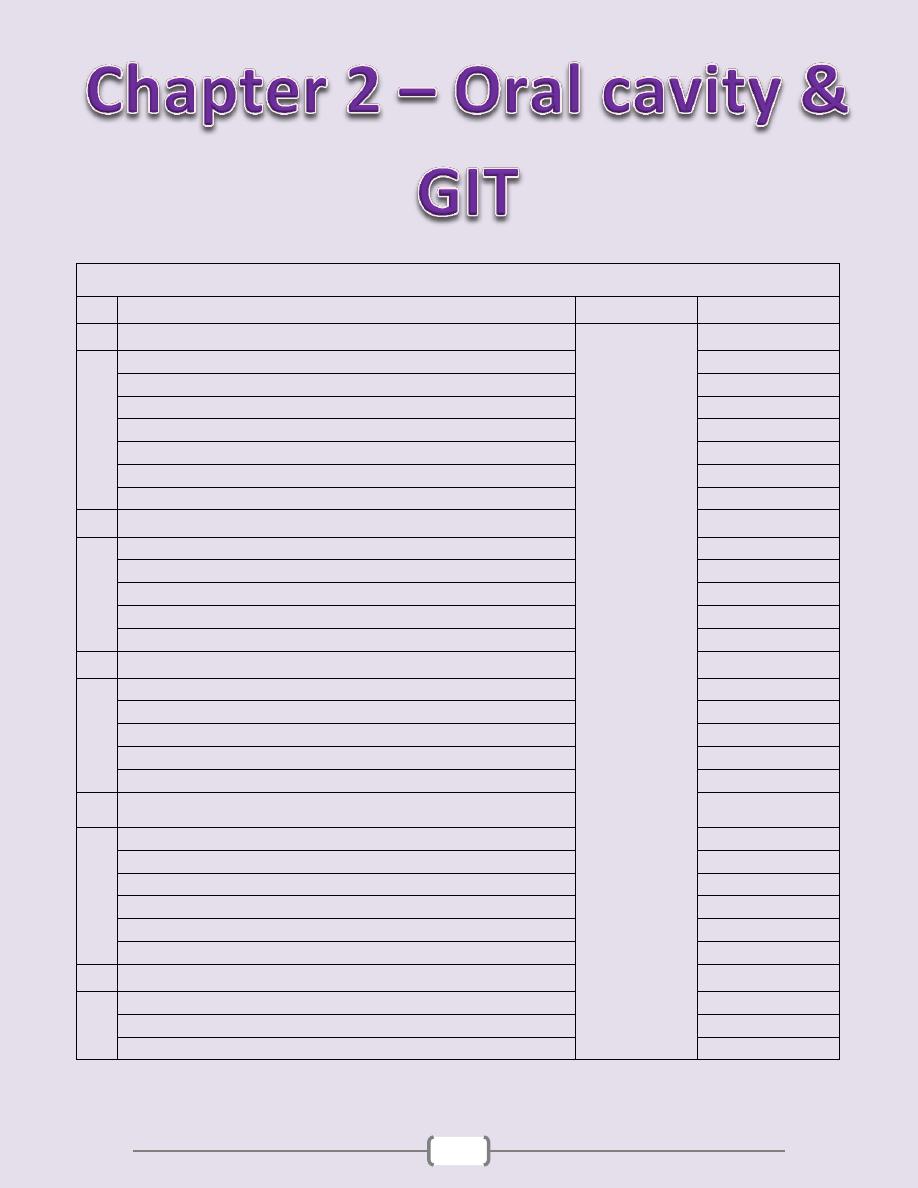
15
Chapter contents (15 – 50)
Topics
Directed by
Page number
1
Oral cavity & Oropharynx
.د
سالم
(16 - 21)
Gingivitis
16
Proliferative lesions
16
Inflammatory conditions
16
Infections
17
Oral manifestations of systemic diseases
17
Tumors & Precancerous lesions
18
Salivary Glands
19
2
Esophagus
(22 - 27)
Congenital anomalies
22
Lesions associated with motor dysfunction
22
Esophageal varices
23
Esophagitis
24
Tumors of the esophagus
26
3
Stomach
(28 - 34)
Congenital anomalies
28
Gastritis
28
Peptic ulcer
30
Acute gastric ulceration
32
Tumors of the stomach
32
4
Small & Large intestine
(35 - 49)
Congenital anomalies
35
Enterocolitis
35
Vascular diseases
44
Diverticular disease
45
Intestinal obstruction
45
Tumors of the small & large intestine
46
5
Appendix
(50)
Acute appendicitis
50
Tumors of the appendix
50
Mucocele and pseudomyxoma peritonei
50
Chapter 2 - Oral Cavity & Gastrintestinal Tract
16
“” The oral cavity & oropharynx “”
Many pathological processes can affect the constituents of the oral cavity. The more
important and frequent conditions will covered in this lecture. Diseases involving the
teeth and related structures will not be discussed.
Gingivitis
Gingivitis refers to "inflammation of soft tissues surrounding the teeth (gum)." It is
primarily due to lack of proper oral hygiene that leads to accumulation of dental plaques.
The latter consist of normal flora, proteins of saliva, and desquamated epithelial cells.
Plaques are converted to calculi through mineralization. Continuous and persistent
irritation by these calculi leads to chronic gingivitis. The condition manifests as redness,
edema, and bleeding. Eventually there is loss of soft tissue adaptation to the teeth (loose
tooth). (Fig. 5-1)
Proliferative lesions
The most common proliferative lesions of the oral cavity are
1. Irritation Fibroma and Ossifying fibroma
2. Ossifying fibroma
2. Pyogenic granuloma
3. Peripheral giant cell granuloma
Irritation fibroma
is a nodular mass of fibrous tissue that occurs mainly in the buccal
mucosa along the bite line & gingivo-dental margin. (Fig. 5-2)
Ossifying fibroma
is a common growth of the gingiva. Some may be due to maturation
of a long-standing pyogenic granuloma.
Pyogenic granuloma (granuloma pyogenicum)
is a highly vascular lesion that is
usually seen in the gingiva of children, young adults, and pregnant women (pregnancy
tumor). The lesion is typically ulcerated and bright red in color (due to rich vascularity)
(Fig. 5-3). Microscopically there is vascular proliferation similar to that of granulation
tissue. (Fig. 5-3) They lesion either regresses (particularly after pregnancy), or undergoes
fibrous maturation and may develop into ossifying fibroma.
Peripheral giant cell granuloma (giant cell epulis)
is a relatively common lesion that
characteristically protrudes from the gingiva at sites of chronic inflammation. It is so
named because microscopically there are aggregates of multinucleate giant cells separated
by a fibro-vascular stroma. (Fig. 5-4)
Inflammatory conditions
Inflammatory ulcerations
The most common inflammatory ulcerations of the oral cavity are
1)
Traumatic ulcers
, usually the result of trauma (e.g. fist fighting) or licking a jagged tooth.
2)
Aphthous ulcers
are extremely common, single or multiple, painful, recurrent,
superficial, ulcerations of the oral mucosa. The ulcer is covered by a thin yellow exudate
and rimmed by a narrow zone of erythema. (Fig. 5-5)
3)
Herpetic ulcers
(see under herpes simplex infection)
Glossitis
This is inflammation of the tongue, but sometimes it is also applied to the beefy-red
tongue that occurs in certain deficiency states. The latter is the result of atrophy of the
papillae and thinning of the mucosa, thus exposing the underlying vasculature. (Fig. 5-6)
However, in some instances, the atrophy leads to inflammation (and even shallow
ulcerations). Examples of such deficiency states that include:
1. B12 (pernicious anemia), 2. Riboflavin 3. Niacin 4. Pyridoxine 5.Iron-deficiency anemia
Plummer-Vinson syndrome
is a combination of
1. Iron-deficiency anemia 2. Glossitis 3. Esophageal dysphagia (due to esophageal webs)
Chapter 2 - Oral Cavity & Gastrintestinal Tract
17
Glossitis (with ulcerations) may also be seen with
* Jagged carious teeth * Ill-fitting dentures
* Exposure to hot fluids or corrosive chemicals
* Inhalation of burn fumes including excessive smoking
* Syphilis
Infections
1) Herpes simplex infections
Most of these are caused by herpes simplex virus (HSV) type 1 & sometimes 2. Primary
HSV infection typically occurs in children aged 2 to 4 years; is often asymptomatic, but
sometime presents as acute herpetic gingivostomatitis, characterized by vesicles and
ulcerations throughout the oral cavity. The great majority of affected adults harbor latent
HSV-1 (the virus migrates along the regional nerves and eventually becomes dormant in
the local ganglia e.g., the trigeminal). In some individuals, usually young adults, the virus
becomes reactivated to produce the common but usually mild cold sore. (Fig. 5-7)
Factors activating the virus include
1. Trauma 2. Allergies 3. Exposure to ultraviolet light (sunlight)
4. Upper respiratory tract infections 5. Pregnancy 6. Menstruation 7. Immunosuppression
The viral infection is associated with intracellular and intercellular edema, yielding clefts that
may become transformed into vesicles. The vesicles range from a few millimeters to large
ones that eventually rupture to yield extremely painful, red-rimmed, shallow ulcerations.
2) Other Viral Infections
These include
- Herpes zoster - EBV (infectious mononucleosis) - CMV - Enterovirus - Measles
3) Oral Candidiasis (thrush)
This is the most common fungal infection of the oral cavity. The thrush is a grayish white,
superficial, inflammatory psudomembrane composed of the fungus enmeshed in fibrino-
suppurative exudates. (Fig. 5-8) This can be readily scraped off to reveal an underlying
red inflammatory base. The fungus is a normal oral flora but causes troubles only
1) In the setting of immunosuppression (e.g. diabetes mellitus, organ or bone marrow
transplant recipients, neutropenia, cancer chemotherapy, or AIDS) or
2) When broad-spectrum antibiotics are taken; these eliminate or alter the normal
bacterial flora of the mouth.
3) In infants, where the condition is relatively common, presumably due to immaturity of
the immune system in them.
4) Deep Fungal Infections
Some fungal infections may extends deeply to involve the muscles & bones in relation to
oral cavity. These include, among others, histoplasmosis, blastomycosis, and
aspergillosis. The incidence of such infections has been increasing due to increasing
number of patients with AIDS, therapies for cancer, & organ transplantation
5)
Diphtheria
Characterized grossly by dirty white, fibrino-suppurative, tough, inflammatory
pseudomembrane over tonsils & posterior pharynx. (Fig. 5-9)
Oral manifestations of systemic disease
Many systemic diseases are associated with oral lesions & it is not uncommon for oral
lesions to be the first manifestation of some underlying systemic condition.
1)
Scarlet fever:
strawberry tongue: white coated tongue with hyperemic papillae projecting (Fig. 5-10)
2)
Measles:
Koplik spots: small whitish ulcerations (spots) on a reddened base, about Stensen
duct (Fig. 5-11)
3)
Diphtheria:
Dirty white, fibrinosuppurative, tough pseudomembrane over the tonsils and retropharynx
Chapter 2 - Oral Cavity & Gastrintestinal Tract
18
4)
AIDS
A. opportunistic oral infections: herpesvirus, Candida, other fungi
b. Kaposi sarcoma (Fig. 5-12)
c. hairy leukoplakia; Approximately 80% of patients with hairy leukoplakia have been
infected with HIV; the remainig 20% are seen in association with other
immunodeficiency states. The condition presents as a white fluffy ("hairy") patches that
are situated on the lateral border of the tongue. (Fig. 5-15) EBV is now accepted as the
cause of the condition. When hairy leukoplakia precedes HIV infection, manifestations of
AIDS generally appear within 2 or 3 years.
5)
AML
(especially monocytic leukemia): enlargement of the gingivae + periodontitis (Fig. 5-13)
6)
Melanotic pigmentation
(Fig. 5-14)
a. Addison disease
b. hemochromatosis
c. fibrous dysplasia of bone
d. Peutz-Jegher syndrome
7)
Pregnancy:
pyogenic granuloma ("pregnancy tumor")
Tumors and precancerous lesions
Many of the oral cavity tumors (e.g., papillomas, hemangiomas, lymphomas) are not
different from their homologous tumors elsewhere in the body. Here we will consider
only oral squamous cell carcinoma and its associated precancerous lesions.
Leukoplakia and Erythroplakia are considered premalignant lesions of squamous cell
carcinoma.
Leukoplakia
(Fig. 5-16) is a white patch that cannot be scraped off and cannot be attributed clinically
or microscopically to any other disease i.e. if a white lesion in the oral cavity can be given
a specific diagnosis it is not a leukoplakia. As such, white patches caused by entities such
as candidiasis are not leukoplakias. All leukoplakias must be considered precancerous
(have the potential to progress to squamous cell carcinoma) until proved otherwise
through histologic evaluation.
Erythroplakias
(Fig. 5-17) are red velvety patches that are much less common, yet much more serious
than leukoplakias. The incidence of dysplasia and thus the risk of complicating squamous
cell carcinoma is much more frequent in erythroplakia compared to leukoplakias.
Both leukoplakia and erythroplakia are usually found between ages of 40 and 70 years,
and are much more common in males than females. The use of tobacco (cigarettes, pipes,
cigars, and chewing tobacco) is the most common incriminated factor.
Squamous cell carcinoma
The vast majority (95%) of cancers of the head and neck are squamous cell carcinomas;
these arise most commonly in the oral cavity. The 5-year survival rate of early-stage oral
cancer is approximately 80%, but this drops to about 20% for late-stage disease. These
figures highlight the importance of early diagnosis & treatment, optimally of the
precancerous lesions.
The pathogenesis of squamous cell carcinoma is multifactorial.
1) Chronic smoking and alcohol consumption
2) Oncogenic variants of human papilloma virus (HPV). It is now known that at least
50% of oropharyngeal cancers, particularly those of the tonsils and the base of tongue,
harbor oncogenic variants of HPV.
3) Inheritance of genomic instability; a family history of head & neck cancer is a risk factor.
