Thyroid glands
ProfessorZuhair Bashir Kamal
M.B.Ch.B , CABS
1
Learning objectives
The development and anatomy of thyroid glands.Physiology and investigation of thyroid .
Investigations of thyroid swelling.The management of thyrotoxicosis and hypothyroidism.
The indications for and types of surgical treatment.
Types and management of thyroid cancers.
The risk and complications of thyroid surgery.Tuesday, November 04, 2014
2
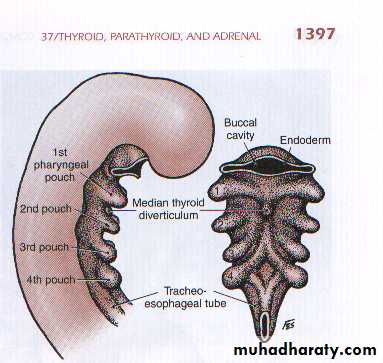
The main analogue (portion) of thyroid gland develops as a median endodermal down growth from the 1st & 2nd pharyngeal pouches.
During its migration caudally, it contacts the ultimobranchial bodies developing from the 4th pharyngeal pouches.
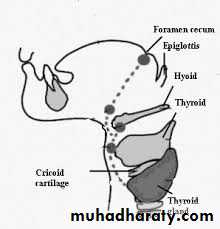
When it reaches the position it occupy in adult (just below the cricoid cartilage ) it divides into 2 lobes.
The site from which it originate persist as the foramen cecum at the base of the tongue.
3Embryology
Thyroid development
4
The path the gland follows may result in thyroglossal remnants:
• Ectopic thyroid tissue at the foramen cecum (lingual thyroid).• Ectopic midline thyroid tissue (supra & infrahyoid).
• Mediastinal thyroid.• Thyroglossal duct cysts and sinuses.
• Pyramidal lobe.• Agenesis of one thyroid lobes.
Tuesday, November 04, 2014
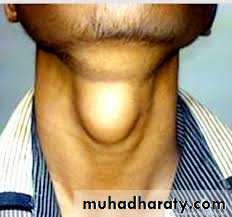
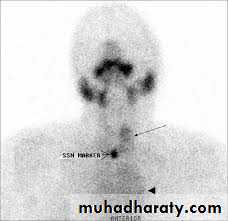
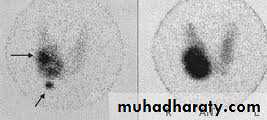
5Lingual thyroid
Thyroid scanTuesday, November 04, 2014
6Hyoid bone
Infrahyoid Thyroglossal Cyst
Suprahyoid Thyroglossal cyst
Hyoid bone
Tuesday, November 04, 2014
7
Mediastinal thyroid gland
Tuesday, November 04, 2014
8Pyramidal lobe
Tuesday, November 04, 2014
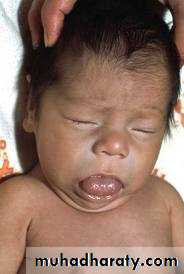
9AThyriosis
Cretinism
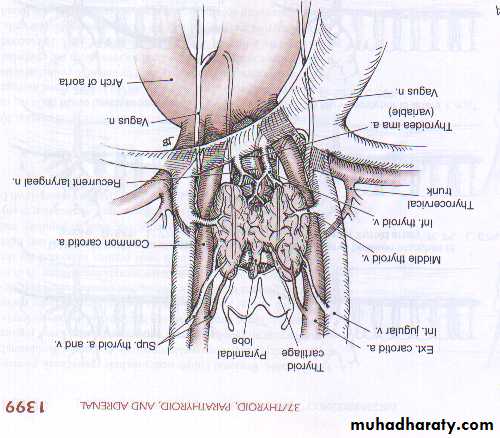
The normal thyroid gland weight ranges from(15-25 gms).
It is attached to the trachea by loose connective tissues.It is highly vascular organ that derives its blood supply from :
• Superior thyroid artery (external carotid artery).• Inferior thyroid artery (thyro-cervical trunk).
• Thyroidae ima artery (aorta).
Tuesday, November 04, 2014
10
Anatomy
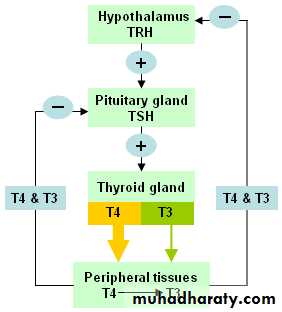
physiology
Secretion ®ulation of
thyroid hormones
stress
Tuesday, November 04, 2014
12The main function of thyroxin is to
• synthesize.• Store.
• Secrete thyroxin.
• The daily requirement of thyroxin is 0.1 mg/day.
Thyroid hormone function
Tuesday, November 04, 2014
13
• Free T4 enter the cell membrane by diffusion or by specific carrier.
