Mumps(Infectious parotitis)
MumpsAcute viral illness
Parotitis and orchitis described by Hippocrates in 5th century B.C.
Viral etiology described by Johnson and Goodpasture in 1934
Frequent cause of outbreaks among military personnel in prevaccine era
What is mumps?
It is a disease caused by the mumps virus.Who gets mumps?
Past infection with mumps makes a person immune to mumps; most people born before 1957 most likely have already had mumps. In addition, people who receive two doses of the mumps vaccine are much less likely to be infected. The greatest risk of infection occurs among older children, adolescents, and adults.
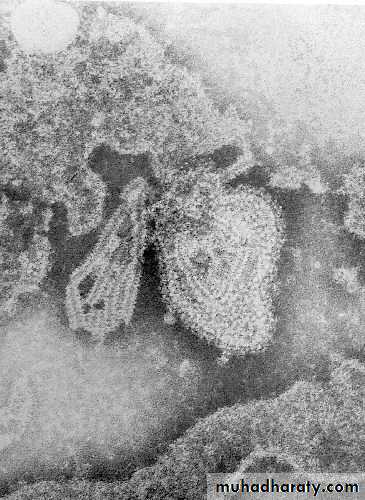
Mumps Virus
ParamyxovirusIt is a single-stranded RNA virus
One antigenic type
Rapidly inactivated by chemical agents (formalin, ether, chloroform), heat and ultraviolet light.
•
How is mumps spread?
Mumps is spread in droplets from the nose or throat of an infected person, usually when a person coughs or sneezes. Mumps can also spread by direct contact with saliva and discharges from the nose and throat of aninfected person.
Mumps Clinical Features
Incubation period 14 - 18 daysNonspecific prodrome of low-grade fever, headache, malaise, myalgias
Parotitis in 30% - 40%
Up to 20% of infections asymptomatic
May present as lower respiratory illness, particularly in preschool-aged children
About one in three persons infected with mumps virus do not have any signs or symptoms of illness. The most common signs and symptoms of mumps include fever, headache, and swelling and tenderness of one or more salivary glands. Swelling of the testicles occurs in 20-30% of infected males - this does not usually result in sterility.
Mumps can also cause central nervous system disorders such as encephalitis (inflammation of the brain) and meningitis (inflammation of the covering of the brain and spinal column). Other complications include miscarriage of a pregnancy, arthritis, pancreatic involvement, or deafness.
How soon after infection do signs and symptoms occur?
Signs and symptoms of mumps usually appear within 18 days after exposure, but may appear any time within 12 to 25 days after exposure.
When and for how long is a person able to spread mumps?
Mumps is contagious from three days before until five days after the onset of swelling.What is the treatment for mumps?
Supportive care to relieve symptoms may include applying intermittent ice or heat to the affected neck area, and pain relievers. Warm salt water gargles, soft foods, and extra fluids may also help. Avoid fruit juice or acidic foods, since these stimulate the salivary glands, which can be painful.
CNS involvement
Orchitis
Pancreatitis
DeafnessDeath
15% of clinical cases
20% - 50% in post- pubertal males
2% - 5%1 / 20,000
1 - 3 / 10,000Mumps Complications
Mumps Epidemiology
Reservoir HumanTransmission Respiratory drop nuclei
Subclinical infections may transmit
Temporal pattern Peak in late winter and spring
Communicability Three days before to five
days after onset of activedisease
During adulthood, infection is likely to produce more sever disease including orchitis.
Death attributable to mumps is rare, the estimated case fatality rate is 3.8 per 10000. more than fatalities occur in people older than 19 years of age.Mumps infection during the first trimester of pregnancy is associated with an increased risk of spontaneous abortion.
There is no evidence exists that mumps infection during pregnancy causes congenital malformations.
Peak incidence was between January and May
Treatment: Supportive
Isolation of the hospitalized patient: in addition to standard precautions, droplet precautions are recommended until 9 days after onset of parotid swelling.
Control Measures:
1- School and child care : children should be excluded for 9 days from the onset of parotid swelling
2- Care of exposed people: vaccine not effective in preventing infection after exposure. However mumps vaccine can be given after exposure, because Immunization will provide protection against subsequent exposure. .Immunization during the incubation period has no increased risk. Mumps Ig is of no value
Mumps Vaccine:
This is generally given as measles-mumps-rubella (MMR) vaccine. MMR is usually given on or after a child's first birthday. A second vaccination is recommended, again in combination with measles and rubella vaccine, at 4-6 years of age. Persons of any age who are unsure of their mumps disease history and/or mumps vaccination history should be vaccinated, especially if they are likely to be exposed.
Mumps Vaccine
Composition Live virusEfficacy 95% (Range, 90% - 97%)
Duration ofImmunity Lifelong
Schedule 2 Doses (as MMR)
Should be administered with measles and rubella (MMR)
Mumps Vaccine (MMR) IndicationsAll infants >12 months of age
Susceptible adolescents and adults without documented evidence of immunity
Second Dose Recommendations
First dose of MMR at 12-15 monthsSecond dose of MMR at 4-6 years
Second dose may be given any time >4 weeks after the first dose
Second Dose of MMR Vaccine
Intended to produce immunity in persons who failed to respond to the first dose (primary vaccine failure)
The second dose of MMR is recommended to produce immunity in those 2-5% who failed to respond the first dose. It’s not technically a booster dose, although the second dose may also boost antibody titers in some of those who did respond to the first dose.
What can be done to prevent the spread of mumps?
The single most effective control measure is maintaining the highest possible level of immunization in the community.Children with mumps should not attend school, and adults should not work, until five days after swelling began or until they are well, whichever is longer. Measures such as covering coughs and sneezes, washing hands frequently, and not sharing food or eating utensils can also help. A person who may have had contact with a mumps case should be evaluated by their physician.
However
High MMR vaccine coverage levels and vaccine effectiveness likely prevented thousands of additional mumps cases (9 out of 10 exposures that may have resulted in infection in 2 dose vaccinees prevented)Incidence relatively low
Disease may be modified
Adverse Reactions:
febrile seizures, nerve defness,meningitis, encephalitis, rash ,pruritis .orchitis and parotitis have been reported rarely.Precautions and Contraindications:
1- Febrile illness: fever is not contraindication to immunization . However if other manifestations suggest a more serious illness , the child should not be immunized until recovered .
2-Allergies
3- Recent administration of immune globulin: because high dose of Ig can inhibit the response to measles vaccine for longer intervals , MMR immunization should be deferred for a longer period after administration of IG.4- Altered immunity : patients with immunodeficiency diseases or people receiving immunosuppressive therapy except patients with HIV infection.
5. Corticosteroids: the recommended interval is at least one month after steroids is discontinued.
Pregnancy: live – virus mumps vaccine can infect the placenta but the virus has not been isolated from fetal tissue
However conception should be avoided for 28 days after mumps immunization.
Out break control :
Exclusion of susceptible students from affected schools judged by local public health authorities to be at risk of transmission should be considered.