THYROID DISEASES
1PRESENTING PROBLEMS IN THYROID DISEASE
HypothroidismThyrotoxicosis
Goitre
Malignancy and other tumors
Autoimmune disease
Sick euthyroid syndrome
2
Clinical syndromes
TSH T4 T3 DiseaseUndetectable Raised Raised Primary thyrotoxicosis
Undetectable Normal Raised Primary T3-toxicosis
Undetectable Normal Normal Subclinical thyrotoxicosis
Undetectable Raised L, N, H Sick euthyroidism/non-thyroidal illness
Undetectable Low Low Secondary hypoth,Transient thyroiditis
Normal Low Low Secondary hypothyroidism
elevated 5-20 Low Low Primary or Secondary hypothyroidism
Elevated > 20 Low Low Primary hypothyroidism
elevated 5-20 Normal Normal Subclinical hypothyroidism
Elevated 20-500 Normal Normal Artefact
Elevated High High Non-compliance R,Secondary thyrotoxicosis
3
Thyrotoxicosis
EtiologyMultinodular goitre
Autonomously functioning solitary thyroid nodule
Thyroiditis
Subacute (de Quervain's) Post-partum
Iodide-induced Drugs (e.g. amiodarone)Radiographic contrast mediaIodine prophylaxis programme
Extrathyroidal source of thyroid hormone Factitious hyperthyroidismStruma ovarii
TSH-induced TSH-secreting pituitary adenomaChoriocarcinoma and hydatidiform mole
Follicular carcinoma ± metastases
4
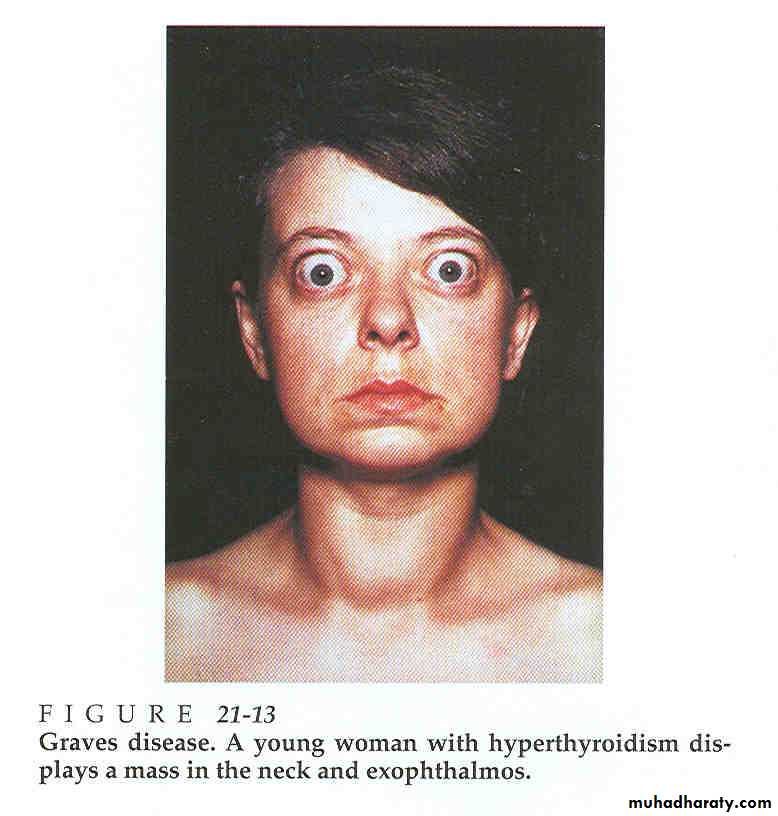
Graves Disease
Autoimmune disorderAbs directed against TSH receptor with intrinsic activity. Thyroid and fibroblasts
Responsible for 60-80% of Thyrotoxicosis
More common in women
5
Clinical features
weight loss with a normal or increased appetite
heat intolerance
palpitations, tremor and irritability
Tachycardia, AF
palmar erythema
lid lag. lid retraction
palpable goitre, but experienced clinicians can discriminate the diffuse soft goitre of Graves' disease from the irregular enlargement of a multinodular goitre.
Graves' disease causes other features of ophthalmopathy, including periorbital oedema, conjunctival irritation, exophthalmos and diplopia.
