietin Stimulates Red Cell Production, and Its Formation
Increases in Response to Hypoxia
.
The principal stimulus for red blood cell production in low
oxygen states is a circulating hormone called erythropoietin.
hypoxia causes a marked increase in erythropoietin production, and
the erythropoietin in turn enhances red blood cell production until
the hypoxia is relieved.
Role of the Kidneys in Formation of Erythropoietin.
In the normal person, about
90 per cent
of all
erythropoietin is formed in the kidneys (tubular epithelial cells and
stimulated by oxygen concentration in blood) the remainder is
formed mainly in the liver.
Hypoxia in other parts of the body, but not in the kidneys,
stimulates kidney erythropoietin secretion, In particular, both
norepinephrine
and
epinephrine
and several of the prostaglandins
stimulate erythropoietin production.
when the kidneys are destroyed by renal disease, the person
invariably becomes very anemic.
Effect of Erythropoietin in Erythrogenesis.
At hypoxia erythropoietin secretion is increased which
then
stimulate
the
production
of
proerythroblasts
from
hematopoietic stem cells in the bone marrow. In addition, once the
proerythroblasts are formed, the erythropoietin causes these cells
to pass more rapidly through the different erythroblastic stages
than they normally do.
the rate of red blood cell production
can rise to perhaps 10
or more times normal.
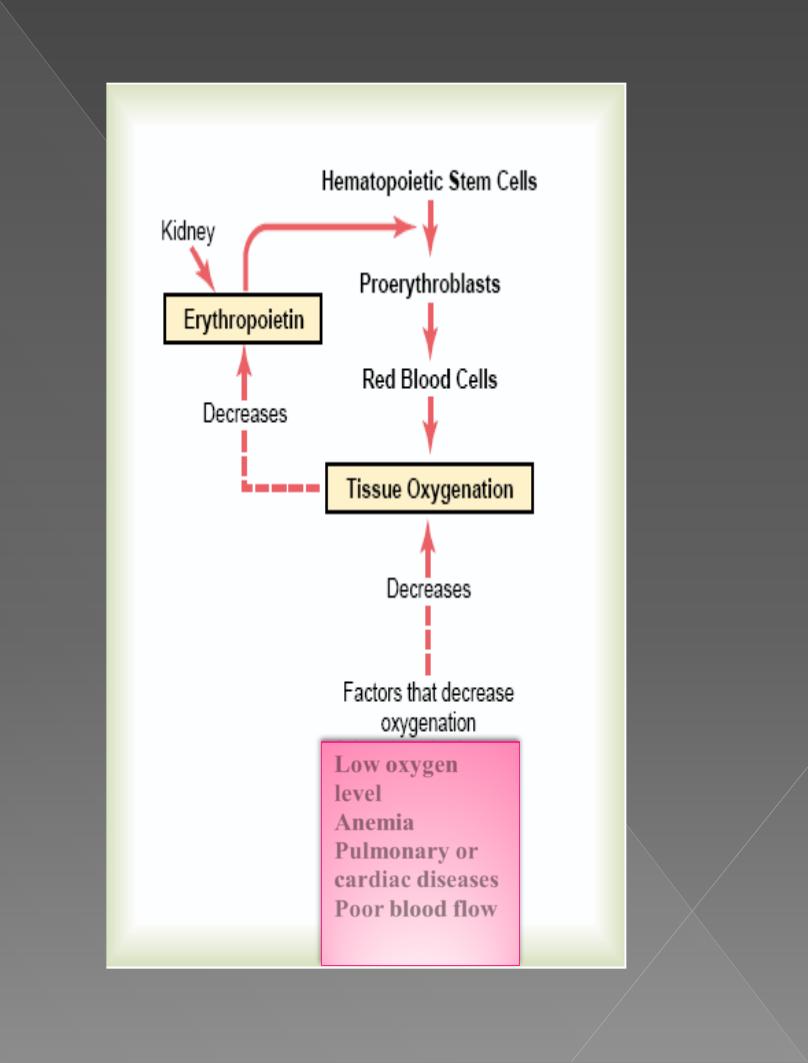
Low oxygen
level
Anemia
Pulmonary or
cardiac diseases
Poor blood flow