4) Exposure to actinic radiation (sunlight) & pipe smoking are known predisposing
factors for cancer of the lower lip.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
19
Gross features (Fig. 5-18 A)
may arise anywhere in the oral cavity, but the favored locations are
1. The tongue 2. Floor of mouth 3. Lower lip 4. Soft palate 5. Gingiva
In the early stages, cancers of the oral cavity appear as roughened areas of the mucosa. As
the lesion enlarges, it typically appears as either an ulcer or a protruding mass (fungating).
Microscopic features (Fig. 5-18 B)
Early there is full-thickness dysplasia (carcinoma in situ) followed by invasion of the
underlying connective tissue stroma.
The grade varies from from well-differentiated keratinizing to poorly differentiated.
As a group, these tumors tend to infiltrate and extend locally before they eventually
metastasize to cervical lymph nodes and more remotely. The most common sites of
distant metastasis are mediastinal lymph nodes, lung, liver and bones
Salivary glands
There are three major salivary glands—parotid, submandibular, and sublingual.
Additionally, there are numerous minor salivary glands distributed throughout the mucosa
of the oral cavity.
Xerostomia
refers to dry mouth due to a lack of salivary secretion; the causes include
1. Sjögren syndrome: an autoimmune disorder, that is usually also accompanied by
involvement of the lacrimal glands that produces dry eyes (keratoconjunctivitis sicca).
2. Radiation therapy
Inflammation (sialadenitis)
Sialadenitis refers to inflammation of a salivary gland; it may be
1) Traumatic
2) Infectious: viral, bacterial
The most common form of viral sialadenitis is mumps, which usually affects the
parotids. The pancreas and testes may also be involved.
Bacterial sialadenitis is seen as a complication of
1. Stones obstructing ducts of a major salivary gland (Sialolithiasis), particularly the
submandibular. (Fig. 5-19)
2. Dehydration with decreased secretory function as is sometimes occurs in
a. patients on long-term phenothiazines that suppress salivary secretion.
b. elderly patients with a recent major thoracic or abdominal surgery.
Unilateral involvement of a single gland is the rule & the inflammation may be suppurative.
The inflammatory involvement causes painful enlargement and sometimes a purulent
ductal discharge.
3) Autoimmune
Sjögren syndrome causes an immunolgically mediated sialadenitis i.e. inflammatory
damage of the salivary tissues.
Mucocele
This is common salivary lesion results from interruption of salivary outflow due to
blockage or rupture of a salivary gland duct. This leads to seepage of saliva into the
surrounding tissues. The lower lip is the most common location due to exposure of this
site to trauma (fist fighting, falling etc.). It presents as fluctuant swelling.
Microscopically, there is accumulation of mucin with inflammatory cells. (Fig. 5-20)
Ranula is a mucocele of the sublingual gland; it may become extremely large.
Neoplasms of salivary glands
Neoplasms of the salivary glands (benign and malignant) are generally uncommon,
constituting less than 2% of human tumors. We will restrict our discussion on the more
common examples.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
20
The relative frequency distributions of these tumors in relation to various salivary glands
are as follows
Salivary gland
Relative frequency of tumors (%)
Parotid gland
80%
Submandibular gland
10%
Minor salivary and sublingual glands
10%
The incidence of malignant tumors within the glands is, however, different from the
above
Salivary gland affected
Relative frequency of malignant tumors (%)
Sublingual tumors
80%
Minor salivary glands
50%
Submandibular glands
40%
Parotid glands
25%
These tumors usually occur in adults, with a slight female predominance. Excluded from
this rule is Warthin tumor, which occurs much more frequently in males than in females.
The benign tumors occur most often around the age of 50 to 60 years; the malignant ones
tend to appear in older age groups. Neoplasms of the parotid produce distinctive swellings
in front of, or below the ear. Clinically, there are no reliable criteria to differentiate benign
from the malignant tumors; therefore, pathological evaluation is necessary. (Fig. 5-21)
Pleomorphic Adenomas (Mixed Salivary Gland Tumors)
These benign tumors commonly occur within the parotid gland (constitute 60% of all
parotid tumors).
o Gross features (Fig. 5-22 A)
Most tumors are rounded, encapsulated masses.
The cut surface is gray-white with myxoid and light blue translucent areas of chondroid.
o Microscopic features (Fig. 5-22 B)
The main constituents are a mixture of ductal epithelial and myoepithelial cells, and it is
believed that all the other elements, including mesenchymal, are derived from the above
cells (hence the name adenoma).
The epithelial/myoepithelial components of the neoplasm are arranged as glands, strands,
or sheets. These various epithelial/myoepithelial elements are dispersed within a
background of loose myxoid tissue that may contain islands of cartilage-like islands and,
rarely bone. Sometimes, squamous differentiation is present.
In some instances, the tumor capsule is focally deficient allowing the tumor to extend as
tongue-like protrusions into the surrounding normal tissue.
Enucleation of the tumor is, therefore, not advisable because residual foci (the protrusions)
may be left behind and act as a potential source of multifocal recurrences. (Fig. 5-23)The
incidence of malignant transformation increases with the duration of the tumor.
Warthin Tumor
Is the second most common salivary gland neoplasm. It is benign, arises usually in the
parotid gland and occurs more commonly in males than in females. About 10% are
multifocal and 10% bilateral. Smokers have a higher risk than nonsmokers for developing
these tumors. Grossly, it is round to oval, encapsulated mass & on section display gray
tissue with narrow cystic or cleft-like spaces filled with secretion. Microscopically, these
spaces are lined by a double layer of neoplastic epithelial cells resting on a dense
lymphoid stroma, sometimes with germinal centers. This lympho-epithelial lining
frequently project into the spaces. The epithelial cells are oncoytes as evidenced by their
eosinophilic granular cytoplasm (stuffed with mitochondria). (Fig. 5-24)
Mucoepidermoid Carcinoma
As the name indicates, these neoplasms are composed of variable mixtures of mucus-
secreting cells (muco), and squamous cells (epidermoid). They are the most common form
of primary malignant tumor of the salivary glands. They occur mainly in the parotids.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
21
Low-grade tumors may invade locally but do not metastasize. By contrast, high-grade
neoplasms metastasize to distant sites in 30% of cases. Grossly, mucoepidermoid
carcinomas are gray-white, infiltrative tumors that frequently show small, mucin-
containing cysts. Microscopically, there are cords, sheets, and cysts of squamous and
mucous-secreting cells. (Fig. 5-25)
Other Salivary Gland Tumors
Two less common neoplasms worth brief description:
o Adenoid cystic carcinoma: half of the cases are found in the minor salivary glands (in
particular the palate). Although slow growing, they have a tendency to invade perineural
spaces and to recur. Eventually, 50% or more disseminate widely to distant sites such as
bone, liver, and brain. Microscopically, they are composed of small cells having dark,
compact nuclei and scant cytoplasm. These cells tend to be disposed in sieve-like
(cribriform) patterns. The spaces between the tumor cells are often filled with a hyaline
material thought to represent excess basement membrane. (Fig. 5-26)
o Acinic cell tumor is composed of cells resembling the normal acinar cells (hence the
name). Most arise in the parotids; the small remainder arises in the submandibular glands.
On histologic examination, they reveal a variable architecture and cell morphology. Most
characteristically, the cells have clear cytoplasm & are disposed in sheets, microcysts,
glands, or papillae. About 10% to 15% of these neoplasms metastasize to lymph nodes.
(Fig. 5-27)
Chapter 2 - Oral Cavity & Gastrintestinal Tract
22
Esophagus
The main functions of the esophagus are to 1. Conduct food and fluids from the pharynx to
the stomach 2. Prevent reflux of gastric contents into the esophagus. These functions
require motor activity coordinated with swallowing, i.e. wave of peristalsis, associated
with relaxation of the LES in anticipation of the peristaltic wave. This is followed by
closure of the LES after the swallowing reflex. Maintenance of sphincter tone (positive
pressure relative to the rest of esophagus) is necessary to prevent reflux of gastric contents.
Congenital anomalies
Several congenital anomalies affect the esophagus including
The presence of
ectopic
gastric mucosa & pancreatic tissues within the esophageal wall,
congenital cysts
&
congenital herniation
of the esophageal wall into the thorax. The
latter is due to impaired formation of the diaphragm.
Atresia and fistulas
are uncommon but must be recognized & corrected early because
they cause immediate regurgitation, suffocation & aspiration pneumontis when feeding is
attempted. In atresia, a segment of the esophagus is represented by only a noncanalized
cord, with the upper pouch connected to the bronchus or the trachea and a lower pouch
leading to the stomach. (Fig. 5-28)
Webs, rings, and stenosis
(Fig. 5-29)
Mucosal webs
are shelf-like, eccentric protrusions of the mucosa into the esophageal
lumen. These are most common in the upper esophagus. The triad of upper esophageal
web, iron-deficiency anemia, and glossitis is referred to as Plummer-Vinson syndrome.
This condition is associated with an increased risk for postcricoid esophageal carcinoma.
Esophageal rings
unlike webs are concentric plates of tissue protruding into the lumen of
the distal esophagus. Esophageal webs and rings are encountered most frequently in
women over age 40. Episodic dysphagia is the main symptom.
Stenosis
consists of fibrous thickening of the esophageal wall. Although it may be
congenital, it is more frequently the result of severe esophageal injury with inflammatory
scarring, as from gastroesophageal reflux disease (GERD), radiation, scleroderma and
caustic injury. Stenosis usually manifests as progressive dysphagia, at first to solid foods
but eventually to fluids as well.
Lesions associated with motor dysfunction (fig. 5-30)
Coordinated motor activity is important for proper function of the esophagus. The major
entities that are caused by motor dysfunction of the esophagus are
1. Achalasia 2. Hiatal hernia 3. Diverticula 4. Mallory-Weiss tear
Achalasia
Achalasia means "failure to relax." It is characterized by three major abnormalities:
1. Aperistalsis (failure of peristalsis)
2. Increased resting tone of the LES
3. Icomplete relaxation of the LES in response to swallowing
In most instances, achalasia is an idiopathic disorder. In this condition there is progressive
dilation of the esophagus above the persistently contracted LES. The wall of the
esophagus may be of normal thickness, thicker than normal owing to hypertrophy of the
muscular wall, or markedly thinned by dilation (when dilatation overruns hypertrophy).
The mucosa just above the LES may show inflammation and ulceration. Young adults are
usually affected and present with progressive dysphagia. (Fig. 5-31)
Complications of achalasia are
1. Aspiration pneumonitis of undigested food 2. Monilial esophagitis
3. Esophageal squamous cell carcinoma (about 5% of patients)
4. Lower esophageal diverticula
Chapter 2 - Oral Cavity & Gastrintestinal Tract
23
Hiatal Hernia (Fig. 5-32)
Hiatal hernia is characterized by separation of the diaphragmatic crura leading to
widening of the space around the esophageal wall. Two types of hiatal hernia are
recognized: 1. The sliding type (95%)
2. The paraesophageal type
In the sliding hernia the stomach skates up through the patent hiatus above the diaphragm
creating a bell-shaped dilation. In paraesophageal hernias, a separate portion of the
stomach, usually along the greater curvature, enters the thorax through the widened
foramen. The cause of hiatal hernia is unknown. It is not clear whether it is a congenital
malformation or is acquired during life. Only about 10% of adults with a sliding hernia
suffer from heartburn or regurgitation of gastric juices into the mouth. These are due to
incompetence of the LES and are accentuated by positions favoring reflux (bending
forward, lying supine) and obesity.
Complications of hiatal hernias include
1. Ulceration, bleeding and perforation (both types)
2. Reflux esophagitis (frequent with sliding hernias)
3. Strangulation of paraesophageal hernias
Diverticula
(Fig. 5-33)
By definition a diverticulum is a "focal out pouching of the alimentary tract wall that
contains all or some of its constituents"; they are divided into
1. False diverticulum
is an out pouching of the mucosa and submucosa through weak
points in the muscular wall.
2. True diverticulum
consists of all the layers of the wall and is thought to be due to
motor dysfunction of the esophagus. They may develop in three regions of the esophagus
a. Zenker diverticulum, located immediately above the UES
b. Traction diverticulum near the midpoint of the esophagus
c. Epiphrenic diverticulum immediately above the LES.
Lacerations (Mallory-Weiss Syndrome)
These refer to longitudinal tears at the GEJ or gastric cardia and are the consequence of
severe retching or vomiting. They are encountered most commonly in alcoholics, since
they are susceptible to episodes of excessive vomiting, but have been reported in persons
with no history of vomiting or alcoholism. During episodes of prolonged vomiting, reflex
relaxation of LES fails to occur. The refluxing gastric contents suddenly overcome the
contracted musculature leading to forced, massive dilation of the lower esophagus with
tearing of the stretched wall.
Pathological features
The linear irregular lacerations, which are usually found astride the GEJ or in the gastric
cardia, are oriented along the axis of the esophageal lumen. The tears may involve only
the mucosa or may penetrate deeply to perforate the wall. (Fig. 5-34) Infection of the
mucosal defect may lead to inflammatory ulcer or to mediastinitis. Usually the bleeding is
not profuse and stops without surgical intervention. Healing is the usual outcome. Rarely
esophageal rupture occurs.
Esophageal Varices
Portal hypertension when sufficiently prolonged or severe induces the formation of
collateral bypass veins wherever the portal and caval venous systems communicate.
Esophageal varices refer to the prominent plexus of deep mucosal and submucosal venous
collaterals of the lower esophagus subsequent to the diversion of portal blood through
them through the coronary veins of the stomach. From the varices the blood is diverted
into the azygos veins, and eventually into the systemic veins. Varices develop in 90% of
Chapter 2 - Oral Cavity & Gastrintestinal Tract
24
cirrhotic patients. Worldwide, after alcoholic cirrhosis, hepatic schistosomiasis is the
second most common cause of variceal bleeding.
Pathological features (Fig. 5-35)
The increased pressure in the esophageal plexus produces dilated tortuous vessels that are
liable to rupture.
Varices appear as tortuous dilated veins lying primarily within the submucosa of the distal
esophagus and proximal stomach.
The net effect is irregular protrusion of the overlying mucosa into the lumen. The mucosa
is often eroded because of its exposed position.
Variceal rupture produces massive hemorrhage into the lumen. In this instance, the
overlying mucosa appears ulcerated and necrotic.