Pretibial myxoedema
6
7
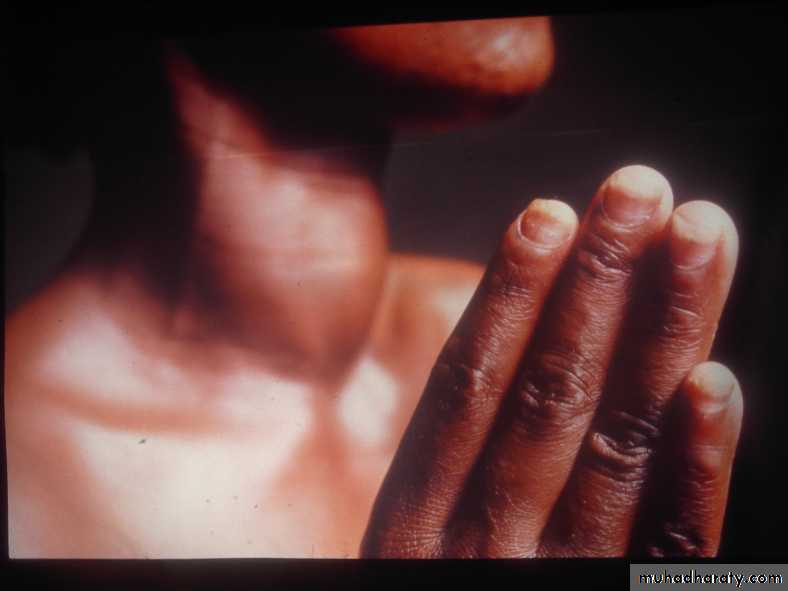
Graves Disease Other Manifestations
Pretibial mixoedemaThyroid acropachy
Onycholysis
Thyroid enlargement with a bruit frequently audible over the thyroid
8
Graves Disease Eye Signs
N - no signs or symptomsO – only signs (lid retraction or lag) no symptoms
S – soft tissue involvement (peri-orbital oedema)
P – proptosis (>22 mm)(Hertl’s test)
E – extra ocular muscle involvement (diplopia)
C – corneal involvement (keratitis)
S – sight loss (compression of the optic nerve)
9
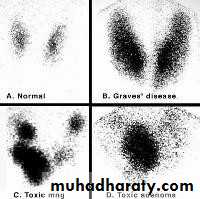
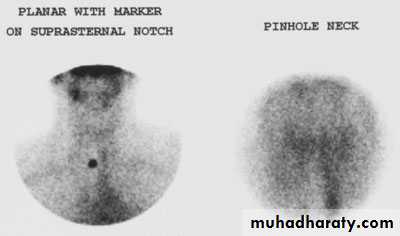
Diagnosis of Graves Disease
TSH , free T4 Thyroid auto antibodies
Nuclear thyroid scintigraphy (I123, Te99)
10
Management
Antithyroid drugs are introduced at high doses, e.g. carbimazole 40-60 mg daily or prophylthiouracil 400-600 mg daily. There is subjective improvement within 10-14 days and the patient is usually clinically and biochemically euthyroid at 3-4 weeks, when the dose can be reduced. The maintenance dose is determined by measurement of T4 and TSH(1-2y).Subtotal thyroidectomy Patients must be rendered euthyroid with antithyroid drugs before operation. Potassium iodide, 60 mg 8-hourly orally, is often added for 2 weeks before surgery to inhibit thyroid hormone release and reduce the size and vascularity
Radioactive iodine 131I is administered orally as a single dose and is trapped and organified in the thyroid
B-blockers to control symptoms, steroid for ophthalmopathy
11
Hypothyroidism
Clinical featuresdepend on the duration and severity of hypothyroidism.
infiltration of many body tissues by the mucopolysaccharides, hyaluronic acid and chondroitin sulphate
low-pitched voice and poor hearing
slurred speech due to a large tongue
carpal tunnel syndrome
non-pitting oedema (i.e. myxoedema)
periorbital puffiness is often striking and
facial pallor due to vasoconstriction and anaemia
lemon-yellow tint to the skin due to carotenaemia, purplish lips and malar flush
bradycardia., cold intolerance.
12
13
Hypothyroidism etiology
PrimaryHASHIMOTO'S thyroiditis posess positive thyroid peroxidase autoantibodies and a firm goitre who may or may not be hypothyroid
'spontaneous atrophic hypothyroidism' for hypothyroid patients without a goitre in whom TSH receptor-blocking antibodies may be more important than antiperoxidase antibodies.
Post-thyroid abalation
Iodin and other drugs
Radiation
Secondary hypothyroidism
Hormone resistance
14
Transient Hypothyroidism
during the first 6 months after subtotal thyroidectomy131I treatment of Graves' disease
post-thyrotoxic phase of subacute thyroiditis
post-partum thyroiditis.
