بسم هللا الرحمن الرحيم
Tubular function 2
Additional Examples of
Secondary Active Transport
• Like glucose reabsorption,
amino acid
reabsorption is
most marked in the early portion of the
proximal
convoluted
tubule.
• Absorption in this location resembles absorption in the
intestine .
• The main carriers in the luminal membrane
cotransport Na
+
,
whereas the carriers in the
basolateral membranes are not Na
+
-dependent.
• Na
+
is pumped out of the cells by
Na
+
-K
+
ATPase
and
the amino acids leave by
passive or facilitated
diffusion
to the interstitial fluid.

Additional Examples of
Secondary Active Transport
• Some Cl
-
is reabsorbed with Na
+
and K
+
in the
thick ascending limb of the loop of Henle .
• In addition,
two members
of a family of Cl
-
channels have been identified in the kidney.
• The family is characterized by
12
transmembrane domains
, and members of it
are also found in muscle and other tissues.

Tubuloglomerular Feedback &
Glomerulotubular Balance
• Signals from the renal tubules feed back to affect
glomerular filtration.
• As the
rate of flow
through the ascending limb of the loop
of Henle and first part of the distal tubule increases,
glomerular filtration in the same nephron decreases, and,
conversely, a
decrease in flow
increases the GFR .
• This process, which is called
tubuloglomerular feedback
,
tends to maintain the constancy of the load delivered to
the distal tubule .
• The sensor for the response appears to be the
macula
densa
, and GFR is adjusted by constriction or dilation of the
afferent arteriole
.
• Constriction may be mediated by
thromboxane A
2
.
Tubuloglomerular Feedback &
Glomerulotubular Balance
• Conversely
, an increase in GFR causes an increase in the
reabsorption of solutes, and consequently of water,
primarily in the proximal tubule, so that in general the
percentage of the solute reabsorbed is held constant.
• This process is called
glomerulotubular balance
, and it is
particularly prominent for Na
+
.
• The change in Na
+
reabsorption occurs within seconds
after a change in filtration, so it seems unlikely that an
extrarenal humoral factor is involved.
• One factor is the
oncotic pressure
in the peritubular
capillaries.
• When the GFR is high, there is a relatively large increase in
the oncotic pressure of the plasma by the time it reaches
the
efferent arterioles and their capillary branches
. This
increases the reabsorption of Na
+
from the tubule.

REGULATION OF NA
+
& CL
-
EXCRETION
• Na
+
is filtered in large amounts, but it is actively
transported out of all portions of the tubule
except the
thin loop of Henle.
• Normally,
96%
to well over
99%
of the filtered
Na
+
is reabsorbed.
• Most of the
Na
+
is reabsorbed with Cl
-
, but some
is reabsorbed in the processes by which one Na
+
ion enters the bloodstream
for each H
+
ion
secreted by the tubules, and in the distal tubules
a small amount is actively reabsorbed in
association with the
secretion of K
+
.

Regulation of Na
+
Excretion
• Because Na
+
is the
most abundant
cation in ECF
and because Na
+
salts account for over
90%
of
the
osmotically active
solute in the plasma and
interstitial fluid, the amount of Na
+
in the body
is
a prime determinant of the ECF volume.
• Through the operation of the regulatory
mechanisms, the amount of Na
+
excreted
is
adjusted to
equal
the amount
ingested
over a
wide range of dietary intakes, and the individual
stays in Na
+
balance.
• Thus,
urinary Na
+
output ranges from
less than 1
meq/d
on a low-salt diet to
400 meq/d
or more
when the dietary Na
+
intake is high.

Regulation of Na
+
Excretion
• In addition, there is a
natriuresis
when saline is
infused intravenously and a
decrease in Na
+
excretion
when ECF volume is reduced.
• Variations in Na
+
excretion are effected by changes
in the
amount filtered
and the
amount reabsorbed
in
the tubules.
• The factors affecting the GFR, including
tubuloglomerular feedback
.
• Factors affecting Na
+
reabsorption include the
circulating level of
aldosterone
and
other
adrenocortical hormones, the circulating level of
ANP
and other
natriuretic
hormones, the amount of
angiotensin II
and
PGE
2
in the kidneys, and the rate
of tubular secretion of H
+
and K
+
.

