The Prostate and
Benign Prostatic Hyperplasia
:
اﻟﻣﺣﺎﺿر
د.ﺣﺎرث ﻣﺣﻣد ﻗﻧﺑر
ﻛﻠﯾﺔ
طب
اﻟﻛﻧدي
-
ﺟﺎﻣﻌﺔ
ﺑﻐداد
The Protate
u
The prostate is a fibromuscular and glandular organ lying just inferior to the
bladder The normal prostate weighs about 20 g and contains the posterior urethra,
which is about 2.5 cm in length
u
It starts at 12th week fetal life under androgen effect from the fetal testes.
u
According to the classification of Lowsley, the prostate consists of 5 lobes:
anterior, posterior, median, right lateral, and left lateral. According to McNeal, the
prostate has a peripheral zone, a central zone, and a transitional zone; an anterior
segment; and a preprostatic sphincteric zone.
u
The peripheral zone is (androgen dependent), while the central zone is(non-
androgenic dependent); Therefore castration of baby before puberty lead to
failure of gland development. So the effect of androgen on the prostate
development is documented.
blood supply:
q
Arterial:
ü
Inferior vesical artery
ü
Internal pudendal artery
ü
Middle rectal (haemorrhoidal) artery
q
Venous:
The veins from the prostate drain into the periprostatic plexus,
which has connections with the deep dorsal vein of the penis and the internal
iliac (hypogastric) veins
Nerve supply:
From the sympathetic & parasympathetic nerve plexuses.
Lymphatics:
The lymphatic from the prostate drain into internal iliac(hypogastric), sacral,
vesical , and external iliac lymph nodes.
Benign Prostatic Hyperplasia (BPH)
Epidimiology:
Ø
Usually occur in men a er 50 years of age ( most o en between 60 — 70 y)
Ø
It is rare in Negro & very rare in Japanese
Etiology:
Ø
It may be due to discrepancy between Androgen/Estrogen ratio, with ageing the
androgen decreases & lead to reversible changes of A/E ratio àrelative increase in
estrogenà periurethral gland proliferation
Ø
Cell death & apoptosis is deregulated à imbalance between cell proliferation &
cell death à increase mass
Histology:
Ø
The term BPH refers to well-defined histologic changes characterized by slowly
progressive nodular hyperplasia of the periurethral (transitional) zone
Ø
The hyperplasia is made of many components which may be of epithelial type or
interglandular (Fibromuscular) stroma.
Ø
The adenoma may be of epithelial type (epithelial T. is dominant), fibrous type
(dominant fibrous T.) or mixed fibro muscular adenoma.
Ø
The size of the enlargement that occurs in nodular hyperplasia is unrelated to the
degree of obstruction , the smallest prostates may cause the worst outflow
obstruction & huge glands may cause no obstruction at all.
Pathophysiology:
I.
Urethra: The prostatic urethra is lengthened, sometimes to twice its normal
length, there will be compression of the urethra & verumontanum. The urethra
may be compressed from side to side or to one side.
II.
Bladder: Over time, outflow obstruction leads to characteristic changes in the
bladder & upper urinary tract. these changes may be observed cystoscopically &
radiologically:
1.
Trabeculation: Prominence of the detrusor fibers observed through a cystoscope.
It is a manifestation of increased collagen deposition in the bladder wall. This
finding is often associated with outflow obstruction but may also be seen in
unobstructed bladders (e.g., enuresis, neurogenic bladder dysfunction, idiopathic
bladder instability).
2.
Cellule formation: Extreme degrees of trabeculation allow the vesical mucosa to
be pushed between the muscle fibers of the bladder wall to form small pockets
called cellules.
3.
Diverticulum formation: Herniation of the vesical mucosa through the detrusor
muscle constitutes a bladder diverticulum . Because of stasis of urine within the
diverticulum, they are likely to harbor infection, stones, & urothelial cancer. A
diverticulum near the ureteric orifice may cause vesicoureteral reflux.
4.
bladder calculi: The presence of a bladder stone is a strong evidence of
longstanding bladder outflow obstruction. Bladder calculi form most commonly as
a result of outflow obstruction, residual urine, stasis, & infection.
III.
Upper Tract: With hypertrophy & fibrosis of the detrusor wall, increased work is
required to transport the urinary bolus from the ureter into the bladder. This will
lead to dilatation of the upper tract (Bilateral Hydroureteronephrosis). In the early
stages, the condition appears radiologically as mild dilatation of the distal segment
& elongation & some tortuosity of the ureter.
Cilnical feature:
ü
A decrease in the force of & caliber of the urinary stream is the first & most
frequent symptom.
