
بسم هللا الرحمن الرحيم
Renal function

Renal function
it is important to recognize that the kidneys serve
multiplefunctions, including the following:
Excretion of metabolic waste
products and foreign
chemicals
Regulation of
water and electrolyte
balances
Regulation of body fluid
osmolality
and electrolyte
concentrations
Regulation of
arterial pressure
Regulation of
acid-base balance
Secretion
,
metabolism
, and
excretion of hormones
Gluconeogenesis
Introduction
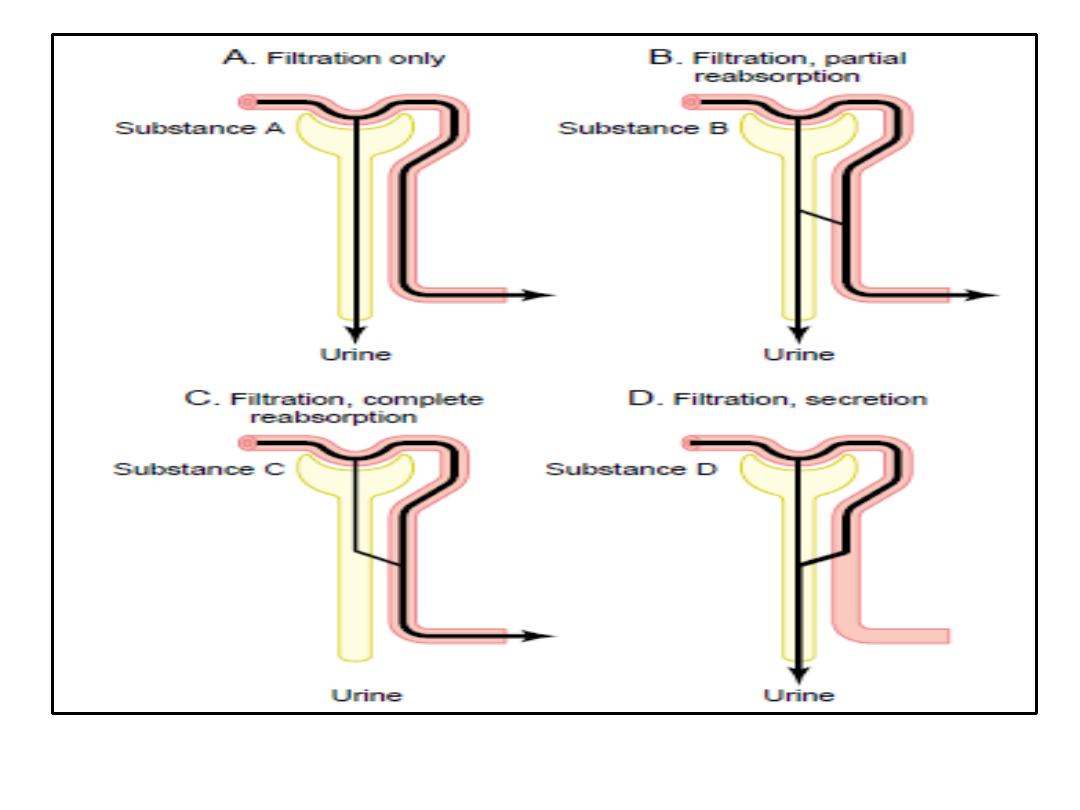
• In the kidneys, a fluid that resembles plasma is filtered
through the glomerular capillaries into the renal
tubules (
glomerular filtration
).
• As this glomerular filtrate passes down the tubules, its
volume is reduced and its composition altered by the
processes of
tubular reabsorption
(removal of water
and solutes from the tubular fluid) and
tubular
secretion
(secretion of solutes into the tubular fluid) to
form the urine that enters the renal pelvis.
•
A comparison
of the composition of the
plasma
and an
average
urine
specimen illustrates the magnitude of
some of these changes and emphasizes the manner in
which wastes are eliminated while water and
important electrolytes and metabolites are conserved.