• T4 is de-iodinated into T3 and enter the nucleus of the cell via active transport where it bind thyroid hormone receptor similar to nuclear receptors of corticosteroids, mineralocorticoids, estrogen, Vit D , retinoic acid. (T3 is the only active thyroid hormone at the cellular level)
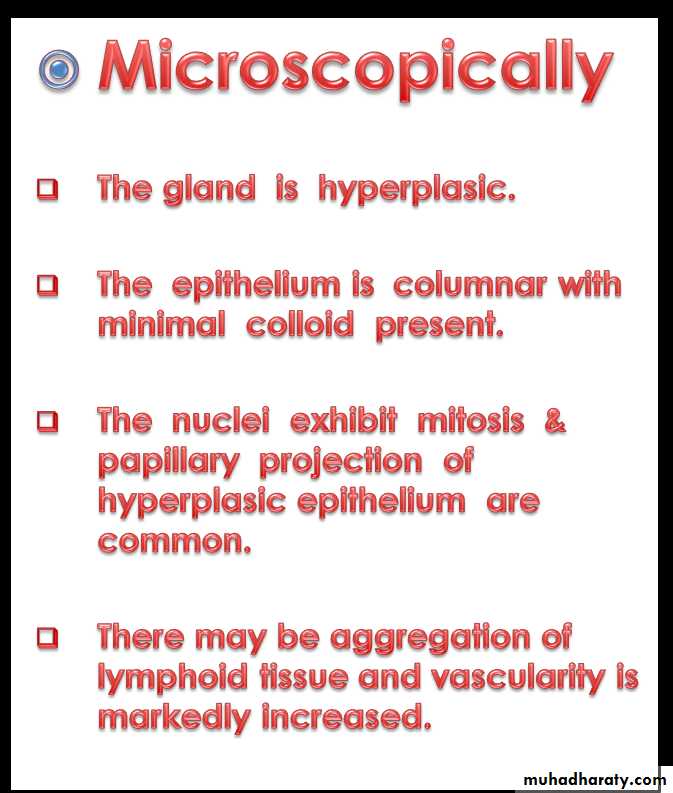
• Thyroid hormone affect every system in the body:
• Fetal brain development. ( Cretinism).
• Skeletal maturation. (Myopathies).
• T3 increase oxygen consumption, BMR, heat production by stimulation of Na+ -K+ ATPase in various tissues. ( intolerance to heat ,weight loss ,good appetite , warm ,moist hands).
• It has (+ ve ) inotropic & Chronotropic effect on the heart. (Tachycardia, palpitation).
Tuesday, November 04, 2014
14cont
• It is responsible for maintaining the normal hypoxic & hypercapnic drive in the respiratory centers of the brain.
( increase respiratory rate and depth of respiration).
• They also increase the gastrointestinal motility leading to
( diarrhea in hyperthyroidism & constipation in hypothyroidism).• It increase the bone & protein turn over & speed of muscle contraction & relaxation. ( bone resorption and decrease in bone calcium density , muscle wasting).
• It increase glycogenolysis, hepatic gluconeogenesis, intestinal glucose absorption, cholesterol synthesis & degradation.
( increased blood sugar, decrease of cholesterol in hyperthyroidism, increase of cholesterol in hypothyroidism).
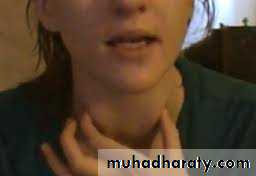
Evaluation of patients with goiter
historyClinical examination
investigations
Goiter
is defined as enlargement of thyroid gland
Size
SiteSurface
Consistency
Mobility
Exam for tracheal displacement
Presence of cervical lymphadenopathy
Tuesday, November 04, 2014
16
Clinical features
Systematic examination should be done
history
It should interpreted in the light of clinical situation.
One test alone is insufficient.
T3,T4,TSH. --is usually done by ------RIA.
Tuesday, November 04, 2014
17
Thyroid Function Tests
Tuesday, November 04, 2014
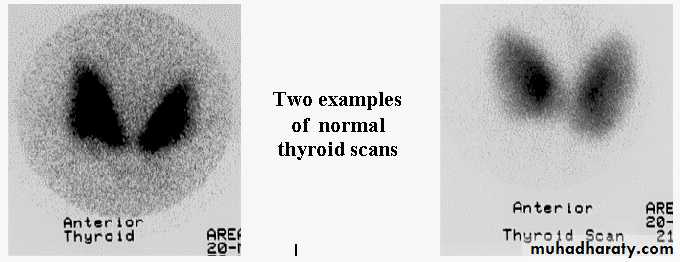
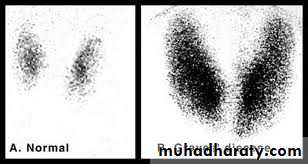
18Normal
Thyroid scan
Tuesday, November 04, 2014
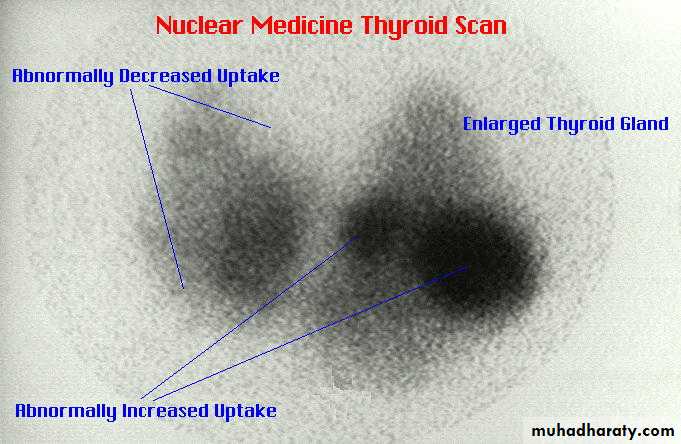
19Multinodular toxic
goiter
Autonomous thyroid
noduleGraves disease
Tuesday, November 04, 201420
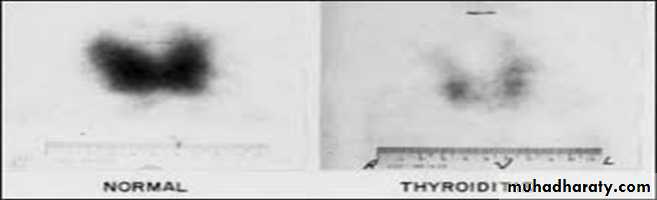
Nodular
non toxicgoiter
Thyroiditis
Tuesday, November 04, 2014
21Thyroid function state
(TSH
(0.3-3.3mui/lFree T4
(10-30 nmol/l)Free T3
(3.5-7.5Umol/l)Euthyroid
normalnormal
normalThyrotoxic
undetectable
high
highMyxedema
highlow
low
Suppressive T4 therapy
undetectablehigh
High or normalT3 toxicity
Low or undetectable
normal
High
Tuesday, November 04, 2014
22FNAC of thyroid gland.