Rupture of esophageal varices usually produces massive hematemesis. Among patients
with advanced liver cirrhosis, such a rupture is responsible for 50% of the deaths. Some
patients die as a direct consequence of the hemorrhage (hypovolemic shock); others of
hepatic coma triggered by the hemorrhage.
Esophagitis
This term refers to inflammation of the esophageal mucosa. It may be caused by a variety
of physical, chemical, or biologic agents.
Reflux Esophagitis (Gastroesophageal Reflux Disease or GERD)
Is the most important cause of esophagitis & signifies esophagitis associated with reflux of
gastric contents into the lower esophagus. Many causative factors are involved, the most
important is decreased efficacy of esophageal antireflux mechanisms, particularly LES tone.
In most instances, no cause is identified. However, the following may be contributatory
a. Central nervous system depressants including alcohol
b. Smoking
c. Pregnancy
d. Nasogastric tube
e. Sliding hiatal hernia
f. hypothyroidism
g. Systemic sclerosis
Any one of the above mechanism may be the primary cause in an individual case, but
more than one is likely to be involved in most instances. The action of gastric juices is
vital to the development of esophageal mucosal injury.
Gross (endoscopic) features (Fig. 5-36 A)
These depend on the causative agent and on the duration and severity of the exposure.
Mild esophagitis may appear grossly as simple hyperemia. In contrast, the mucosa in
severe esophagitis shows confluent erosions or total ulceration into the submucosa.
Microscopic features (Fig. 5-36 B)
Three histologic features are characteristic:
1. Inflammatory cells including eosinophils within the squamous mucosa.
2. Basal cells hyperplasia
3. Extension of lamina propria papillae into the upper third of the mucosa.
The disease mostly affects those over the age of 40 years. The clinical manifestations
consist of dysphagia, heartburn, regurgitation of a sour fluid into the mouth, hematemesis,
or melena. Rarely, there are episodes of severe chest pain that may be mistaken for a
"heart attack."
The potential consequences of severe reflux esophagitis are
1. Bleeding
2. Ulceration
3. Stricture formation
4. Tendency to develop Barrett esophagus
Chapter 2 - Oral Cavity & Gastrintestinal Tract
25
Barrett Esophagus (BE)
o 10% of patients with long-standing GERD develop this complication. BE is the single
most important risk factor for esophageal adenocarcinoma. BE refers to columnar
metaplasia of the distal squamous mucosa; this occurs in response to prolonged injury
induced by refluxing gastric contents. Two criteria are required for the diagnosis of
Barrett esophagus:
1. Endoscopic evidence of columnar lining above the GEJ
2. Histologic confirmation of the above in biopsy specimens.
The pathogenesis of Barrett esophagus appears to be due to a change in the differentiation
program of stem cells of the esophageal mucosa. Since the most frequent metaplastic
change is the presence of columnar cells admixed with goblet cells, the term "intestinal
metaplasia" is used to describe the histological alteration.
o Gross features
Barrett esophagus is recognized as a red, velvety mucosa located between the smooth,
pale pink esophageal squamous mucosa and the light brown gastric mucosa.
It is displayed as tongues, patches or broad circumferential bands replacing the
squamocolumnar junction several centimeters. (Fig. 5-37 A)
o Microscopic features
the esophageal squamous epithelium is replaced by metaplastic columnar epithelium,
including interspersed goblet cells, & may show a villous pattern (as that of the small
intestine hence the term intestinal metaplasia). (Fig. 5-37 B)
Critical to the pathologic evaluation of patients with Barrett mucosa is the search for
dysplasia within the metaplastic epithelium. This dysplastic change is the presumed
precursor of malignancy (adenocarcinoma). Dysplasia is recognized by the presence of
cytologic and architectural abnormalities in the columnar epithelium, consisting of
enlarged, crowded, and stratified hyperchromatic nuclei with loss of intervening stroma
between adjacent glandular structures. Depending on the severity of the changes,
dysplasia is classified as low-grade or high-grade.
Approximately 50% of patients with high-grade dysplasia may already have adjacent
adenocarcinoma.
o Most patients with the first diagnosis of Barrett esophagus are between 40 and 60 years.
Barrett esophagus is clinically significant due to
1. The secondary complications of local peptic ulceration with bleeding and stricture.
2. The development of adenocarcinoma, which in patients with long segment disease
(over 3 cm of Barrett mucosa), occurs at a frequency that is 30- to 40 times greater than
that of the general population.
Other causes of esophagitis
In addition to GERD (which is, in fact, a chemical injury), esophageal inflammation may
have many origins. Examples include ingestion of mucosal irritants (such as alcohol,
corrosive acids or alkalis as in suicide attempts), cytotoxic anticancer therapy, bacteremia
or viremia (in immunosuppressed patients), fungal infection (in debilitated or
immunosuppressed patients or during broad-spectrum antimicrobial therapy; candidiasis
by far the most common), and uremia.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
26
Tumors
Benign Tumors
Leiomyomas are the most common benign tumors of the esophagus. (Fig. 5-38)
Malignant Tumors
Carcinomas of the esophagus (5% of all cancers of the GIT) have, generally, a poor
prognosis because they are often discovered too late. Worldwide, squamous cell
carcinomas constitute 90% of esophageal cancers, followed by adenocarcinoma.
Other tumors are rare.
Squamous Cell Carcinoma (SCC)
o Most SCCs occur in adults over the age of 50. The disease is more common in males than
females. The regions with high incidence include Iran & China. Blacks throughout the
world are at higher risk than are whites.
o Etiology and Pathogenesis
Factors Associated with the Development of Squamous Cell Carcinoma of the Esophagus
are classified as
1. Dietary
Deficiency of vitamins (A, C, riboflavin, thiamine, and pyridoxine) & trace elements (zinc)
Fungal contamination of foodstuffs
High content of nitrites/nitrosamines
Betel chewing (betel: the leaf of a climbing evergreen shrub, of the pepper family, which
is chewed in the East with a little lime.)
2. Lifestyle
Burning-hot food
Alcohol consumption
Tobacco abuse
3. Esophageal Disorders
Long-standing esophagitis
Achalasia
Plummer-Vinson syndrome
4. Genetic Predisposition
Long-standing celiac disease - Racial disposition
The marked geographical variations in the incidence of the disease strongly implicate
dietary and environmental factors, with a contribution from genetic predisposition. The
majority of cancers in Europe and the United States are attributable to alcohol and
tobacco. Some alcoholic drinks contain significant amounts of such carcinogens as
polycyclic hydrocarbons, nitrosamines, and other mutagenic compounds. Nutritional
deficiencies associated with alcoholism may contribute to the process of carcinogenesis.
Human papillomavirus DNA is found frequently in esophageal squamous cell
carcinomas from high-incidence regions.
o Gross features (Fig. 5-39 A)
Like squamous cell carcinomas arising in other locations, those of the esophagus begin as
in situ lesions.
When they become overt, about 20% of these tumors are located in the upper third, 50%
in the middle third, and 30% in the lower third of the esophagus.
Early lesions appear as small, gray-white, plaque-like thickenings of the mucosa but with
progression, three gross patterns are encountered:
1. Fungating (polypoid) (60%) that protrudes into the lumen
2. Flat (diffusely infiltrative) (15%) that tends to spread within the wall of the esophagus,
causing thickening, rigidity, and narrowing of the lumen
3. Excavated (ulcerated) (25%) that digs deeply into surrounding structures and may
erode into the respiratory tree (with resultant fistula and pneumonia) or aorta (with
catastrophic bleeding) or may permeate the mediastinum and pericardium.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
27
Local extension into adjacent mediastinal structures occurs early, possibly due to the
absence of serosa for most of the esophagus. Tumors located in the upper third of the
esophagus also metastasize to cervical lymph nodes; those in the middle third to the
mediastinal, paratracheal, and tracheobronchial lymph nodes; and those in the lower third
most often spread to the gastric and celiac groups of nodes.
o Microscopic features (Fig. 5-39 B)
Most squamous cell carcinomas are moderately to well-differentiated,
They are invasive tumors that have infiltrated through the wall or beyond.
The rich lymphatic network in the submucosa promotes extensive circumferential and
longitudinal spread.
o Esophageal carcinomas are usually quite large by the time of diagnosis, produces
dysphagia and obstruction gradually. Cachexia is frequent. Hemorrhage and sepsis may
accompany ulceration of the tumor.
The five-year survival rate in patients with superficial esophageal carcinoma is about
75%, compared to 25% in patients who undergo "curative" surgery for more advanced
disease. Local recurrence and distant metastasis following surgery are common. The
presence of lymph node metastases at the time of resection significantly reduces survival.
Adenocarcinoma
With increasing recognition of Barrett mucosa, most adenocarcinomas in the lower third
of the esophagus arise from the Barrett mucosa.
o Etiology and Pathogenesis
These focus on Barrett esophagus. The lifetime risk for cancer development from Barrett
esophagus is approximately 10%. Tobacco exposure and obesity are risk factors.
Helicobacter pylori infection may be a contributing factor.
o Gross features: (Fig. 5-40 A)
Adenocarcinomas arising in the setting of Barrett esophagus are usually located in the
distal esophagus and may invade the adjacent gastric cardia.
As is the case with squamous cell carcinomas, adenocarcinomas initially appear as flat
raised patches that may develop into large nodular fungating masses or may exhibit
diffusely infiltrative or deeply ulcerative features.
o Microscopic features (Fig. 5-40 B)
Most tumors are mucin-producing glandular tumors exhibiting intestinal-type features.
Multiple foci of dysplastic mucosa are frequently present adjacent to the tumor.
o Adenocarcinomas arising in Barrett esophagus chiefly occur in patients over the age of 40
years and similar to Barrett esophagus, it is more common in men than in women, and in
whites more than blacks (in contrast to squamous cell carcinomas). As in other forms of
esophageal carcinoma, patients usually present because of difficulty swallowing,
progressive weight loss, bleeding, and chest pain. The prognosis is as poor as that for
other forms of esophageal cancer, with under 20% overall five-year survival.
Identification and resection of early cancers with invasion limited to the mucosa or
submucosa improves five-year survival to over 80%. Regression or surgical removal of
Barrett esophagus has not yet been shown to eliminate the risk for adenocarcinoma.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
28
Stomach
In developed countries, peptic ulcers occur in up to 10% of the general population.
Chronic infection of the gastric mucosa by the bacterium H. pylori is the most common
infection worldwide. Gastric cancer is still a significant cause of death, despite its
decreasing incidence.
Congenital anomalies
These include
Various
heterotopias
(normal tissues in abnormal locations), which are usually
asymptomatic, e.g. pancreatic heterotopia.
Congenital diaphgramatic hernia
, which is due to defective closure of the diaphragm;
this leads to herniation of abdominal contents into the thorax in utero.
Congenital hypertrophic pyloric stenosis
is encountered in male infants four times more
often than females. Persistent, projectile vomiting usually appears in the second or third
week of life. There is visible peristalsis and a firm, ovoid palpable mass in the region of
the pylorus resulting from hypertrophy and hyperplasia of the muscularis propria of the
pylorus. (Fig. 5-41)
Acquired pyloric stenosis in adults may complicate
1. Antral gastritis or peptic ulcers close to the pylorus.
2. Malignancy e.g. carcinomas of the pyloric region or adjacent panceas, or gastric lymphomas
3. Hypertrophic pyloric stenosis (rare) due to prolonged pyloric spasm
Gastritis
This is by definition, "inflammation of the gastric mucosa". It is a microscopic diagnosis.
The inflammation may be acute, with neutrophilic infiltration, or chronic, with
lymphocytes and/or plasma cells.
Acute gastritis
Is usually transient in nature. The inflammation may be accompanied by hemorrhage into
the mucosa (acute hemorrhagic gastritis) and, sometimes by sloughing (erosions) of the
superficial mucosa (acute erosive gastritis). (Fig. 5-42) The latter is a severe form of the
disease & an important cause of acute gastrointestinal bleeding. Although a large number
of cases have no obvious cause (idiopathic), acute gastritis is frequently associated with
1) Heavy use of nonsteroidal anti-inflammatory drugs (NSAIDs) particularly aspirin, cancer
chemotherapeutic drugs, or radiation
2) Excessive consumption of alcohol, heavy smoking, and ingestion of strong acids or alkali
as in suicidal attempts
3) Uremia
4) Severe stress (e.g., trauma, burns, surgery)
5) Mechanical trauma (e.g., nasogastric intubation)
6) Distal gastrectomy (reflux of duodenal contents).
Chronic Gastritis
Is defined as "chronic inflammation of the gastric mucosa that eventuates in mucosal
atrophy and intestinal metaplasia". The epithelial changes may progress to dysplasia,
which constitute a soil for the development of carcinoma.
Pathogenesis
The major etiologic associations of chronic gastritis are:
1. Chronic infection by H. pylori 2. autoimmune damage
3. Excessive alcohol consumption & heavy cigarette smoking
4. Post-antrectomy (due to reflux of bile-containing duodenal secretions)
5. Outlet obstruction, uremia, and other rare causes
Chapter 2 - Oral Cavity & Gastrintestinal Tract
29
o Helicobacter pylori Infection and Chronic Gastritis
Infection by H. pylori is the most important etiologic cause of chronic gastritis. Effective
treatment with antibiotics has revolutionized the management of chronic gastritis and
peptic ulcer disease. Those with H. pylori-associated chronic gastritis are at increased
risk for the development of
1. Peptic ulcer disease 2. Gastric carcinoma
3. Gastric lymphoma
H. pylori are curvilinear, gram-negative rods. They have adapted to survive within gastric
mucus, which is lethal to most bacteria. The specialized features that allow these
bacteria to flourish include:
1) Motility (via flagella), allowing them to swim through the viscous mucus
2) Urease production, which releases ammonia and CO
2
from endogenous urea, thereby
buffering the harmful gastric acid in the immediate vicinity of the bacteria
3) Expression of adhesion molecules, which enhances binding of the bacteria to adjacent
foveolar cells
The bacteria appear to cause gastritis by stimulating production of pro-inflammatory
cytokines as well as by directly damaging epithelial cells by the liberation of toxins &
degrading enzymes e.g. vacuolating toxin (VacA), urease, proteases and phospholipases.