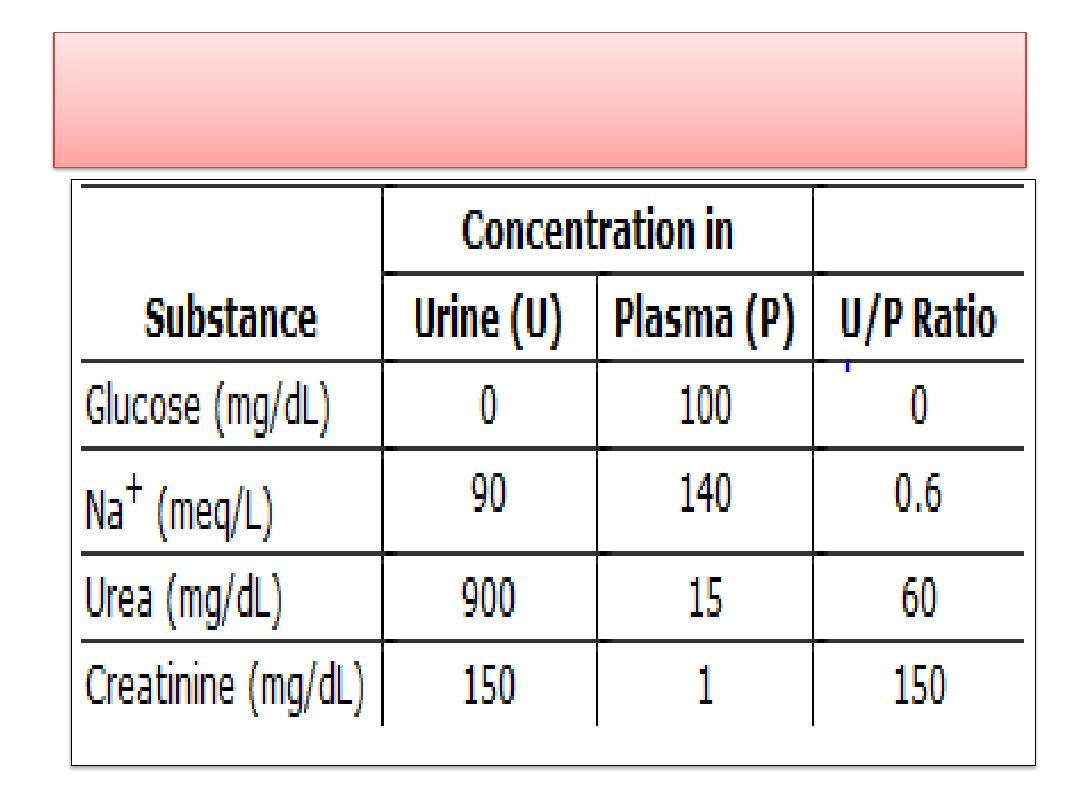
Urinary and plasma concentrations of some physiologically
important substances
.
Introduction
• Furthermore, the composition of the urine can be
varied
, and many
homeostatic regulatory
mechanisms
minimize or prevent changes in the
composition of the ECF by changing the amount
of water and various specific solutes in the urine.
• From the renal pelvis, the urine passes to the
bladder and is expelled to the exterior by the
