GLOMERULAR FILTRATION
Measuring GFR
•
The
glomerular filtration rate
(GFR) can be measured
in humans by measuring the
excretion and plasma
level
of a substance that is freely filtered through the
glomeruli and neither secreted nor reabsorbed by the
tubules.
• Therefore, if the substance is designated by the letter
X
, the GFR is equal to the
concentration of X in urine
(U
X
) times the
urine flow
per unit of time
(V.)
divided
by the
arterial plasma level of X (P
X
), or
U
X
V./P
X
.
• This value is called the
clearance of X
(C
X
).
•
P
X
is
, of course, the same in all parts of the arterial
circulation, and if X is
not metabolized
to any extent in
the tissues, the level of X in peripheral
venous plasma
can be substituted for the
arterial plasma
level
Substances Used to Measure GFR
• In addition to the requirement that it be
freely filtered
and
neither
reabsorbed nor secreted
in the tubules, a substance suitable for
measuring the GFR should be
nontoxic
and
not metabolized
by the
body.
• Inulin
, a polymer of fructose with a molecular weight of 5200,
meets these criteria
in humans and most animals and is extensively
used to measure GFR.
•
Radioisotopes such as
51
Cr-EDTA
are also used, but inulin remains
the standard substance.
• In practice, a loading dose of inulin is administered intravenously,
followed by a sustaining infusion to keep the arterial plasma level
constant.
• After the inulin has equilibrated with body fluids, an accurately
timed urine specimen is collected and a plasma sample obtained
halfway through the collection.
•
Substances Used to Measure GFR
• Plasma and urinary inulin concentrations are
determined and the clearance calculated:
Uin = 35 mg /ml
V = 0.9 ml /min
Pin = 0.25 mg /ml
Cin= Uin* V/Pin =35*0.9/0.25=
In C= 126ml/min
Substances Used to Measure GFR
• clearance of creatinine (C
Cr
)
can also be used to determine
the GFR, but in humans, some creatinine is
secreted
by the
tubules and some may be
reabsorbed
.
• In addition,
plasma creatinine
determinations are
inaccurate
at low creatinine levels because the method for
determining creatinine measures small amounts of other
plasma constituents.
•
In spite of this, the clearance of endogenous creatinine is
frequently measured in patients.
• The values agree quite well with the GFR values measured
with inulin because, although the value for U
Cr
V. is high as a
result of tubular secretion, the value for P
Cr
is also high as a
result of nonspecific chromogens, and the errors thus tend
to cancel.

Normal GFR
• The GFR in an average-sized normal man is
approximately
125 mL/min
.
• Its magnitude correlates fairly well with
surface
area
, but values in
women
are
10%
lower than
those in
men
even after correction for surface
area.
• A rate of
125 mL/min is 7.5 L/h
, or
180 L/d
,
whereas the normal urine volume is about 1 L/d.
• Thus,
99%
or more of the filtrate is normally
reabsorbed.