After exposure to H. pylori, gastritis occurs in two patterns:
1) Antral-predominant gastritis with high acid production & elevated risk for duodenal ulcer
2) Pan gastritis with low acid secretion and higher risk for adenocarcinoma
IL-1β is a potent pro-inflammatory cytokine and a powerful gastric acid inhibitor. Patients
who have higher IL-1β production in response to the infection tend to develop pangastritis,
while patients who have lower IL-1β production exhibit antral-predominant gastritis.
A number of diagnostic tests have been developed for the detection of H. pylori. (Fig. 5-43)
1. Noninvasive tests including
a. Serologic test for antibodies b. Stool culture for bacterial detection
c. Urea breath test: based on the generation of ammonia by bacterial urease.
2. Invasive tests (through gastroscopy): detection of H. pylori in gastric biopsy tissue
samples including
a. visualization of the bacteria in histologic sections with special stains
b. bacterial culture of the biopsy c. bacterial DNA detection by the PCR
o Autoimmune gastritis
About 10% of chronic gastritis are autoimmune in nature. It results from the presence of
autoantibodies to components of parietal cells, including the acid-producing enzyme
H+/K+-ATPase, gastrin receptor, and intrinsic factor. Gland destruction and mucosal
atrophy lead to loss of acid production (hypo- or achlorhydria). (Fig. 5-44) In the most
severe cases, production of intrinsic factor is also impaired, leading to pernicious anemia.
Affected patients have a significant risk for developing gastric carcinoma and endocrine
tumors (carcinoid tumor).
Pathological features of chronic gastritis
Autoimmune gastritis is characterized by diffuse mucosal damage of the body-fundic
mucosa, with sparing of antral rgion (Corpus-predominant gastritis).
Environmental gastritis i.e. due to environmental etiologies (including H. pylori infection) tends
to affect antral mucosa (antral gastritis) or both antral and body-fundic mucosa (pangastritis).
o Gross (endoscopic) features
The mucosa of the affected regions is usually hyperemic & has coarser rugae than normal.
With long-standing disease, the mucosa may become thinned & flattened because of atrophy.
o Microscopic features (Fig. 5-45)
Irrespective of cause or location, the microscopic changes are similar:
The mucosa is infiltrated by lymphocytes & plasma cells.
Frequently the lymphocytes are disposed into aggregates i.e. follicles, some with germinal centers.
Neutrophils may or may not be present.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
30
Several additional histologic features are characteristic; these include
* Intestinal metaplasia: the mucosa may become partially replaced by metaplastic
columnar cells and goblet cells of intestinal morphology; these may display flat or villous
arrangement. If the columnar cells are absorptive (with ciliated border) the metaplasia is
termed complete, otherwise it is incomplete.
* Atrophy as evidecnced by marked loss of the mucosal glands. Parietal cells, in
particular, may be absent in the autoimmune form.
* Dysplasia: with long-standing chronic gastritis, the epithelium develops dysplastic
changes. Dysplastic alterations may become so severe as to constitute in situ carcinoma.
The development of dysplasia is thought to be a precursor lesion of gastric cancer. It
occurs in both autoimmune and H. pylori- associated chronic gastritis.
* In those individuals infected by H. pylori, the organism lies in the superficial mucus
layer on the surface and within the gastric pits. They do not invade the mucosa. These
bacteria are most easily demonstrated with silver or Giemsa (special) stains.
Peptic ulcer disease
An ulcer is defined as "a breach in the mucosa of the alimentary tract that extends into the
submucosa or deeper." Although they may occur anywhere in the alimentary tract, they
are most common in the duodenum and stomach. Ulcers have to be distinguished from
erosions. The latter is limited to the mucosa and does not extend into the submucosa.
Peptic Ulcers are chronic, most often solitary lesions and usually small. They occur in
any portion of the GIT exposed to the aggressive action of acid-peptic juices. They are
located, in descending order of frequency in:
1. Duodenum (first portion) 2. Stomach, (usually antral, along the lesser curve)
3. Gastro-esophageal junction (complicating GERD or Barrett esophagus)
4. Margins of a gastro-jejunostomy
5. Multiple in the duodenum, stomach, and/or jejunum (in Zollinger-Ellison syndrome)
6. Within or adjacent to a Meckel diverticulum (containing ectopic gastric mucosa)
The male-to-female ratio for duodenal ulcers is 3:1, and for gastric ulcers 2:1. Women are
most often affected at or after menopause.
Pathogenesis of peptic ulcers
Peptic ulcers are produced by an imbalance between gastro-duodenal mucosal defenses
and the damaging forces, particularly of gastric acid and pepsin.
Hyperacidity is not necessary; only a minority of patients with duodenal ulcers has
hyperacidity, and it is even less common in those with gastric ulcers.
H. pylori infection is a major factor in the pathogenesis of peptic ulcer. It is present in
virtually all patients with duodenal ulcers and in about 70% of those with gastric ulcers;
that is why peptic ulcer disease is now considered infectious in nature. Antibiotic
treatment of the infection promotes healing of ulcers and prevents their recurrence. The
possible mechanisms by which this tiny organism impairs mucosal defenses include:
1) H. pylori induce intense inflammatory and immune responses. As a result there is
increased production of pro-inflammatory cytokines, most notably, IL-8, by the mucosal
epithelial cells. This recruits and activates neutrophils with their damaging properties.
2) Several bacterial products cause epithelial cell injury; this is mostly caused by a
vacuolating toxin called VacA. H. pylori also secrete urease, proteases and
phospholipases, which also cause direct epithelial damage.
3) H. pylori enhance gastric acid secretion and impair duodenal bicarbonate production, thus
reducing luminal pH in the duodenum with its damaging effects on the duodenal mucosa.
4) Thrombotic occlusion of surface capillaries is provoked by a bacterial platelet-activating
factor. Thus, an additional ischemic element may contribute to the mucosal damage.
Most persons (80-90%) infected with H. pylori do not develop peptic ulcers. Perhaps there are
unknown interactions between H. pylori & the mucosa that occur only in some individuals.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
31
Other factors may act alone or in concert with H. pylori to encourage peptic ulceration:
1) Gastric hyperacidity: this when present, may be strongly ulcerogenic. The classic example
is Zollinger-Ellison syndrome, in which there are multiple peptic ulcerations in the
stomach, duodenum, and even jejunum. This is due to excess gastrin secretion by a
gastrinoma and, hence, excess gastric acid production.
2) Chronic use of NSAIDs: this suppresses mucosal prostaglandin synthesis; aspirin also is a
direct irritant.
3) Cigarette smoking: this impairs mucosal blood flow and healing of the ulcer.
4) Corticosteroids: these in high doses and with repeated use encourage ulcer formation.
5) Rapid gastric emptying: this is present inn some patients with duodenal ulcers; this
phenomeneon exposes the duodenal mucosa to an excessive acid load & hence ulcerations
6) Patients with the following diseases are more prone to develop duodenal ulcer exposes
a. alcoholic cirrhosis b. chronic obstructive pulmonary disease
c. chronic renal failure d. hyperparathyroidism.
Chronic renal failure and hyperparathyroidism are associated with hypercalcemia. The
latter stimulates gastrin production and therefore acid secretion.
7) Personality and psychological stress seems to be important contributing factors.
Gross features (Fig. 5-46)
The vast majority of peptic ulcers are located in the first portion of the duodenum or in the
stomach, in a ratio of about 4:1. Gastric and duodenal ulcers may coexist in up to 20% of
the cases. Gastric ulcers are predominantly located along the lesser curvature.
Although over 50% of peptic ulcers have a diameter less than 2 cm but about 10% are
greater than 4 cm. Ulcerated carcinomas (which tend to be large) may be less than 4 cm in
diameter and may be located anywhere in the stomach. Thus, size and location do not
differentiate a benign from a malignant ulcer.
The classic peptic ulcer is a round to oval with sharply demarcated crater. The margins are
usually level with the surrounding mucosa or only slightly elevated. Heaping-up of these
margins is rare in the benign ulcer but is characteristic of the malignant ones.
Peptic ulcers penetrate the wall to a variable extent. When the entire wall is penetrated,
the base of the ulcer may be formed by adherent pancreas, omental fat, or liver.
The base of a peptic ulcer is smooth and clean, owing to peptic digestion of any exudate
that may form. Sometimes, thrombosed or patent blood vessels (the source of life
threatening hemorrhage) are evident at the base of the ulcer.
Ulcer-related scarring may involve the entire thickness of the gastric wall; puckering of
the surrounding mucosa creates mucosal folds that radiate from the crater in spoke-like
fashion. This is different from malignant ulcers where there is flattening of the mucosal
folds (because of malignant infiltration) in the immediately surrounding of the ulcerative.
Microscopic features (Fig. 5-46 B)
In active ulcers four zones are recognized
1) The base and walls have a superficial thin layer of necrotic fibrinoid necrosis.
2) Beneath this layer is a zone of predominantly neutrophilic inflammatory
infiltrate.
3) Deeper still, there is granulation tissue infiltrated with inflammatory cells. This rests on
4) Fibrous or collagenous scar.
H. pylori-associated chronic gastritis is seen in up to 100% of patients with duodenal ulcers
and in 70% with gastric ulcers. With present-day therapies aimed at inhibition of acid
secretion (H
2
receptor antagonists and parietal cell H
+
/K
+
-ATPase pump inhibitors), and
eradication of H. pylori infection (with antibiotics), most ulcers heal within a few weeks.
The complications of peptic ulcer disease are
1) Bleeding is the most frequent complication (20%). It may be life-threatening; fatal in 25%
of the affected patients. It may be the first warning of an ulcer.
2) Perforation is much less frequent (5% of patients) but much more serious being fatal in
60% of patients.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
32
3) Obstruction (from edema or scarring) occurs in 2%, most often due to pyloric channel ulcers
but may occur with duodenal ulcers. Total obstruction with intractable vomiting is rare.
4) Malignant transformation does not occur with duodenal ulcers and is extremely rare with
gastric ulcers. When it occurs, it is always possible that a seemingly benign gastric ulcer
was, from the outset an ulcerative gastric carcinoma.
Acute Gastric Ulceration
Focal, acutely developing gastric mucosal defects are a well-known complication of
1) Therapy with NSAIDs
2) Severe stress (stress ulcers) as in shock states, extensive burns & severe trauma; they
usually occur in proximal duodenum (Curling ulcers)
3) Sepsis
4) Rraised intracranial pressure or intracranial surgery; these are seen as gastric, duodenal,
and esophageal ulcers & are designated as Cushing ulcers, which carry a high incidence
of perforation.
Generally, acute ulcers are multiple lesions predominantly gastric but sometimes also
duodenal. They range in depth from mere shedding of the superficial epithelium
(erosions) to deeper lesions that involve the entire mucosal thickness and deeper
(ulceration). Acute ulcers are not precursors of chronic peptic ulcers.
Gross features (Fig. 5-47)
Acute ulcers are usually small (less than 1 cm) and circular.
The ulcer base is frequently stained a dark brown by the acid digestion of blood.
They differ from chronic peptic ulcers by the following
1. They are found anywhere in the stomach, and are often multiple
2. The margins and base of the ulcers are not indurated
3. The related mucosal folds (rugae) are normal (cf. chronic peptic ulcer, which show
convergence on the ulcer)
Microscopically
There is focal loss of the mucosa & at least part of the submucosa
Unlike chronic peptic ulcers, there is no chronic gastritis or scarring.
Healing with complete re-epithelialization occurs after the causative factor is removed.
Bleeding from superficial gastric erosions or ulcers sufficient to require transfusion develops
in up to 5% of these patients. If the underlying cause is corrected recovery is complete.
Tumors of the stomach
These can be classified as benign and malignant lesions.
Benign tumors
Gastric polyps
In the alimentary tract, the term polyp is applied to any nodule or mass
that projects above the level of the surrounding mucosa. They are uncommon and
classified as non-neoplastic or neoplastic.
Hyperplastic polyps
(The most frequent; 90%) are small, sessile and multiple in about 25% of cases. There is
hyperplasia of the surface epithelium and cystically dilated glandular tissue. (Fig. 5-48)
Adenomatous polyp (adenoma)
(10% of polypoid lesions) (Fig. 5-49):
They contain proliferative dysplastic epithelium and hence have malignant potential. They
are usually single, and may grow up to 4 cm in size before detection. Up to 40% of gastric
adenomas contain a focus of carcinoma; there may also be an adjacent carcinoma that is
why histologic examination of all gastric polyps is obligatory.
Other specific types of gastric polyps are relatively uncommon and include fundic gland
polyps, hamartomatous Peutz-Jeghers polyps, juvenile polyps, and inflammatory fibroid polyp
Chapter 2 - Oral Cavity & Gastrintestinal Tract
33
Cancers of the stomach
Carcinoma is the most important and the most common (90%) of malignant tumors of the
stomach. Next in order of frequency are lymphomas (5%); the rest of the tumors are even
rarer e.g. carcinoids, and gastrointestinal stromal tumors (GISTs), leiomyosarcoma, and
schwannoma.
Gastric Carcinoma
Is a quite common tumor in the world. There are, however, marked geographical variations
in its incidence; it is particularly high in countries such as Japan. It is more common in
lower socioeconomic groups. There has been a steady decline in both the incidence and the
mortality of gastric cancer. There are mainly 2 subtypes of carcinoma: intestinal & diffuse.
These sub-types appear to have different pathogenetic mechanisms of evolution.
o Pathogenesis
The major factors thought to affect the genesis of gastric cancer apply more to the
intestinal type, as the risk factors for diffuse gastric cancer are not well defined.
1) Helicobacter pylori Infection: this generally increases the risk five- fold. The bacterial
infection causes chronic gastritis, followed by atrophy, intestinal metaplasia, dysplasia,
and carcinoma. Long-standing mucosal inflammation is associated with damage of
epithelial cells, which leads to compensatory epithelial cell proliferation, and hence
increased risk of genomic mutation. Since most individuals infected with H. pylori do not
develop cancer, other factors must be involved in carcinogenesis.
2) Adenomatous polyps: 40% of adenomas harbor carcinmatous foci; also adjacent
carcinoma is found in relation to adenomatous polyps in 30% of the cases.
