
The skin & hair
follicle
by
Dr. Suhair Majeed
The skin
The skin covers the exterior of the body and
constitutes a large organ with several functions.
It protects the body from mechanical injury and
loss of fluid, acts as a barrier against noxious
agents, aids in temperature regulation, excretes
various waste products, and through its
receptors for sensations of heat, cold,touch, and
pain, provides information about the external
environment.
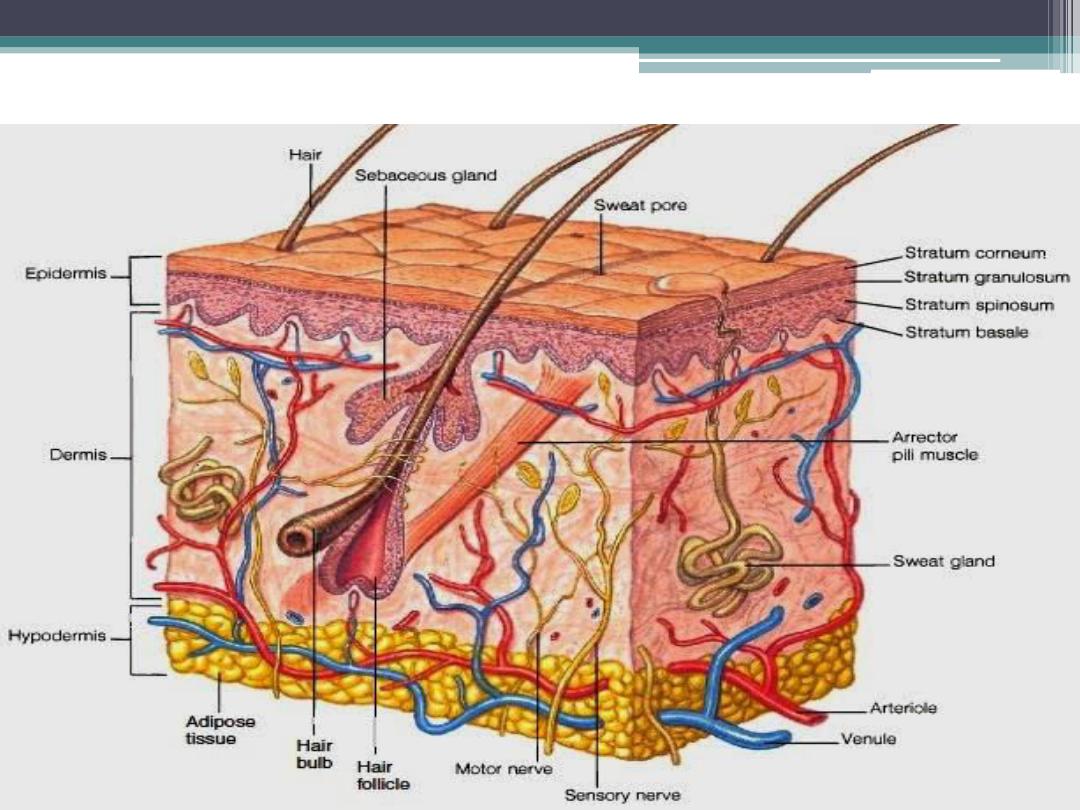
The skin
Cont.
In addition, the ultraviolet rays of sun light
stimulate the deep epidermis to produce
vitamin D (calciferol).
Skin and its derivatives and appendages form
the integumentary system. In humans, skin
derivatives include :
nails, hair, and several types of sweat and
sebaceous glands.
skin consists of two distinct regions :
- superficial epidermis
- deep dermis
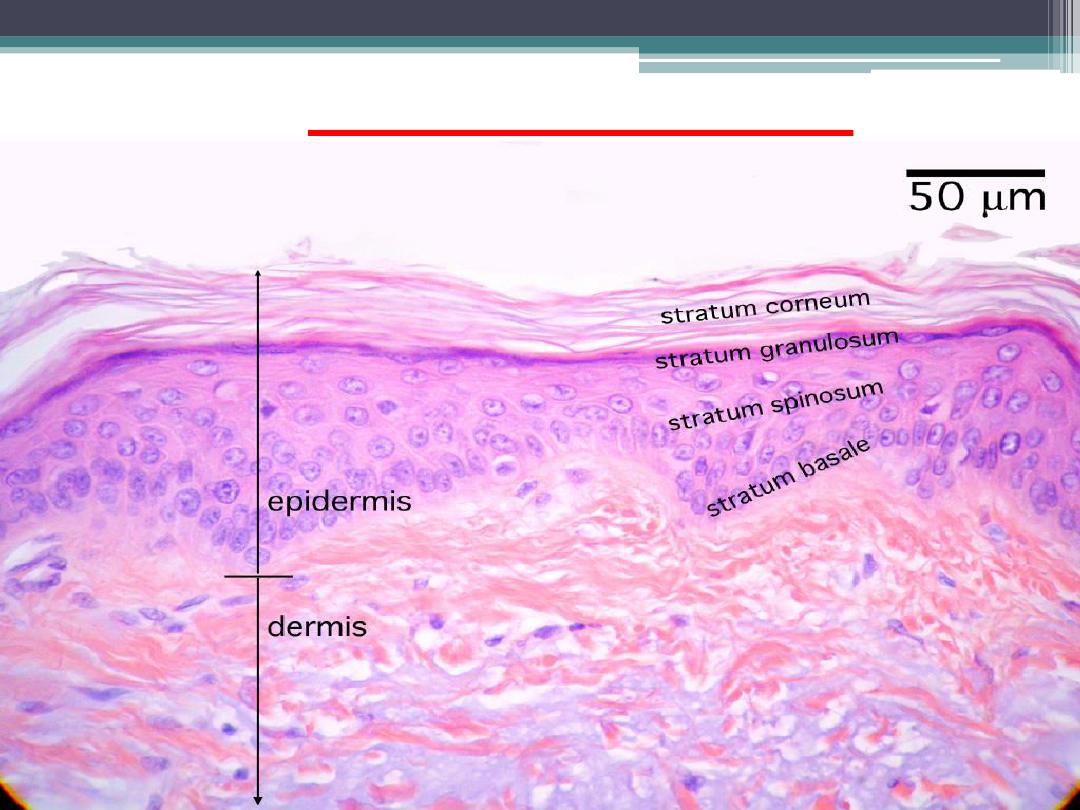
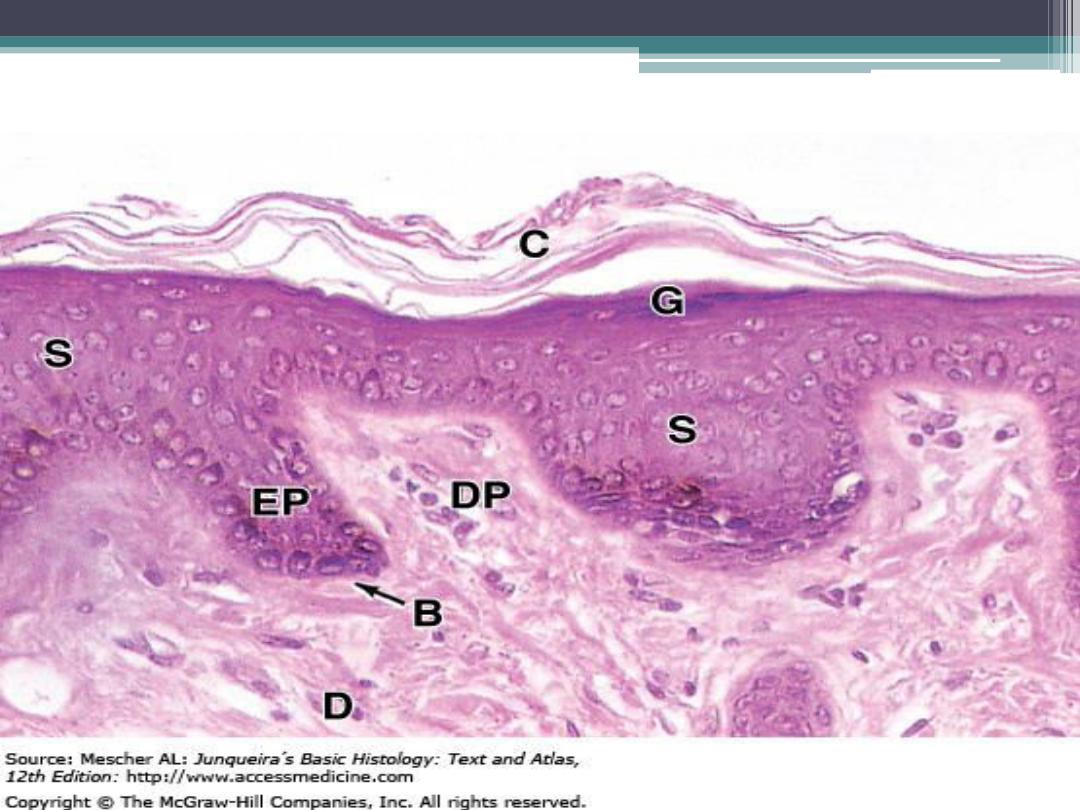
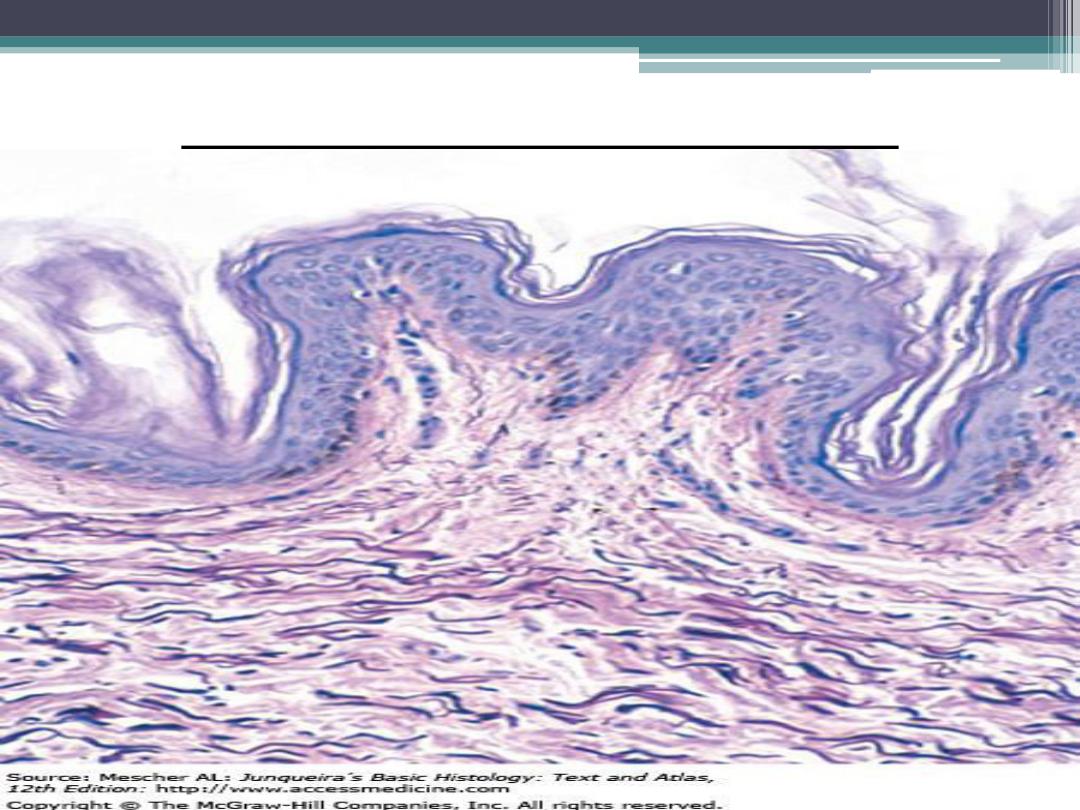
Epidermis & dermis
cont.
The superficial epidermis :
is nonvascular and lined by keratinized
stratified squamous epithelium with distinct
cell types and cell layers.
Inferior to the epidermis is the vascular
dermis,
characterized by dense irregular
connective tissue. Beneath the dermis is
hypodermis
or a subcutaneous layer of
connective tissue and adipose tissue that forms
the superficial fascia seen in gross anatomy.
Epidermis ,dermis &hypodermis
cont.
