Assistance Prof. Dr .Ghazi F. Haji
CardiologistArrhythmias
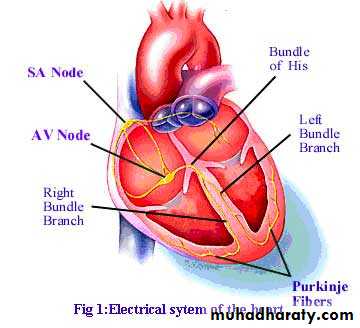
A cardiac arrhythmia
@is a disturbance of the electrical rhythm of the heart@Arrhythmias are might be occur in :
1- structural heart disease
2-healthy heart.
A heart rate > 90/min is tachycardia
heart rate < 60/min is a bradycardia.
Mechanisms of tachycardia
• Increased automaticity..• Re-entry. (Most tachyarrhythmias are due to re-entry).
• Triggered activity..
Mechanisms of Bradycardia may be due to:
• Reduced automaticity, e.g. sinus bradycardia.
• Blocked or abnormally slow conduction, e.g. AV block
Classification of arrhythmia ;
1- Supraventricular (Narrow QRS complex )
(sinus ,atrial .junctional)
2-Ventricular (wide ,bizzar QRS complex)
Sometime :supraventricular with wide QRS complex
1-BBB2-accessory conduction
Noticeable arrhythmia symptoms may include:
A fluttering in your chestA racing heartbeat (tachycardia)
A slow heartbeat (bradycardia)
Chest pain
Shortness of breath
Lightheadedness
Dizziness
Fainting (syncope) or near fainting
Polyurea
Sinus rhythm :
@Sinus arrhythmia : change in heart rate during respiration (increase in inspiration VS expirat)occur in children,autonomic neuropathy
@Sinus bradycardia :
In -atheletic -sleep
MI.
Sinus node dysfunction(sick sinus syndrom(tachy-brady syndrome)
hypothyroidism,hypothermia,cholestaesis juandic
increase intracranial pressure .
drugs (b-blocker .calcium channel blocker .antiarrhythmic drugs)
Treatment : (if asymptomatic –no treatment .if symptomatic -atropin) pacemaker if not response
@Sinus tachycardia: (physiological ,pathological)
The upper limit of normal rate for sinus tachycardia is thought to be 220 bpm minus age.cause by anxiety ,fever. anemia. thyrotoxosis .phaeochrmocytoma .pregnancy .heart failure ,drugs(sympathomametic ,b-agoinst like ventolin,butadinie )
Treatment :if asymptomatic not need treatment
if ymptomatic :treated depend on types , onset and hemodynamic status
Atrial rhythm :
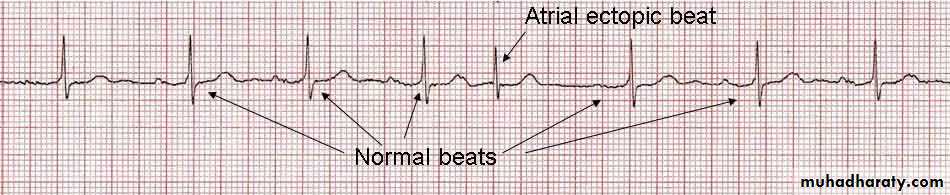
#Atrial ectopic beat (extrasystolic ,premature beat)no symptoms or sensation of a missed beat or an abnormally strong beat.
The ECG –shows a premature but otherwise normal
QRS complex; if visible, the preceding P wave has a
different morphology
Treatment ;avoid coffee.tea,stress@ .b blocker
Atrial tachycardia
@Atrial tachycardia caused by sinoatrial disease or digoxin toxicity.@It produces a narrow complex tachycardia with abnormal P-wave morphology.
@Treatment :
β-blockers
class I or III anti-arrhythmic drugs
.Catheter ablation.
Atrial flutter
due to a large (macro) re-entry circuit, usually within the RA encircling the tricuspid annulus.The atrial rate is approximately 300/min, and is usually associated with 2:1, 3:1 or 4:1 AV block.
The ECG shows saw-toothed flutter waves .