Tuesday, November 04, 2014
23Histopathological examination of Excisional biopsy specimen.
Tuesday, November 04, 2014
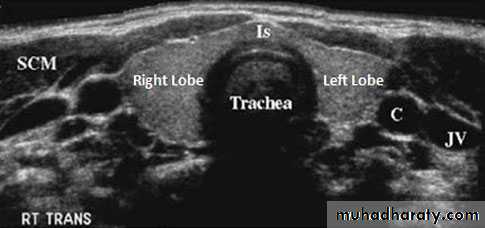
24Us of thyroid gland and neck
Tuesday, November 04, 2014
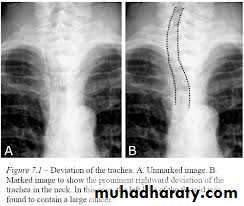
25X-ray of soft tissue of the neck
• Calcification.
• Trachéal displacement.
• Retro sternal extension.
Tuesday, November 04, 2014
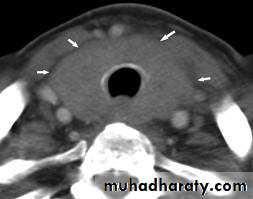
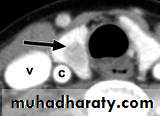
26CT scan of the neck
Nodule
Diffuse enlargementTuesday, November 04, 2014
27Tuesday, November 04, 2014
28
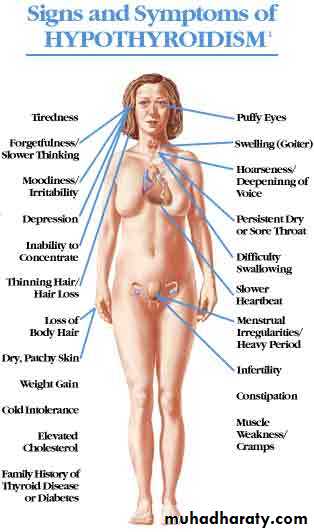
Hypothyroidism
Diseases of thyroid gland
Tuesday, November 04, 2014
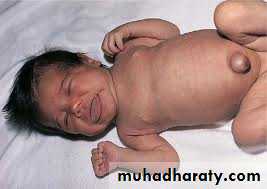
29Cretinism
• Macroglossia• Prone belly
• Umbilical hernia
• Mental retardation
• Short stature
Tuesday, November 04, 2014
30
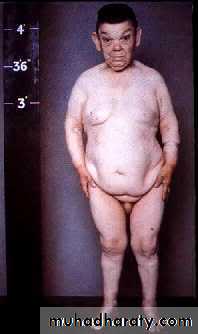
hypothyroidism
Tuesday, November 04, 201431
Hypothyroidism
Tuesday, November 04, 2014
32• The signs and symptoms of hypothyroidism are accentuated.
• The facial appearance is typical.
• there is often supraclavicular puffiness.
• A malar flush and a yellow tinge to the skin.
Myxedema
• Characterized by altered mental state,
hypothermia and a precipitating medical condition,e.g. cardiac failure or infection,
carries a high mortality rate.
• Treatment comprises thyroid replacement, either a bolus of 500 mg of T4 or 10 μg of T3 either intravenously or orally every 4–6 hours. If the body temperature is less than 30∞C the patient must be warmed slowly.
• Intravenous broad-spectrum antibiotics and hydrocortisone (in divided doses) are recommended.
• Primary or atrophic myxedema is considered to be an autoimmune disease
similar to chronic lymphocytic (Hashimoto’s) thyroiditis without goiter
formation.
• Delay in diagnosis is common and the degree of hypothyroidism is usually more severe than in goitrous autoimmune thyroiditis
Myxedema coma
Tuesday, November 04, 201433
Tuesday, November 04, 2014
34
• These show low T4 and T3 levels with a high TSH (except in the rare event of pituitary failure).
• High serum levels of TPO ( thyroid peroxidase ) antibodies are characteristic of autoimmune disease.
Laboratory investigations
• Oral thyroxine (0.10–0.20 mg) as a single daily dose is curative.
• Caution is required in the elderly or those with cardiac disease; in
such cases the replacement dose is commenced at 0.05 mg daily
and increased cautiously.
• If a rapid response is required, triiodothyronine (20 μg t.d.s.) may be used.
Treatment
Tuesday, November 04, 2014
35Tuesday, November 04, 2014
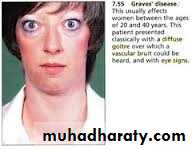
36Graves disease
Exophthalmic
goiterTuesday, November 04, 2014
37Graves disease
Multinodular toxic goiter(Plummer`s disease)Tuesday, November 04, 2014
38
Single toxic thyroid nodule
Tuesday, November 04, 201439
Rare causes
Tuesday, November 04, 201440
• Molar pregnancy
• TSH secreting tumor of pituitary.
• Struma ovarii.
• Thyrotoxicosis factitia.