The basic histology of skin is similar in
different regions of the body, except in the
thickness of the epidermis , palms and soles
are constantly exposed to increased wear, tear,
and abrasion. As a result, the epidermis in
these regions is thick, especially the outermost
stratified keratinized layer.
cont.
The skin in these regions is called
thick
skin
. Thick skin also contains numerous sweat
glands, but lacks hair follicles ,sebaceous
glands, and smooth muscle fibers
.
The remainder of the body is covered by
thin
skin
. In these regions, the epidermis is
thinner and it’s cellular composition simpler
than that of thick skin.
Thin skin
Thick skin
cont.
Present in thin skin are :
- hair follicles
- sebaceous glands,
- sweat glands
The epidermis
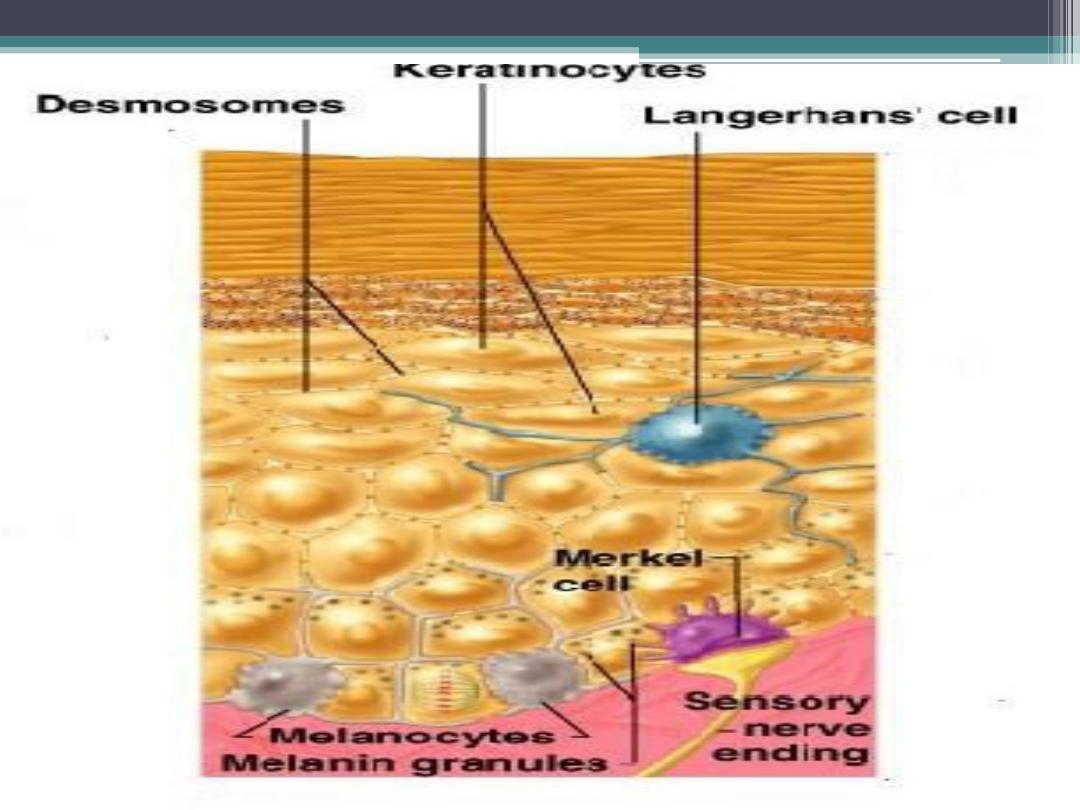
1-Epidermal Cells
There are four cell types in the epidermis of
skin,with the keratinocytes being the dominant
cells.
a- Keratinocytes
divide, grow, migrate up, and undergo
keratinization or cornification, and form the
protective epidermal layer for the skin. The
epidermis is composed of stratified keratinized
squamous epithelium .
Cont.
There are other less abundant cell types in
the epidermis. These are the
- melanocytes,
-Langerhans cells,
-
Merkel’s cells,which are located among
the keratinocytes in the epidermis .
B- Melanocytes
Melanocytes have long irregular
cytoplasmic extensions that branch into the
epidermis.
Melanocytes are located between the
stratum basale and stratum spinosum of the
epidermis and synthesize the dark brown
pigment ( melanin ).
Melanin is synthesized from the amino acid
tyrosine by the melanocytes.
cont.
The melanin granules in the melanocytes
migrate to their cytoplasmic extensions, from
which they are transferred to keratinocytes in
the basal cell layers of the epidermis .
Melanin imparts a dark color to the skin, and
exposure of the skin to sunlight promotes
increased synthesis of melanin.
The function of melanin is to protect the skin
from the damaging effects of ultraviolet
radiation .
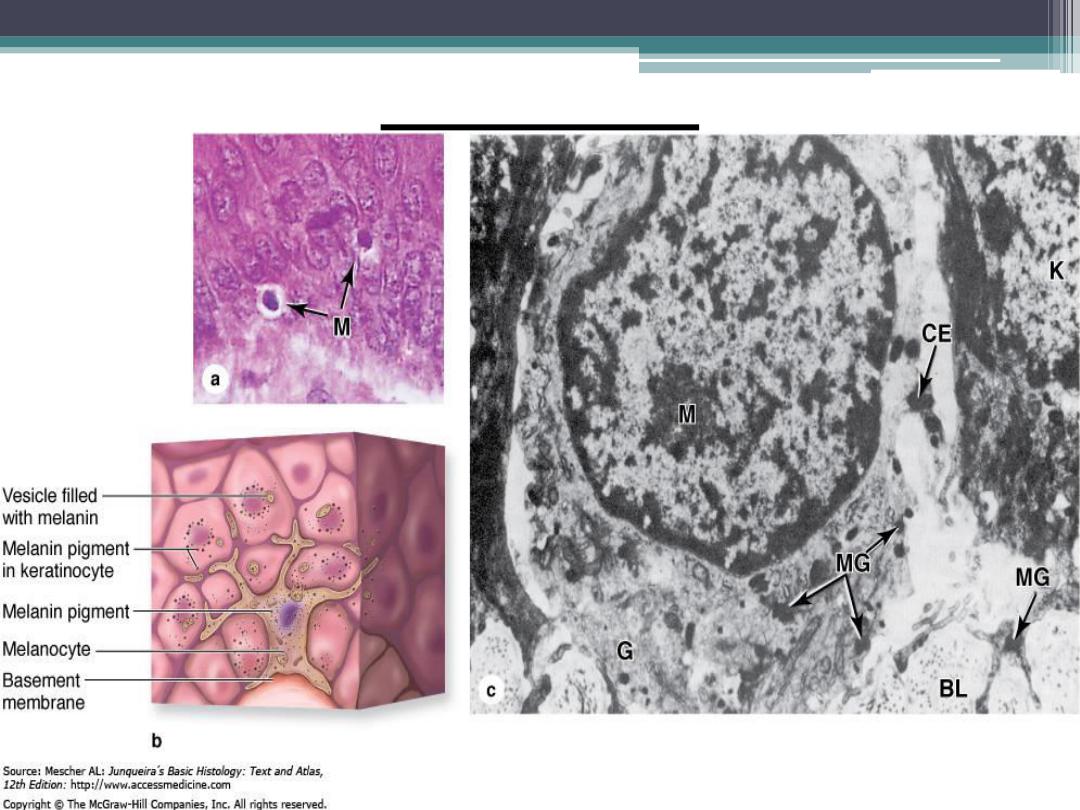
Melanocyte
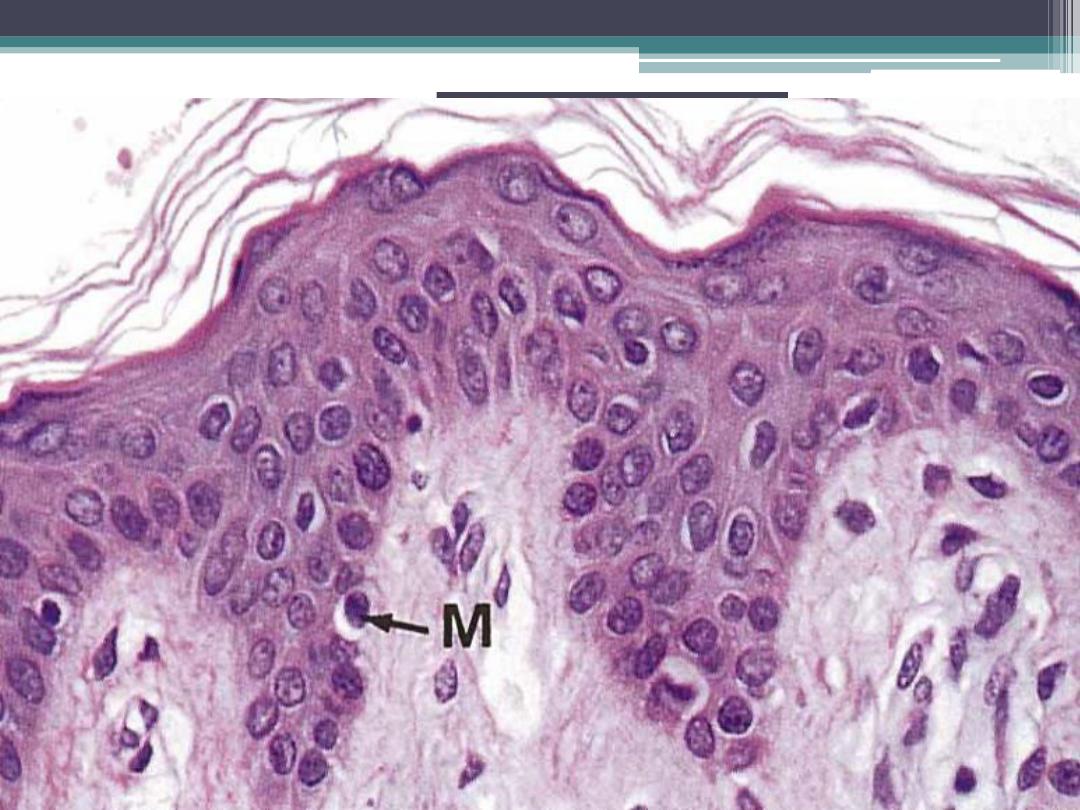
melanocytes
C- Langerhans cells
Langerhans cells are found mainly in the
stratum spinosum. They participate in the
body’s immune responses.
Langerhans cells recognize, phagocytose,
and process foreign antigens, and then present
them to T lymphocytes for an immune
response.
Thus, these cells function as antigen
presenting cells of the skin .
Langerhans cells
d-
Merkel’s cells
Merkel’s cells are found in the basal layer of
the epidermis and are most abundant in the
fingertips.
Because these cells are closely associated
with afferent (sensory) unmyelinated axons,
it is believed that they function as
mechanoreceptors to detect pressure.
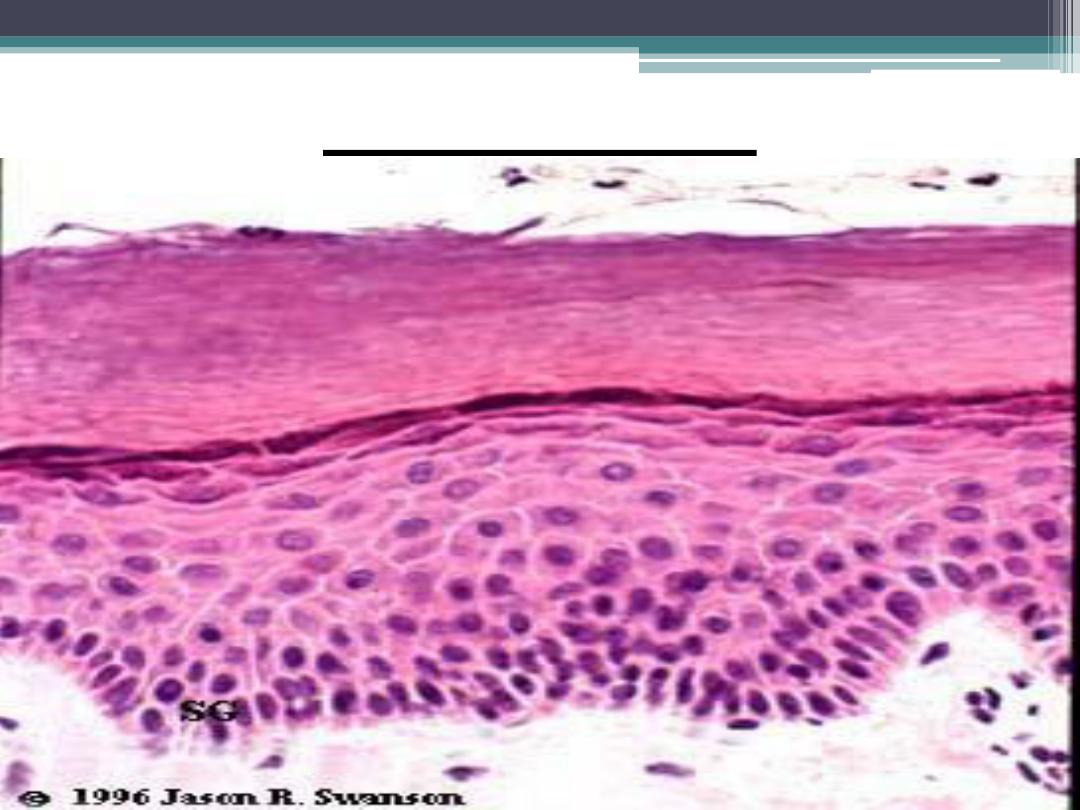
2-The Epidermal cell layers :
In thick skin, five distinct and recognizable
cell layers can be identified , while in thin skin
four cell layers can be identified .