Management
Treatment :1-Carotid sinus pressure or intravenous adenosine may help to establish the diagnosis
2-Digoxin, β-blockers or verapamil can be used to control the ventricular rate .
3-direct current (DC) cardioversion or by using intravenous amiodaron
4-Beta-blockers or amiodarone can also be used to prevent recurrent episodes of atrial flutter.
5-Catheter ablation offers a 90% chance of complete cure
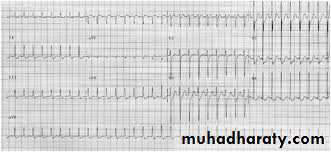
Atrial fibrillation
@Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, with an overall prevalence of 0.5%,The prevalence rises with age,
@Due to multiple re-entry circuits looping around the atria.
@‘irregularly irregular’ pulse.
The ECG -irregular QRS complexes; there are no P waves.
@AF can be classified
Paroxysmal –self terminated within 7days
Persistent –last more than 7 days
Permanent- if not terminated or relapse within 24hof cardio version
Lone –absence of structural heart disease ,
@structural remodelling occurs with atrial fibrosis and dilatation that further predispose to AF
@ AF is often completely asymptomatic
@AF can cause palpitation, breathlessness and fatigue. In patients with poor ventricular function or valve disease it may precipitate or aggravate cardiac failure
.@A fall in BP may cause lightheadedness, and chest pain may occur with underlying coronary disease.
@AF is associated with significant morbidity and a twofold increase in mortality
Common causes of atrial fibrillation
• Coronary artery disease(including acute MI)
• Valvular heart disease,
especially rheumatic mitral valve disease
• Hypertension
• Sinoatrial disease
• Hyperthyroidism
• Alcohol
• Cardiomyopathy
• Congenital heart disease
• Chest infection
• Pulmonary embolism
• Pericardial disease
• Idiopathic (lone AF)
Management
Assessment of patients with newly diagnosed AF includes
a full history, physical examination, 12-lead ECG, echocardiogram,thyroid function tests. ect
The goal of treatment:
1-restore sinus rhythm
2-prevent recurrent episodes of AF,
3-, minimize the risk of thromboembolism
Paroxysmal atrial fibrillation
1-not necessarily require treatment.2-Beta-blockers are normally used
Beta-blockers reduce the ectopic firing that normally initiates AF.
3-Class Ic drugs such as propafenone or flecainide, are also effective at
preventing episodes but should not be given to patients with coronary disease or left ventricular dysfunction
.4-Amiodarone is the most effective agent for preventing AF but its side-effects restrict its use to patients
.@Digoxin and verapamil are not effective drugs for preventing paroxysms of AF,
If no response or because of side effects of drugs –can do
5-Cardiac ablation -Ablation prevents AF in
approximately 70% of patients. Complication s are
*small risk of embolic
*stroke or cardiac tamponade.
Persistent and permanent atrial fibrillation
There are two options for treating persistent AF:
$= rhythm control: attempting to restore and maintain sinus rhythm
$=rate control: accepting that AF will be permanent and
$=prevent embolic complications.
Rhythm control. An attempt to restore sinus rhythm
Attempts to restore and maintain sinus rhythm are most successful1- if AF has been present for < 3 months
2-the patient is young
3- no important structural heart disease.
1-Immediate DC cardioversion after the administration of intravenous heparin is appropriate if AF has been present for < 48 hours.
2-Chemical cardioversion is performed with drugs, such as amiodarone, dronedarone, procainamide, dofetilide, ibutilide, propafenone, or flecainide.(Vernakalant, an investigational drug)
In other situations, >48h AF--DC cardioversion deferred until the patient has been established on warfarin, with an international normalised ratio (INR) > 2.0 for a minimum of 4 weeks,.
3-Anticoagulation should be maintained for at least 3 months following successful cardioversion
Concomitant therapy with amiodaroneor β-blockers may reduce the risk of recurrence.
4-Catheter ablation( radiofrequency ablation The Maze procedure)
but it is a less effective treatment for persistent AF than for paroxysmal AF.Rate control. If sinus rhythm cannot be restored, treatment
should be directed at maintaining an appropriate heart rate.