• Jod-basedow thyrotoxicosis
Tuesday, November 04, 2014
41
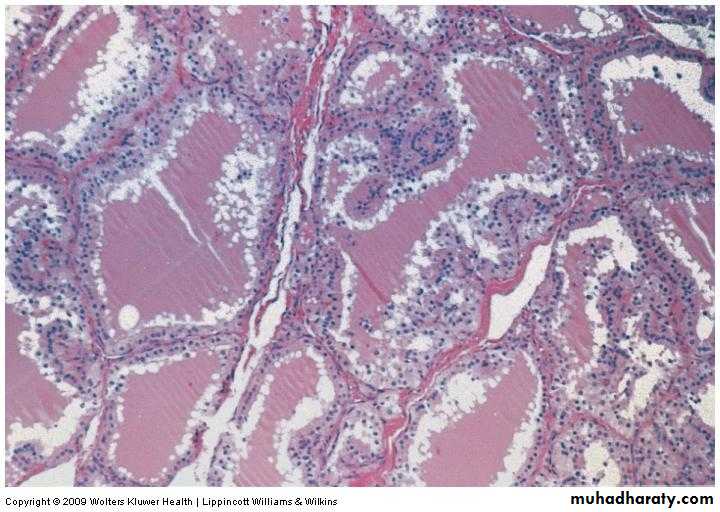
Macroscopically
The gland is diffusely enlarged .smooth .
increase in vascularity.Tuesday, November 04, 2014
42Pathology
Tuesday, November 04, 201443
Essentials for diagnosis
Tuesday, November 04, 201444
Clinical features
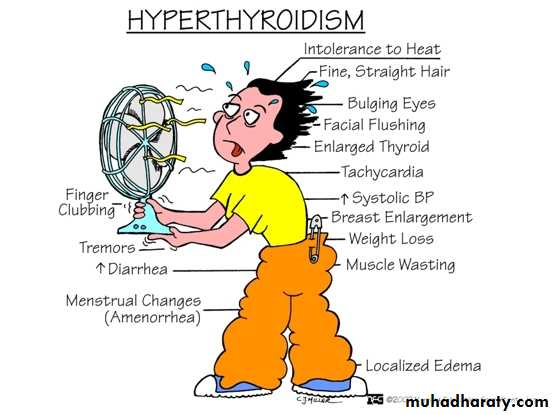
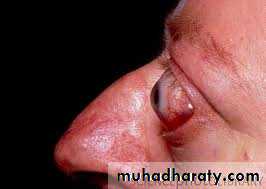
Staring eyes ( Lid retraction)Lid lag
Exophthalmos
Congestion of conjunctiva.
Chemosis.
Corneal ulceration.
Leucoma.
Tuesday, November 04, 2014
45Eye signs of graves disease
Laboratory investigations
Hyperthyroidism is diagnosed by suppressed TSH with orwithout increase T3 ,T4.
If Eye signs are present other tests are not needed.
If Eye signs are absent , I 123 uptake and scan should be performedElevated up take with diffusely enlarged gland confirm the diagnosis of
graves disease & help to differentiate it from other causes of hyperthyroidism.
If free T4 level is normal free T3 levels should be estimated as often free T3 levels
are elevated at the early graves or Plummer's disease ( T3 Thyrotoxicosis).
Antithyroid globulins (Anti Tg ) & Anti TPO antibodies are elevated in up to 75% of cases ( not specific).
Elevated thyroid stimulating hormone receptors ( TSH-R( or TS-Ab are diagnostic for graves disease & increased in 90% of cases.
MRI scans of the orbits are useful in evaluating graves ophthalmopathy.
Tuesday, November 04, 201446
In difficult cases T3 suppression test & TRH stimulation test are used:
T3 suppression test:Hyperthyroid patient fail to suppress the radioactive iodine uptake by thyroid gland when given exogenous T3.
TRH stimulation test:
Serum level of TSH fail to rise in response to TRH administration in hyperthyroid patient.Other findings :
Low cholesterol level.Lymphocytosis.
Hypercalcemia.
Hypercalciuria
Glucosuria.
Tuesday, November 04, 2014
47
Differential diagnosis
Anxiety state.Heart disease.
Anemia.
GI diseases.
Cirrhosis.
Tuberculosis.
Myasthenia gravis.
Muscular diseases.
Menopausal syndromes.
Primary ophthalmopathy.
Factious thyrotoxicosis.
Tuesday, November 04, 2014
48Treatment
It can effectively treated by :Antithyroid drugs.
Radioactive iodine.
Thyroidectomy.Tuesday, November 04, 2014
49Treatment should be individualized & depends on the patient:
• Age.2. General status of health.
3. Size of goiter.4. Underlying pathological process.
5. Patient ability to obtain follow-up.
Tuesday, November 04, 2014
50
Antithyroid drugs
The principle antithyroid drug used is carbimazole( 5mg tablet) (dose ranges from 10-30 mg/day).
It act by :
• Interfere with organic binding of iodine.
• prevent coupling of iodotyrosines in the thyroid gland.
• Its advantage over Thyroidectomy & radioactive iodine is that it inhibit the function of the gland without destroying tissues, so there is lower incidence of hypothyroidism subsequently.
• When it is given as definitive treatment ,the aim is to maintain the patient in a Euthyroid state until natural spontaneous remission occur ( some advocate that induce spontaneous remission).
• Reliable patients with small goiters are good candidate for such treatment.
• Prolong remission after 18 month treatment occurs in 30% , about 50% of them eventually became hypothyroid.
• Side effect: include Rash, agranulocytosis (0.1-0.4%) , fever (3-4%) , patient should be warned to stop the drug & see physician if sore throat or fever develop.
Tuesday, November 04, 2014
51
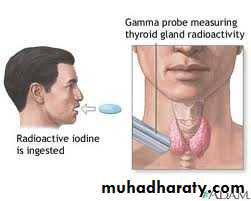
Radioactive Iodine
It may be given safely after the patient become Euthyroid.It is indicated for patients who are:
Elderly.
Poor risk patients.
Patients with recurrent hyperthyroidism.