1- stratum basale
2- stratum spinosum
3- stratum granulosum
4- stratum lucidum
5- stratum corneum
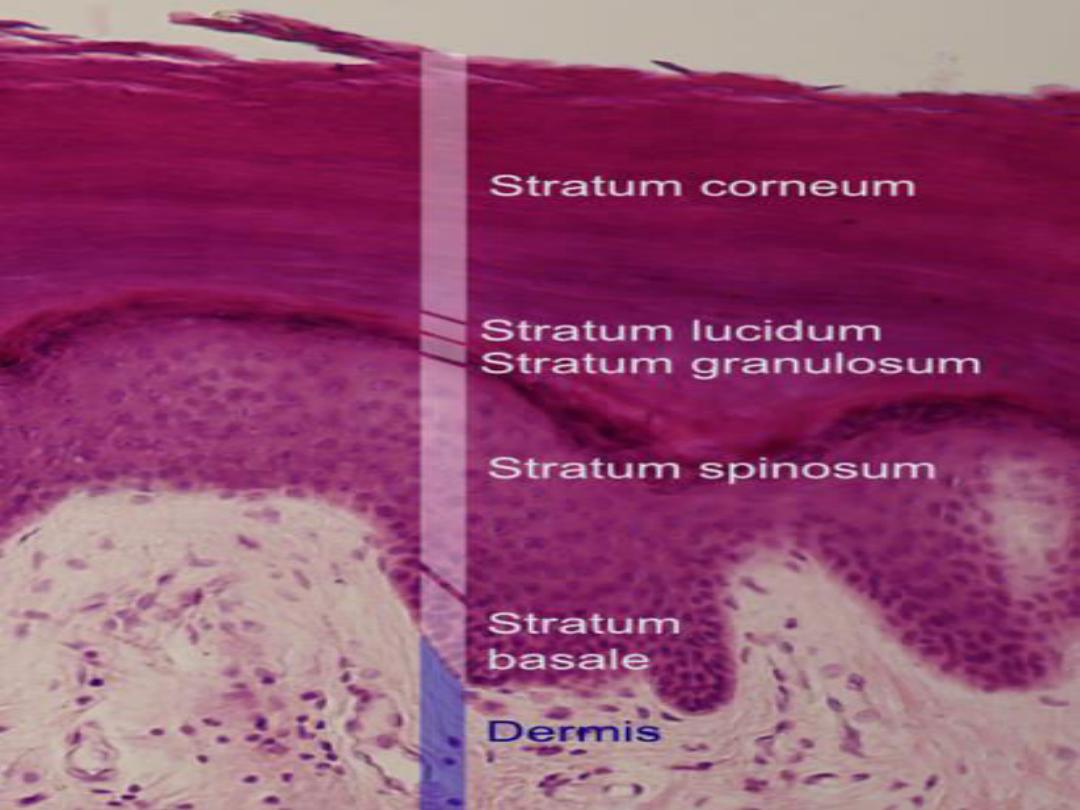
1- Stratum Basale (Germinativum)
The stratum basale is the deepest, or
basal layer, in the epidermis. It consists of a
single layer of columnar to cuboidal cells
that rest on a membrane separating the
dermis from the epidermis .
The cells are attached to one another by
cell junctions, called desmosomes, and to
the underlying basement membrane by
hemidesmosomes.
Stratum basale
(cont.)
Cells in stratum basale serve as stem cells for
the epidermis; thus, much increased mitotic
activity is seen in this layer.
The cells divide and mature as they migrate
up toward the superficial layers.
All cells in the stratum basale produce and
contain intermediate keratin filaments
that increase in number as the cells move
superficially.
2- Stratum Spinosum :
As the keratinocytes move upward in the
epidermis, a second cell layer, or stratum
spinosum, forms.
This layer consists of four to six rows of cells.
In routine histologic preparations, cells in this
layer shrink .
As a result, the developed intercellular
spaces between cells appear to form
numerous cytoplasmic extensions ,or spines
that project from their surfaces .
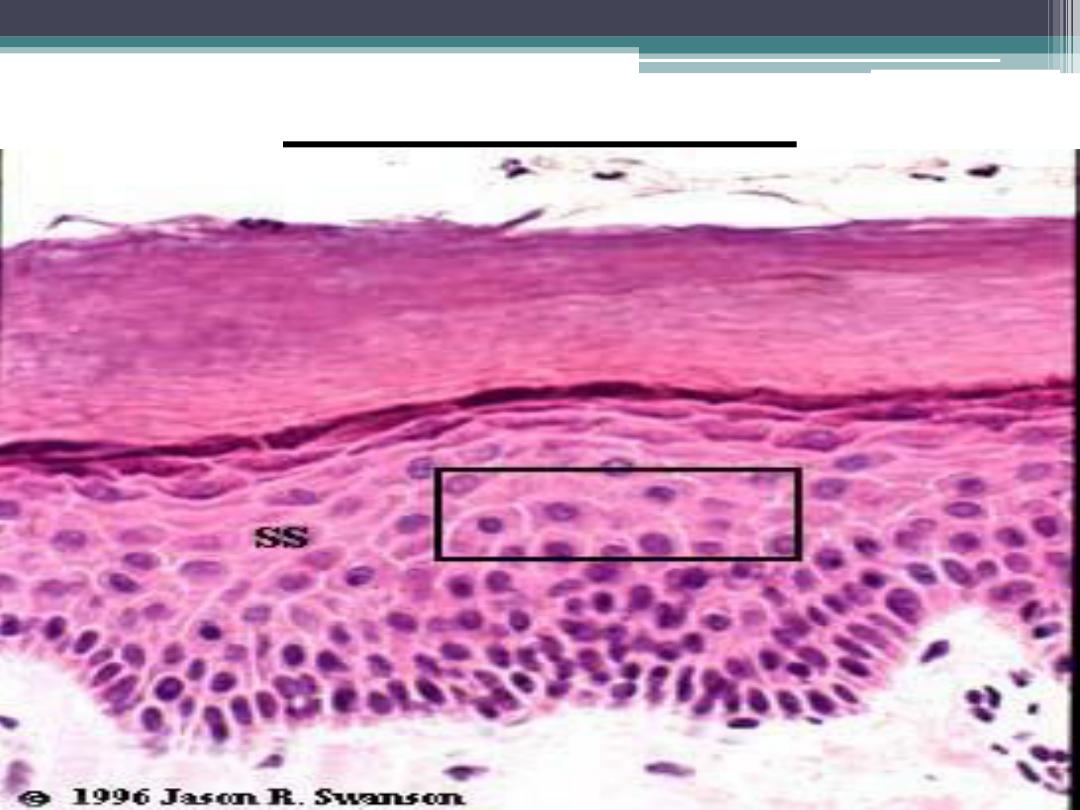
Strstum spinosum
Stratum spinosum
(cont.)
The spines represent the sites where
desmosomes are anchored to bundles of
intermediate keratin filaments, or
tonofilaments , and to neighboring cells.
The synthesis of keratin filaments continues
in this layer that become assembled into
bundles of tonofilaments.
Tonofilaments maintain cohesion among
cells and provide resistance to abrasion of the
epidermis.
3- Stratum Granulosum
Cells above the stratum spinosum become
filled with dense basophilic keratohyalin
granules and form the third layer ,stratum
granulosum .
Three to five layers of flattened cells form
this layer.
The granules are not surrounded by a
membrane and are associated with bundles of
keratin tonofilaments .
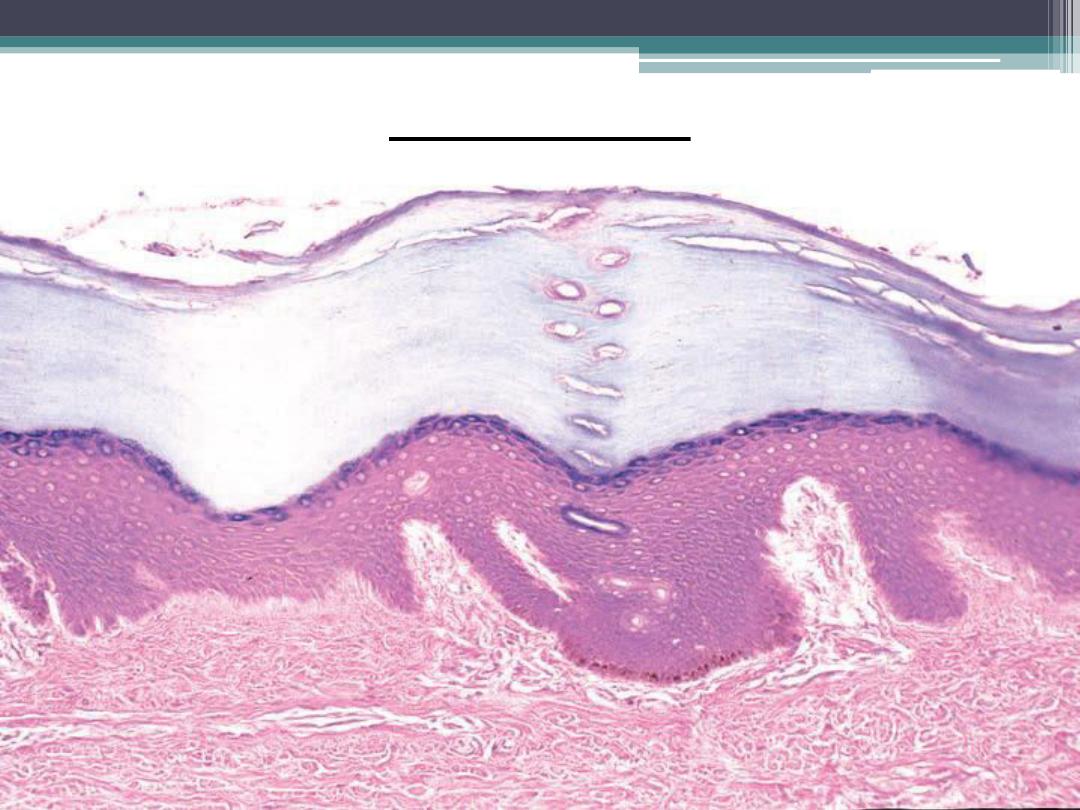
Thick skin
Cont.
The combination of keratin tonofilaments
with keratohyalin granules in these cells
produces keratin.
The keratin formed by this process is the
soft keratin of skin. The lamellar granules are
discharged into the intercellular spaces of
stratum granulosum as layer of lipid and seal
the skin. This process renders the skin
relatively impermeable to water .
4- Stratum Lucidum :
In thick skin only, the stratum lucidum is
translucent and barely visible; it lies just
superior to stratum granulosum and inferior
to the stratum corneum.
The tightly packed cells lack nuclei or
organelles and are dead. The flattened cells
contain densely packed keratin filaments.
5- Stratum Corneum :
The stratum corneum is the fifth and most
superficial layer of skin. All nuclei and
organelles have disappeared from the cells.
Stratum corneum primarily consists of
flattened, dead cells filled with soft keratin
filaments .
Cont.
The keratinized, superficial cells from this
layer are continually shed or desqumated and
are replaced by new cells arising from the deep
stratum basale.