@Digoxin, β-blockers or rate-limiting calciu m antagonists such as verapamil or diltiazem
@catheter ablation+a permanent pacemaker
must be implanted beforehand. This is known as
the ‘pace and ablate’ strategy.
Prevention of thromboembolism
Loss of atrial contraction and left atrial dilatation cause stasisof blood in the LA and may lead to thrombus formation
in the left atrial appendage. This predisposes patients to
stroke and other forms of systemic embolism.
@warfarin (target INR 2.0–3.0) reduces the risk of stroke by about two-thirds,
@aspirin reduces the risk of stroke by only one-fifth
.
@Echocardiography is valuable in risk stratification.
CHA2DS2-VASc
1Congestive heart failure
C
1
Hypertension>
140/90
H
2
Age>75y
A2
1
Diabetes
D
2
Prior Stroke or TIA or thromboembolism
S2
1
Vascular diseasesVascular disease (e.g. peripheral artery disease, myocardial
V
1
Age 65-74y
A
1
Sex category (female )
Sc
consideration
Anticoagulant
Risk
• Score
Aspirine dialy
None or aspirin
low
0
Aspirine dialy or riase to INR2-3
Aspirine ,warfarin or other
moderate
1
Riase INR 2-3
Warfarin or other anticoagulant
dabigatran, rivaroxabanand apixaban
Moderate to high
2 or more
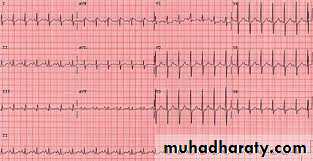
Quiz 1-describe the ECG2- What are the treatment
Supraventricular’ tachycardias
(SVT) is a narrow QRS complex :Atrioventricular nodal re-entrant tachycardia (AVNRT)(120-240/m)
@This is due to re-entry in a circuit involving the AV node and its two right atrial input pathways: a ‘fast’ pathway and ‘slow’ pathway .
@It tends to occur in hearts that are otherwise normal and episodes may last from a few seconds to many hours.
1-a fast heart beat and may feel faint or breathless.
2-Polyuria,
The ECG usually shows a tachycardia with normal QRS complexes
Supraventricular tachycardia
Management
Treatment is not always necessary.@ carotid sinus pressure or other
Measures that increase vagal tone (e.g. Valsalva manoeuvre)
@Intravenous adenosine or verapamil
@Suitable alternative drugs
include β-blockers or flecainide.
@In severe haemodynamic compromise, the tachycardia
should be terminated by DC cardioversion
@If episodes are frequent or disabling, prophylactic
oral therapy with a β-blocker or verapamil may be indicated.
@Catheter ablation offers a high chance ofcomplete cure and is usually preferable to long-term drug treatment.
Wolff–Parkinson–White syndromeand atrioventricular re-entranttachycardia(AVRT)
@In these conditions, an abnormal band of conductingTissue connects the atria and ventricles. is known as an accessory pathway.
50%-concealed accessory pathway -\ does not alter the appearance of the ECG in sinus rhythm.
50%--conduction takes place partly through the AV node and partly through the accessory pathway-short PR interval and a ‘slurring’ of the QRS complex, called a delta wave known as Wolff Parkinson–White syndrome.
The ECG appearance of this tachycardia may be indistinguishable from that of AVNRT .
. @. It should be treated as an emergency, usually with DC cardioversion.
@If atrial fibrillation occurs, it may produce a dangerously rapid ventricular rate because the accessory pathway lacks the rate-limiting properties of the AV node .@Prophylactic anti-arrhythmic drugs, such as flecainide, propafenone or amiodarone , can also be used. Catheter ablation is first-line treatment in symptomatic patients and is nearly always curative
@Digoxin and verapamil shorten the refractory period of the accessory pathway and should be avoided.
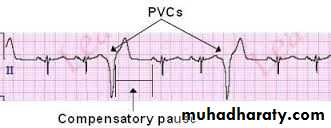
Ventricular tachy arrhythmias
@Ventricular ectopic beats(extrasystoles, premature beats)ventricular ectopic beats are premature, broad and bizarre
The complexes may be unifocal or multifocal
. ‘Couplet’ and ‘triplet’ ‘bigeminy’.