3) Environmental factors: when families migrate from high-risk to low-risk areas (or the
reverse), successive generations acquire the level of risk that prevails in the new
environments. The diet is suspected to be a primary factor. Consumption of preserved and
salted foods; water contamination with nitrates; and lack of fresh fruit and vegetables are
common in high-risk areas. The intake of green, leafy vegetables and citrus fruits, which
contain antioxidants such as vitamin C, vitamin E and beta-carotene, seems to play a
protective role.
4) Autoimmune gastritis, like H. pylori infection, increases the risk of gastric cancer.
o Gross features
The most common location of gastric carcinomas is the pyloric antrum (50%). A favored
location is the lesser curvature. Although less common, an ulcerative lesion on the greater
curvature is more likely to be malignant.
Depth of invasion is the most important determinant of prognosis. Early gastric carcinoma
is defined as "a lesion confined to the mucosa and submucosa." Advanced gastric
carcinoma is a neoplasm extending into the muscular wall.
The three macroscopic growth patterns of gastric carcinoma, which may be evident at
both the early and advanced stages, are: 1. Fungating (exophytic) 2. Flat or depressed 3.
(Fig. 5-50) Ulcerative (excavated). Fungating tumors are readily identified by radiography
and endoscopy in contrast to flat (depressed) malignancy. Ulcerative cancers may closely
mimic chronic peptic ulcers. In advanced cases, there are heaped-up, beaded margins and
necrotic bases. The neoplastic tissue extends into the surrounding mucosa and wall; this
leads to flattening of the mucosa surrounding the ulcer. (Fig. 5-51)
Uncommonly, a broad region of the gastric wall or the entire stomach is extensively
infiltrated by malignancy, creating a rigid, thickened "leather bottle," termed linitis
plastica. (Fig. 5-52)
o Microscopic features
There are two main microscopic type of gastric carcinoma; intestinal and diffuse.
The intestinal variant is composed of neoplastic glands with mucin in their lumina. The
diffuse variant is composed of mucus-containing cells, which do not form glands, but
infiltrate the mucosa and wall as scattered individual and small clusters of cells. In this
Chapter 2 - Oral Cavity & Gastrintestinal Tract
34
variant, mucin formation expands the malignant cells and pushes the nucleus to the
periphery, creating"signet ring" morphology. (Fig. 5-53)
Sometimes, there is excessive mucin production that generates large mucin lakes
(mucinous carcinoma).
Infiltrative tumors often evoke a strong desmoplastic reaction (fibrosis), in which the
scattered cells are embedded; the fibrosis creates local rigidity of the wall.
Whatever the microscopic type, all gastric carcinomas eventually penetrate the wall to
involve the serosa and spread to regional and more distant lymph nodes.
o For obscure reasons, gastric carcinomas frequently metastasize to the supraclavicular
(Virchow) node as the first clinical manifestation of an occult neoplasm. (Fig. 5-54) The
tumor can also metastasize to the periumbilical region to form a subcutaneous nodule.
This nodule is called a Sister Mary Joseph nodule, after the nun who noted this lesion as a
marker of metastatic carcinoma. (Fig. 5-55) Local extension of gastric carcinoma into the
duodenum, pancreas, and retroperitoneum is also characteristic. At the time of death,
widespread peritoneal seeding and metastases to the liver and lungs are common. A
notable site of visceral metastasis is to one or both ovaries. Although uncommon,
metastatic adenocarcinoma to the ovaries (from stomach, breast, pancreas, and even
gallbladder) is distinctive & designated Krukenberg tumor. (Fig. 5-56)
o Gastric carcinoma is an insidious disease that is generally asymptomatic until late in its course.
The symptoms include weight loss, abdominal pain, anorexia, vomiting, dysphagia,
anemia, and hemorrhage. In Japan, where mass endoscopy screening programs are
employed (because of the high incidence of the disease), early gastric cancer constitutes
about one third of all newly diagnosed gastric cancers. In Europe and the United States,
this figure is only 10% to 15%.
o Prognosis
This depends primarily on
1. The depth of invasion and 2. The extent of nodal and distant metastasis
The histologic type (intestinal or diffuse) has minimal independent prognostic
significance. The five-year survival rate of surgically treated early gastric cancer is 90%;
this drops to below 15% for advanced gastric cancer.
Gastric Lymphomas
Represent 5% of all gastric malignancies. However, the stomach is the most common site
for extra-nodal lymphoma (20%). Nearly all primary gastric lymphomas are B-cell type
and of mucosa-associated lymphoid tissue (MALT lymphomas). The majority of gastric
lymphomas (>80%) are associated with chronic gastritis and H. pylori infection. The role
of H. pylori infection as an important etiologic factor for gastric lymphoma is supported
by the elimination of about 50% of early gastric lymphomas with antibiotic treatment for
H. pylori. Generally, the prognosis of gastric lymphoma is better than carcinoma.
Gastrointestinal Stromal Tumors (GISTs)
These are thought to originate from the interstitial cells of Cajal (normally control
gastrointestinal peristalsis). 95% of GISTs stain with antibodies against c-KIT (CD117).
The tumor can protrude into the lumen or extrude on the serosal side of the gastric wall.
Microscopically, the tumor can exhibit spindle cells, plump "epithelioid" cells, or a
mixture of both. Most of the tumors are quite cellular but mitotic activity is variable.
Gastric Neuroendocrine Cell (Carcinoid) Tumors
Most gastric carcinoid tumors originate from the enterochromaffin-like cells (ECL) cells
in the oxyntic mucosa. The tumor can arise in the setting of chronic atrophic gastritis. The
underlying pathogenesis is probably related to the hypergastrinemia, resulting in ECL-cell
hyperplasia, a presumed pre-neoplastic condition. Gastric carcinoid tumors exhibit similar
histologic features to other carcinoid tumors. The clinical course is quite variable.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
35
Small & large intestine
Several pathological conditions, such as infections, inflammatory diseases, motility
disorders, and tumors, affect both the small and large intestines simultaneously. These
two organs will therefore be considered together.
Congenital anomalies
Anomalies of the intestine are rarely encountered; these include
Duplication
of the small intestine or colon;
Malrotation
of the entire bowel;
Omphalocele
(birth of an infant with herniation of abdominal contents into a ventral
membranous sac related to umbilicus);
Heterotopia
of pancreatic tissue or gastric mucosa;
Atresia and stenosis
;
Imperforate anus
(due to failure of the cloacal diaphragm to rupture).
Meckel diverticulum
(Fig. 5-57)
Results from failure of involution of the vitelline duct, which embryologically connects
the lumen of developing gut to the yolk sac. The small pouch lies on the antimesenteric
side of the bowel, usually 30 cm proximal to the ileo-cecal valve. It consists of mucosa,
submucosa, and muscularis propria. The mucosal lining may be that of normal small
intestine, but heterotopic gastric mucosa or pancreatic tissue are frequently found. Meckel
diverticula are present in 2% of the normal population, but most remain asymptomatic.
When peptic ulceration occurs in the small intestinal mucosa adjacent to the heterotopic
gastric mucosa, intestinal bleeding or symptoms simulating those of an acute appendicitis
may result. Other complications include intussusception, incarceration, or perforation.
Congenital Aganglionic Megacolon (Hirschsprung Disease)
(Fig. 5-58)
This congenital disorder is characterized by the absence of ganglia of the submucosal and
myenteric neural plexuses, within a portion of the intestinal tract. The outcome is
contraction and functional obstruction of the aganglionic segment with secondary
proximal dilation. The rectum is always affected and most cases involve the rectum and
sigmoid colon only (short-segment disease). In some cases longer segments, and rarely
the entire colon may be aganglionic (long-segment disease). Proximal to the aganglionic
segment, the ganglionic colon undergoes progressive dilation and hypertrophy, sometimes
massively (megacolon). When distention overruns hypertrophy, the colonic wall becomes
markedly thinned and may rupture. Diagnosis of Hirschsprung is made histologically by
failure to detect ganglion cells in intestinal biopsy samples of the contracted (agnaglionic)
segment. The disease usually manifests itself in the immediate neonatal period by failure
to pass meconium, followed by obstructive constipation. Abdominal distention may
secondarily develop. The major threats to life are superimposed enterocolitis with fluid
and electrolyte disturbances and perforation with peritonitis.
Enterocolitis
These are divided into three etiological categories
I. Infectious (caused by microbiologic agents)
II. Malabsorption-associated
III. Idiopathic inflammatory bowel diseases
Diarrhea and Dysentery
Diarrhea is present when there is an increase in stool frequency, and/or stool fluidity.
This consists of daily stool production in excess of 250 gm, containing 70% to 95% water.
However, over 6 liters of fluid may be lost per day in severe cases of diarrhea (e.g.
cholera); this is the equivalent of the circulating blood volume.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
36
Dysentery is characterized by low-volume, painful diarrhea with blood.
Malabsorption-associated diarrhea is the result of interference with absorption of
nutrients, which produces bulky stools containig excess fat (steatorrhea).
Infectious enterocolitis
This is the cause of more than 12,000 deaths per day among children in developing
countries & constituting 50% of all deaths before the age of 5 years worldwide. Acute, self-
limited infectious diarrhea is most frequently caused by enteric viruses (such as rotavirus
and adenoviruses). Bacterial infections, such as that caused by enterotoxigenic Escherichia
coli, are also common. In up to 50% of cases, the specific agent cannot be isolated.
Viral enterocolitis
The lesions caused by enteric viruses in the intestinal tract are similar. The small intestinal
mucosa shows partial villous atrophy (shortening of the villi) with infiltration of the
lamina propria by lymphocytes. However, in infants, rotavirus and adenoviruses can
produce total villous atrophy (flat mucosa), thus resembling celiac disease (see later).
Bacterial enterocolitis
o Salmonellosis and Typhoid Fever
Salmonellae are gram-negative bacteria that cause either a self-limited food-borne and
water-borne gastroenteritis (S. enteritidis, S. typhimurium, and others) or typhoid fever
(S. typhi) a life-threatening systemic illness. In typhoid fever, Peyer patches in the
terminal ileum become sharply prominent forming flat elevations. Shedding of the
mucosa and the lymphoid tissue creates oval ulcers with their long axes parallel to that of
the ileum. Microscopic examination reveals macrophages containing bacteria & red blood
cells. Intermingled with the phagocytes are lymphocytes and plasma cells; the infiltrate is
characteristically devoid of neutrophils.
o Campylobacter Enterocolitis
This flagellated, comma-shaped bacterium may involve the entire intestine from the
jejunum to the anus. The small intestine exhibits partial villous atrophy. In colonic
infection, the colonic mucosa appears friable and superficially ulcerated. Microscopically,
the formation of colonic crypt abscesses and mucosal ulceration may be confused with
those of ulcerative colitis.
o Cholera
Vibrio cholerae affect the proximal small intestine. The mucosa remains essentially
intact as the bacteria never invade the epithelium but remain within the lumen and secrete
an enterotoxin that stimulates excessive secretions from the enterocytes. The re-absorptive
function of the colon is not affected but overwhelmed, thus liters of dilute "rice water"
diarrhea containing flecks of mucus occurs. This causes dehydration and electrolyte
disturbances. Because overall absorption in the gut remains intact, oral electrolytes-
containing fluids can replace the massive sodium, chloride, bicarbonate, and fluid losses
and reduce the mortality rate from 50% to less than 1%.
o Antibiotic-Associated Colitis (Pseudomembranous Colitis) (Fig. 5-59)
This is an acute colitis characterized by formation of an adherent layer of pseudomembrane
overlying sites of mucosal injury. It is caused by toxins of Clostridium difficile, which is a
normal gut commensal. The disease mostly follows a course of broad-spectrum antibiotic
therapy. Clostridium difficile flourish following alteration of the normal intestinal flora.
Diagnosis is confirmed by the detection of the C. difficile cytotoxin in stool. Grossly, there
are plaque-like adhesions of fibrinopurulent-necrotic debris and mucus to damaged colonic
mucosa. Microscopically, the lesion is characteristic in that the superficially damaged
crypts are distended by a mucopurulent exudate, which erupts out of the crypt to form a
mushrooming cloud (akin to volcano eruption).
Chapter 2 - Oral Cavity & Gastrintestinal Tract
37
o Tuberculous enteritis
Intestinal tuberculosis contracted by the drinking of contaminated milk was common as a
primary focus of the disease. In developed countries today, intestinal tuberculosis is more
often a complication of advanced pulmonary tuberculosis i.e. secondary to the swallowing
of coughed-up infective sputum. Typically, the organisms are trapped in mucosal
lymphoid aggregations of the small and large bowel, which then undergo inflammatory
enlargement with ulceration of the overlying mucosa, particularly in the ileum (Fig. 5-60).
Microscopy shows typical caseating granulomas that coalesce to form larger ones.
General pathological features of bacterial enteric diseases
These are quite variable.
Dramatic, even lethal, diarrhea may occur without a significant pathologic lesion, as in cholera.
Characteristic histology may enable diagnosis with reasonable certainty, as with C.
difficile-induced pseudomembranous colitis, and caseating granulomas of TB.
Parasitic enterocolitis
Parasitic diseases collectively affect over one-half of the world's population on a chronic
or recurrent basis. The intestine can harbor as many as 20 species of parasites, including
roundworms Ascaris and Strongyloides, hookworms, pinworms, flatworms, tapeworms,
flukes, and protozoa.
o Ascaris lumbricoides
This is the most common nematode, infecting over a billion individuals worldwide. Adult
worm masses can physically obstruct the intestine or the biliary tree. Diagnosis is usually
made by detection of the eggs in the feces.
o Strongyloides
The eggs of Strongyloides can hatch within the intestine & larvae can penetrate the mucosa,
causing autoinfection. Hence, Strongyloides infection can persist in one individual for life.
Immunosuppressed individuals can have overwhelming autoinfection. Strongyloides incites
a strong tissue eosinophilic reaction associated with blood eosinophilia.
o Hookworm (Necator duodenale and Ancylostoma duodenale) infection
This affects an estimated 1 billion people worldwide and causes significant morbidity.