During the keratinization process, the
hydrolytic enzymes disrupt the nucleus and
cytoplasmic organelles, which disappear as
the cells fill with keratin.
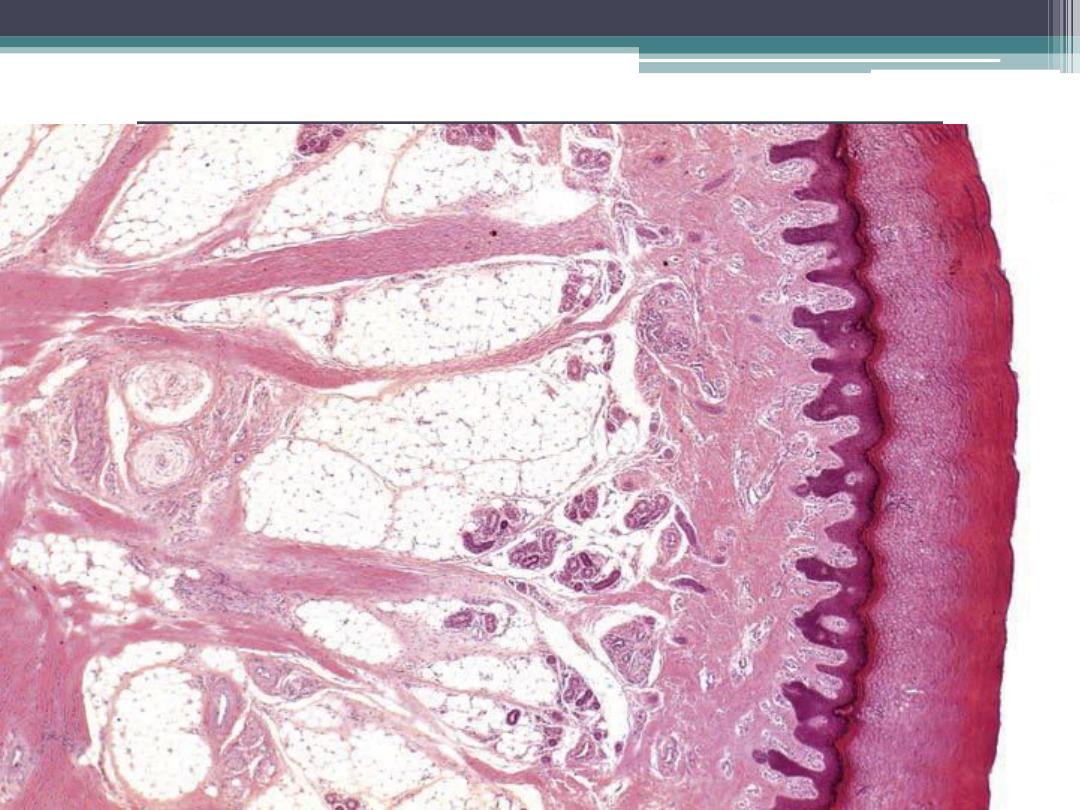
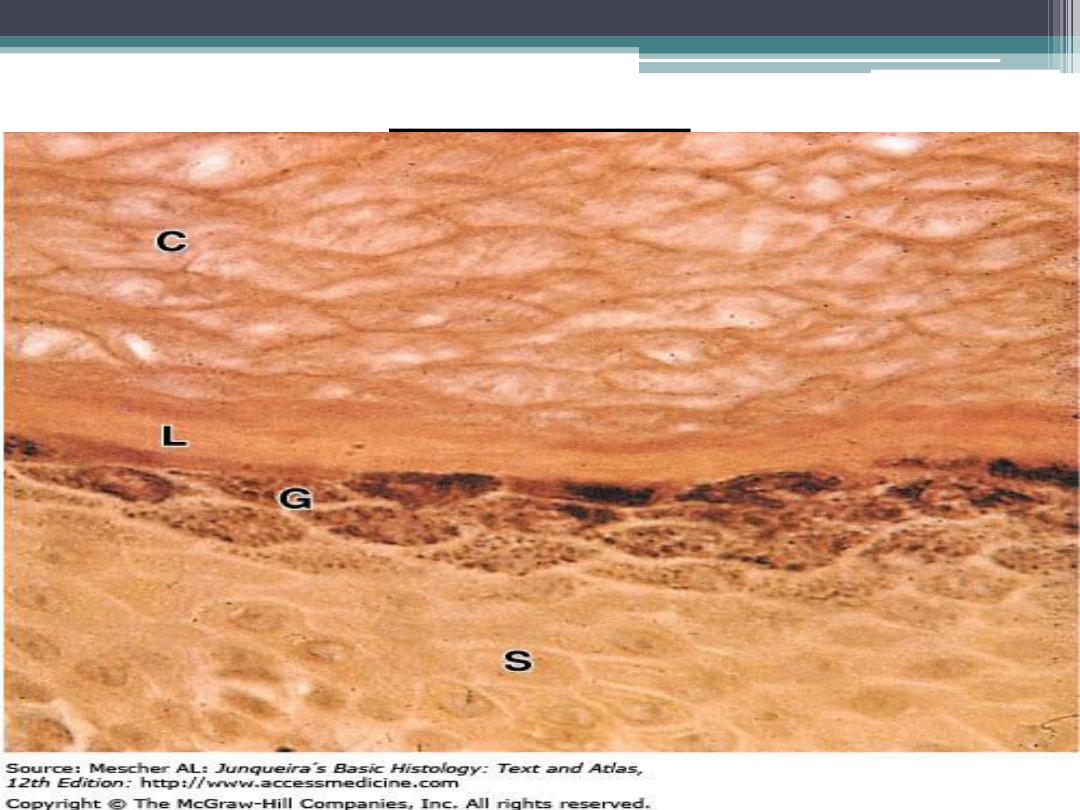
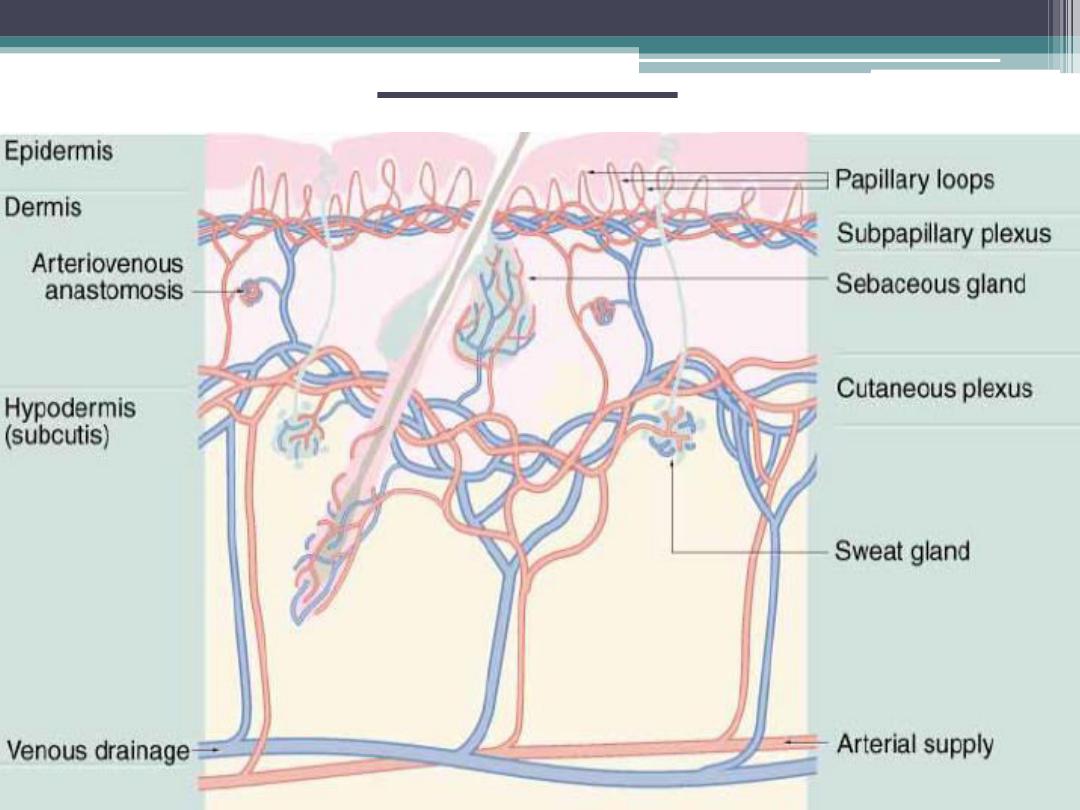
Dermis: Papillary and Reticular Layers
Dermis is the connective tissue layer that
binds to epidermis. A distinct basement
membrane separates the epidermis from the
dermis. In addition, dermis also contains
epidermal derivatives such as sweat glands ,
sebaceous glands, and hair follicles.
(cont.)
The junction of the dermis with the
epidermis is irregular. The superficial layer of
the dermis forms numerous raised
projections called
dermal papillae
, which
interdigitate with evaginations of epidermis,
called
epidermal ridges.
(cont.)
This region of skin is
the papillary layer
of the dermis.
This layer is filled with loose irregular
connective tissue fibers, capillaries, blood
vessels, fibroblasts , macrophages , and other
loose connective tissue cells.
(cont.)
The deeper layer of dermis is called the
reticular layer
. This layer is thicker and is
characterized by dense irregular connective
tissue fibers (mainly type I collagen), and is less
cellular than the papillary layer. There is no
distinct boundary between the two dermal
layers, and the papillary layer blends with the
reticular layer.
Reticuler fibers of dermis
Dermis (cont.)
The connective tissue of the dermis is
highly vascular and contains numerous blood
vessels,lymph vessels, and nerves.
Certain regions of skin exhibit
arteriovenous anastomoses used for
temperature regulation.
Sensory receptors :
Two types of encapsulated touch/pressure
receptors are commonly found in the dermis.
Relatively small Meissner's corpuscles are
located near the crests of the dermal papillae.
Larger Pacinian corpuscles are encapsulated
pressure receptors located deep in the reticular
layer.
1-
Meissner’s corpuscles:
Meissner’s tactile corpuscles occur singular
or in small groups in the dermal papillae
immediately underneath the epidermis. They
are long oval and positioned vertical to the skin
surface.
Meissner’s corpuscles are about 40–
70
μm wide and 100–150μm long and consist of
myelinated afferent nerve fibers with wide,
plate-like nerve terminals . Approximately
seven myelinated afferent axons are found per
corpuscle.
Cont.
Meissner’s tactile corpuscles are
mechanoreceptors, which react to pressure and
adapt with medium speed.