@Ectopic beats produce a low stroke volume because left ventricular contraction occurs before filling is complete.
@The pulse is therefore irregular, with weak or missed beats
.@ Patients are usually asymptomatic but may complain of an irregular heart beat, missed beats or abnormally strong beats.
Ventricular ectopic beats in otherwise healthy subjects
increases with age. disappear with exercise.
@Treatment is not necessary unless the patient is highly symptomatic, in which case β-blockers can be used.
@investigations such as an echocardiogram (looking for structural heart disease) and an exercise stress test (to detect underlying ischaemic heart disease).
Ventricular ectopic
Ventricular ectopic beats associatedwith heart disease
@acute MI . Persistent, frequent (> 10/hour) ventricular ectopic beats in patients who have survived the acute phase of MI indicate a poor long-term outcome.Other than β-blockers, anti-arrhythmic drugs do not improve and may even worsen prognosis.
..
Treatment should be directed at the underlying condition.
Ventricular tachycardia (VT)
@The common causes of VT includeacute MI,
cardiomyopathy
@chronic ischaemic heart disease particularly when it is associated with a ventricular aneurysm or poor left ventricular function.
@It is caused by abnormal automaticity or triggered or by re-entry within.
@Patients may complain of palpitation or symptoms of low cardiac output, such as dizziness, dyspnoea or syncope.
The ECG shows tachycardia with broad, abnormal QRS complexes with a rate > 120/min .
VT may be difficult to distinguish from SVT with bundle branch block or pre-excitation(WPW syndrome).
Wide QRS
Narrow QRS@idioventricular rhythm (‘slow’ VT) at a rate only slightly above the preceding sinus rate and below 120/ min. These episodes often reflect reperfusion of the infarct territory and may be a good sign. They are usually self-limiting and asymptomatic, and do not require treatment.
@(‘normal heart VT’), usually because of abnormal automaticity in the right ventricular outflow tract or one of the fascicles of the left bundle branch. The prognosis is good and catheter ablation can be curative
Management
@Synchronised DC cardioversion is the treatment of choice if systolic BP is < 90 mmHg.@intravenous amiodarone may be given as a bolus followed by a continuous infusion
@Intravenous lidocaine can be used but may depress left ventricular function, causing hypotension or acute heartfailure.
@ Hypokalaemia, hypomagnesaemia, acidosis and hypoxaemia should be corrected.
@Beta-blockers .
@ Class Ic anti-arrhythmic drugs should not be used for prevention of VT in patients with ischaemic heart disease
In patients at high risk of arrhythmic death (e.g. those with poor left ventricular function, or where VT is associated with haemodynamic compromise), the use of an implantable cardiac defibrillator is recommended .
Features in favour of ventricular tachycardia inthe differential diagnosis of broad-complex tachycardia
@History of MI
• AV dissociation (pathognomonic)
• Capture/fusion beats (pathognomonic,)
• Extreme left axis deviation
• Very broad QRS complexes (> 140 ms)
• No response to carotid sinus massage or i.v. adenosine
Torsades de pointes (ventriculartachycardia) Polymorphic VT
@The ECG shows rapid irregular complexes that oscillate from an upright to an inverted position and seem t twist around the baseline as the mean QRS axis changes@degenerate into ventricular fibrillation
@During periods of sinus rhythm, the ECG will usually show
a prolongeQT interval (> 0.42 s at a rate of 60/min).
.@The arrhythmia is more common in women and is often
triggered by a combination of aetiological factors (e.g.
QT-prolonging medications and hypokalaemia).
Causes of long QT interval and torsades depointes
BradycardiaElectrolyte disturbance
• Hypokalaemia
• Hypomagnesaemia
• Hypocalcaemia
Drugs
• Disopyramide (and other class Ia anti-arrhythmic drugs, p. 573)
• Sotalol, amiodarone (and other class III anti-arrhythmic drugs)
• Amitriptyline (and other tricyclic antidepressants)
• Chlorpromazine (and other phenothiazines)
• Erythromycin (and other macrolides)
Congenital syndromes
• LQT1: gene affected KCNQI: K+ channel, 30–35%
• LQT2: gene affected HERG: K+ channel, 25–30%
• LQT3: gene affected SCNSA: Na+ channel, 5–10%
• LQT4–12: rar
@Thecongenital long QT syndromes are a family of genetic disorder.