ü
Frequency is the earliest symptom. At first nocturnal, the patient being obliged to
get up to micturate twice or more during the night. Freq. occur because the patient
can not empty the U.B. completelyà residual urine àthe UB. Will full at a quicker
rate.
ü
Urgency when the vesical sphincter becomes stretched, a little urine escapes into
the normally empty prostatic urethra, causing an intense reflex desire to void.
ü
Hesitancy (difficulty in initiating the stream), patient can not start to urinate.
ü
Acute Urinary Retention.
ü
Chronic Retention with overflow incontinence: the patient complains that urine
constantly dribbles away.
ü
Sustained bladder outlet obst. Plus hypertrophy or overdistention of the bladder
may cause vesicoureteral refluxàHydroureteronephrosisà later on produce renal
failure.
ü
Haematuria: may be a presenting symptom, a drop of blood at the beginning or
end of micturation is not unusual.
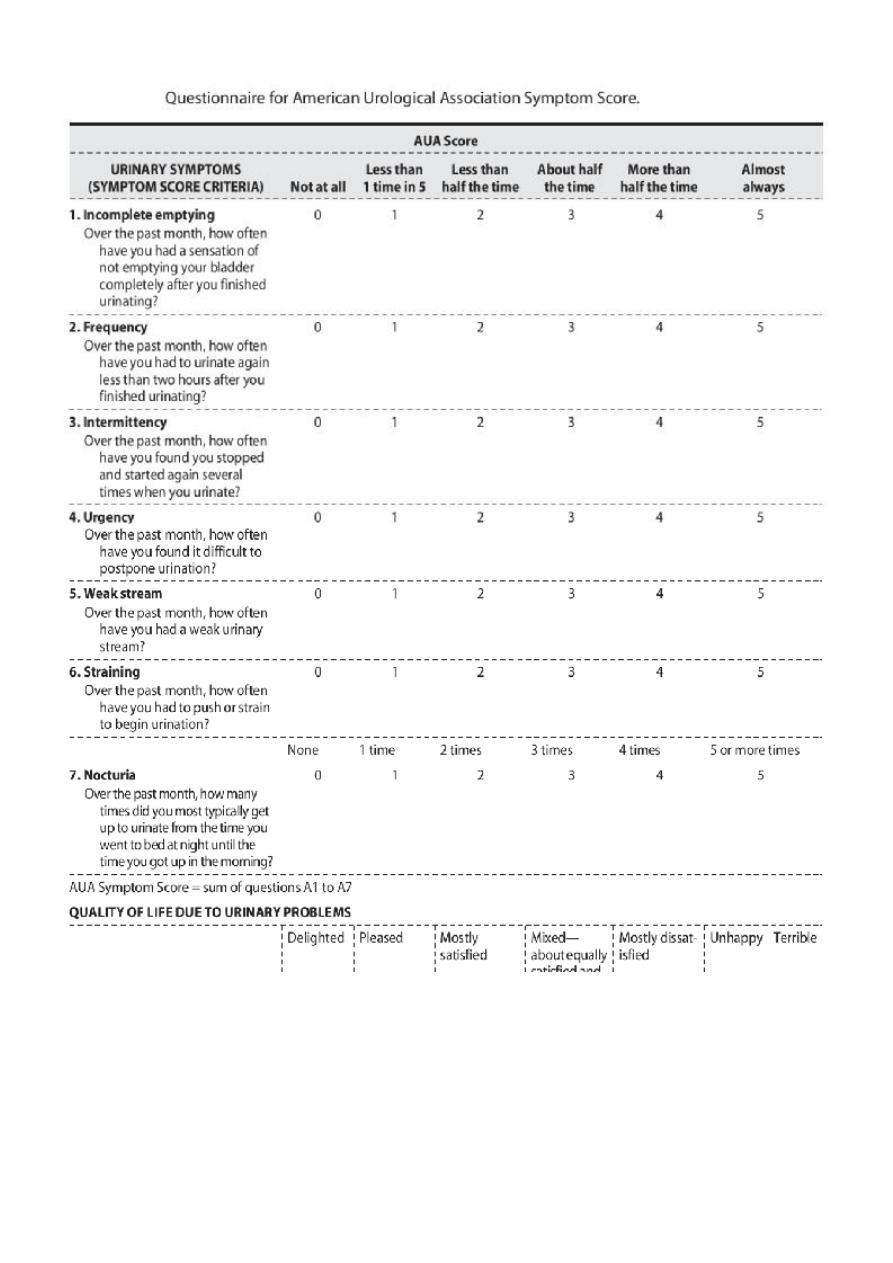
Assessment of the patient with LUTS
q
Abdominal examination: is usually normal. In patients with chronic retention, a
distended bladder will be found on palpation, percussion & sometimes on
inspection.
q
General physical examination may demonstrate signs of chronic renal impairment
with anemia & dehydration.
q
The external urinary meatus should be examined to exclude stenosis, & the
epididymes are palpated for signs of inflammation
q
Rectal examination: in BPH, the posterior surface of the prostate is smooth,
convex, & firm. The rectal mucosa can be made to move over the prostate. Hard or
nodular prostate
gives suspicion of malignancy.
q
Neurological examination:
ü
the nervous syst. Is examined to exclude a neurological lesion.