Meissner’s corpuscles
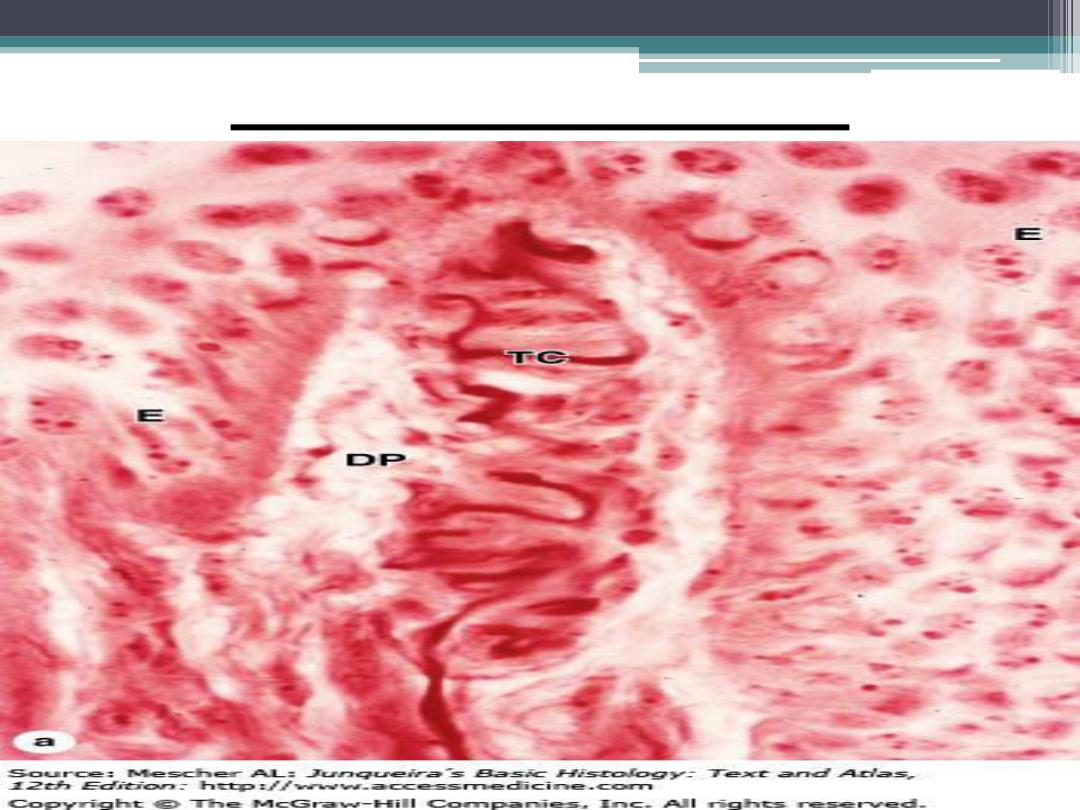
Meissner’s corpuscles
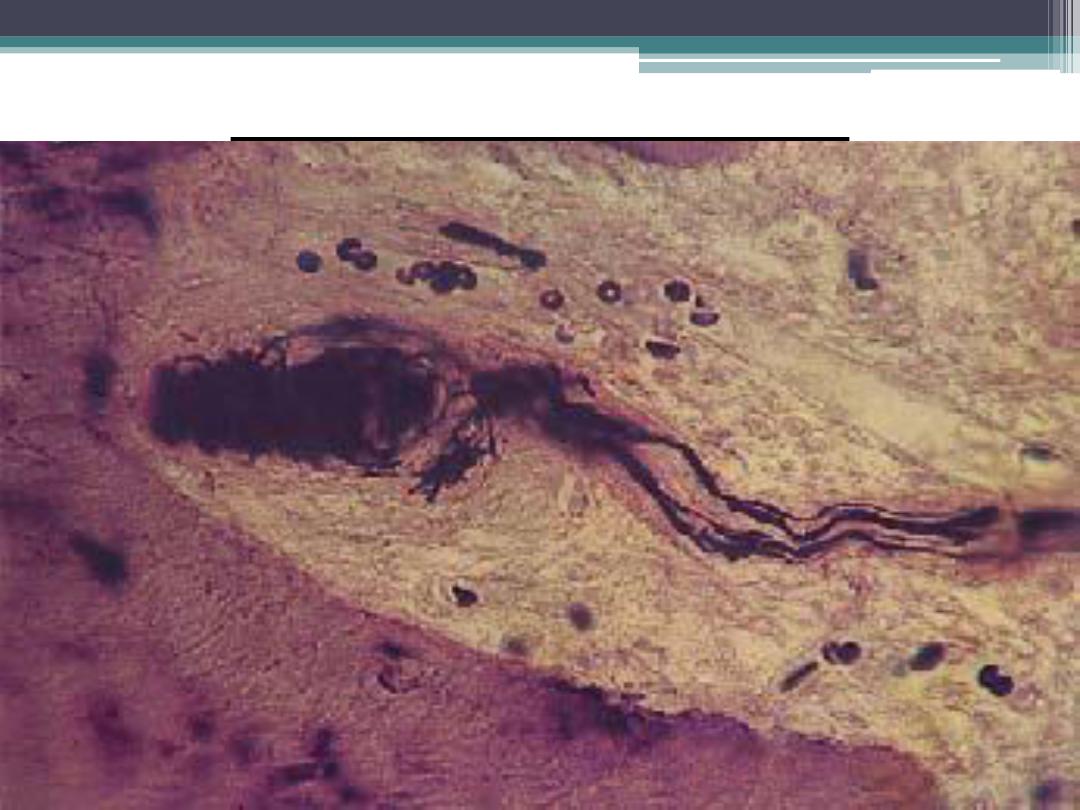
2- Pacinian corpuscles :
large lamellated corpuscles are up to 4 mm
long and 2 mm thick. Their giant size makes
them easy to detect, e.g., in the subcutaneous
tissue of the palms of the hand and the soles of
the feet and proximal phalanxes as well as in
the vicinity of fasciae, periosteum and tendons.
The sheaths of these terminal nerve systems are
a characteristic feature.
Cont.
They consist of 40
–60 concentric layers of
cytoplasmic processes (perineural lamellae) in
an onionlike arrangement.
The nerve fiber is found in the center (inner
afferent axon) . The connective tissue capsule
around the corpuscle contains a meshwork of
elastic fibers.
Pacini corpuscles are pressure and vibration
receptors .
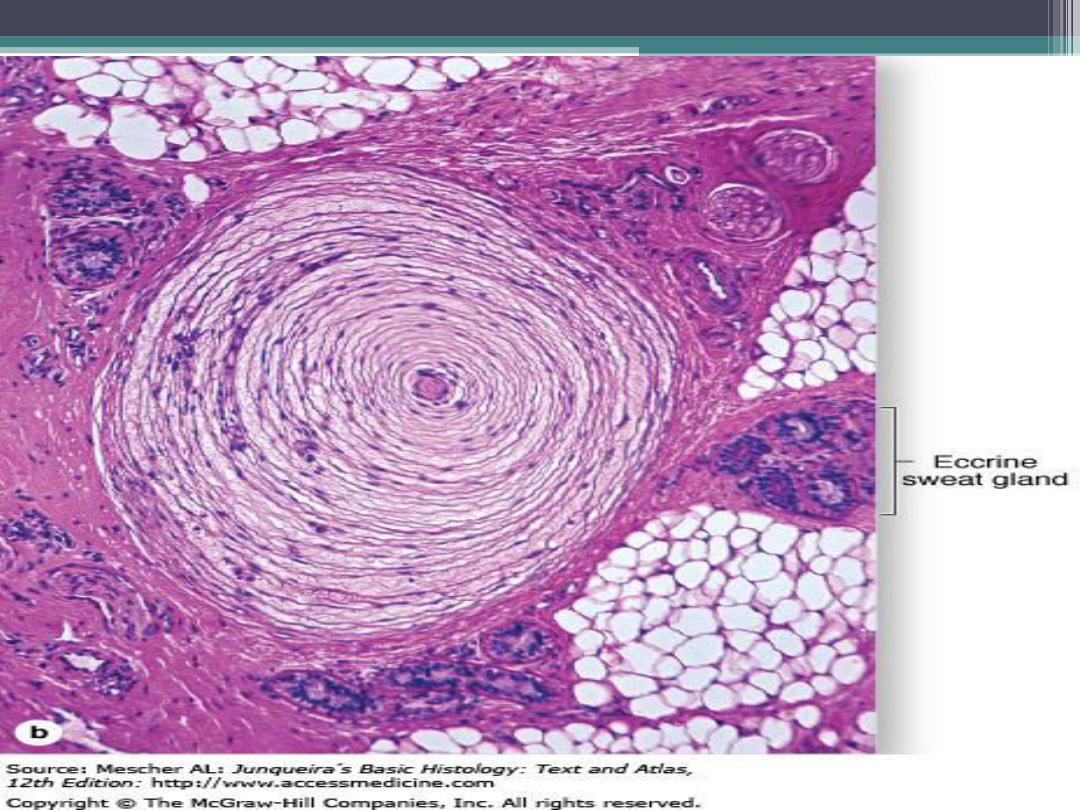
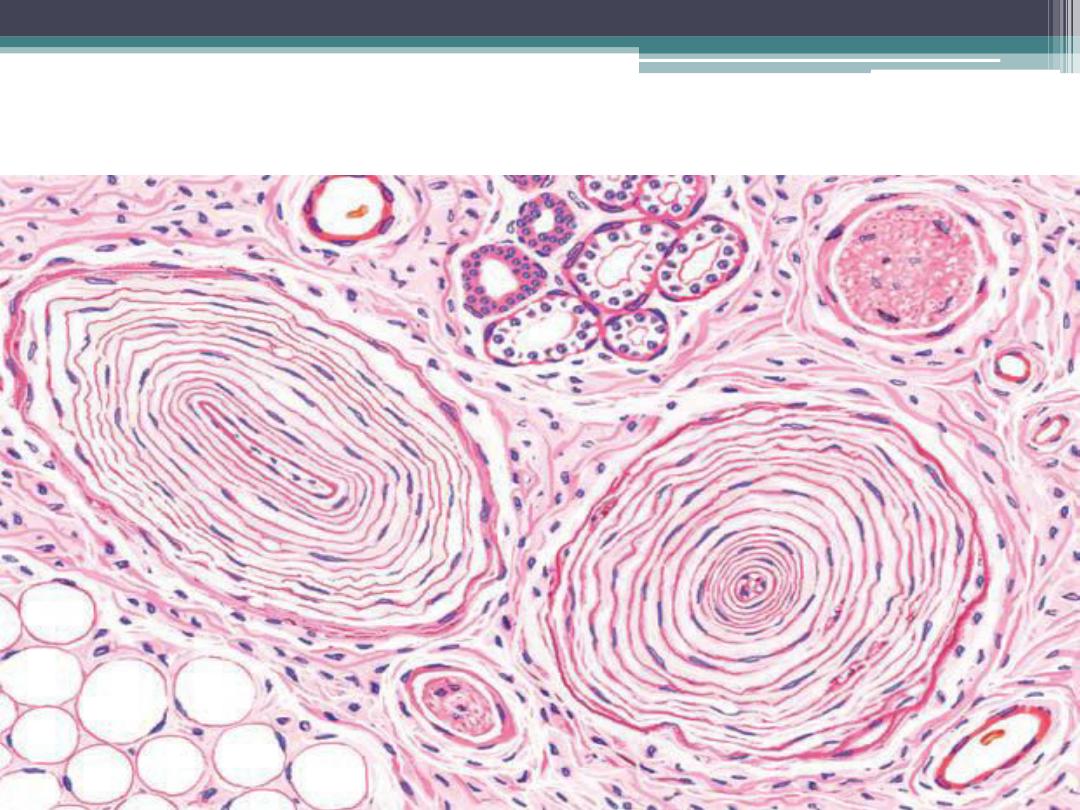
Pacinian corpousle in dermis of
thick skin
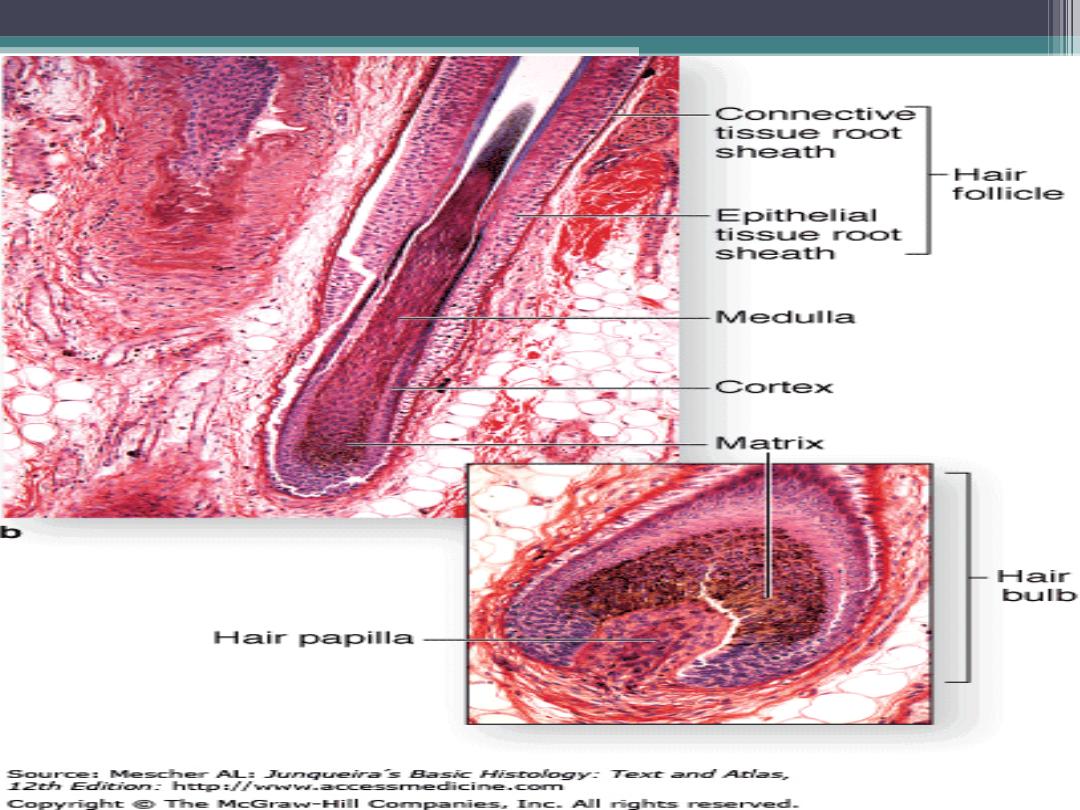
Hair follicle :
Hairs are the hard, cornified, cylindrical
structures that arise from hair follicles in the
skin. One portion of the hair projects through
the epithelium of the skin to the exterior
surface; the other portion remains embedded in
the dermis. Hair grows in the expanded portion
at the base of the hair follicle called the hair
bulb.