@Treatment should be directed at the underlying cause. Intravenous magnesium should be given in all cases.
@Atrial pacing.
@Intravenous isoprenaline is a reasonable alternative to
pacing.
.@ Beta-blockers are effective at preventing syncope in patients with congenital long
Sinoatrial disease (sick sinus syndrome)
@occur at any age but is most common in older people.@The underlying pathology involve fibrosis, degenerative changes or ischaemia of the SA(sinus) node.
@may present with palpitation, dizzy spells or syncope, due to intermitten tachycardia, bradycardia, or pauses with no atrial or ventricular activity (SA block or sinus arrest)
@A permanent pacemaker.
Common features of sinoatrial diseaseSinus bradycardia
• SA block (sinus arrest)
• Paroxysmal atrial tachycardia
• Paroxysmal atrial fibrillation
• AV block
Atrioventricular and bundle branchblock
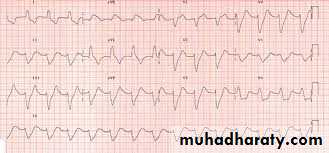
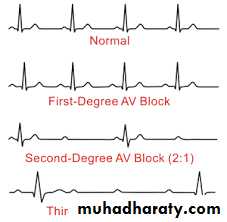
First-degree AV block
In this condition, AV conduction is delayed so the PR
interval is prolonged (> 0.20 s;). It rarely causes
symptoms.
Second-degree AV block.
In Mobitz type I second-degree AV block :there is progressive lengthening of successive PR intervals culminating in a dropped beat.. This is known as Wenckebach’s phenomenon and is usually due to impaired conduction in the AV node itself..In Mobitz type II second-degree AV block -the PR interval of the conducted impulses remains constant but some P waves are not conducted. This is usually caused by disease of the His–Purkinje system and carries a risk of asystole.
.
Third-degree (complete) AV block
When AV conduction fails completely, the atria and ventriclesbeat independently (AV dissociation, ) Complete AV block -produces a slow (25–50/min), regular pulse that,.
.
Cannon waves may be visible in the neck and the intensity of the firstheart sound varies due to the loss of AV synchrony
Aetiology of complete AV block
CongenitalAcquired
• Idiopathic fibrosis
• MI/ischaemia
• Inflammation
Acute (e.g. aortic root abscess in infective endocarditis)
Chronic (e.g. sarcoidosis, p. 708; Chagas disease, p. 354)
• Trauma (e.g. cardiac surgery)
• Drugs (e.g. digoxin, β-blocker)
Stokes–Adams attacks
Episodes of ventricular asystole may complicate completeheart block or Mobitz type II second-degree AV
block, or occur in patients with sinoatrial disease
This may cause recurrent syncope or ‘Stokes–
Adams’ attacks.A typical episode is characterised by sudden loss of
consciousness that occurs without warning and results
in collapse..
AV block complicating acute MI
Acute inferior MI is often complicated by transient AV
block because the RCA supplies the AV node.
if the patient remains well, no treatment is required.
Symptomatic second- or third-degree AV block may respond to atropine(0.6 mg i.v., repeated as necessary) or, if this fails, a temporary pacemaker.
In most cases the AV block will resolve within 7–10 days.
Second- or third-degree AV heart block complicating
acute anterior MI indicates extensive ventricular damage
involving both bundle branches and carries a poor prognosis.
Bundle branch block and hemiblock
Conduction block in the right or left bundle branchcan occur as a result of many pathologies, including
Ischaemic or hypertensive heart disease or cardiomyopathies
.
This causes delayed conduction into the LV or RV,
broadens the QRS complex (≥ 0.12 s) and produces
the characteristic alterations in QRS morphology
Right bundle branch block (RBBB can occur in healthy people but left bundle branch block (LBBB) often signifies important underlying
heart disease.