Control of GFR
• The factors governing filtration across the glomerular
capillaries are the same as those governing filtration across
all other capillaries , ie,
the size
of the capillary bed, the
permeability
of the capillaries, and the
hydrostatic
and
osmotic pressure
gradients across the capillary wall. For
each nephron:
GFR = Kf [(Pgc – Pt) – (π
GC
- π
T )
]
K
f
, the
glomerular ultrafiltration coefficient
, is the product
of the glomerular capillary wall hydraulic conductivity (ie,
its
permeability
) and the effective filtration
surface area
.
P
GC
is the
mean hydrostatic pressure
in the glomerular
capillaries, P
T
the mean hydrostatic pressure in the tubule,
π
GC
the
osmotic pressure
of the plasma in the glomerular
capillaries, and π
T
the osmotic pressure of the filtrate in the
tubule.
Permeability
• The permeability of the
glomerular capillaries
is about
50 times
that of the
capillaries in skeletal muscle.
• Neutral substances with effective molecular diameters of less
than 4 nm
are freely filtered, and the filtration of neutral substances with diameters
of
more than 8 nm
approaches zero .
•
Between these values, filtration is
inversely
proportionate to
diameter
.
•
However,
sialoproteins
in the glomerular capillary wall are
negatively
charged
, and studies with anionically charged and cationically charged
dextrans indicate that the negative charges repel negatively charged
substances in blood, with the result that filtration of anionic substances 4
nm in diameter is less than half that of neutral substances of the same
size.
• This probably explains why
albumin
, with an effective molecular diameter
of approximately
7 nm
, normally has a glomerular concentration only
0.2%
of its plasma concentration rather than the higher concentration that
would be expected on the basis of diameter alone;
circulating albumin is
negatively charged.
•
Filtration of
cationic substances
is greater than that of
neutral substances
.
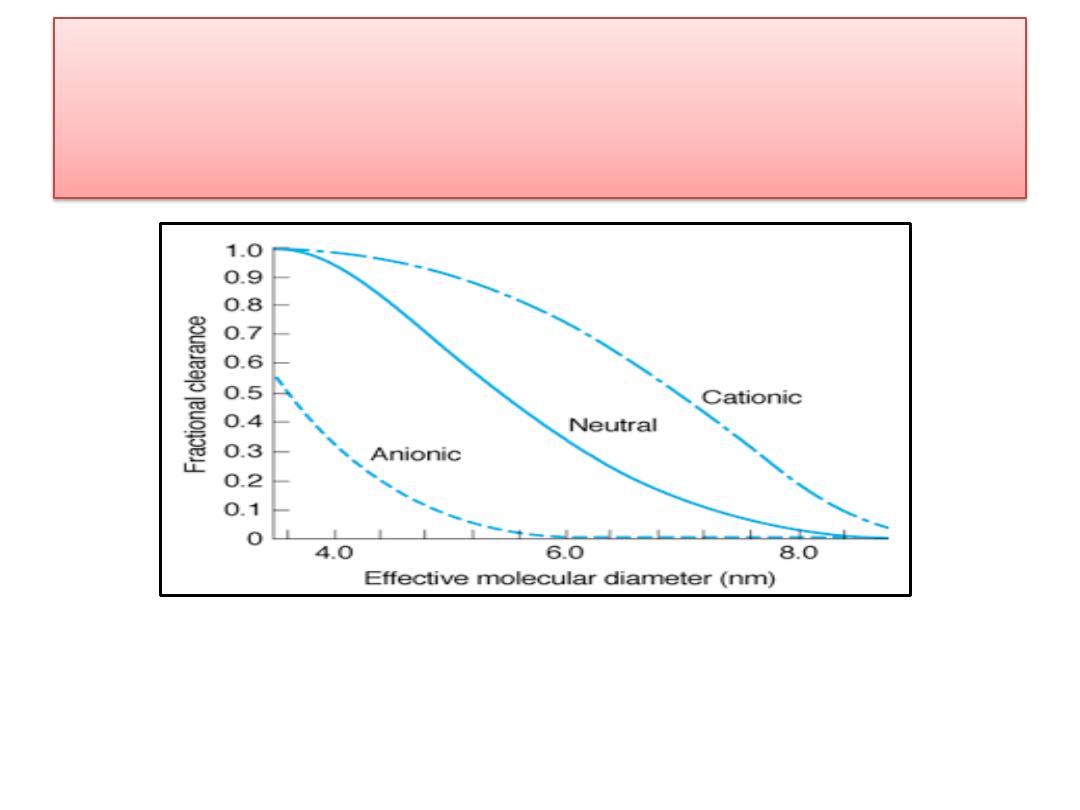
Effect of electrical charge on the fractional clearance of dextran molecules of various
sizes in rats. The negative charges in the glomerular membrane retard the passage of
negatively charged molecules (anionic dextran) and facilitate the passage of positively
charged molecules (cationic dextran).
Permeability
• The amount of protein in the urine is normally
less than
100 mg/d
, and most of this is not
filtered but comes from
shed tubular cells
.
• The presence of significant amounts of albumin
in the urine is called
albuminuria
.
• In nephritis, the
negative charges
in the
glomerular wall are dissipated, and albuminuria
can occur for this reason
without an increase in
the size of the "pores"
in the membrane.