Effects of Adrenocortical Steroids
• Adrenal mineralocorticoids such as aldosterone
increase tubular
reabsorption of Na
+
in association
with
secretion of K
+
and H
+
and also
Na
+
reabsorption
with Cl
-
.
• When these hormones are injected into
adrenalectomized animals, there is a latent period of
10-30 minutes before their effects on Na
+
reabsorption
become manifest, because of the time required for the
steroids to
alter protein synthesis via their action on
DNA.
• The mineralocorticoids
act
primarily on the
cortical
collecting ducts.
• As noted , they act on
P cells
to increase the number
of active
ENaCs
in the apical membranes of these cells .
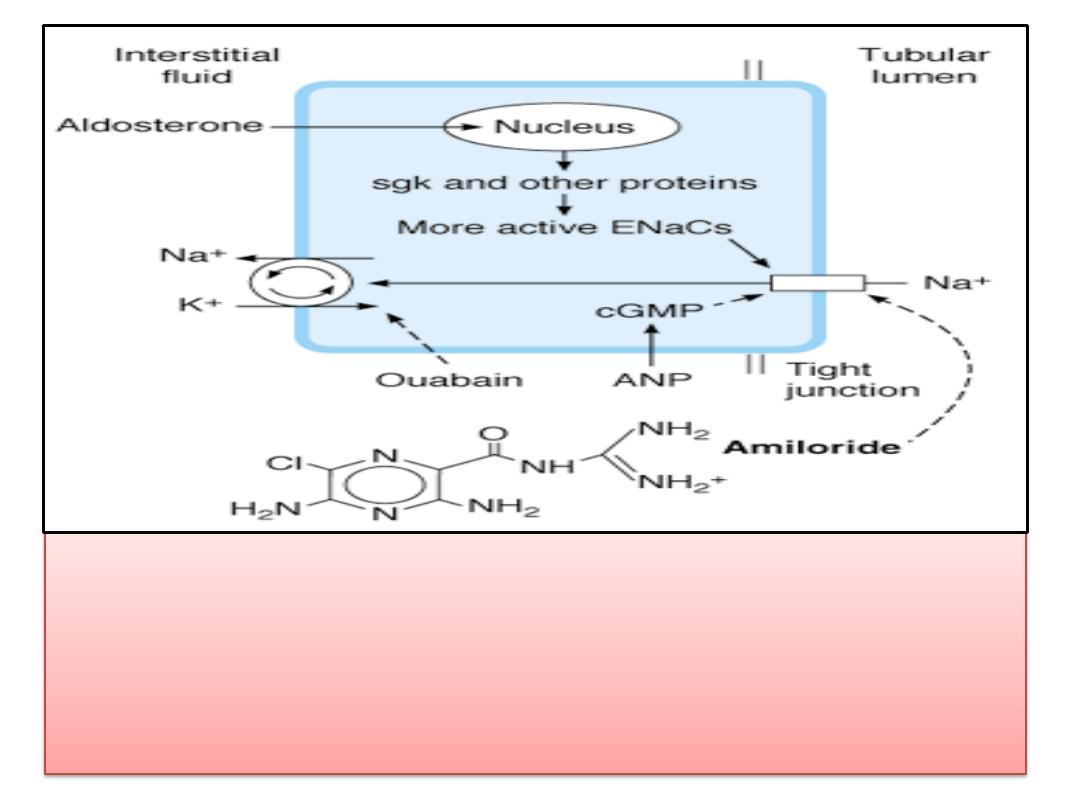
Renal P cell. Na
+
enters via the ENaCs in the apical membrane and is
pumped into the interstitial fluid by Na
+
-K
+
ATPases in the basolateral
membrane. Aldosterone activates the genome to produce sgk and
other proteins, and the number of active ENaCs is increased
.
Effects of Adrenocortical Steroids
• In
Liddle's syndrome
, mutations in the
genes that code for the
β subunit
and less
commonly the
γ subunit
of the
ENaCs
cause
them to become
constitutively active
in the
kidney.
• This leads to
Na
+
retention
and
hypertension
.

Other Humoral Effects
• Reduction of
dietary
intake of
salt
increases
aldosterone secretion , producing marked but slowly
developing decreases in Na
+
excretion.
• A variety of other humoral factors affect Na
+
reabsorption.
• PGE
2
causes
a natriuresis
, possibly by inhibiting Na
+
-K
+
ATPase .
•
Endothelin
and
IL-1
cause natriuresis, probably by
increasing the formation of
PGE
2
.
• ANP
and related molecules increase intracellular
cGMP,
and this inhibits transport via the
ENaCs
.
• Inhibition of
Na
+
-K
+
ATPase
by the other natriuretic
hormone, also increases Na
+
excretion.
•
Angiotensin II increases reabsorption
of Na
+
and HCO
3
-
by an action on the proximal tubules.

Other Humoral Effects
• There is an appreciable amount of
angiotensin-converting
enzyme
in the kidneys, and the kidneys convert of the
circulating angiotensin I reaching them to angiotensin II. In
addition,
angiotensin I is generated in the kidneys.
• Prolonged exposure to high levels of circulating
mineralocorticoids does not cause edema
in otherwise
normal individuals
because eventually the kidneys
escape from the effects of the steroids.
• This
escape phenomenon
, which may be due to increased
secretion of
ANP
,
• It appears to be reduced or absent in
nephrosis, cirrhosis,
and heart failure,
and patients with these diseases continue
to retain Na
+
and become edematous when exposed to
high levels of mineralocorticoids.