The combination of right bundle branch and left anterior or posterior hemiblock is known as bifascicular block
Common causes of bundle branch block
Right bundle branch block• Normal variant
• Right ventricular hypertrophy or strain, e.g. pulmonary embolism
• Congenital heart disease, e.g. atrial septal defect
• Coronary artery disease
Left bundle branch block
• Coronary artery disease
• Hypertension
• Aortic valve disease
• Cardiomyopathy
Anti-arrhythmic drug therapy
Classification of anti-arrhythmic drugsaccording to effect on the intracellular action potentialClass I: membrane-stabilising agents (sodium channel blockers)
(a) Block Na+ channel and prolong action potential
• Quinidine, disopyramide
(b) Block Na+ channel and shorten action potential
• Lidocaine, mexiletine
(c) Block Na+ channel with no effect on action potential
• Flecainide, propafenone
Class II: b-adrenoceptor antagonists (b-blockers)
• Atenolol, bisoprolol, metoprolol, I-sotalol
Class III: drugs whose main effect is to prolong the action potential
• Amiodarone, d-sotalol
Class IV: slow calcium channel blockers
• Verapamil, diltiazem
N.B. Some drugs (e.g. digoxin and adenosine) have no place in this
classification, while others have properties in more than one class:
e.g. amiodarone, which has actions in all four classes.
Other anti-arrhythmic drugs
Atropine sulphate (0.6 mg i.v., repeated if necessary to
a maximum of 3 mg).
Adenosine. Must be given intravenously. It produces transient AV block lasting a few seconds.
Adenosine is givenas an intravenous bolus, initially 3 mg over 2 seconds If there is no response after 1–2 minutes, 6 mg should be given; if necessary, after another 1–2 minutes, the maximum dose of 12 mg may be given.
Patients should be warned that they may experience short-lived and sometimes distressing flushing, breathlessness and chest pain. Adenosine can cause bronchospasm and should be avoided in asthmatics; its effect are greatly potentiated by dipyridamole and inhibited by theophylline and other xanthines.
Response to intravenous adenosine
Arrhythmia ResponseSupraventricular tachycardia Termination
Atrial fibrillation, atrial flutter Transient AV block
Ventricular tachycardia No effect
Digoxin. A purified glycoside from the European foxglove, Digitalis lanata, which slows conduction and prolongs the refractory period in the AV node..
Digoxin is largely excreted by the kidneys, and the maintenance dose should be reduced in children, older People and those with renal impairment.
It is widely distributed and has a long tissue half-life (36 hours), so that effects may persist for several days after th last dose..
Therapeutic procedures
External defibrillation and cardioversionThis will interrupt any arrhythmia and produce a brief period of asystole -that is usually followed by the resumption of sinus rhythm.
Defibrillators deliver a DC, high-energy, short-duration shock via two metal paddles coated with conducting jelly or a gel pad, positioned over the upper right sternal edge andthe apex.
Modern units deliver a biphasic shock, during which the shock polarity is reversed mid-shock. This reduces the total shock energy required to depolarise the heart.
Electrical cardioversion
This is the termination of an organised rhythm suchas AF or VT with a synchronised shock, usually under
general anaesthesia.
The shock is delivered immediately after detection of the R wave,
High-energy shocks may cause chest wall pain post-procedure, so if there is no urgency it is appropriate to begin with a lower-amplitude shock
(e.g. 50 joules), going on to larger shocks if necessary.
-
Catheter ablation
The technique has revolutionised the management ofmany arrhythmias and is now the treatment of choice for
AVNRT and AV re-entrant (accessory pathway) tachycardias,
when it is curative in > 90% of cases.
Focal atrialtachycardias and atrial flutter can also be eliminated by radiofrequency ablation,
Temporary pacemakers
. Permanent pacemakersImplantable cardiac defibrillators(ICDs)
Primary prevention
• After MI, if LV ejection fraction < 30%
• Mild to moderate symptomatic heart failure on optimal drug
therapy, with LV ejection fraction < 35%
Secondary prevention
• Survivors of VF or VT cardiac arrest not due to transient or
reversible cause
• VT with haemodynamic compromise or significant LV
impairment (LV ejection fraction < 35%)