Size of the Capillary Bed
• K
f
can be
altered
by the
mesangial cells
,
contraction
of
these cells producing a
decrease
in K
f
that is largely due
to a reduction in the area available for filtration.
• Contraction of
points
where the capillary loops
bifurcate
probably shifts flow away from some of the
loops, and elsewhere, contracted mesangial cells
distort and encroach on the capillary lumen.
• Angiotensin II
is an important regulator of
mesangial
contraction
, and there are angiotensin II receptors in
the
glomeruli
.
• In addition, there is some evidence that
mesangial
cells
make renin
.
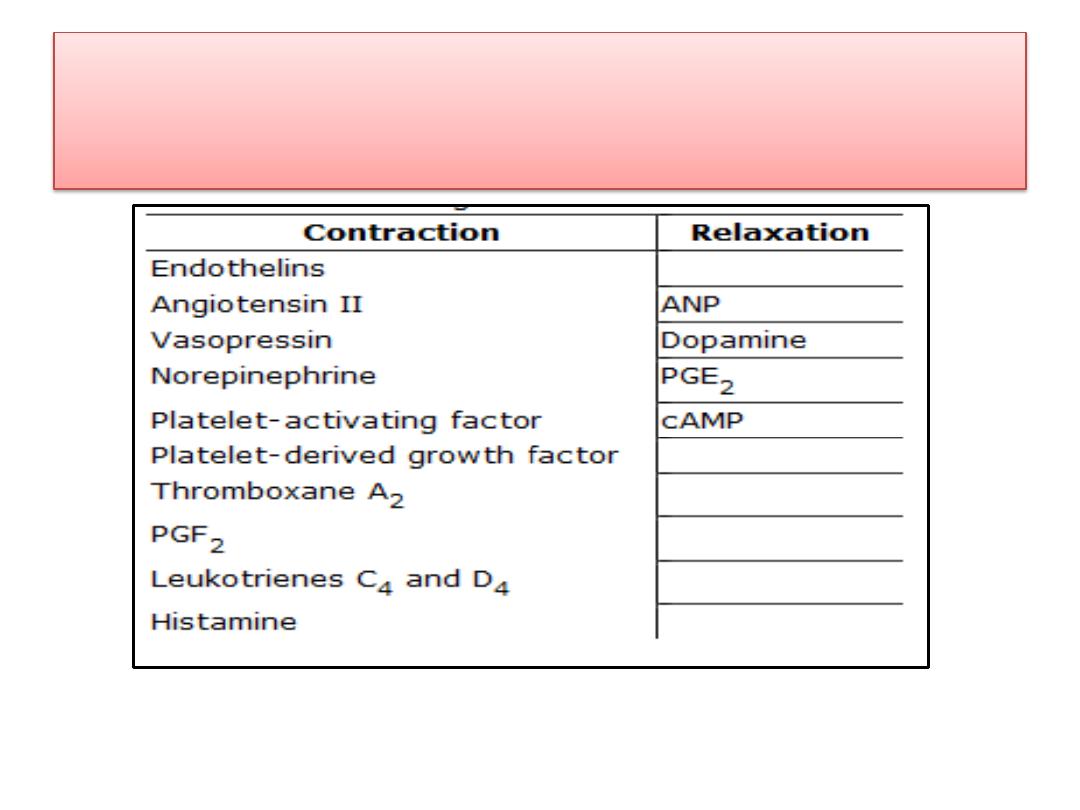
Agents causing contraction or
relaxation of mesangial cells.
Hydrostatic & Osmotic Pressure
• The
pressure in the glomerular capillaries
is higher
than that in other capillary beds because the afferent
arterioles are short, straight branches of the
interlobular arteries.
• Furthermore, the vessels "downstream" from the
glomeruli, the
efferent
arterioles, have a
relatively high
resistance.
• The
capillary
hydrostatic pressure is opposed by the
hydrostatic pressure in
Bowman's capsule
.
• It is also opposed by the
osmotic pressure
gradient
across the glomerular capillaries (π
GC
- π
T
).
• π
T
is normally negligible, and the gradient is equal to
the
oncotic pressure
of the plasma proteins.

Hydrostatic & Osmotic Pressure
• The
net filtration pressure
(P
UF
) is
15 mm Hg
at the
afferent end of the glomerular capillaries, but it falls to
zero—ie,
filtration equilibrium
is reached—proximal to
the efferent end of the glomerular capillaries.
• This is because fluid leaves the plasma and the oncotic
pressure rises as blood passes through the glomerular
capillaries.
• It is apparent that portions of the glomerular
capillaries do not normally contribute to the formation
of the glomerular ultrafiltrate; ie, exchange across the
glomerular capillaries
is flow-limited rather than
diffusion-limited
.
Changes in GFR
• Changes in renal vascular resistance as a result of
autoregulation
tend to stabilize filtration
pressure, but when the
mean systemic arterial
pressure
drops below
90 mm Hg
, there is a sharp
drop in GFR.
• The GFR tends to be maintained when
efferent
arteriolar constriction is greater than afferent
constriction
, but either type of constriction
decreases blood flow to the tubules.
Factors affecting the GFR
1. Changes in
renal blood flow .
2. Changes in glomerular capillary
hydrostatic pressure .
3. Changes in
systemic blood pressure
4. Afferent
or
efferent
arteriolar
constriction
5. Changes in
hydrostatic pressure in Bowman's
capsule
6. Ureteral obstruction
7.
Edema of kidney inside tight renal capsule
8. Changes in concentration of
plasma proteins
:
dehydration, hypoproteinemia, etc (minor factors)
9. Changes in
K
f
.
10. Changes in glomerular capillary
permeability
11. Changes in effective filtration
surface area

Filtration Fraction
• The ratio of the
GFR
to the
renal plasma flow
(RPF), the
filtration fraction
, is normally 0.16-
0.20.
• The GFR varies less than the RPF.
• When there is a fall in systemic blood
pressure, the GFR falls less than the RPF
because of efferent arteriolar constriction, and
consequently the filtration fraction rises.