The worms attach to the mucosa of small intestine, suck blood, and reproduce. Long-term
infection causes iron deficiency anemia. Diagnosis can be made by detection of the eggs
in fecal smear.
o Enterobius vermicularis (pinworms)
These do not invade host tissue and live their entire life within the intestinal lumen. Adult
worms living in the intestine migrate to the anal orifice at night, where the female
deposits eggs on the perirectal mucosa. As the eggs are quite irritative, rectal and perineal
pruritus ensues. Diagnosis is easily made by applying cellophane tape to the perianal skin
and examining the tape for eggs under the microscope.
o
Amebiasis
Is caused by the protozoan Entamoeba histolytica. The parasite infects approximately 500
million persons in developing countries resulting in approximately 40 million cases of
dysentery and liver abscesses. The presence in stool of trophozoites containing ingested
RBCs is diagnostic. The patient may present with abdominal pain & bloody diarrhea.
Pathologic features (Fig. 5-61)
Amebiasis most frequently involves the cecum and ascending colon. In severe cases,
however, the entire colon is involved (pancolitis).
Amebae invade through the crypt epithelium and burrow into the mucosa and submucosa,
eliciting a neutrophilic reaction.
They are stopped by the muscularis propria thus forced to spread out laterally to create a
flask-shaped ulcer with a narrow neck and broad base.
The mucosa between ulcers is often normal.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
38
o Giardiasis
Giardia lamblia is the most common pathogenic parasitic infection in humans. Infection
may cause acute or chronic diarrhea, steatorrhea, or constipation. Trophozoites multiply
in the intestinal lumen. The flagellated trophozoite has two nuclei & resides in the
duodenum, adhering to, but does not invade the intestinal epithelial cells. Tight contact
between the parasite and the epithelial cell is made by a sucker-like disc. It also contains
surface protein that resembles diarrhea-causing toxins secreted by certain snakes. The
physical presence of rapidly proliferating trophozoites as well as their toxic proteins that
damages the microvillus brush border are responsible for the associated malabsorption.
Pathological features (Fig. 5-62)
In stool smears, G. Iamblia trophozoites are pear shaped and binucleate.
Duodenal biopsy specimens are often packed with sickle or pear-shaped trophozoites,
which are tightly bound to the surface of the small intestinal villi.
As Giardia does not invade the mucosa, small intestinal morphology is often normal.
Diagnosis
This is readily made by
1) Examination of stool for cysts & trophozoites
2) Small intestinal biopsy or examination of a small intestinal aspirate that permit
identification of the trophzoite
Necrotizing enterocolitis (nec)
This acute, necrotizing inflammation of the small & large intestines may progress to
transmural necrosis of intestinal segments. It is the most common acquired gastrointestinal
emergency of neonates, particularly those who are premature or of low birth weight.
Collagenous and lymphocytic colitis
These distinctive disorders of the colon are characterized by chronic watery diarrhea (no
blood). Collagenous colitis is characterized by band-like collagen deposits directly under
the surface epithelium, whereas lymphocytic colitis is characterized by prominent
intraepithelial infiltrate of lymphocytes. Collagenous colitis occurs primarily in middle-
aged and older women; lymphocytic colitis affects males and females equally.
Radiographic studies are unremarkable, and endoscopy characteristically reveals normal
mucosa. The pathogenesis of these conditions remains unclear. While collagenous colitis
and lymphocytic colitis are uncommon, they must be considered in every adult patient
who presents with a noninflammatory, watery diarrhea.
Solitary rectal ulcer syndrome
This is an inflammatory condition of the rectum resulting from motor dysfunction of the
anorectal musculature, in particular impaired relaxation of the anorectal sling. The latter may
create sharp angulation of the anterior rectal wall. Abrasion of the overlying rectal mucosa
creates an oval ulcer & surrounding mucosal inflammation. Associated partial prolapse of
the rectal mucosa is common. Patients experience rectal bleeding & mucus discharge.
The malabsorption syndromes
Malabsorption is characterized by defective absorption of fats, fat-soluble and other
vitamins, proteins, carbohydrates, electrolytes and minerals, and water. The most common
clinical presentation is chronic diarrhea, and the hallmark of malabsorption is steatorrhea
(excessive fecal fat content). Although many causes of malabsorption can be established
clinically, small intestinal mucosal biopsy may be required to satisfactorily identify or
exclude celiac disease.
Major Malabsorption Syndromes
Clinically, the malabsorption syndromes resemble each other more than they differ. The
consequences of malabsorption affect many organ systems. The passage of abnormally
Chapter 2 - Oral Cavity & Gastrintestinal Tract
39
bulky, frothy, greasy, yellow, or gray stools (steatorrhea) is a prominent feature of
malabsorption; this is accompanied by weight loss, abdominal distention & muscle wasting.
The malabsorptive disorders most commonly encountered are
1) Celiac disease 2) Pancreatic insufficiency 3) Crohn disease
Pancreatic insufficiency
Primarily from chronic pancreatitis or cystic fibrosis, is a major cause of defective
intraluminal digestion that leads to diarrhea and steatorrhea.
Celiac Disease
Celiac disease (gluten-sensitive enteropathy, GSE) is a chronic disease, in which there is a
characteristic mucosal lesion of the small intestine and impaired nutrient absorption,
which improves on withdrawal of wheat gluten from the diet.
o Pathogenesis
The fundamental disorder in celiac disease is sensitivity to gluten component called
gliadin, which is a protein present in wheat and closely related grains (e.g. oat).
There is a T-cell mediated chronic inflammatory reaction, which develops as a
consequence of a loss of tolerance to gluten.
Interplay between genetic predisposing factors, the host immune response, and
environmental factors, is central to disease pathogenesis.
The small intestinal mucosa, when exposed to gluten, accumulates intraepithelial CD8+ T
cells and large numbers of lamina propria CD4+ T cells, which are sensitized to gliadin.
Gliadin is deamidated by the enzyme transglutaminase; the resultant peptides are recognized
by CD4+ T cells. This leads to secretion of interferon γ, which damages enterocytes.
o Pathological features (5-63)
By endoscopy, the duodenal mucosa appears flat (normally shows mucosal folds).
Biopsies demonstrate enteritis with partial or total loss of villi (partial villous atrophy or
completely flat mucosa respectively)
The surface epithelium shows degeneration, loss of the microvillus brush border, and an
increased number of intraepithelial lymphocytes.
The crypts exhibit increased mitotic activity and are hyperplastic, so that, despite villous
atrophy, the overall mucosal thickness remains the same.
The lamina propria has an overall increase in plasma cells and lymphocytes.
Although the above changes are characteristic of celiac disease, they can be mimicked by
other diseases, most notably tropical sprue.
Mucosal histology usually reverts to normal or near-normal following gluten exclusion
from the diet.
Dermatitis herpetiformis (DH) is a characteristic itchy skin-blistering disease can occur in
some patients with celiac disease.
Detection of serum anti-gliadin or "anti-endomysial" antibodies strongly favors the diagnosis
of celiac disease.
o Definitive diagnosis of celiac disease rests on
1. clinical documentation of malabsorption
2. demonstration of the intestinal lesions by small bowel biopsy and
3. Definite improvement in both symptoms and mucosal histology on gluten withdrawal
from the diet.
4. If there is doubt about the diagnosis, gluten challenge (reintroduction of gluten to the diet)
followed by rebiopsy has been advocated.
5. Serologic tests, mentioned above, are used for screening or treatment follow-up.
Most patients with celiac disease who adhere to a gluten-free diet remain well indefinitely
and ultimately die of unrelated causes. However, there is a long-term risk of malignant
disease, which includes small intestinal non-Hodgkin lymphoma (moderate risk), small
intestinal adenocarcinoma, and esophageal squamous cell carcinoma (50- to 100-fold
higher risk than the general population).
Chapter 2 - Oral Cavity & Gastrintestinal Tract
40
o Tropical Sprue (Postinfectious Sprue)
This condition is a celiac-like disease that occurs almost exclusively in people living in or
visiting the tropics. Malabsorption usually becomes apparent within days or a few weeks.
The condition improves on treatment with broad-spectrum antibiotics. This supports an
infectious etiology. Intestinal lymphoma does not appear to be associated with this
disorder (cf. celiac disease).
o Whipple Disease
Whipple disease is a rare systemic disease that principally affects the intestine, central
nervous system, and joints. It is caused by the bacterium Tropheryma whippelii. The
bacteria proliferate preferentially within macrophages. The hallmark of Whipple disease
is a small-intestinal mucosa laden with distended macrophages (stuffed with the bacteria).
Whipple disease is principally encountered in adults, with a strong male predominance. It
usually presents as malabsorption with diarrhea and weight loss. Response to antibiotic
therapy is usually rapid.
o Disaccharidase (Lactase) Deficiency
The disaccharidases, of which the most important is lactase, are located in the apical cell
membrane of the absorptive epithelial cells. Congenital lactase deficiency is a very rare
condition, but acquired lactase deficiency is common. Incomplete breakdown of the
disaccharide lactose into its monosaccharides glucose and galactose leads to osmotic
diarrhea from the unabsorbed lactose. Bacterial fermentation of the unabsorbed sugars
leads to increased hydrogen production, which is readily measured in exhaled air by gas
chromatography. Malabsorption is quickly corrected when exposure to milk and milk
products is terminated. In the adult, lactase insufficiency develops as an acquired disorder,
sometimes in association with viral and bacterial enteric infections. Neither light nor
electron microscopy has disclosed abnormalities of the mucosal cells of the bowel.
o Abetalipoproteinemia
This condition is a rare autosomal recessive inborn error of metabolism and characterized
by a defect in the synthesis and export of lipoproteins from intestinal mucosal cells. The
failure to absorb certain essential fatty acids leads to lipid membrane defects, evident in
the characteristic acanthocytic RBCs (burr cells) in blood films. The disease becomes
manifest in infancy and is dominated by failure to thrive, diarrhea, and steatorrhea.
Idiopathic inflammatory bowel disease (IBD)
The two disorders known as inflammatory bowel disease (IBD) are Crohn's disease (CD)
and ulcerative colitis (UC). These diseases have distinctly different clinical and
pathological features. Both CD and UC are chronic, relapsing inflammatory disorders of
obscure origin. CD is an autoimmune disease that may affect any portion of the
gastrointestinal tract from mouth to anus, but most often involves the distal small intestine
and colon. UC is a chronic inflammatory disease limited to the rectum and colon. Both
exhibit extra-intestinal inflammatory manifestations.
Etiology and Pathogenesis
In the normal GIT, the mucosal immune system is always ready to respond against
ingested pathogens but is unresponsive to normal intestinal microflora. In IBD, this state
of homeostasis is disrupted, leading to two key pathogenic abnormalities
1. Strong immune responses against normal microflora
2. Defects in epithelial barrier that cause microflora to reach the lymphoid tissue of the
intestine
The exact cause (s) leading to the above is still not established, hence the designation
idiopathic. It is postulated that IBD result from exaggerated local immune responses to
microflora in the gut, in genetically susceptible individuals.
Thus, the pathogenesis of IBD involves
1. Failure of immune regulation
Chapter 2 - Oral Cavity & Gastrintestinal Tract
41
2. Genetic susceptibility
3. Environmental triggers specifically microbial flora.
CD appears to be the result of a chronic delayed-type hypersensitivity reaction induced by
IFN-γ- producing T
H
1 cells. This is supported by the presence of granulomas in this
disease.
Experiments on animals suggest that UC is caused by excessive activation of T
H
2 cells.
Diagnosis of IBD
Since the exact etiology of IBD is not known, the diagnosis of IBD and the distinction
between CD and UC depend on clinical history, radiographic examination, laboratory
findings (serum ANCA is positive in 75% of UC Vs only 10% of CD.), and pathologic
examination of tissues involved. Pathologic appearances, both macroscopic and
microscopic, play a central role in establishing a definitive diagnosis.
Crohn disease (CD)
o This disease may involve any level of the alimentary tract. CD occurs at any age, but the
peak age of incidence is between 10 and 30 years. Smoking has been found to be a strong
risk factor.
o Pathological features
When fully developed, Crohn disease is characterized pathologically by
1. Sharply segmental and typically transmural involvement of the bowel by an
inflammatory process with mucosal damage
2. The presence of
- Small noncaseating granulomas
- Deep fissures that may eventuate in the formation of fistulae
In CD, there is involvement of the small intestine alone in about 40% of cases, of small
intestine and colon in 30%, and of the colon alone in about 30%. Other portions of the
GIT may also be uncommonly involved.
o Gross features (Fig. 5-64 A)
Segments of the small bowel involved by the disease show granular and dull gray serosa
(normally transparent and glistening).
Often the mesenteric fat wraps around the bowel (creeping fat)
The involved bowel wall is thick and rubbery (because of edema, inflammation, and
fibrosis). As a result, the lumen is narrowed.
A classic feature of CD is the sharp demarcation of diseased bowel segments from
adjacent uninvolved, essentially normal bowel (skip lesions).
Early disease shows small mucosal ulcers that coalesce to form long, serpentine linear
ulcers (i.e. long and twisted or sinuous).
As the intervening mucosa (between the ulcers) tends to be accentuated by inflammation
and edema, it acquires a cobblestone appearance. (Cobble-stone, is a rounded stone, esp.
of the size used for paving).
Narrow fissures develop between the mucosal folds, often penetrating deeply through the
bowel wall. Further extension of these fissures leads to fistulae or sinus tracts formation,
between the diseased intestinal segment and adherent structures (bowel loops, vagina,
urinary bladder, skin of the abdomen) or the sinuses may end blindly within the
abdominal cavity.
Free perforation or localized abscesses may develop.
o Microscopic features (Fig. 5- 64 B)
The characteristic histologic features of CD are:
1) Acute mucosal inflammation: there is neutrophilic infiltration of the surface & crypt
epithelium that eventually collects within the lumen of the crypts forming crypt abscesses.
2) Chronic mucosal damage: This is the hallmark of chronicity of CD (and UC). It
manifests as architectural distortion (in the small intestine as villus blunting; in the colon,
Chapter 2 - Oral Cavity & Gastrintestinal Tract
42
the crypts exhibit irregularity, and branching). Crypt destruction leads to progressive
mucosal atrophy.