REGULATION OF K
+
EXCRETION
• Much of the filtered K
+
is removed from the tubular
fluid by
active reabsorption
in the
proximal
tubules ,
and K
+
is then
secreted
into the fluid by the
dista
l
tubular cells.
• The
rate of K
+
secretion
is proportionate to the
rate of
flow
of the tubular fluid through the distal portions of
the nephron, because with rapid flow there is less
opportunity for the tubular K
+
concentration to rise to
a value that stops further secretion.
• In the absence of complicating factors,
the amount
secreted
is approximately
equal to the K
+
intake
, and K
+
balance is maintained.
• In the distal tubules
, Na
+
is generally reabsorbed and
K
+
is secreted
.
•

REGULATION OF K
+
EXCRETION
• There is no rigid
one-for-one
exchange, and
much of the
movement of K
+
is passive
.
• However, there is electrical coupling in the
sense that
intracellular migration of Na
+
tends
to lower the potential difference across the
tubular cell, and this favors movement of K
+
into the tubular lumen.
• Since
Na
+
is also reabsorbed in association
with
H
+
secretion, there is competition for the
Na
+
in the tubular fluid.

REGULATION OF K
+
EXCRETION
• K
+
excretion is decreased
when the amount of
Na
+
reaching the distal tubule is
small
, and it is also
decreased when
H
+
secretion
is
increased
.
• When
total body K
+
is high
, H
+
secretion is inhibited,
apparently because of intracellular alkalosis; K
+
secretion and excretion are therefore facilitated.
• Conversely
, the cells are acidic in
K
+
depletion
, and K
+
secretion declines.
• Apparently the K
+
secretory mechanism is capable of
"
adaptation
," because the amount of K
+
excreted
gradually increases when a constant large dose of a
potassium salt is administered for a prolonged period.
Hypokalemia
•
Hypokalemia
is common and can be severe.
• In addition to its occurrence when there is
excessive loss in the urine
, it is occasionally
seen in patients with excess loss in
diarrheic
stools
, in patients in whom K
+
is
shifted
into
cells by
insulin
or
β-adrenergic agonists
, and in
patients with a prolonged
low intake of K
+
.
• Hyperkalemia
is a more dangerous condition
because of its effects on the heart , but
it
rarely occurs unless
renal function is
depressed.
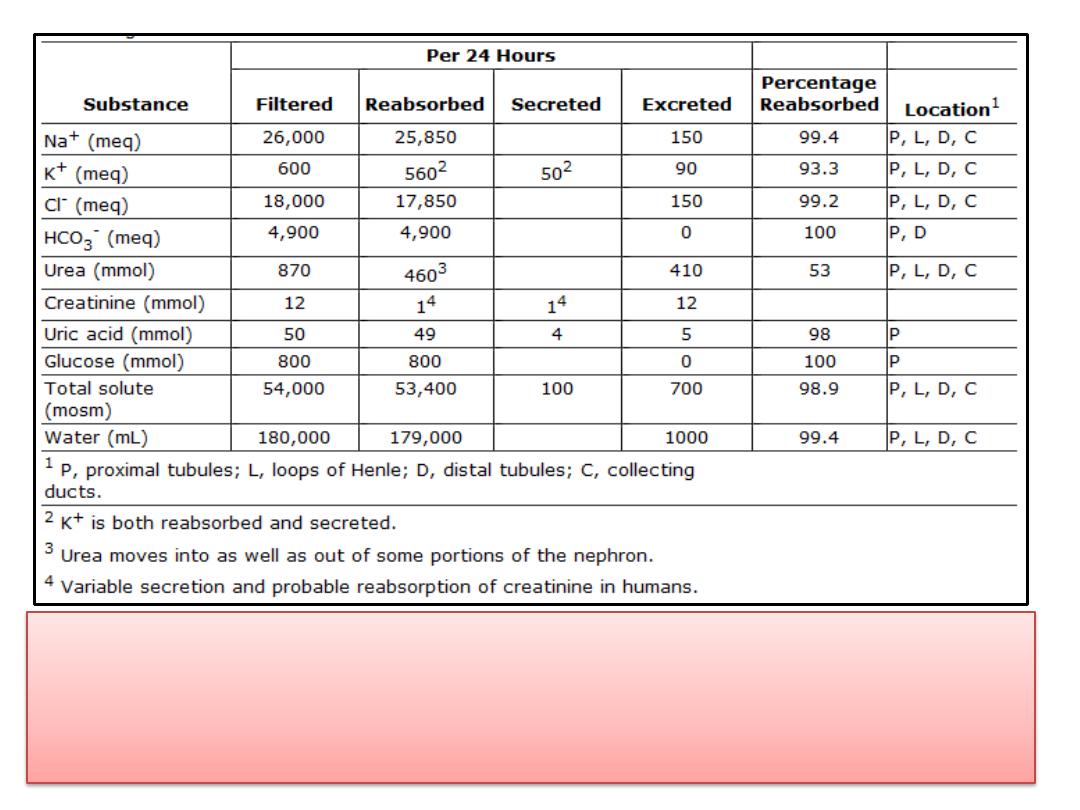
Renal handling of various plasma constituents in a
normal adult human on an average diet
.
THANK
YOU