(cont.)
The base of the hair bulb is indented by a
connective tissue papilla, a highly vascularized
region that brings essential nutrients to hair
follicle cells, the hair cells divide, grow, cornify,
and form the hairs.
Associated with each hair follicle are one or
more sebaceous glands that produce an
oily secretion called sebum.
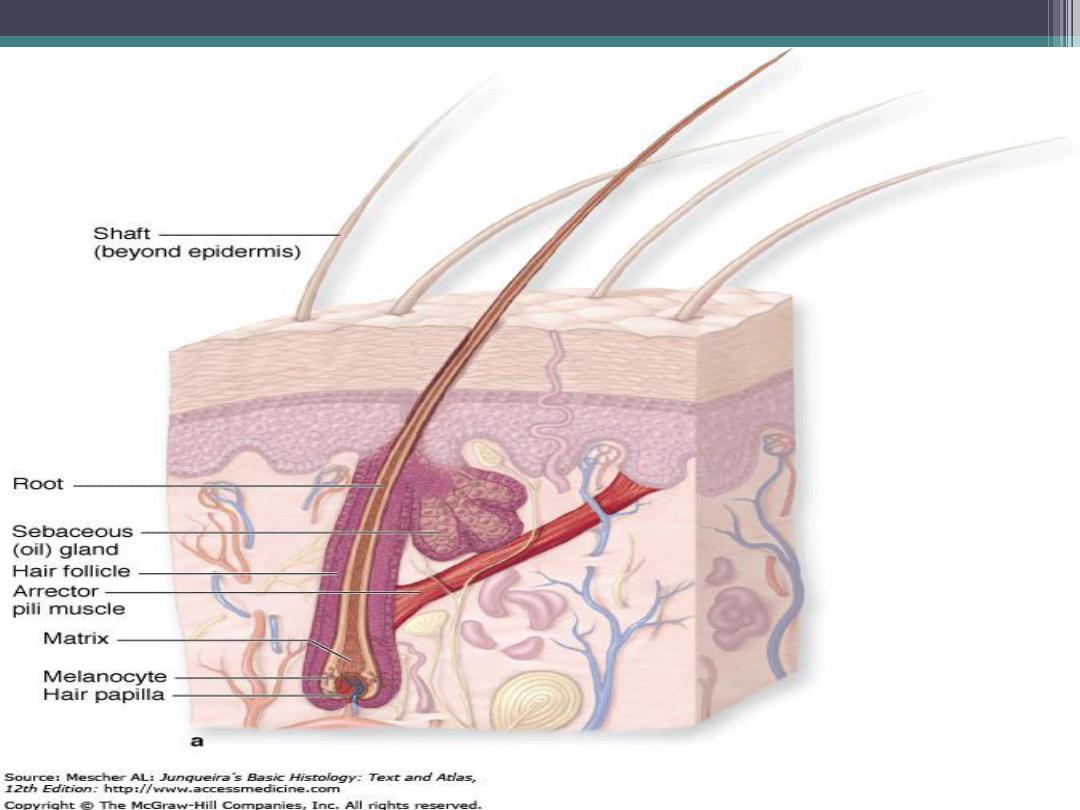
Cont.
Sebum forms when cells die in sebaceous
glands. Also, extending from the connective
tissue around the hair follicle to the papillary
layer of the dermis are bundles of smooth
muscle called arrector pili. The sebaceous
glands are located between the arrector pili
muscle and the hair follicle.

cont.
Arrector pili muscles are controlled by the
autonomic nervous system and contract during
strong emotions, fear, and cold.
Contraction of the arrector pili muscle erects
the hair shaft, depresses the skin where it
inserts ,and produces a small bump on the
surface of skin, often called a goose bump.
cont.
In addition, this contraction forces the
sebum from sebaceous glands onto the hair
follicle and skin .
Sebum oils keeps the skin smooth,
waterproofs it, prevents it from drying, and
gives it some antibacterial protection.
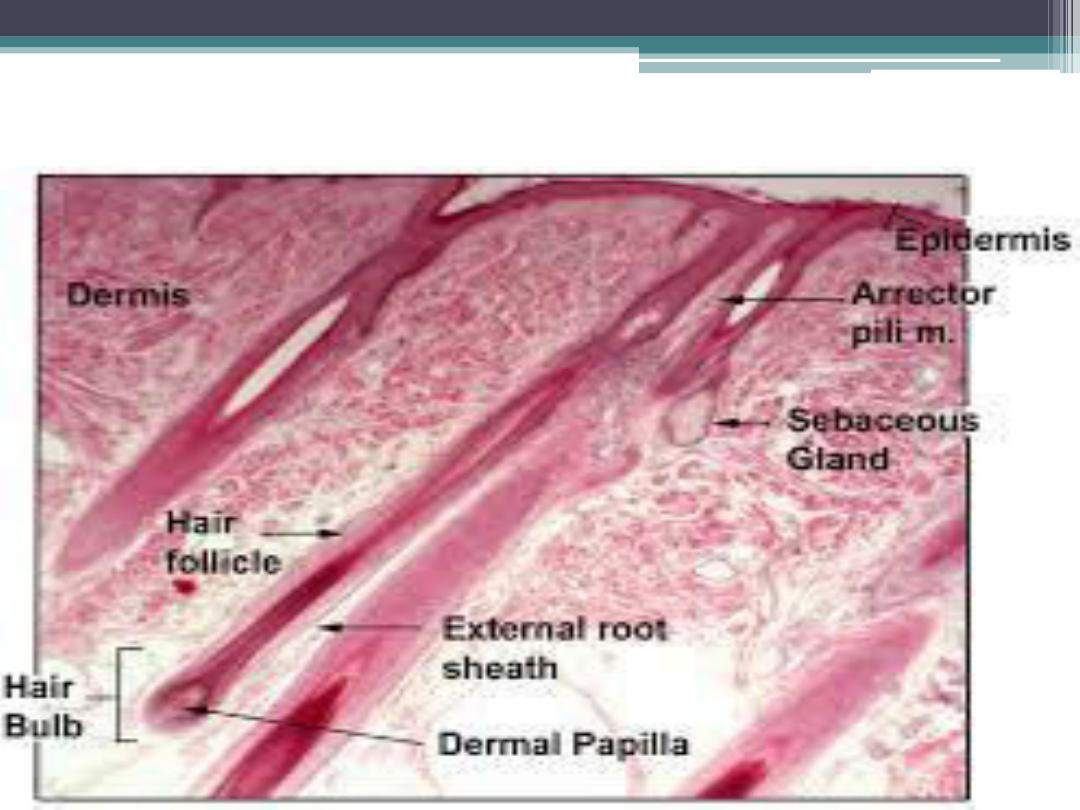
Hair follicle
Sebaceous Glands
Sebaceous glands occur in most parts of the
skin and are especially numerous in the scalp
and face and around the anus, mouth, and
nose. They are absent from the palms of the
hands and soles of the feet, sebaceous glands
are associated with hairs and drain into the
upper part of the hair follicle,
Cont.
The glands vary in size and consist of a
cluster of two to five oval alveoli drained by a
single duct.
The secretory alveoli lie within the dermis
and are composed of epithelial cells enclosed in
a well defined basement membrane and
supported by a thin connective tissue capsule.
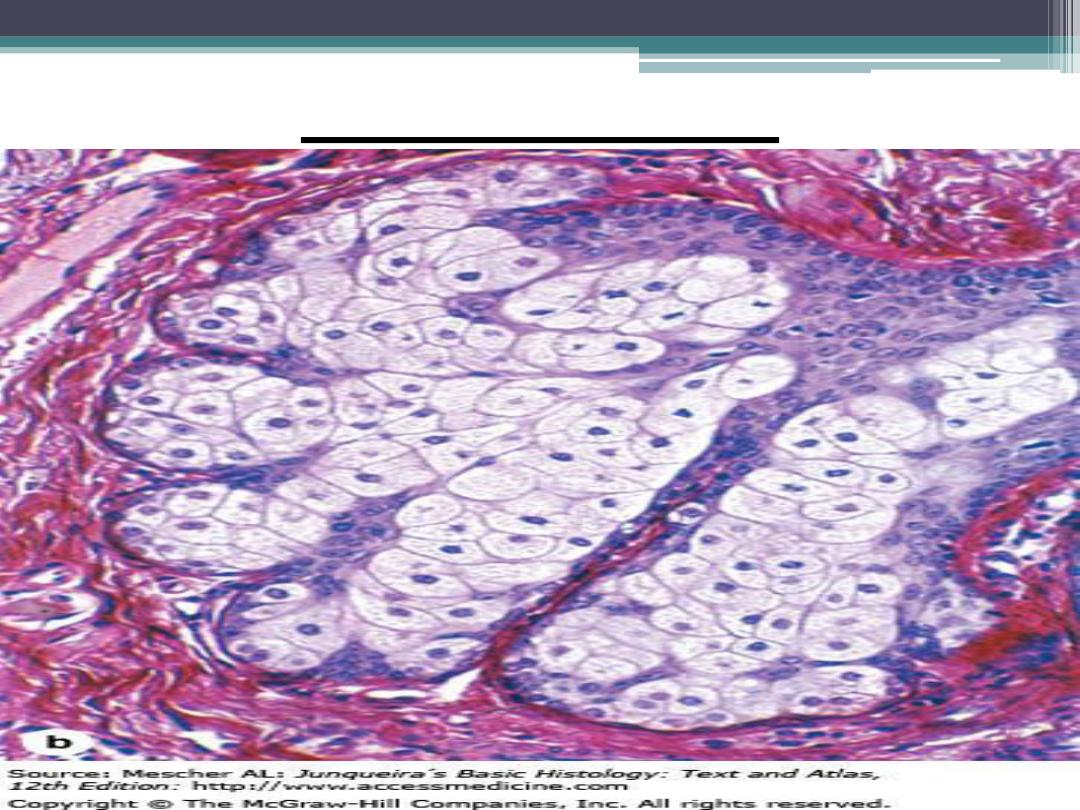
Sebaceous gland
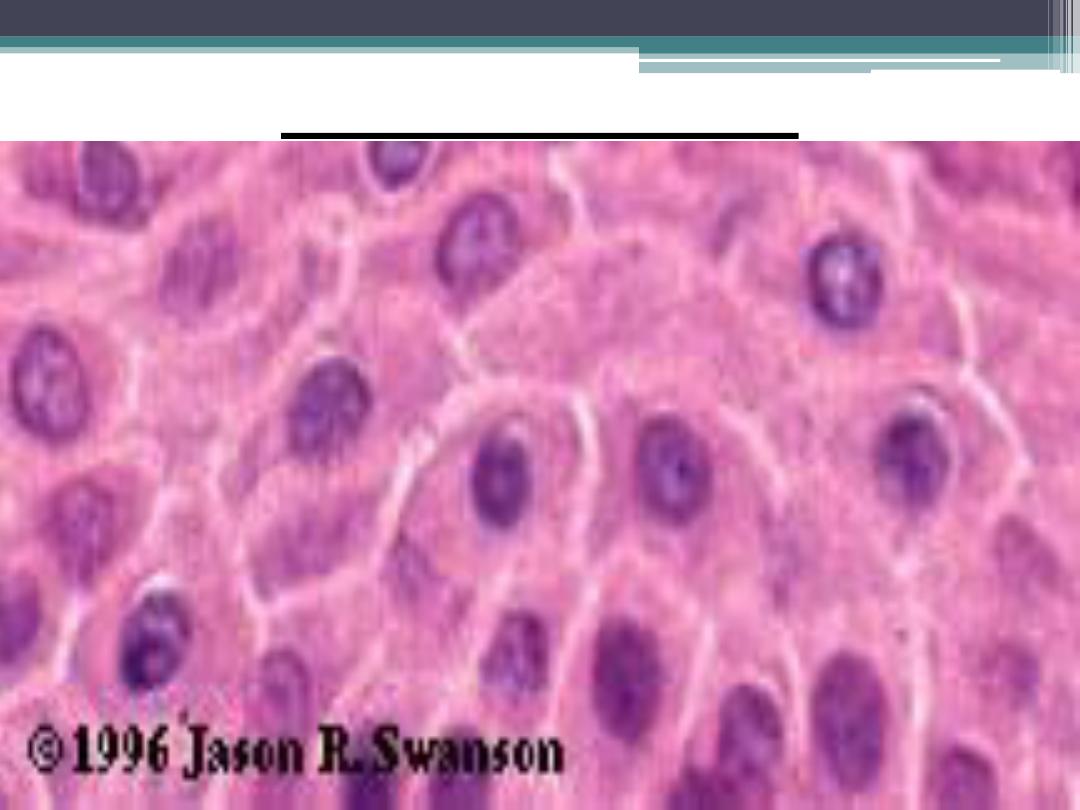
Cont.
cells are small and cuboidal and contain
round nuclei. The entire alveolus is filled with
cells that, centrally, become larger and
polyhedral and gradually accumulate fatty
material in their cytoplasm. Secretion is of the
holocrine type, meaning the entire cell breaks
down, and cellular debris, along with the
secretory product (triglycerides, cholesterol,
and wax esters),is released as sebum .