15
Lab Investigations of Hypothyroidism
TSH , free T4
Ultrasound of thyroid – little value
Thyroid scintigraphy – little value
Anti thyroid antibodies – anti-TPO
S-CK , s-Chol , s-Trigliseride
Normochromic or macrocytic anemia
ECG: Bradycardia with small QRS complexes
16
Treatment of Hypothyroidism
LevothyroxineIf no residual thyroid function 1.5 μg/kg/day
Patients under age 60, without cardiac disease can be started on 50 – 100 μg/day. Dose adjusted according to TSH levels
In elderly especially those with CAD the starting dose should be much less (12.5 – 25 μg/day)
17
SUBACUTE (DE QUERVAIN'S) THYROIDITIS
patients are usually females aged 20-40 yearsIn its classical painful form, subacute thyroiditis is a virus-induced (e.g. Coxsackie, mumps or adenovirus) transient inflammation of the thyroid gland.
pain may radiate to the angle of the jaw and the ears, and is made worse by swallowing, coughing and movement of the neck
inflammation in the thyroid gland is associated with release of colloid and stored thyroid hormones, but also with damage to follicular cells and impaired synthesis of new thyroid hormones. As a result, T4 and T3 levels are raised for 4-6 weeks until the pre-formed colloid is depleted.
a period of hypothyroidism of variable severity before the follicular cells recover and normal thyroid function is restored within 4-6 months
Low-titre thyroid autoantibodies appear transiently in the serum, and the erythrocyte sedimentation rate (ESR) is usually raised
NSAID ,prednisolone 40 mg daily for 3-4 weeks
18
Acute Thyroiditis
Bacterial – Staph, Strep
Fungal – Aspergillus, Candida, Histoplasma, Pneumocystis
Radiation thyroiditis
Amiodarone (acute/ sub acute)
Painful thyroid, ESR usually elevated, thyroid function normal
19
Chronic Thyroiditis
Hashimoto’sAutoimmune
Initially goiter later very little thyroid tissue
Rarely associated with pain
Insidious onset and progression
Most common cause of hypothyroidism
TPO abs present (90 – 95%)
20
Thyroiditis
The most common form of thyroiditis is Hashimoto thyroiditis, this is also the most common cause of long term hypothyroidism
The outcome of all other types of thyroiditis is good with eventual return to normal thyroid function
21
Solitary Thyroid Nodule
HistoryDuration, recent enlargement, voice change, H/O hypo/hyperthyroidism, irradiation, F/H goitre/cancer
Physical examination
Dominant nodule, movement on deglutition, cervical lymph nodes, fixation, hardnessThyroid function studies
Serum TSHT4 & T3 levels
Antibody levels; ATA, AMA 1:100
Thyroid imaging; Scanning (99mTc, 123I, 131I)
22
Solitary Thyroid Nodule
CXRUltrasound
Solid/cystic
Multicentric
Lymph node involvement
Ultrasound-assisted FNA
CT/MRI of neck
Mainly for large/recurrent cancers
Vascular/lymphatic invasion
Cervical/mediastinal metastasis
23
Solitary Thyroid Nodule
• Serum TSH low ScintiscanInadequate Repeat FNA
24
Thyroid Cancer
Incidence 1%M/F ratio 3:1
Risk factors
Radiation exposure
External
Medical treatment for benign conditions
Medical treatment for malignancies
Environmental exposure- Nuclear weapons or accidents
Internal
Medical treatment of benign condition with I131
Diagnostic tests with I131
Environmental- fallout from nuclear weapons
Other factors
Diet- Iodine deficiency, goitrogens
Hormonal factors- female gender predominance
Benign thyroid disease
Alcohol
25
Thyroid Cancer
Pathology
Papillary carcinoma;
60-70% of all cases
Multifocal
Nonencapsulated, but circumscribed
Lymphatic spread
80% 10 year survival
Follicular carcinoma
15-20% of thyroid cancers
Usually encapsulated
60% 10 year survival
26
Thyroid Cancer
Hurthle cell neoplasm5% of thyroid cancers
Variant of follicular cancer
Lymph node spread slightly higher than follicular cancer
Lees avidity for 131I
Medullary cancer
Parafollicular C cells
Autosomal dominance inheritance in 20%
Unilateral involvement in sporadic, bilaterality in familial forms
Calcitonin secretion
Metastasis both by lymphatic and blood stream
10 year survival 90% in localised disease, 70% with cervical mets, 20% with distant mets
27
Thyroid cancer
Anaplastic cancer
Undifferentiated
Rapidly growing, often inoperable
Invade locally, metastasize both locally and distantly
Mean survival 6 months
5 year survival rate 7%
Lymphoma
Rare, rapidly enlarging tumour
Primary or secondary
Seventh decade, 6:1 F/M ratio
5 year survival rate 75-80%, when confined to thyroid
28
Thyroid cancer
Treatment of thyroid cancerPapillary cancer
< 1.5 cms Lobectomy & isthmusectomy
> 1.5 cms Total thyroidectomy
Follicular cancer Total thyroidectomy
Hurthle Total thyroidectomy
Medullary Total thyroidectomy & central neck dissection
29Thyroid cancer
Adjuvant therapyTSH suppression
Post operative radioactive Iodine ablation
External beam radiotherapy
Surveillance
Serum thyroglobulin levelsCXR or CT scan
Repeat 131I if positive
30