It is less expensive than operative treatment.& effective.To date it has not been associated with increased risk of leukemia ,thyroid cancer or induce congenital anomalies.
But it increase the incidence of benign thyroid tumors & in young patient it certainly increased the incidence of radiation hazards.
The chances of development of hypothyroidism may reach up to 100% , as the risk increases by ( 2-3%) / year after the first year of treatment
it is contraindicated in hyperthyroid children & pregnant women.
Tuesday, November 04, 201452
Surgery
Advantages
Rapid control of disease.
Lower incidence of Hypothyroidism that can follow radioactive iodine therapy.Tuesday, November 04, 2014
53Preparation of patients to surgery
The risk in patients with toxic goiter become negligible since the introduction of :• Iodides
• Anti thyroid drugs.
• Beta blockers.
• These drugs one of them or in combination can be given to prepare thyrotoxic patients for surgery.
• Iodide alone.
• Iodide+ beta blockers.
• Iodides +beta blockers + antithyroid drugs.
• Beta blockers + antithyroid drugs.
Tuesday, November 04, 2014
54
Indications
Large diffuse toxic goiter.Thyroid nodule that may be malignant.
Treatment of pregnant patients & children.For treatment of older patients who wish to be pregnant within a year of treatment.
Treatment of psychologically & mentally incompetent patients.Patients that can not maintain adequate long term follow-up evaluation.
Tuesday, November 04, 201455
Antithyroid drugs
Neomercazole :is the representative drug which is most commonly used .
It is available as ( 5 mg tablet) & is given in a dose of 10 mg thrice daily orally then the dose is reduced to the minimum dose that can maintain Euthyroid state..
Clinical improvement can be noticed after 2 weeks from the time of onset of treatment.
Biochemical improvement can be achieved in 6-8 weeks.
( Euthyroid state).
Logol`s Iodine or potassium iodide solution:
It can be given as solution in a dose of (2-5 drops twice daily) for 10 days .It can result in block of the uptake of iodine in to the thyroid gland . After 14 days it can result in release phenomenon with increase in the secretion of thyroid gland.
It can be used with Neomercazole as it decrease vascularity of the gland it can facilitate thyroid removal.
Tuesday, November 04, 2014
56Tuesday, November 04, 2014
57In urgent thyroid surgery
Untreated patients or inadequately treated patients may require either thyroid surgery for an urgent cause or need another operation as appendicectomy or patients with perforated Duodenal ulcer such patients require immediate control of hyperthyroid state.
Such patients should be treated in a manner similar to patients who suffer from thyrotoxic crisis ( thyroid storm) as such storm can be precipitated by surgical stress or trauma.
Treatment of patients who require emergency operation or in thyroid storm includes:
Prevent the release of preformed thyroid hormone by administration of Logol`s iodine solution.2. Administration of beta blockers ( e.g. Propranolol) as it result in:
Antagonize the peripheral manifestation of thyroid hormone production.Decrease the extra thyroid conversion of T4 to T3 in the peripheral tissues.
Both treatments had been proved to decrease serum level of thyroid hormone s.Treat the precipitating cause.
Tuesday, November 04, 201458
Surgical procedure
Subtotal Thyroidectomy
It eliminates both hyperthyroidism & goiter.
The aim of the procedure is remove the thyroid tissue & leaving only between(3-10 gms of tissue) + parathyroid glands & recurrent laryngeal nerves intact.
The mortality is less than 1%.
It provides a quick and soft correction of thyrotoxic state in most of the cases.The frequency of hyper & hypothyroidism depends on
The amount of tissue removed .B. Natural history of hyperthyroidism.
The incidence of recurrent laryngeal nerve palsy is < 2 % if the patient is prepared preoperatively.Adequate exposure & precise identification of vasculature, recurrent laryngeal nerve & parathyroid glands are essential.
Tuesday, November 04, 2014
59
Total or Near Total Thyroidectomy(Total lobectomy on one side+ subtotal thyroidectomy on the other side)
Patients with coexistent thyroid cancer.
Those who refuse radioactive iodine.Patients with severe ophthalmopathy.
Patients who have life –threatening reaction to antithyroid medications. ( vasculitis , agranulocytosis , liver failure ).In near total Thyroidectomy you should leave 1-2 gms of thyroid tissue.
Tuesday, November 04, 201460
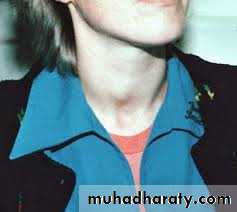
Toxic nodular goiter (Plummer`s Disease)
It usually affect people after the age of 50 year who were involved by multinodular non-toxic goiter.Following several years enough thyroid nodules will become autonomous to cause hyperthyroidism .
The presentation is usually insidious in that hyperthyroidism may be only obvious when the patient s are placed on low doses of thyroxin suppression dose for the goiter.
Some patients had T3 thyrotoxicosis , where as the others have apathetic hyperthyroidism , atrial fibrillation or congestive heart failure.
Thyrotoxicosis can also be precipitated by iodine containing drugs such as contrast media or anti arrhythmic drugs amiodarone ( jodbasedow phenomenon).
Symptoms and signs of hyperthyroidism but less severe than graves disease & extra thyroidal manifestations may be absent.
Similar to graves disease with suppressed TSH level & elevated T4 & T3 levels.
RAI uptake is also increased show multiple nodules with increased uptake and suppression of the normal gland.Tuesday, November 04, 2014
61Diagnostic tests
Treatment
hyperthyroidism must be adequately controlled as in graves disease.
Subtotal Thyroidectomy is the treatment of choice .
Remnant of thyroid tissue is not as crucial a concern because such patients needs thyroid hormone suppression to prevent recurrence of the goiter.Identification of recurrent laryngeal nerve should be done which may be found laterally on the thyroid ( rather than posterior) or stretched anteriorly over the nodule.