Sweat glands :
Sweat glands are widely distributed in skin
,and are of two types :
1- eccrine (merocrine)
2- apocrine
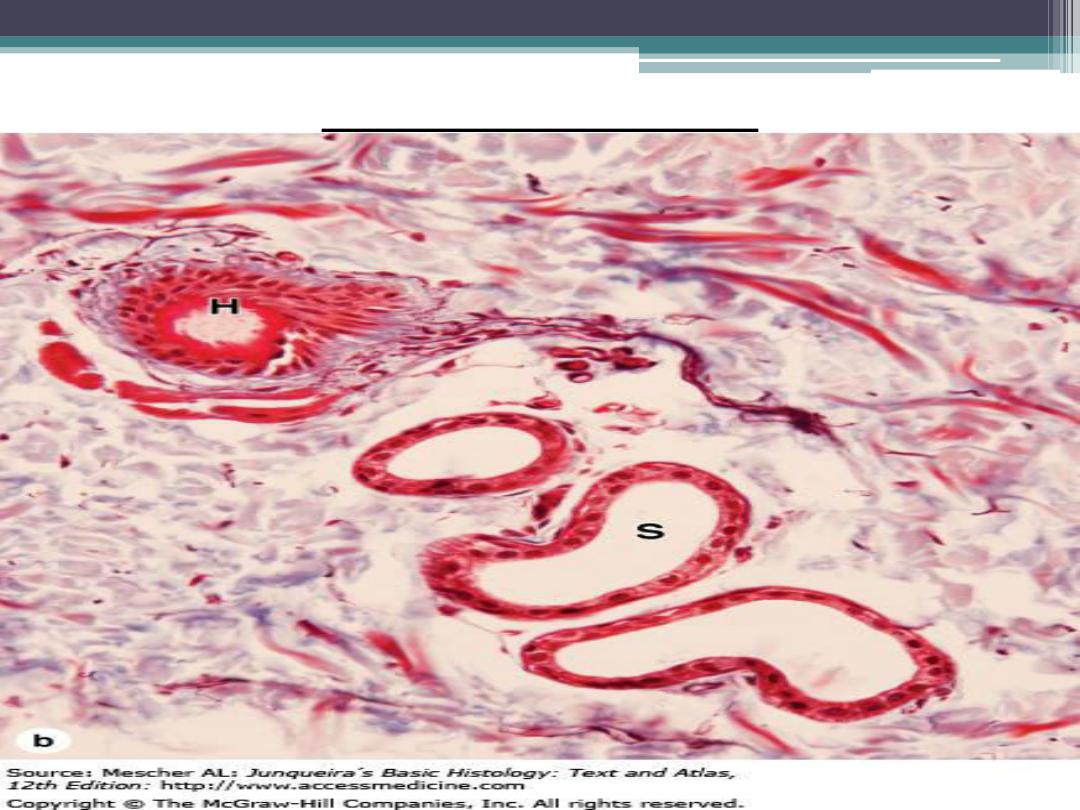
1- eccrine glands :(merocrine)
Eccrine sweat glands are simple, coiled
tubular glands. Their secretory portion is found
deep in the dermis , from which a coiled
excretory duct leads to the skin surface. The
eccrine sweat glands contain two cell types:
clear cells without secretory granules and
dark cells with secretory granules.
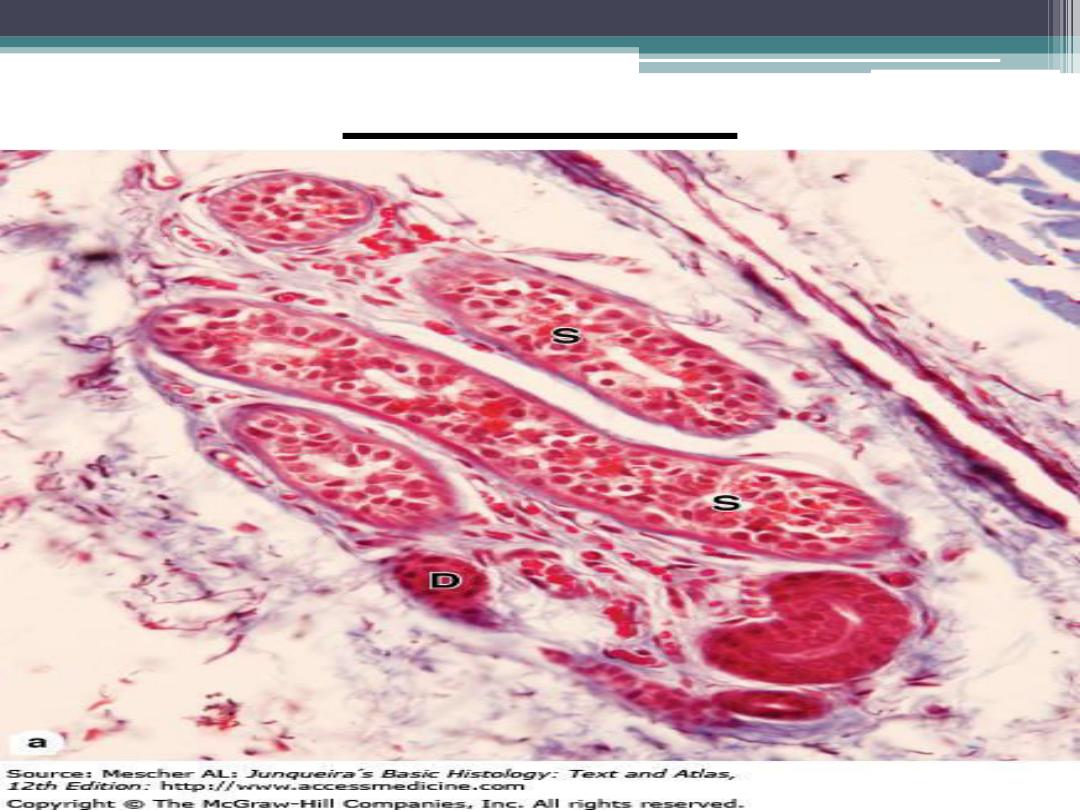
Eccrine gland
(cont.)
Secretion from the dark cells is primarily
mucous, whereas secretion from clear cells is
watery.
Surrounding the basal region of the
secretory portion of each sweat gland are
myoepithelial cells, whose contraction
expels the secretion (sweat) from sweat glands.
Eccrine glands (cont.)
Eccrine sweat glands are most numerous
in the skin of the palms and soles. The eccrine
sweat glands assist in temperature regulation.
Sweat glands also excrete water, sodium
salts, ammonia, uric acid, and urea.
Secretory portion of eccrine gland
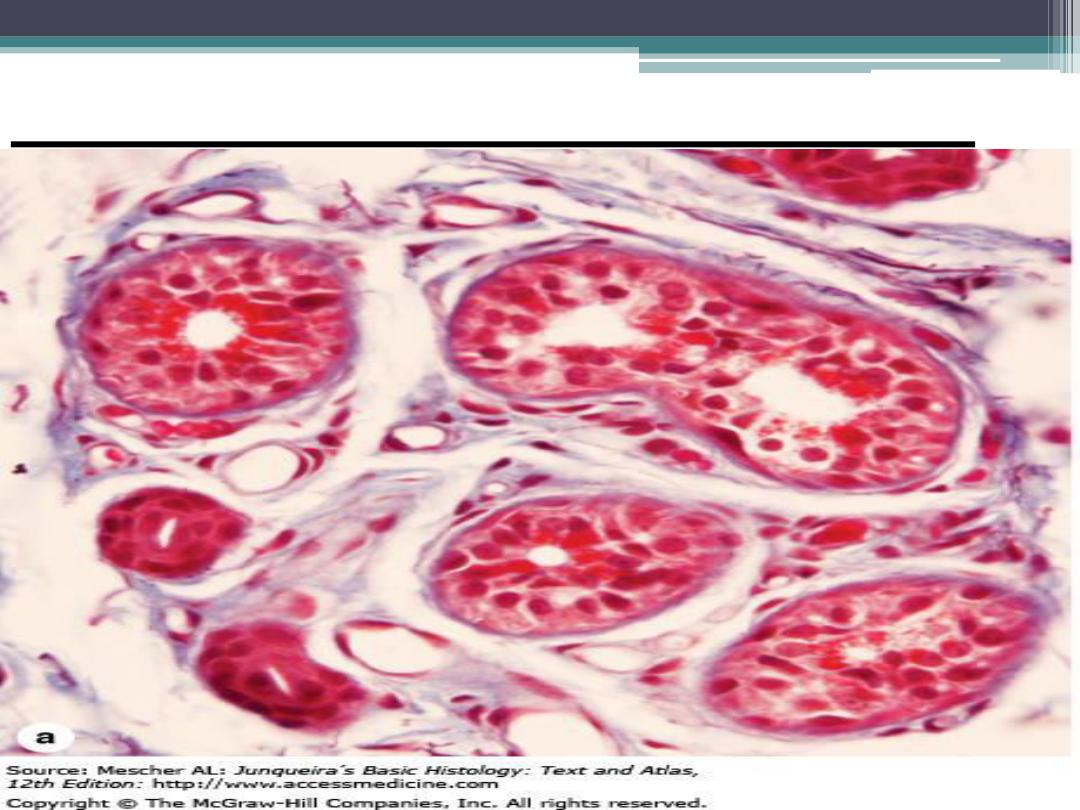
2- apocrine glands :
Apocrine sweat glands are also found in
the dermis and are primarily limited to the
axilla ,anus , and areolar regions of the
breast.
These sweat glands are larger than eccrine
sweat glands, and their ducts open into the
hair follicle.