3) Ulcerations are the usual outcome of severe active disease; these may be superficial, or
may penetrate deeply (as fissures) into underlying tissue layers.
4) Transmural chronic inflammation affecting all layers: chronic inflammatory cells
(lymphocytes & plasma cells) fill the affected mucosa and, to a lesser extent, all underlying
intestinal layers. Lymphoid aggregates are usually scattered throughout the bowel wall.
5) Noncaseating granulomas: in about 50% of the cases, noncaseating small granulomas
may be present in all tissue layers. Because they are not always present; the absence of
granulomas does not rule out the diagnosis of CD.
6) Other mural changes: in diseased segments, the muscularis mucosae usually exhibits
duplication & thickening. There is also fibrosis of the submucosa, muscularis propria, and
serosa that eventually leads to stricture formation.
7) Dysplastic changes of the mucosal epithelial cells are particularly important in persons
with long-standing chronic disease are. These may be focal or widespread, tend to
increase with time, and are thought to be related to increased risk of carcinoma,
particularly of the colon.
o Clinical Features
The disease usually begins with intermittent attacks of diarrhea, fever, and abdominal
pain, spaced by asymptomatic periods lasting for weeks to many months. In those with
colonic involvement, occult or overt fecal blood loss may lead to anemia. During this
lengthy, chronic disease, complications may arise from
1. Fibrosing strictures, particularly of the terminal ileum (intestinal obstruction)
2. Fistulas formed to other loops of bowel, urinary bladder, vagina, or perianal skin, or
into a peritoneum. In the latter focal abscesses may occur.
3. Extensive involvement of the small bowel, including the terminal ileum, may cause
a. marked loss of albumin (protein-losing enteropathy) b. generalized malabsorption
c. specific malabsorption of vitamin B
12
(pernicious anemia), or malabsorption of bile
salts, leading to steatorrhea.
Extraintestinal manifestations of this disease include
1. Arthritis & finger clubbing 2. Red nodules of the skin (Erythema nodosum)
3. Primary sclerosing cholangitis, (but the association is not as strong as in UC).
4. Renal disorders secondary to trapping of the ureters in the inflammatory process
sometimes develop and leading to hydronephrosis and pyelonephritis.
5. Systemic amyloidosis (rare late consequence).
6. An increased incidence of cancer of the GIT in patients with long-standing progressive
CD; however, the risk of cancer in CD is considerably less than in patients with chronic UC.
Ulcerative colitis
o In contradistinction to CD, ulcerative colitis is a chronic ulcero-inflammatory disease
limited to the colon and affecting only the mucosa and submucosa; it extends in a
continuous fashion proximally from the rectum. Well-formed granulomas are absent.
However, like CD, UC is a systemic disorder associated in some patients with arthritis,
uveitis, hepatic involvement (primary sclerosing cholangitis), and skin lesions. The onset
of disease peaks between ages 20 and 25 years. Nonsmoking is associated with UC; ex-
smokers are at higher risk for developing UC than never-smokers.
o Pathological features
Ulcerative colitis involves the rectum and extends proximally in a retrograde fashion to
involve the entire colon ("pancolitis") in the more severe cases. It is a disease of
continuity, and "skip" lesions are not found (cf. CD).
o Gross features (Fig. 5-65 A)
A key feature of UC is that the mucosal damage is continuous from the rectum and
extending proximally.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
43
The mucosa may exhibit reddening and granularity with easy bleeding.
With fully developed severe, active inflammation, there may be extensive ulcerations of
the mucosa.
Isolated islands of regenerating mucosa bulge upward to create polypoid projections
(pseudopolyps).
With chronicity or healing of active disease, progressive mucosal atrophy occurs.
Thickening of the bowel wall does not occur in UC; the serosal surface is usually
completely normal (cf. CD).
Only in the most severe cases of ulcerative disease (UC, CD,& other severe inflammatory
diseases) does toxic damage to the muscularis propria and neural plexus lead to complete
shutdown of neuromuscular function. In this instance the colon progressively swells and
becomes gangrenous, a life-threatening condition called toxic megacolon.
o Microscopic features (Fig. 5-65 B)
The basic mucosal alterations in UC are similar to those of colonic CD, with
inflammation, chronic mucosal damage, and ulceration.
There is diffuse, predominantly chronic inflammatory infiltrate in the lamina propria.
Neutrophilic infiltration of the epithelial layer may produce crypt abscesses. The latter are
not specific for UC and may be observed in CD or any active inflammatory colitis.
Unlike CD, there are no granulomas.
Destruction of the mucosa leads to broad-based ulcerations that are superficial i.e.
extending at most into the submucosa.
Isolated islands of regenerating mucosa bulge upward to create pseudopolyps.
Features of chronic but healed (inactive) disease include submucosal fibrosis; mucosal
architectural distortion and atrophy.
Particularly significant is the spectrum of epithelial dysplasias, which are divided into
low-grade and high-grade depending on the severity. Invasive carcinoma is the ultimate
lesion arising from dysplasia.
To summarize UC differs pathologically from CD in the following
a. Well-formed granulomas are absent.
b. There are no skip lesions.
c. The mucosal ulcers rarely extend below the submucosa, and
d. There is surprisingly little fibrosis.
e. Mural thickening does not occur, and the serosal surface is usually completely normal.
f. There appears to be a higher risk of carcinoma development.
o Course & prognosis
Ulcerative colitis typically presents as a recurrent attacks of bloody mucoid diarrhea that
may persist for days, weeks, or months and then subside, only to recur after an
asymptomatic interval of months to years.
The outcome of UC depends on two factors:
1. The severity of active disease 2. The duration of the disease
The majority of the cases can be controlled medically; however, about 30% of patients
require colectomy due to uncontrollable active disease. On rare occasion, the disease runs
a fulminant course; unless medically or surgically controlled, this toxic form of the
disease can lead to death soon after onset.
The most serious long-term complication of UC is colonic carcinoma. There is a tendency
for dysplasia to arise in multiple sites. The associated carcinomas are often infiltrative
without obvious exophytic masses. Historically, the risk of cancer is highest in patients
with pancolitis of 10 or more years' duration. It is believed that with 10 years of disease
limited to the left colon the risk is minimal, and at 20 years the risk is on the order of 2%.
With pancolitis, the risk of carcinoma is 10% at 20 years and up to 25% by 30 years.
Overall, the annual incidence of colon cancer in persons with ulcerative colitis of more
than 10 years' duration is 1%.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
44
Vascular disorders
Ischemic Bowel Disease
Ischemic lesions may be restricted to the small or large intestine, or may affect both,
depending on the particular vessel(s) affected. Acute occlusion of one of the three major
supply arteries of the intestines—celiac, superior mesenteric, and inferior mesenteric
arteries—may lead to infarction of several meters of intestine. However, gradual occlusion
of one vessel may be without effect, due to the rich anastomotic interconnections. Lesions
within the end arteries, which penetrate the gut wall, produce small, focal ischemic
lesions. Pathologically the outcome of ischemic injury is divided into
1. Transmural infarction, involving all layers (full thickness infarction)
2. Mural infarction involving the mucosa and submucosa.
3. Mucosal infarction extends no deeper than the muscularis mucosae.
Almost always, transmural infarction is caused by occlusion of major mesenteric blood
vessels, whereas mucosal or mural infarctions often result from hypoperfusion.
Mesenteric venous thrombosis is a less frequent cause of vascular insufficiency.
The predisposing conditions for ischemia are:
1. Arterial thrombosis complicating usually severe atherosclerosis.
2. Arterial embolism complicating cardiac vegetations and aortic atheroembolism.
3. Venous thrombosis complicating hypercoagulable states, oral contraceptives,
intraperitoneal sepsis, etc.
4. Nonocclusive ischemia complicating cardiac failure, shock, dehydration, and
vasoconstrictive drugs (e.g., digitalis, vasopressin, propranolol)
5. Miscellaneous such as radiation injury, volvulus, and internal or external herniae.
Pathological features (Fig. 5-66 A)
Transmural Infarction
Small intestinal infarction may follow sudden and total occlusion of mesenteric arterial
blood flow.
It more often involves a considerable length of the bowel.
The splenic flexure of the colon is also at greatest risk of ischemic injury because it is the
watershed between the distribution of the superior and inferior mesenteric arteries.
(Watershed area: a narrow zone between two areas that are supplied by two vessels).
Mesenteric venous occlusion, with subsequent propagation of thrombus may lead to
extensive infarction.
The infarction appears hemorrhagic (dusky red) because of blood re-flow into the
damaged area. The lumen of the affected segment commonly contains bloody mucus or
frank blood.
Within 1 to 4 days, intestinal bacteria produce gangrene & sometimes perforation of the bowel.
Microscopically, (Fig. 5-66 B)
The picture is that of coagulative necrosis with inflammatory cell infiltration.
Chronic Ischemia: Chronic vascular insufficiency, e.g. due to gradual atherosclerotic
narrowing of the relevant vessel to a region of intestine, produces mucosal inflammation &
ulceration. Submucosal chronic inflammation & fibrosis may also occur & lead to strictures.
Angiodysplasia: Is characterized by tortuous dilations of submucosal and mucosal blood
vessels are seen most often in the cecum or right colon, usually only after the age of 50
years. They are responsible for 20% of significant lower intestinal bleeding.
Hemorrhoids
(Fig. 5-67)
Are essentially varices of the anal and perianal venous plexuses. They are extremely
common affecting 5% of the general population. They develop secondary to persistently
elevated venous pressure within the hemorrhoidal plexus. The most frequent predisposing
influences are constipation with straining at stool and the venous stasis of pregnancy.
Except for pregnant women, they are rarely encountered in persons under the age of 30.
Much more rarely, but much more importantly, hemorrhoids may reflect collateral
Chapter 2 - Oral Cavity & Gastrintestinal Tract
45
anastomotic channels that develop because of portal hypertension (as in liver cirrhosis).
The varicosities may develop in the inferior hemorrhoidal plexus and thus are located
below the anorectal line (external hemorrhoids) or from dilation of the superior
hemorrhoidal plexus (internal hemorrhoids). Commonly, both plexuses are affected
(combined hemorrhoids). Microscopically these lesions consist of thin-walled, dilated,
submucosal vessels. Superficial ulceration, fissure formation, and infarction of the
hemorrhoids secondary to their strangulation may develop.
Diverticular disease
A diverticulum is a blind pouch related to the alimentary tract. It is lined by mucosa that
communicates with the lumen of the gut. Congenital diverticula is typified by Meckel
diverticulum. Virtually all other diverticula are acquired and either lack or have an
attenuated muscularis propria. The most common site of multiple diverticula is the left
side of the colon, with the majority in the sigmoid colon; this is termed diverticular
disease of the colon. It manifests mostly after the age of 30 years. They are much less
frequent in underdeveloped tropical countries than in developed countries.
Intestinal obstruction (fig. 5-68)
The small intestine is most often involved due to its narrow lumen. Tumors and
infarction, although the most serious, account for only up to 20% of small-bowel
obstructions. The remaining 80% are due to
1. Hernias
2. Intestinal adhesions
3. Intussusception
4. Volvulus
The clinical manifestations include abdominal pain and distention, vomiting, constipation,
and in complete obstruction failure to pass flatus.
Hernias (Fig. 5-69)
A weakness or defect in the wall of the peritoneal cavity may permit protrusion of a pouch-
like sac of peritoneum called hernial sac. The usual sites of such weakness are at the
1. Inguinal canal 2. Femoral canal 3. Umbilicus 4. In surgical scars
Hernias are of concern chiefly because segments of viscera frequently protrude and
become trapped in hernial sac. This is particularly true with inguinal hernias, since they
tend to have narrow orifices and large sacs. The most frequent contents of a hernial sac
are small-bowel loops, but portions of omentum or large bowel may also become trapped.
Pressure at the neck of the pouch may impair venous drainage of the trapped bowel
segment. The resultant stasis and edema increase the bulk of the herniated loop, leading to
permanent trapping (incarceration). With time, interference with arterial supply and
venous drainage (strangulation) leads to infarction of the trapped segment.
Adhesions (Fig. 5-70)
Surgical procedures, infection, and endometriosis often cause localized or more general
peritonitis. As the peritonitis heals, adhesions may also develop between bowel segments
and abdominal wall at the operative site. These fibrous bridges can create closed loops
through which other viscera may slide and eventually become trapped (internal hernias).
These internal hernias are liable for the same complications as external ones ( obstruction
and strangulation)
Intussusception (Fig. 5-71)
This occurs when one segment of the intestine, constricted by a wave of peristalsis,
suddenly becomes telescoped into the immediately distal segment of bowel. Once trapped,
the invaginated segment is propelled by peristalsis farther into the distal segment, pulling
its mesentery along with it. When encountered in infants and children, there is usually no
underlying anatomic lesion or defect in the bowl, but some cases of intussusception are
associated with rotavirus infection, suggesting that localized intestinal inflammation may
serve as a traction point for the intussusception. However, intussusception in adults
Chapter 2 - Oral Cavity & Gastrintestinal Tract
46
signifies an intraluminal mass or tumor as the point of traction. In both settings, intestinal
obstruction ensues, and trapping of mesenteric vessels leads to infarction.
Volvulus (Fig. 5-72)
This signifies complete twisting of a loop of bowel about its mesenteric base of
attachment. It produces intestinal obstruction and infarction. This lesion occurs most often
in large redundant loops of sigmoid, followed in frequency by the cecum& small intestine
Tumors of the small and large intestine
The large intestine is responsible for more primary neoplasms than any other organ in the
body. The vast majority are adenocarcinomas. The small intestine, despite its great length
(3/4 of the GIT), is an uncommon site for benign or malignant neoplasms.
Tumors of the small intestine
The most common benign tumors in the small intestine are adenomas (Fig. 5-73) and
mesenchymal tumors. Of malignant tumors adenocarcinomas and carcinoids have
roughly equal incidence, followed in order by lymphomas and sarcomas.
Tumors of the Colon and Rectum
Non-neoplastic and benign neoplastic lesions of the colo-rectum are collectively known as
polyps, which are common in the older adult population. Epithelial polyps that arise as the
result of proliferation and dysplasia are termed adenomatous polyps (adenomas). They are
precursors of carcinoma.