Total Thyroidectomy may be done if no normal thyroid tissue was found posteriorly.
Tuesday, November 04, 201462
Radioactive iodine (RAI)
Larger doses should be used to control hyperthyroidism as the radioactive iodine uptake is less than that in graves disease.
Radioactive iodine induced thyroiditis can cause swelling and acute airway compression and leaves the goiter intact with the possibility of recurrent hyperthyroidism.
It occurs in younger age group.
It is noticed by the patient as recent growth of long standing nodule along with symptoms of hyperthyroidism.
Most of the cases are characterized by somatic mutations in the TSH receptor gene.
Most of the hyperfunctioning or autonomous adenomas have attained the size of 3 cm before the thyrotoxic symptom would appear.On physical examination: reveals solitary thyroid nodule with out palpable thyroid tissue on the contra lateral side.
Radioactive iodine scan (RAI scan ) shows Hot nodule with suppression of the rest of the gland.
They are rarely malignant.
Smaller nodules can be treated by antithyroid medications & RAI. But rarely cause hyperthyroidism.Surgery ( Lobectomy & isthmectomy) is recommended to treat young patients & those with large nodules.
Tuesday, November 04, 2014
( Toxic adenoma)Thyroid tumors objectives
To know different types their behavior.Use the appropriate investigations.
Note the risk and possible effect on treatment.
Understanding the role of post operative radiotherapy.Tuesday, November 04, 2014
64
History of irradiation to the neck in some patients.
Painless or enlarged nodule, dysphagia, hoarseness of voice.Firm ,hard ,fixed thyroid nodule, cervical lymphadenopathy.
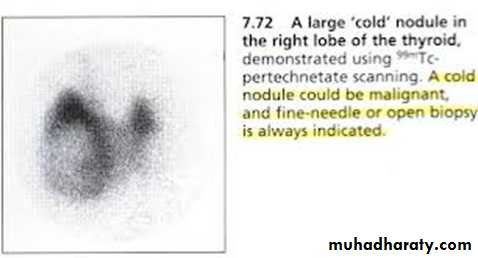
Normal thyroid function, nodule is stippled with calcium (x-ray)Cold thyroid nodule (radioactive iodine . scan, solid (ultrasound), positive or suspicious cytology),
Tuesday, November 04, 2014
65
Essentials for diagnosis
Thyroid tumors
Classification of malignant thyroid tumors is important as it has a wide range of behavior.
In the extreme papillary carcinoma usually occur in young adult ,slowly growing, metastasize late through lymphatic & is compatible with long life even in the presence of metastasis.
On the extreme is the undifferentiated carcinoma which occurs late in life, none capsulated, invasive, forming large infiltrating tumor composed of small and large Anaplastic cells, with poor prognosis, patient usually die as a consequence of local recurrence, pulmonary metastasis or both.
Between the 2 extremes lie the follicular & medullary carcinoma , sarcomas, lymphomas & metastatic tumors.
The prognosis depends on the age , sex , the extent of tumor spread at the time of diagnosis.
Tuesday, November 04, 2014
66
Classification
The causes of most cases of thyroid cancer is unknown.
History of therapeutic radiation at a dose of (6.5-2000 rads) to the thymus, tonsils or skin at infancy have increase the risk of developing thyroid tumors.Children & adults up to the age of 50 years who are exposed to radiation at Hiroshima have increased risk of benign and malignant thyroid tumors with a latency period of 30 years.
Tuesday, November 04, 2014
67
causes
Papillary adenocarcinom.
Follicular adenocarcinom.Medullary carcinoma.
Undifferentiated carcinoma.Types of malignant thyroid tumors
# It accounts for 85% of thyroid carcinomas.# usually affects early adult life. # It presents as solitary thyroid nodule. # It can spread via intra-glandular lymphatics within the gland even to the contra lateral lobe , then to the sub capsular & pericapsular lymph nodes.# 80% of children &20% of adults presents with palpable lymph nodes.# The tumor might metastasize to the lung & bone.# Microscopically it is composed of papillary projections of columnar epithelium , psammoma bodies are present in 60% of cases.# Papillary follicular or follicular variant of papillary carcinoma is sometimes present.# The rate of growth is stimulated by thyroid stimulating hormone ( TSH).
Tuesday, November 04, 2014
69
Papillary adenocarcinom
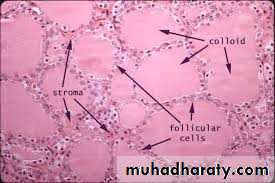
It accounts about 10% of malignant thyroid tumors.
It appears later in life than papillary carcinoma (3rd decade of life).
Present with elastic or rubbery or even soft thyroid nodule.
It appears to be encapsulated and contain colloid material on gross examination.Microscopically :it might be difficult to differentiated from the normal thyroid tissue.
Capsular & vascular invasion can distinguish follicular carcinoma from follicular adenoma.It has great tendency to spread by blood stream( hematogenous spread) to the lung ,bones & liver & less commonly to the regional lymph nodes.
Metastasis from this tumor demonstrate avidity for radioactive iodine after Thyroidectomy.
Skeletal metastasis can appear ( 10-20 ) years after resection of the primary lesion & may follow relatively benign course.The prognosis is not as good as papillary carcinoma.
Tuesday, November 04, 201470
Follicular adenocarcinoma
> It account for approximately (2-5%) of malignant tumors of the thyroid.> It presents usually with solid, nodular tumor and contain amyloid material.> it takes radioactive iodine poorly.> It arises from the ultimobranchial bodies.> It secrete calcitonin hormone ( lower serum calcium level).> It can occurs alone or part of multiple endocrine adenomas which tend to have familial tendency. ( Sipple`s syndrome or Type II MEA).In Sipple's syndrome: Hyperplasia of Para follicular cells precancerous condition,> Small Medullary carcinoma might be diagnosed by determining serum calcitonin level by basal or after calcium or pentagastrin stimulation.