process of urination, or
micturition
.
• The kidneys are also endocrine organs, making
kinins
and
1,25-dihydroxy-cholecalciferol
and
making and secreting
renin
.
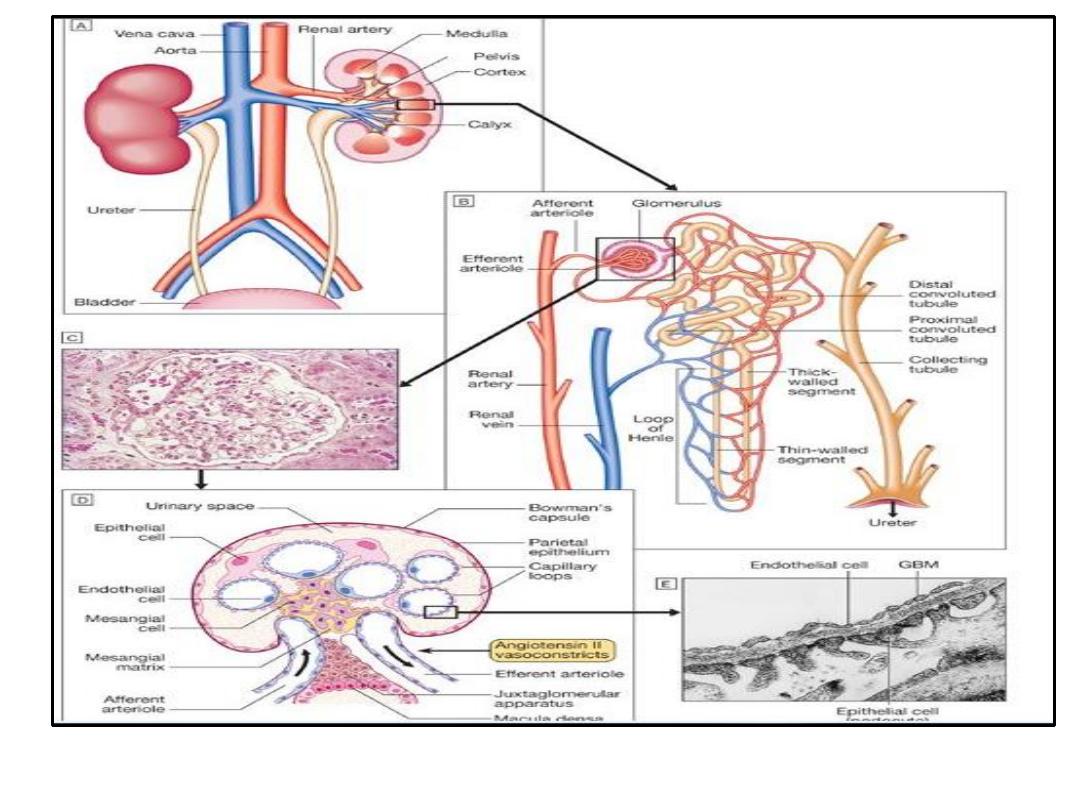
Functional anatomy
FUNCTIONAL ANATOMY
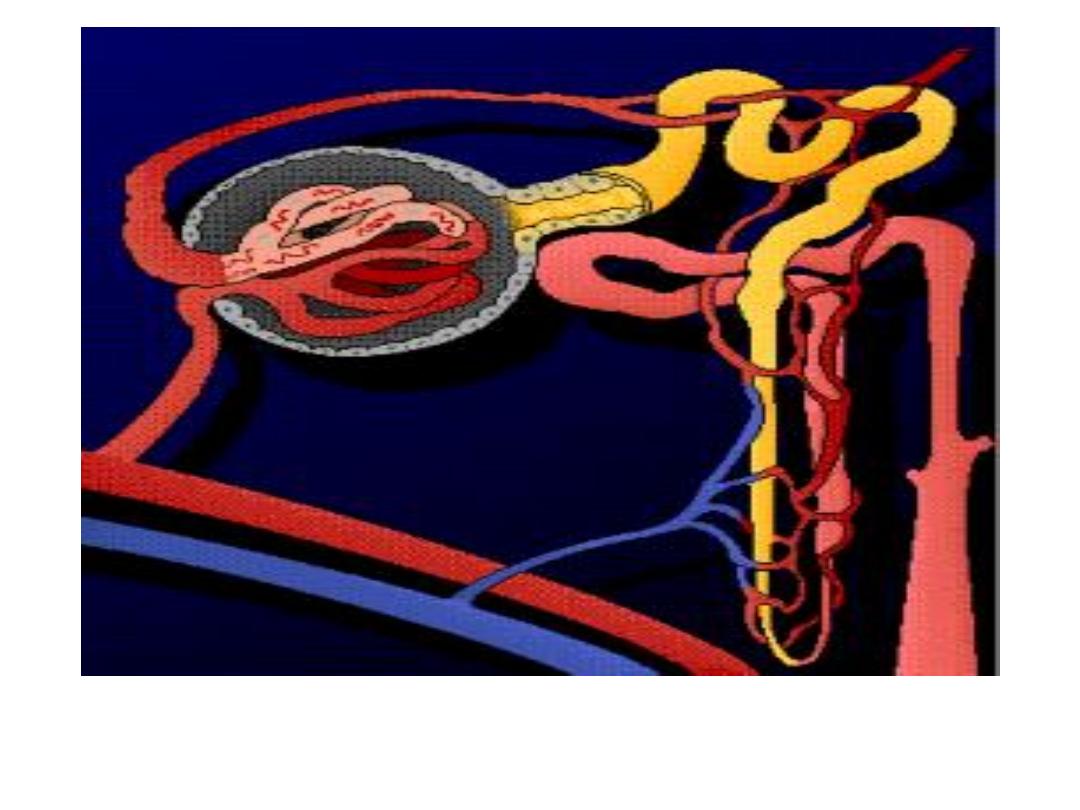
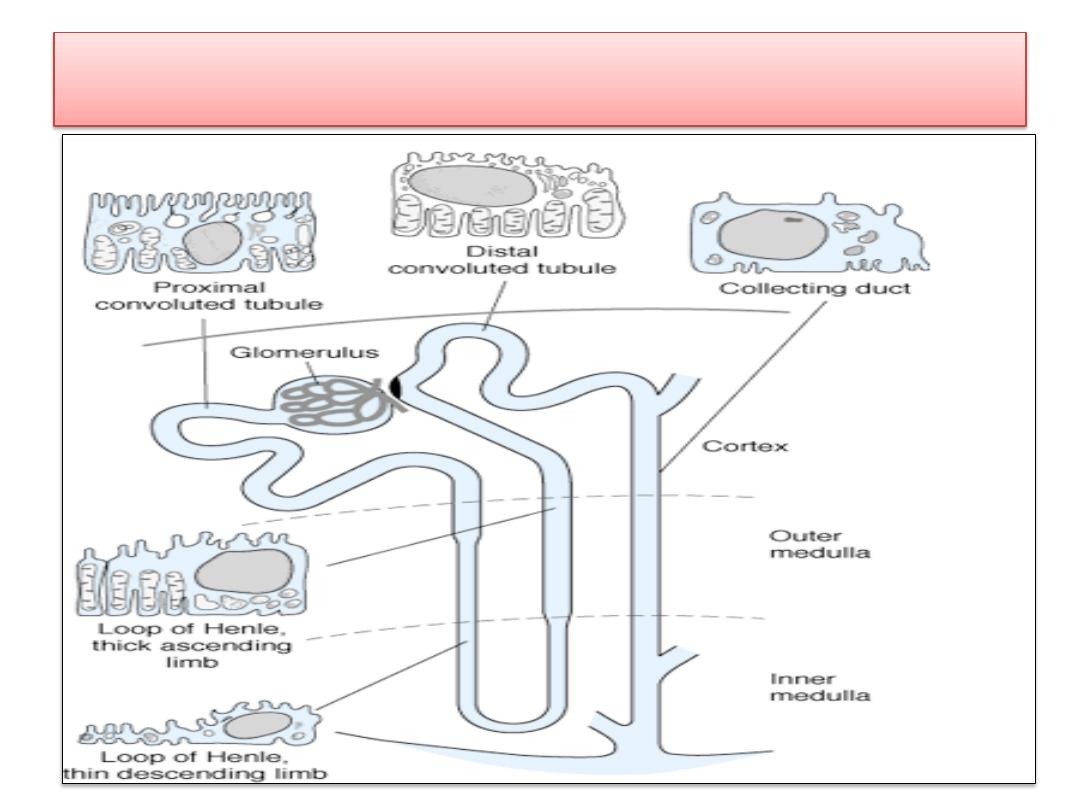
• The Nephron
Each individual renal tubule and its
glomerulus is a unit (
nephron
).
• There are approximately
1.3 million nephrons
in each
human kidney.