Non-Neoplastic Polyps include
1) Hyperplastic polyp 2) hamartomatous polyp 3) inflammatory polyp 4) lymphoid polyp
o Hyperplastic Polyps
These are the most common polyps of the colon and rectum. They are small (usually <5
mm in diameter) and appear as smooth protrusions of the mucosa. They are often multiple
and consists of well-formed glands and crypts lined by non-neoplastic epithelial cells.
o Hamartomatous Polyps
1) Juvenile polyps (Fig. 5-74) are essentially hamartomatous proliferations, mainly of the
lamina propria, enclosing widely spaced, dilated cystic glands. They occur most
frequently in children younger than 5 years old but also are found in adults of any age; in
the latter group they may be called retention polyps. The lesions are usually large in
children (1-3 cm in diameter) but smaller in adults; they are rounded, smooth, or slightly
lobulated and sometimes have a stalk as long as 2 cm. In general, they occur singly and in
the rectum, and have no malignant potential. Juvenile polyps may be the source of rectal
bleeding and in some cases become twisted on their stalks to undergo painful infarction.
2) Peutz-Jeghers polyps (Fig. 5-75) are also hamartomatous polyps that involve the
mucosal epithelium, lamina propria, and muscularis mucosae. They may occur
sporadically or in the setting Peutz-Jeghers syndrome (PJS). PJS is a rare autosomal
dominant syndrome characterized by
a) Multiple hamartomatous polyps scattered throughout the entire GIT
b) Melanotic mucosal & cutaneous pigmentation especially around the lips & in the oral mucosa.
Patients with this syndrome are at risk for intussusception, which is a common cause of mortality.
The polyps are present most frequently in the small intestine.
Adenomas (Adenomatous polyps)
Adenomas are intraepithelial neoplasms that range from small, often pedunculated lesions
to large neoplasms that are usually sessile. The prevalence of colonic adenomas increases
progressively with age. Males and females are affected equally. Adenomatous polyps are
divided into three subtypes on the basis of the epithelial architecture (Fig. 5-76):
1. Tubular adenomas: compose of tubular glands
Chapter 2 - Oral Cavity & Gastrintestinal Tract
47
2. Villous adenomas: composed of villous projections
3. Tubulovillous adenoma: composed of a mixture of the above two.
All adenomas by definition arise as the result of dysplastic epithelial proliferation. The
dysplasia ranges from low-grade to high-grade. There is strong evidence that adenomas are
precursors for invasive colorectal adenocarcinomas. The risk of cancer is high (approaching
40%) in villous adenomas more than 4 cm in diameter. Adenomas may be single or multiple,
may be asymptomatic, and many are discovered during evaluation of anemia (due to occult
bleeding) through endoscopy. Villous adenomas are often are discovered because of overt
rectal bleeding. The most distal villous adenomas may secrete sufficient amounts of mucoid
material rich in protein & potassium to produce hypoproteinemia or hypokalemia. The only
adequate treatment for adenomas is complete resection.
Familial polyposis syndromes
These are uncommon autosomal dominant disorders. Their importance lies in their
tendency for malignant transformation.
1. Peutz-Jeghers syndrome
2. Juvenile polyposis syndrome
3. Familial adenomatous polyposis (FAP)
Another hereditary condition in this context but is not associated with polyp formations is
the hereditary nonpolyposis colorectal cancer syndrome (Lynch syndrome).
o Familial Adenomatous Polyposis (FAP) Syndrome (Fig. 5-77)
This is caused by mutations of the adenomatous polyposis coli (APC) gene on
chromosome 5.
In the classic FAP syndrome, affected patients typically develop 500 to 2500 colonic
adenomas that carpet the mucosal surface; the presence of a minimum of 100 polyps is
necessary for a diagnosis. The lifetime risk of cancer development is 100%. Some
patients already have cancer of the colon or rectum at the time of diagnosis. Cancer-
prevention measures include early detection of the condition and prophylactic colectomy.
Colorectal carcinoma
o A widely accepted proposal of carcinogensis is the adenoma-carcinoma sequence (Fig.
5-78), i.e. most carcinomas arise from preexisting adenomas. This has been supported by
the following observations:
1) Populations that have a high prevalence of adenomas have a high prevalence of colorectal cancer.
2) The distribution of adenomas parallel that of colorectal cancer.
3) The peak incidence of adenomas precedes that of carcinoma by some years.
4) When invasive carcinoma is identified at an early stage, a related adenoma is often present
5) The risk of cancer is directly related to the number of adenomas, that is why carcinoma
complicates all those with FAP syndrome.
6) Removal of all adenomas that are suspicious reduces significantgly the incidence of
cancerinoma. 98% of all cancers in the large intestine are adenocarcinomas. They usually
arise in polyps and produce symptoms relatively early and at a stage generally curable by
surgical resection. Yet, it is responsible for 10% of all cancer-related deaths. The peak
incidence for colorectal carcinoma is between ages 60 and 79.When colorectal carcinoma
is found in a young person, pre-existing ulcerative colitis or one of the polyposis
syndromes must be suspected. Environmental factors, particularly dietary practices, are
implicated in the striking geographic variations in incidence. Japanese families that have
migrated from their low-risk areas to the United States (high-risk areas) have acquired,
over the course of 20 years, the rate prevailing in the new environment; mainly because
the immigrants adopted the common dietary practices of the U.S. population. The dietary
factors receiving the most attention as predisposing to a higher incidence of cancer are
1. Excess dietary caloric intake relative to requirements 2. Low content of unabsorbable
vegetable fibers & high content of refined carbohydrates 3. Intake of red meat
Chapter 2 - Oral Cavity & Gastrintestinal Tract
48
Several epidemiological studies suggest that the use of aspirin and other nonsteroidal anti-
inflammatory drugs exerts a protective effect against colon cancer.
o Gross features (Fig. 5-79 A)
The rectosigmoid colon is the most frequent location (60%), followed by
cecum/ascending colon (20%).
Tumors in the proximal colon tend to grow as polypoid, exophytic masses; obstruction is
uncommon. In the distal colon, they tend to be annular, encircling lesions that produce
napkin-ring constrictions. The lumen is markedly narrowed leading to obstruction with
secondary proximal distention.
Both forms (polypoid and annular) directly penetrate the bowel wall over the course of
time (probably years) and may appear as subserosal and serosal white, firm masses.
o Microscopic features (Fig. 5-79 B)
The features of right- and left-sided colonic adenocarcinomas are similar.
Differentiation (grade) may range from well-differentiated tumors to undifferentiated,
frankly anaplastic masses.
Invasive tumor provokes a strong desmoplastic (fibrotic) stromal response (responsible
for the characteristic firm, hard consistency of most carcinomas).
Carcinomas arising in the anal canal are mostly of squamous cell type.
o Clinical features
remain asymptomatic for years; symptoms develop insidiously and frequently have been
present for months, sometimes years, before diagnosis. Patients with cecal and right
colonic cancers are most often presented with iron-deficiency anemia (due to insidious
blood loss). Left-sided lesions come to attention by producing occult bleeding, changes in
bowel habit or intestinal obstrcution. Iron-deficiency anemia in an older male means GI
cancer until proved otherwise. In females the situation is less clear, since menstrual
losses, multiple pregnancies, or abnormal uterine bleeding may underlie such an anemia.
o Spread & metastsis
All colorectal tumors spread by direct extension into adjacent structures and by metastasis
through the lymphatics and blood vessels. The favored sites of metastatic spread are the
regional lymph nodes, liver, lungs, and bones. In general, the disease has spread beyond
the range of curative surgery in 25% of patients. The single most important prognostic
factor of colorectal carcinoma is the extent of the tumor at the time of diagnosis (stage).
Currently, the staging system most widely used is the tumor-nodes-metastasis (TNM).
(Fig. 5-80) The principal aim is to discover these neoplasms when curative resection is
possible. Indeed, each death from colonic cancer must be viewed as a preventable tragedy.
Carcinoid tumors
o The term carcinoid means carcinoma-like lesion because it shows a much more indolent
clinical course than genuine carcinoma. Carcinoid tumor is derived from resident
endocrine cells, with the gastrointestinal tract and lung as the predominant sites of
occurrence. They comprise less than 2% of colorectal malignancies but 50% of small
intestinal malignant tumors. These tumors may be confined to the mucosa and submucosa
or may be deeply invasive with metastatic spread to regional lymph nodes and the liver.
Appendiceal and rectal carcinoids almost never metastasize.
o Gross features (Fig. 5-81) The appendix is the most common site of gut carcinoid
tumors. In the appendix, they appear as rounded swellings of the tip. A characteristic
feature is a solid, yellow-tan appearance on transection.
o Microscopic features
The neoplastic cells may form islands, trabeculae, glands, or sheets. The tumor cells show
very little if any variation in cell and nuclear size, having a scant, pink granular cytoplasm
and a round to oval nucleus. Mitoses are infrequent or absent.
Electron microscopy: the cells contain dense-core secretory granules in the cytoplasm.
Most carcinoids contain endocrine markers.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
49
o Gastrointestinal carcinoids only rarely produce local symptoms; many (especially rectal
and appendiceal) are asymptomatic and are found incidentally. However, the secretory
products of some carcinoids may produce a variety of syndromes such as Zollinger-
Ellison syndrome (excess production of gastrin), Cushing syndrome (excess production of
corticotrophin). Hyperinsulinism may also occur leading to hypoglycemia. Some
neoplasms are associated with the distinctive carcinoid syndrome, which occurs
especially with carcinoids associated with widespread metastases. Most manifestations
are thought to arise from excess elaboration of serotonin (5-hydroxytryptamine, 5-HT).
Elevated levels of 5-HT and its metabolite, 5-hydroxyindoleacetic acid (5-HIAA), are
present in the blood and urine of most patients with the classic syndrome. The syndrome
is characterized by
- Cyanosis of the face and anterior part of the chest
- Intermittent hypertension & palpitation
- Frequent watery stools
The tumor, sometimes, induces fibrosis of the right-sided cardiac valves that results in so-
called carcinoid heart disease.
Gastrointestinal lymphomas
Any segment of the gastrointestinal tract may be secondarily involved by systemic
dissemination of nodal-based non-Hodgkin lymphomas. However, up to 40% of
lymphomas arise in sites other than lymph nodes (extra-nodal lymphomas), and the gut is
the most common location.
Primary gastrointestinal lymphomas usually arise without an obvious predisposing factor
but they also occur more frequently in certain patient groups
1. Chronic gastritis caused by H. pylori 2. Chronic celiac disease
3. Natives of the Mediterranean region (Mediterranean lymphoma)
4. Congenital immunodeficiency states, infection with HIV or following organ
transplantation with immunosuppression
Most gut lymphomas are of B-cell type (over 95%) and are either low- or high-grade
tumors. Early discovery is the key to survival. The depth of local invasion, size of tumor
and its histologic grade as well as extension into adjacent viscera are important
determinants of prognosis.
Mesenchymal tumors
Mesenchymal tumors may occur anywhere in the alimentary tract and include lipomas,
leiomyosarcomas, gastrointestinal stromal tumors (GISTs) and Kaposi sarcomas.
Tumors of the anal canal
Pure squamous cell carcinomas of the anal canal are closely associated with chronic HPV
infection. The latter often causes precursor lesions such as condyloma acuminatum,
squamous epithelium dysplasia, and carcinoma in situ. Pure adenocarcinoma of the anal
canal is often the extension of rectal adenocarcinoma.
Chapter 2 - Oral Cavity & Gastrintestinal Tract
50
Appendix
Acute appendicitis
Is the most common acute abdominal surgical emergency. It is divided into
1) Acute appendicitis associated with obstruction (up to 80% of cases). The obstructing
agent is usually a fecalith and, less commonly, a gallstone, tumor, or ball of worms
(Entrobias vermicularis). Continued secretion of mucinous fluid in the obstructed portion
leads to a progressive increase in intraluminal pressure that eventuates in compression and
obstruction of the draining veins. The ischemic injury favors bacterial proliferation with
additional inflammatory edema& exudation, which further interfere with the blood supply
2) Acute appendicitis without obstruction, which is of unknown pathogenesis.
Gross features (Fig. 5-82 A)
The transmural inflammatory reaction converts the normal glistening serosa into a dull, red
membrane; this transformation signifies early acute appendicitis for the operating surgeon.
Later the prominent neutrophilic exudate leads to fibrino-purulent reaction over the serosa.
As the inflammatory process worsens, there is abscess formation within the wall, along
with ulcerations and foci of suppurative necrosis in the mucosa. This constitutes acute
suppurative appendicitis.
Further progression leads to large areas of hemorrhagic green ulceration of the mucosa &
green-black gangrenous necrosis through the wall, extending to the serosa, creating acute
gangrenous appendicitis, which is quickly followed by rupture and suppurative peritonitis.
Microscopy (Fig. 5-82 B)
The microscopic criterion for the diagnosis of acute appendicitis is neutrophilic
infiltration of the muscularis propria (transmural inflammation)
Usually, neutrophils and ulcerations are also present within the mucosa.
Tumors of the appendix
Carcinoid tumor
(see above)
Conventional adenomas or adenocarcinomas
of the appendix
These are rare and pathologically identical to those of the large intestine and may cause a
neoplastic enlargement of the appendix.
Mucocele and pseudomyxoma peritonei
Mucocele is the macroscopic description of a dilated appendix filled with mucin. The true
pathologic nature of mucocele runs the range from an innocuous obstructed appendix
containing inspissated mucin, to a mucin-secreting adenoma (mucinous cystadenoma) and
adenocarcinoma (mucinous cystadenocarcinoma). In the last instance, invasion through
the appendiceal wall with intraperitoneal seeding and spread of tumor may occur, this
may be associated with pseudomyxoma peritoneii. (Fig. 5-83) Mucoceles are generally
encountered as an incidental lesion. Mucinous cystadenomas and adenocarcinomas may
present with pain, attributable to distention of the viscus. Laparotomy for presumed acute
appendicitis is a typical diagnostic setting. For lesions confined to the resected specimen
(appendix or more radical excision), the outlook is excellent. Pseudomyxoma peritoneii
may be held in check for years by repeated debulking procedures but in most instances
eventually runs its inexorable fatal course.