Tuesday, November 04, 2014
71
Medullary carcinoma
Undifferentiated (anaplastic) carcinoma
This rapidly growing tumor.It affect mainly females beyond middle age.
It accounts for 3% of all cancer.It can evolve from papillary or follicular carcinoma.
It is solid, quickly enlarging ,hard, irregular mass diffusely ,f gland& invading the trachea, muscles & neurovascular structures early.The tumor may be painful & tender fixed on swallowing & may cause laryngeal or esophageal obstructive symptoms.
Tuesday, November 04, 2014
72
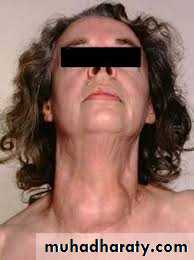
Goiter
Most goiters result from:
Iodine deficiency and /or TSH stimulation secondary to inadequate thyroid hormone synthesis and other paracrine growth factors.
Goiter may be diffuse ,uninodular, Multinodular.
Familial goiter results from inherited deficiency in enzyme necessary for thyroid hormone synthesis.Goiter could be classified into :
• Endemic goiter referre to the occurrence of goiter in a significant proportion of individuals in particular geographic region.In the past dietary iodine deficiency was the most common cause of endemic goiter. The condition had largely disappeared from north America due to routine use of iodized salt and iodination fertilizers, animal feed and preservatives.
Other dietary giotrogens can be incriminated as a cause of goiter like cabbage and cassava, cauliflower.
Tuesday, November 04, 2014
732. Sporadic goiter:
a. it occurs in small No. of population at certain locality.b. It is usually referred to cases of goiter where no cause could be attributed to such goiter but in some cases it may be familial.
It can also classified into :
• Simple goiter – diffuse Hyperplastic , physiological .pubertal , pregnancy, Multinodular goiter.
• Toxic: diffuse (gravis disease), Multinodular, toxic adenoma.
• Neoplastic: benign, malignant.• Inflammatory: Autoimmune (chronic lymphocytic thyroiditis or Hashimotos thyroiditis, Granulomatous (De Quervain`s thyroiditis ). Fibrosing (Riedel`s thyroiditis), Infective : acute (bacterial thyroiditis ,viral thyroiditis , sub acute thyroiditis .
• others ( Amyloid).
Tuesday, November 04, 2014
74Tuesday, November 04, 2014
75Clinical features:
• Asymptomatic (most patients with non toxic goiter).
• If goiter become very large compressive symptoms dyspnea, dysphagia.• Dysphonia from recurrent laryngeal nerve palsy is rare except when malignancy is present.
• Obstruction of venous return at the thoracic inlet from retrosternal goiter with a positive Pemberton sign ( facial flushing and dilatation of cervical veins on raising the arm above the head).
• Sudden enlargement of nodules because of hemorrhage or cyst may causes acute pain.
On physical examination:• Gland is soft, diffusely enlarged (simple) .
• Nodules of various size and consistency in cases of Multinodular goiter.• Tracheal deviation with or without compression is common.
Diagnostic tests
Patients are usually Euthyroid with normal TSH with normal or low-normal free T4 levels.If some nodules develop autonomy ,patients have suppressed TSH levels or become hyperthyroid.
FNA cytology is recommended in Euthyroid patient who have a dominant nodule or one that is painful or enlarged.
Treatment:
Most Euthyroid patients with small. diffuse goiter do not require treatment.Exogenous thyroid hormone (thyroxin) might be given to large goiter to reduce the TSH stimulation of gland growth this will result in decrease or stabilization of goiter size.
Endemic goiter is usually treated by iodine administration (controversial)
Surgical treatment is reserved for goiters:
a. Continue to increase in size in spite of T4 suppression.
b. Cause obstruction.
c. Retrosternal extension.
d. Suspected or proved to be malignant by FNA.
e. Cosmetically unacceptable.
Tuesday, November 04, 2014
76
Total lobectomy in the side of dominant nodule side and subtotal resection of the contralateral is the treatment of choice.
Patients need long life T4 therapy to prevent recurrence.
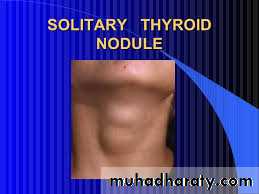
Single (solitary) thyroid noduleAre present in 4% of population.
It is utmost importance to determine which patients with solitary thyroid nodule would be benefit from surgery.History regarding the nodule:
onset, changes in the size ,associated symptoms such as pain, dysphagia ,dyspnea or chocking.
Pain is an unusual symptom and when present raise the suspicion of intrathyroid hemorrhage in a benign nodule, thyroiditis or malignancy.
History of hoarseness of voice may warrant the presence of malignancy with recurrent laryngeal nerve palsy.
Most importantly should be questioned regarding risk factor for malignancy such as exposure to ionizing radiation, family history of thyroid and other malignancies associated with thyroid cancer.
Tuesday, November 04, 2014
77• Physical examination:
• Move with swallowing .• Nodules are hard gritty fixed to the surrounding structures such as to the trachea strap muscles are more likely to be malignant.
• Ipsilateral and contralateral jugular &posterior triangle lymph nodes should be assessed.
• Diagnostic tests:
• FNAC: is the most important diagnostic test.
• The majority of nodules can be categorized into:
• a. Benign (65%).
• b. Suspecious(20%).
• c. Malignant (5%).
• d. Nondiagnostic (10%).
• False positive (1%).