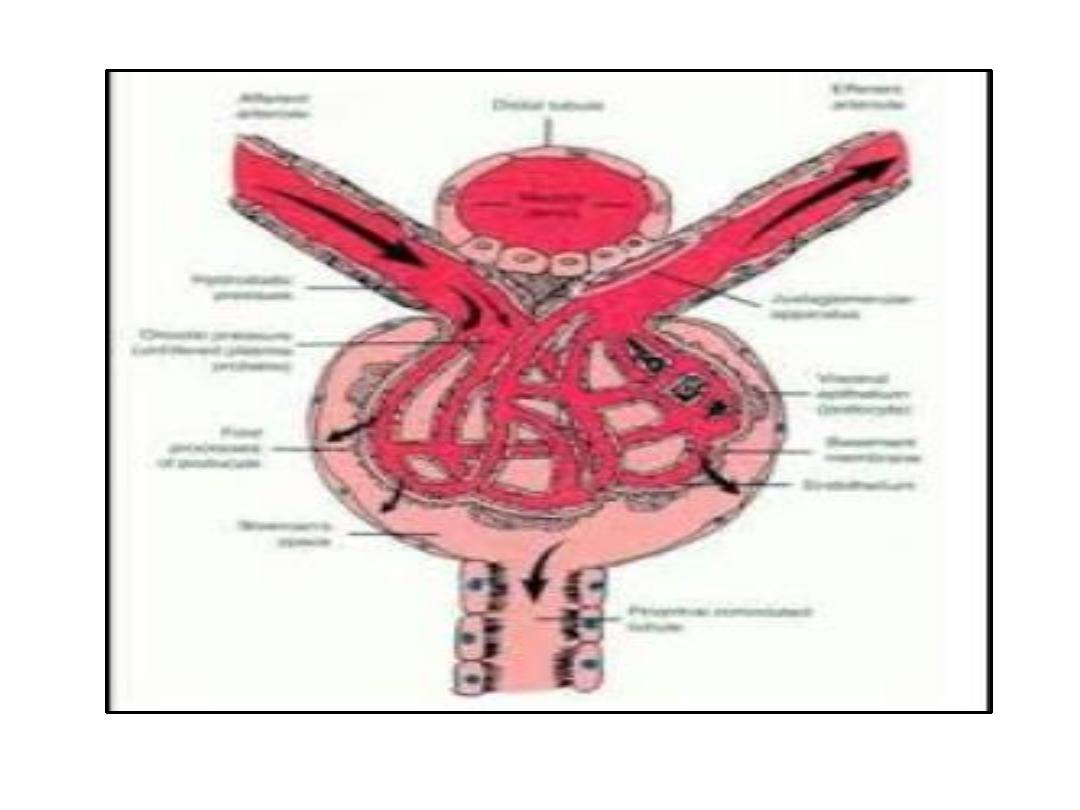
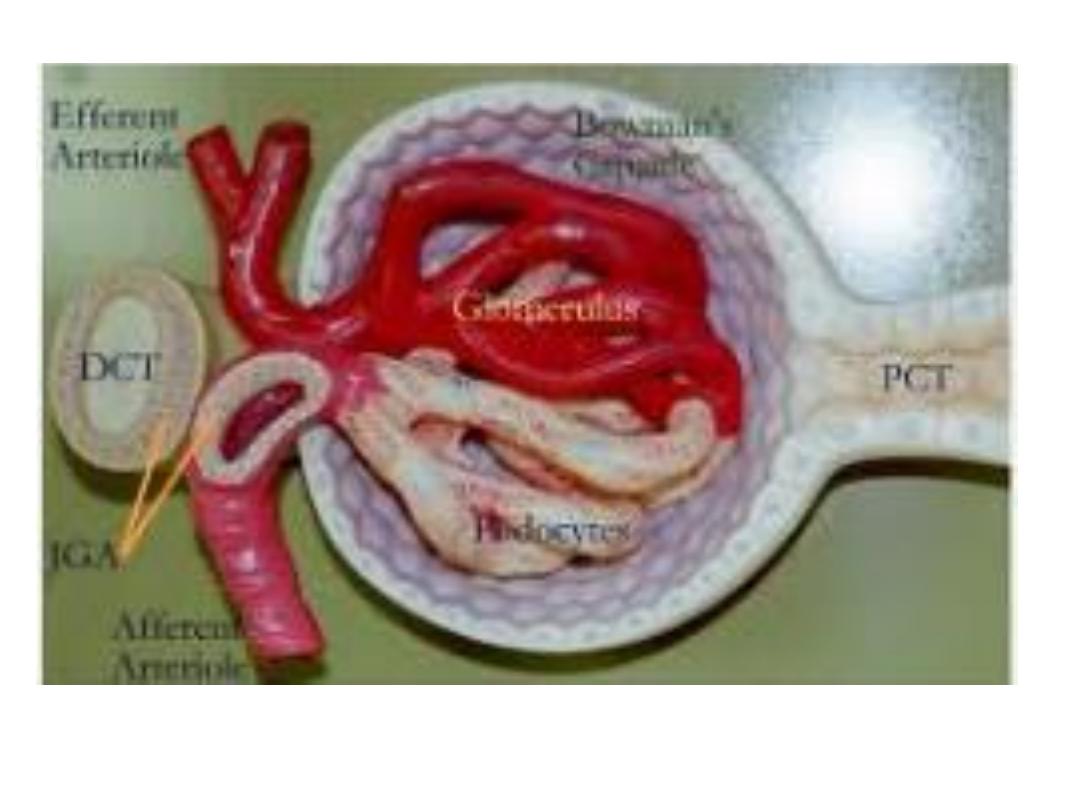
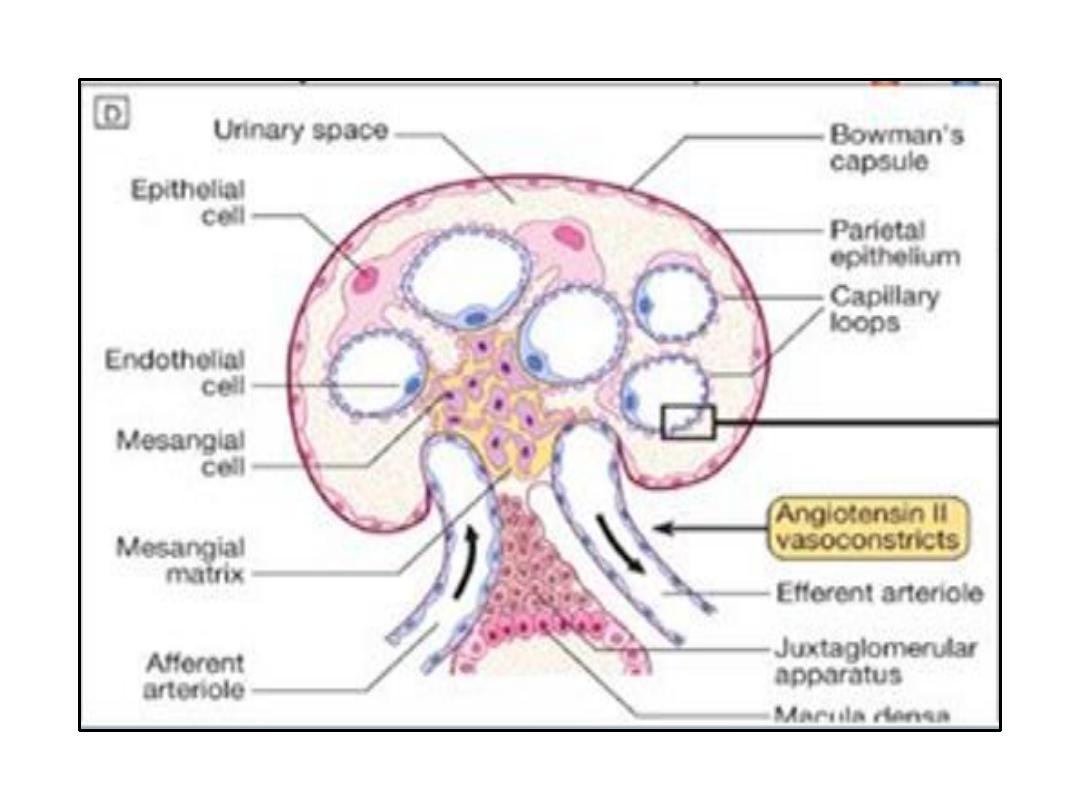
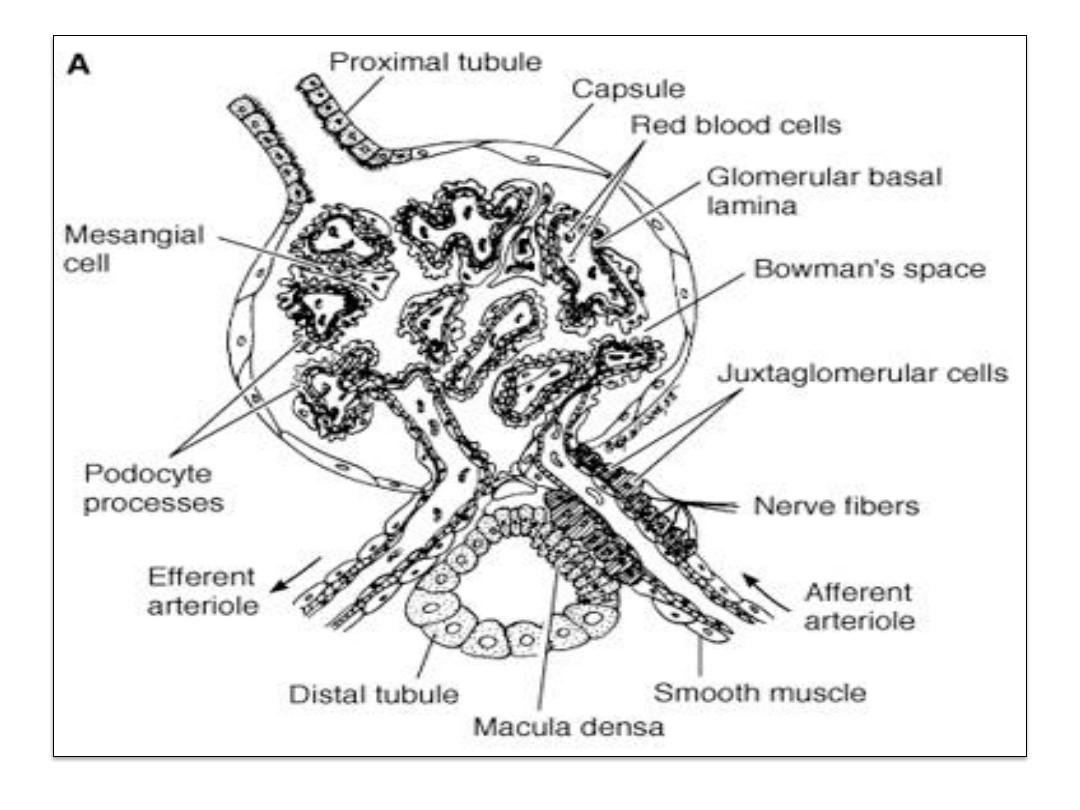
• The glomerulus, is formed by the invagination of a tuft of
capillaries into the dilated, blind end of the nephron
(
Bowman's capsule
).