ü
D.M, tabes dorsalis, M.S, Parkinson’s disease & other neurological states may
mimic prostatic obstion.
ü
examina on of perianal sensa on & anal tone is useful in detec on of an S2 to S4
cauda equina lesion.
Investigations:
§
GUE
§
Blood examination urea, creatinine to assess renal function.
§
PSA (Prostate- Specific Antigen): it is extremely helpful marker in a diagnosis of
prostatic carcinoma which may coexist with the BPH, PSA produced by prostatic
cells & related to how big the prostate is & carcinoma of prostate. If PSA is high (>
4nmol/L) then transrectal US plus transrectal biopsies should be considered.
§
Imaging: US, IVU, it will tell us the renal function, if there is dilatation or not & in
the urinary bladder see any trabeculation, filling defect due to prostatic
enlargement, then do post-voiding film, this will show how much residual urine
there
§
Urodynamics (uroflowmetery & cystometry): this is done if you suspect an atonic
UB or when a clear diagnosis has not been reached.
§
Cystourethroscopy: is the mainstay of diagnosis & should be performed on
patients with haematuria. The urethra is inspected first, & the bladder is then
examined to see trabeculation, stone & diverticulum. It should always be made
before prostatectomy.
Treatment:
I.
Medical Treatment:
A. α- adrenergic blocking agents: The prostate contains smooth muscle that is
controlled by α1 - adrenoreceptors. α- blocker agents have side effects, such as
postural hypotension, tachycardia, palpitations & retrograde ejaculation. e.g.
phenoxybenzamine, Prazosin, Alfuzosin, indoramin, Terazosin, Doxazosin, &
Tamsulosin.
B. Androgen suppressants:
ü the rationale for androgen suppression is observation that the embryonic
development of the prostate is dependent on the androgen dihydrotestosterone
(DHT).
ü Testosterone (T) is produced mainly by testes & to a lesser extent by the adrenals, &
testosterone enters the prostatic cells & converted into an active component (DHT)
by the enzyme 5α-reductase & this enzyme can be inhibited by drugs like
Finasteride (5 α- reductase inhibitor).
ü It will decrease the size of the prostate by 10 — 20%.
ü Median lobe has poor response to androgen suppressants.
II.
Surgical treatment:
surgical removal of prostate by one of the four approaches which are:
ü Open Simple Prostatectomy:
Transvesical Prostatectomy
Retropubic Prostatectomy (Millin
’s Prostatectomy)
ü Transurethral Ressection of the Prostate (TURP):
ü Minimal Invasive Prostatectomy:
o
Transurethral microwave therapy (TUMT).
o
Transurethral needle ablation (TUNA).
o
Photoselective vaporization of the prostate (PVP).
o
Holmium Laser Enucleation of the Prostate (HoLEP).
o
Holmium Laser Ablation of the Prostate (HoLAP).
Ø
The problem with these new methods, is that we can not take a biopsy.
Indications for prostatectomy:
§
Acute urinary retention.
§
Marked hemorrhage from enlarged prostate.
§ P
ersistent or recurrent UTI.
§ R
enal impairment as a result of BOO.
§
Persistent LUTS (Lower Urinary Tract Symptoms) not responding to medical
treatment.
Indications for open prostatectomy:
§
Prostate size >75 gm.
§
Concomitant symptomatic bladder diverticulum
§
Concomitant large, hard bladder stone that cannot be managed transurethrally.
§
Marked ankylosis of the hips that prevents proper placement of the patient in the
dorsal lithotomy position.

Contraindications for open prostatectomy:
§
Small prostate gland.
§
Previous prostatectomy.
§
Prostate cancer.
§
Previous pelvic surgery preventing access to the prostate gland
Post-operative complication of Prostatectomy:
q Local:
Excessive hemorrhage
Perforation
Urinary extravasation
Infection (cystitis, epididymo-orchitis)
Urge or stress incontinence or both
Retrograde ejaculation & impotence
Bladder neck contracture
q General:
DVT
Pulmonary embolism
Water intoxication (TUR syndrome)
Hyponatremia.