• False negative (3%).
Tuesday, November 04, 2014
78
With benign lesions including cysts and adenomas the risk of malignancy in this setting is <3%.
The invidence of malignancy in the setting of suspecious cases ranges from(10-20%).most of the cases were follicular or hurthle cell neoplasm where only histopathological features of vascular invasion is diagnostic.
FNAC is less reliable in patients with history of head and neck irradiation or family hx of thyroid cancer because of likelhood of cancer and coexistent benign & malignant lesions.
Most of the patients are euthyroid ( normal TSH level).
If the nodule is hyperthyroid the incidence of malignancy is 1%.Tuesday, November 04, 2014
79
U/S is used to :
1.Diffrentiate cystic from solid masses.2.Detect nonpalpable lesions.
3. detection of micro calcifications and lymphadenopathy.
CT & MRI are unnecessary as a routine investigation for tumor except for large, fixed, substernal lesions.
I 123 & 99m TC scan is rarely necessary unless for evaluation of hot or autonomous thyroid nodule.
Tuesday, November 04, 2014
80Tuesday, November 04, 2014
81Euthyroid
Hyperthyroid
USS/FNAC
USS/FNAC
123 radioactive iodine scan
Cystic
• Malignant
• Suspicious
• inadequate
Benign
Surgery
<4 cm
• > 4 cm
• Blood stained
• Refill after aspiration
surgery
Review after 6/12 and discharged if no change
• Pressure symptoms
• Tracheal deviation
• Increasing size
surgery
asymptomatic
Repeat FNAC and discharge if no change after 6 months
Hot nodule > 3 cm
Hot nodule < 3 cm
Therapeutic iodine 131
Surgery
Management of single thyroid nodule
Thyroid function tests(T3,T4,TSH)
Thyroiditis
Tuesday, November 04, 2014
82
Chronic lymphocytic (Autoimmune) Thyroiditis (Hashimotos Thyroiditis)
Is a common condition that is associated with raised titer of antithyroid antibodies.(Positive) family history of such condition .
Commonly present as goiter (diffuse or nodular) with bosselated feeling.It might present with signs and symptoms of hyperthyroid , euothyroid or established thyroid failure(hypothyroidism).
Diagnosis can be made by investigating a patient with discrete thyroid swelling or focal .
Histopthological examination show chronic inflammatory cell infiltration .Clinical features: hyperthyroidism , Euothyroid and hypothyroidism , the gland is lobulated or diffuse, the gland may be small or large and the gland is rubbery or firm in consistency depends on the cellularity and fibrosis .
The disease is common in women at menopause but it may occur at any age.
Papillary Carcinoma and lymphoma are occasionally associated with autoimmune thyroiditis.
Tuesday, November 04, 2014
83Tuesday, November 04, 2014
84Diagnosis
• Biochemical tests (thyroid functions ) Hyperthyroid ,Euthyroid .or hypothyroid state . It is of diagnostic value only if hypothyroid state is present.
• Significant increase of one or more of thyroid antibodies are present in 85% of cases.
• Differential diagnosis of nodular goiter,lymphoma,carcinoma and malignant lymphoma is not always easy to differentiate.• Histopthological features of lymphocytic infiltration can lead to difficulty in differentiation between autoimmune thyroiditis and lymphoma when such difficulty is present diagnostic lobectomy may be necessary.
Tuesday, November 04, 2014
85Treatment
• Full replacement dosage of thyroxin should be given for : hypothyroidism ,if the goiter is large or symptomatic .
• Other minor manifestations such as small goiter with raised AB titer or histological evidences of thyroiditis do not justify thyroxin therapy.
• If the gland increase in size in spite of hormonal replacement with thyroxin steroids are indicated.
• Thyroidectomy may be necessary if the goiter is large and causes symptoms.
• Sudden increase in the size of goiter should be assessed urgently because of the possibility of development of malignant lymphoma.
Granulomatous thyroiditis , Subacute thyroiditis ((De Quervain`s thyroiditis
Is caused by viral infection.Typically it presents with pain in the neck , fever , malaise, firm irregular enlargement of one or both thyroid lobes.
ESR is high.
Absent Antithyroid antibodies.Raised serum T4 , normal or slightly higher than normal.
Radioactive iodine uptake is low.It is self limiting condition that subside within months.
Tuesday, November 04, 2014
86Tuesday, November 04, 2014
87• There may be a period of hypothyroidism before eventual recovery.
• In 10% of cases the onset is acute the goiter is very painful and tender with symptoms of hyperthyroidism.• In one 3rd of the cases are asymptomatic and presents with goiter only.
• If the diagnosis is in doubt FNAC ,radioactive iodine uptake and rapid symptomatic response to prednisolone is diagnostic.• In acute case with severe pain the specific treatment is prednisolone (10-20 mg) daily for 7 days the dose is gradually reduced over a period of a month.
• If thyroid failure is prominent thyroxine is given until the function is recovered.
Riedel`s thyroiditisIs a very rare condition (0.5% of goiters).
It is most probably a collagen disease.
Thyroid tissue is replaced by cellular fibrous tissue which infiltrate through the capsule into the adjacent structures including muscles, recurrent laryngeal nerve, parathyroid glands, and carotid sheath.
It is associated with retroperitoneal and medistinal fibrosis .
The goiter may be unilateral or bilateral, if feels hard and fixed .
It should be differentiated from anaplastic carcinoma of thyroid gland .
Diagnosis could be made by biopsy with resection of isthmus of the gland to free the trachea.
If the disease is unilateral the other lobe is involved later with subsequent hypothyroidism.
Treatment
is by high doses of steroids and thyroxine replacement.Reduction of the size of the gland and symptomatic improvement are to be expected if the treatment is started early.