• The capillaries are supplied by an
afferent arteriole
and
drained by a slightly smaller
efferent arteriole
.
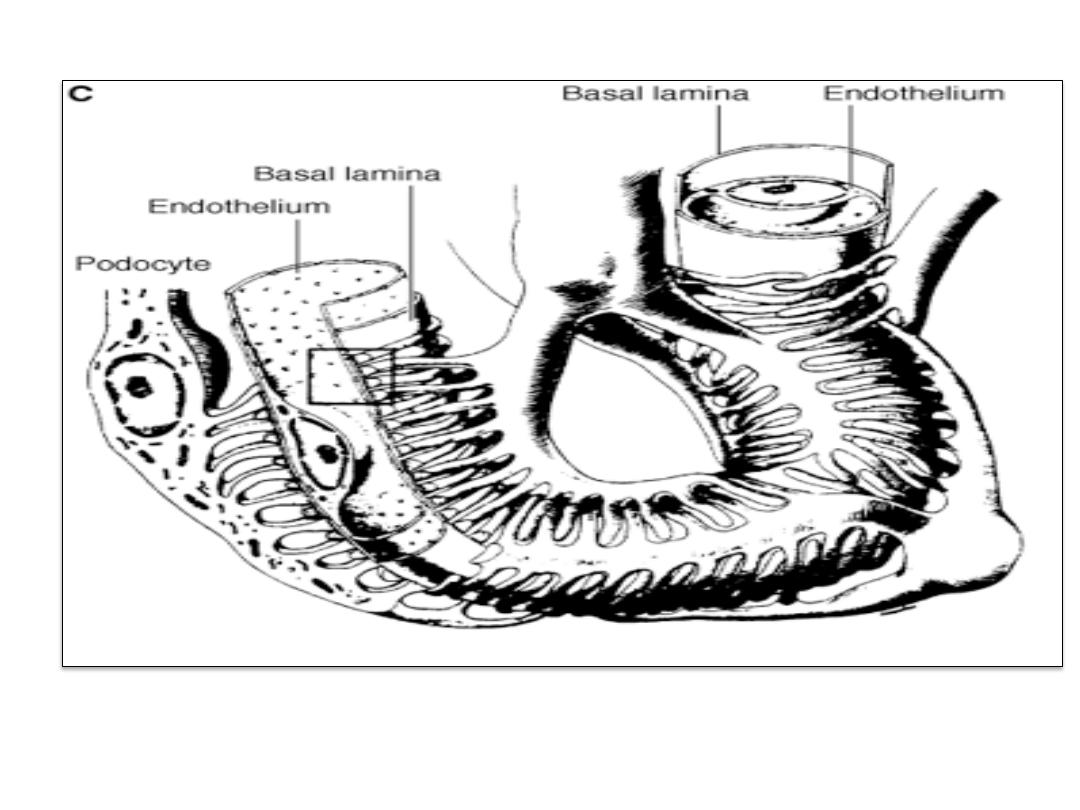
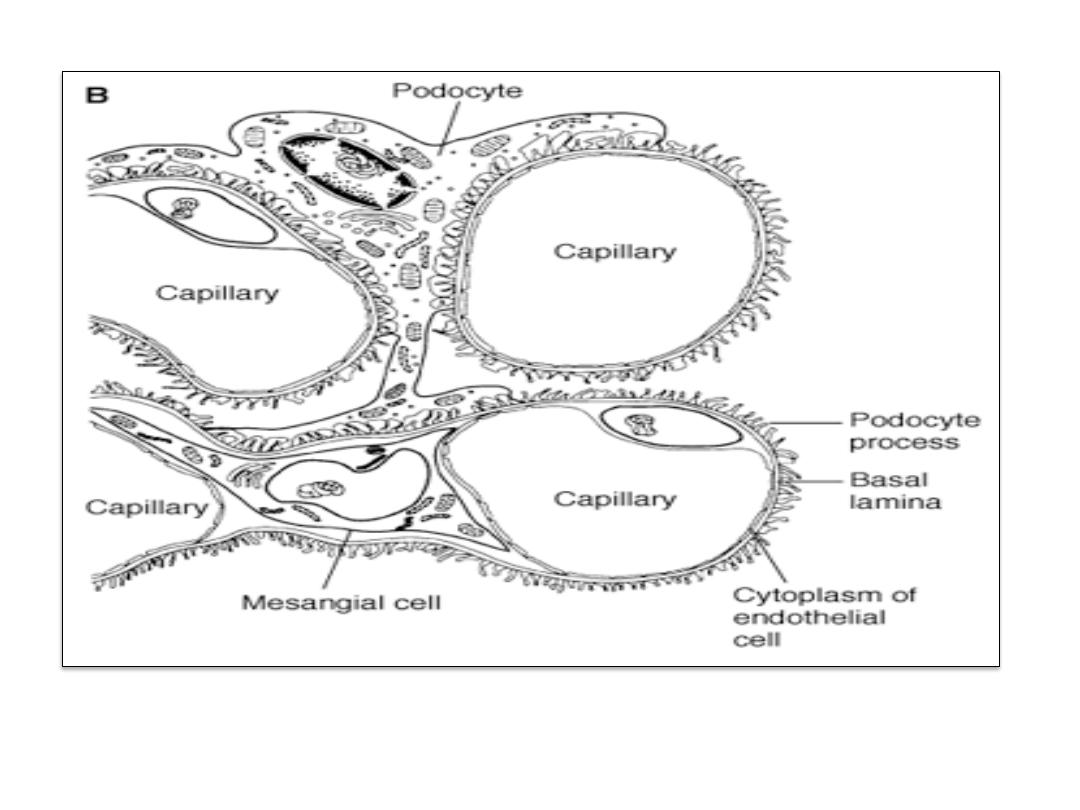
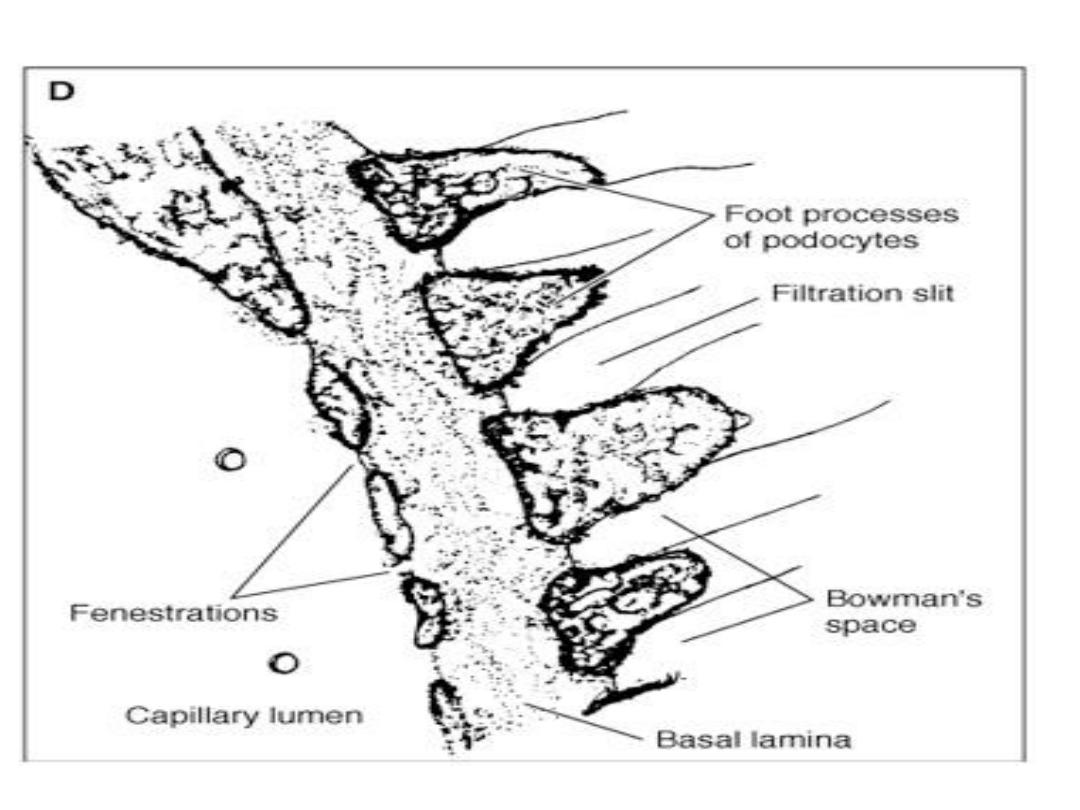
• There are two cellular layers separating the blood from the
glomerular filtrate in Bowman's capsule: the capillary
endothelium
and the specialized epithelium of the capsule
that is made up of
podocytes
overlying the glomerular
capillaries .
• These layers are separated by
a basal lamina
.
FUNCTIONAL ANATOMY
• Stellate cells called
mesangial cells
are located
between the basal lamina and the endothelium.
• Mesangial cells are especially common
between two
neighboring capillaries
, and in these locations the
basal membrane forms a sheath shared by both
capillaries
• The
mesangial cells
are
contractile
and play a role in
the regulation of glomerular filtration .
• They also secrete various substances, take up
immune complexes, and are involved in the
production of glomerular disease.