Apocrine gland
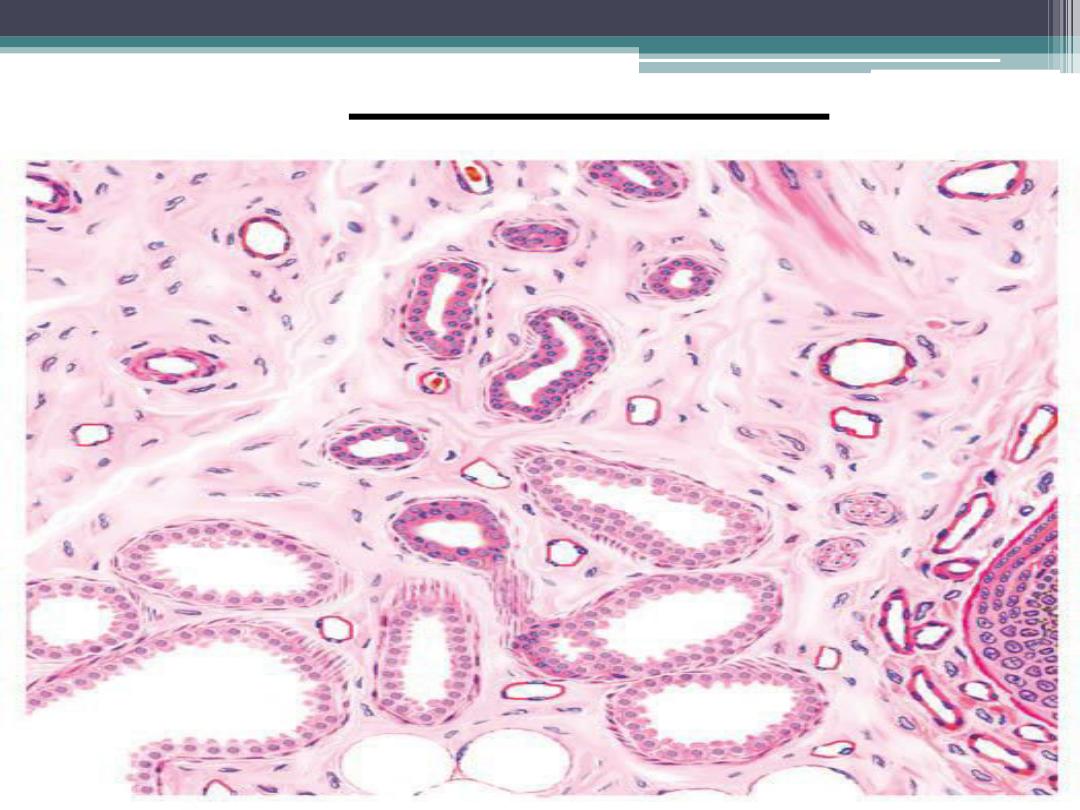
Apocrine glands
(cont.)
The secretory portion of the gland is coiled
and tubular, In contrast to eccrine sweat
glands, the lumina of the secretory portion of
the gland are wide and dilated,and the
secretory cells are low cuboidal ,simillar to
eccrine glands.
(cont.)
The secretory portion of the glands is
surrounded by contractile myoepithelial cells.
The apocrine glands become functional at
puberty ,when sex hormones are produced .
The glands produce a viscous secretion,
which acquires a distinct and unpleasent odor
after bacterial decomposition.
Arteriovenous anastomoses
In numerous tissues, direct
communications between arteries and veins
called arteriovenous anastomoses bypass
the capillaries .
Their main functions are regulation of blood
pressure, blood flow ,and temperature, and
conservation of body heat. A more complex
structure that also forms shunts is called a
glomus
.
circulation
Cont.
A glomus consists of a highly coiled
arteriovenous shunt that is surrounded by
collagenous connective tissue. The function of
the glomus is also to regulate blood flow and
conserve body heat. These structures are found
in the fingertips, external ear ,and other
peripheral areas that are exposed to excessive
cold temperatures and where arteriovenous
shunts are needed.
Nails
The nails are hard, keratinized structures
that cover the dorsal surfaces of the tips of the
fingers and toes. Each nail consists of a visible
body (nail plate) and a proximal part, the
root, which is implanted into a groove in the
skin. The root is overlapped by the proximal
nail fold, a fold of skin that continues along
the lateral borders of the nail, where it forms
the lateral nail folds.
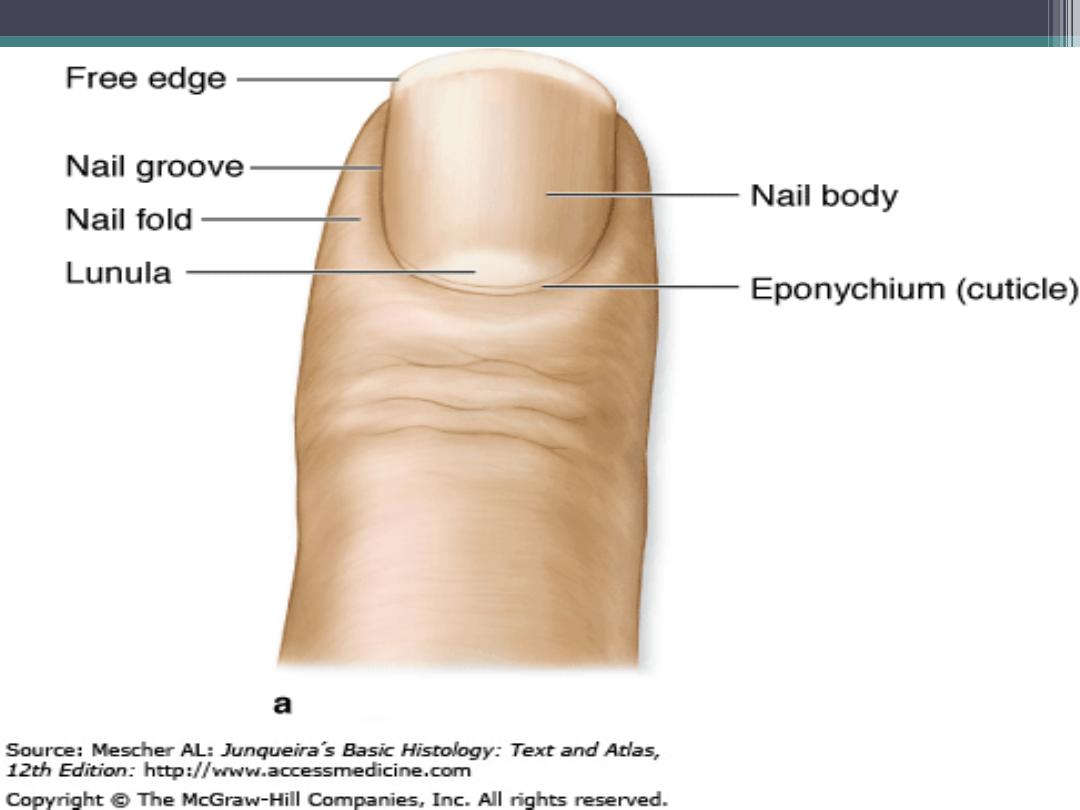
Cont.
Stratum corneum of the proximal nail fold
extends over the upper surface of the nail root
and for a short distance onto the surface of the
body of the nail, where it forms a thin
cuticular fold called the eponychium.
At the free border of the nail, the skin is
attached to the underside of the nail, forming
the hyponychium.
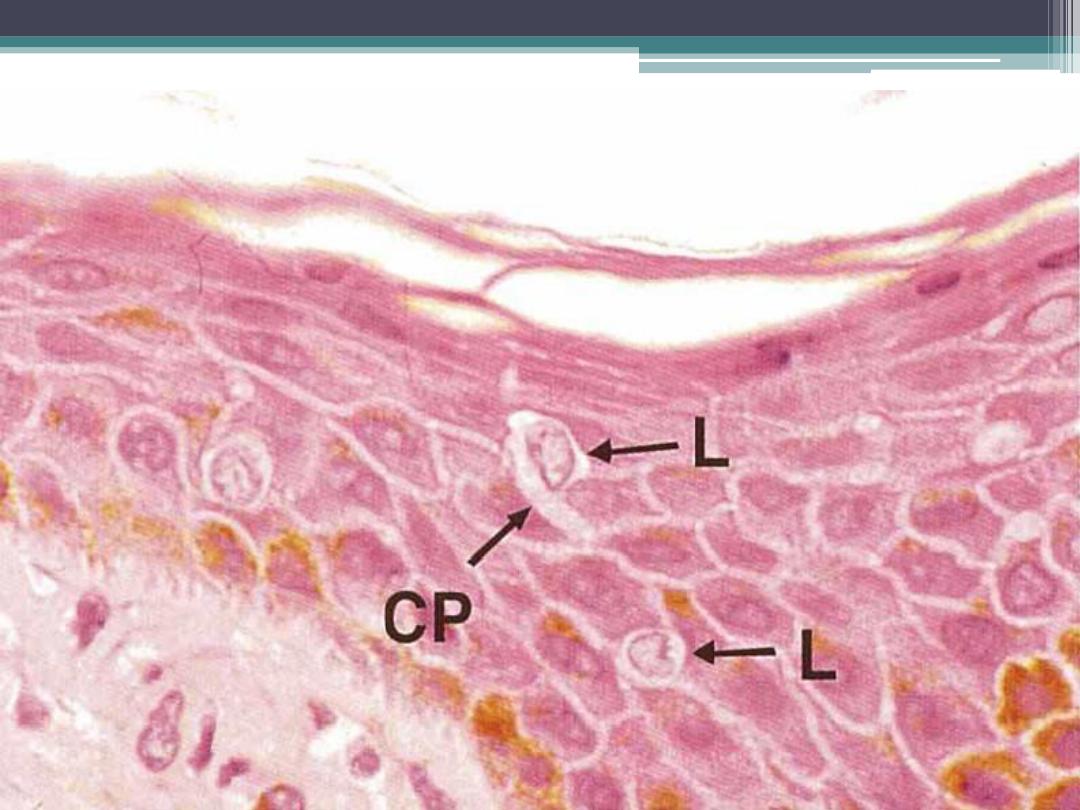
Cont.
The nail is a modification of the cornified
zone of the epidermis and consists of several
layers of flattened cells with shrunken,
degenerate nuclei.
The cells are hard, tightly adherent, and
throughout most of the body of the nail, clear
and translucent. The pink color of the nails is
due to transmission of color from the
underlying capillary bed.
Cont.
Near the root, the nail is more opaque and
forms a crescentic area, the lunule, which is
most visible on the thumb, becoming smaller
and more hidden by the proximal nail fold
toward the little finger. The lunule represents
the region from which nail formation occurs.
Beneath the nail lies the nail bed. It consists of
prickle cells and a stratum basale resting on a
basement membrane.
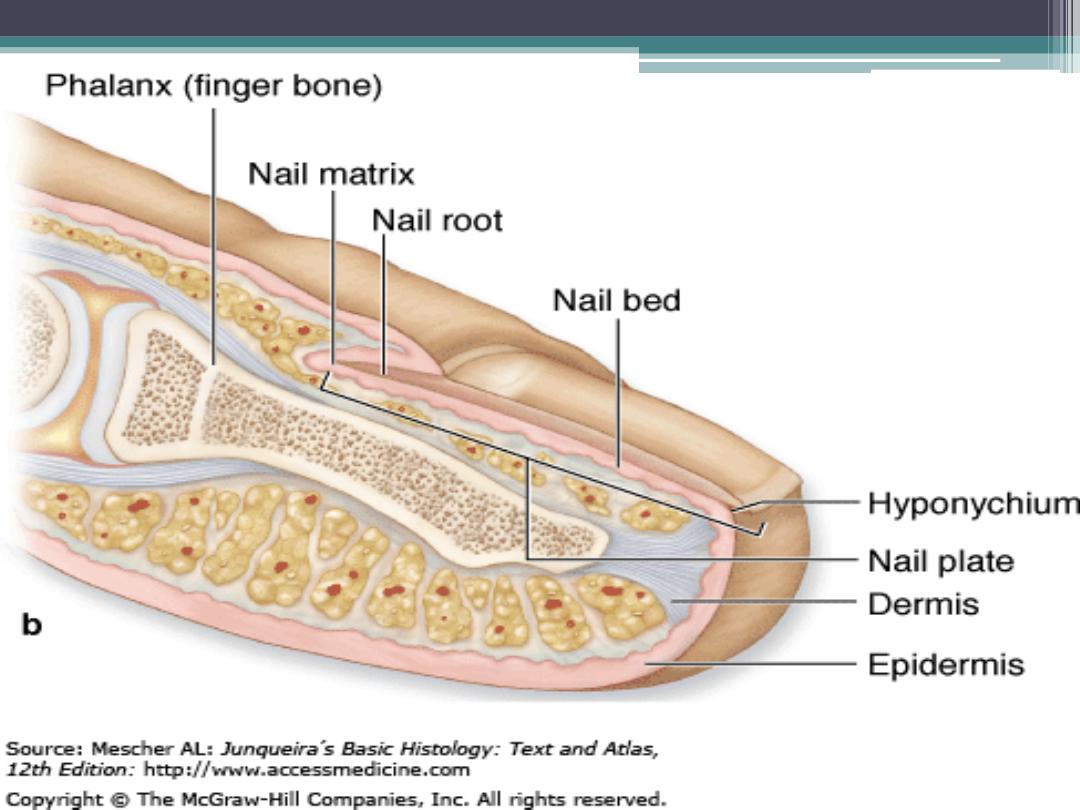
Cont.
The nail bed beneath the root and
lunule is thicker, actively proliferative, and
concerned with growth of the nail; it is called
the nail matrix . Nail keratin has higher
sulfur content than the keratin of the epidermis
and is called hard keratin .
Thank you