FUNCTIONAL ANATOMY
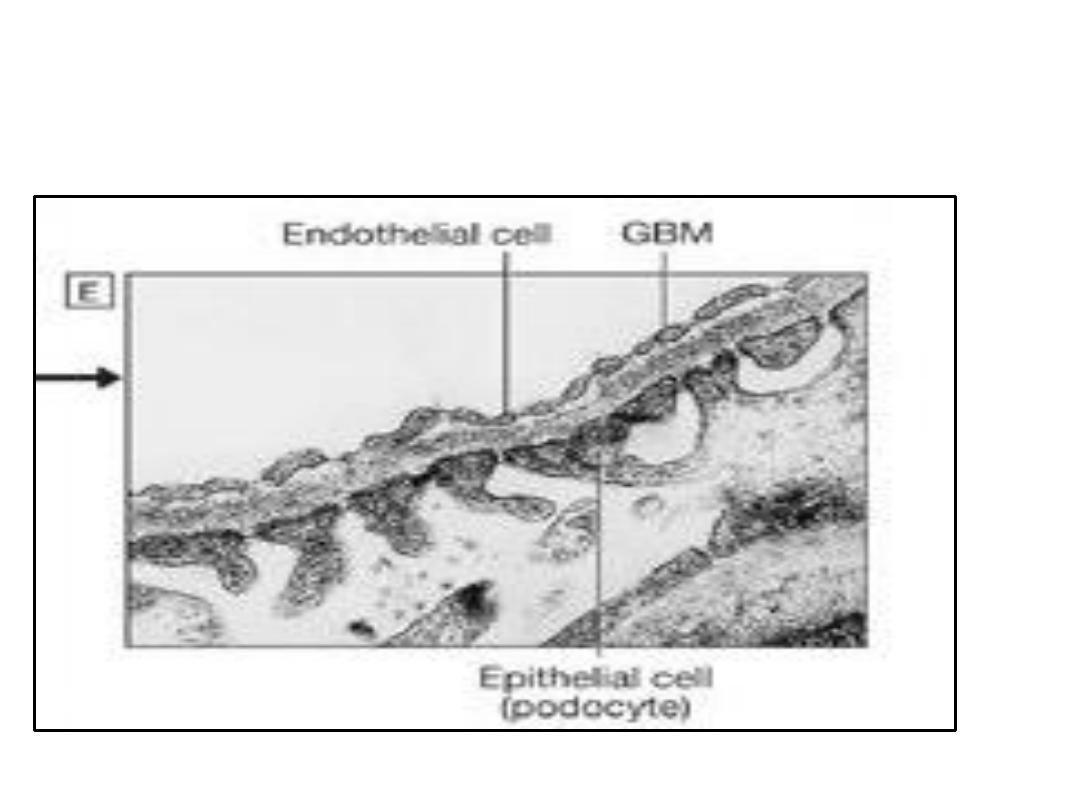
• The
endothelium
of the glomerular capillaries is
fenestrated
, with pores that are
70-90 nm
in diameter.
• The cells of the epithelium (
podocytes
) have
numerous pseudopodia that interdigitate to form
filtration slits
along the capillary wall.
• The slits are approximately
25 nm wide
, and each is
closed by a thin membrane. The basal lamina does not
contain visible gaps or pores.
• Functionally
, the glomerular membrane permits the
free passage of neutral substances up to
4 nm
in
diameter and almost totally excludes those with
diameters greater than
8 nm
.
• However, the
charges on molecules
as well as their
diameters
affect their passage into Bowman's capsule .
FUNCTIONAL ANATOMY
• The human
proximal convoluted tubule
.
• Its wall is made up of a
single layer of cells
that
interdigitate with one another and are united by
apical tight junctions.
• Between the bases of the cells, there are
extensions of the extracellular space called the
lateral intercellular spaces
.
• The luminal edges of the cells have a striate
brush border due to the presence of innumerable
microvilli
.
Functional anatomy
• The convoluted portion of the proximal tubule (
pars
convoluta
) drains into the straight portion (
pars
recta
), which forms the first part of the
loop of Henle
• The proximal tubule terminates in the thin segment
of the descending limb of the loop of Henle, which
has an
epithelium made up of attenuated, flat cells
.
• It ends in the
thick segment of the ascending
limb.
• The cells of the thick ascending limb are
cuboid
.
• They have numerous
mitochondria
, and the basilar
portions of their cell membranes are extensively
invaginated.

Functional anatomy
• The
thick ascending limb
of the loop of Henle
reaches the glomerulus of the nephron from which
the tubule arose and to its afferent arteriole and
efferent arteriole.
•
The walls of the afferent arterioles contain the
renin-secreting
juxtaglomerular cells
.
• At this point, the tubular epithelium is modified
histologically to form the
macula densa
.
•
The juxtaglomerular cells, the macula densa,
and the lacis cells near them are known
collectively as the
juxtaglomerular apparatus
.
Functional anatomy
• The
distal convoluted tubule
. the epithelium is lower than
that of the proximal tubule, and although there are a few
microvilli, there is no distinct brush border.
• The distal tubules coalesce to form
collecting ducts
and pass
through the renal cortex and medulla to empty into the pelvis
of the kidney at the apexes of the
medullary pyramids
.
• The epithelium of the collecting ducts is made up of
principal
cells
(
P cells
) and
intercalated cells
(
I cells
).
• The
P cells
, which predominate, are relatively tall and have
few organelles. They are involved in
Na
+
reabsorption and
vasopressin-stimulated water
reabsorption.
• The
I cells
, which are present in smaller numbers and are also
found in the distal tubules, have more microvilli, cytoplasmic
vesicles, and mitochondria. They are concerned with
acid
secretion and HCO
3
-
transport
.
Blood Vessels
• The
efferent arteriole
from each glomerulus
breaks up into capillaries that supply a number of
different nephrons.
•
In humans, the total surface of the renal
capillaries is approximately equal to the total
surface area of the tubules, both being about 12
m
2
.
• The volume of blood in the renal capillaries at any
given time is 30-40 mL.
THANK YOU
