By
Dr. Suhair Majeed
The Blood
Blood is a unique form of connective tissue that
consists of three major cell types: erythrocytes
(red blood cells), leukocytes (white blood cells), and
platelets (thrombocytes).
These cells, also called the formed elements of
blood, are suspended in a liquid medium called plasma.
Blood cells transport gases, nutrients, waste
products, hormones, antibodies, various chemicals, ions,
and other substances in the plasma to and from different
cells in the body.
Medical Histology
Laboratory Tests
Collect blood in a tube with an anticoagulant and
centrifuge:-
Two major layers form:-
1-Bottom solid cellular layer
Largest layer, red cells, bottom red layer
White cell, “buffy coat” small white/gray
layer
Top layer, invisible thin platelet layer
2-Top aqueous plasma layer
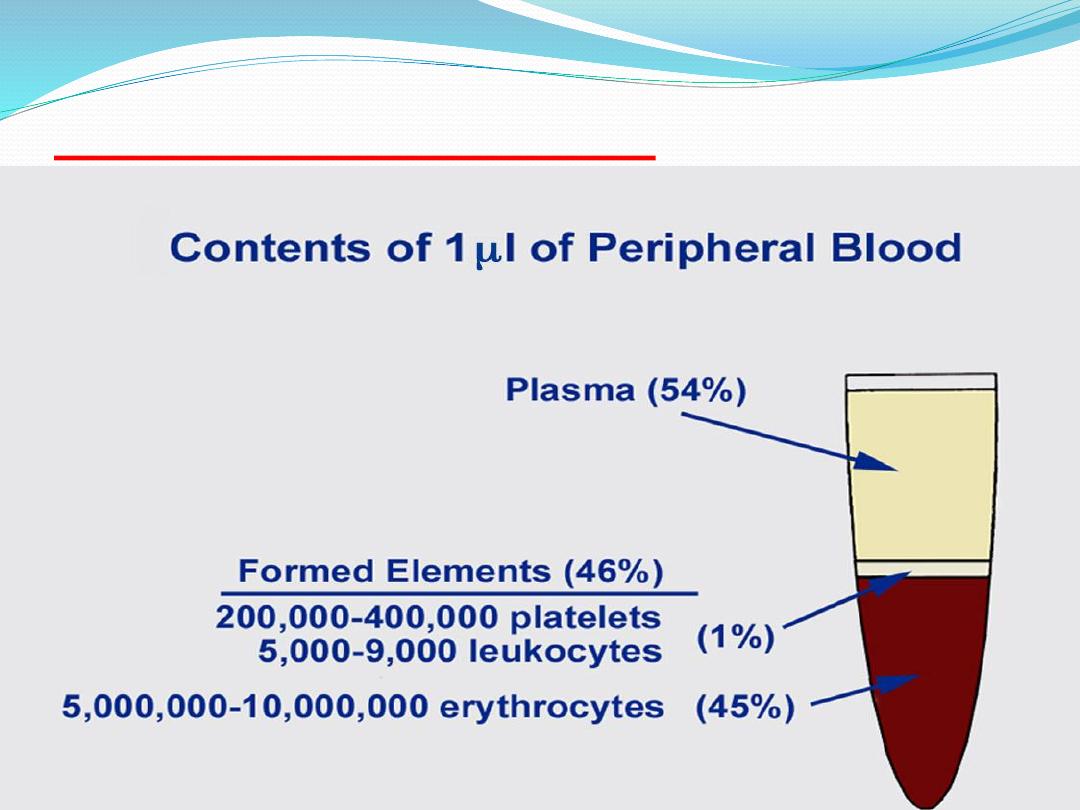
Blood composition
Cont.
Leukocytes (white blood cells, WBC)
1-Granulocytes (with specific granules)
Neutrophil (~60% of WBC)
Eosinophil (~4% of WBC)
Basophil (<1% of WBC)
2-Agranulocytes (without specific granules)
Lymphocyte (B-cell, T-cell) (~27% of WBC)
Monocyte (~8% of WBC)
Plasma
Typical sample of plasma is composed
of :-
90% water
8% protein
1% in organic salts
0.5% lipids
0.1% sugar

plasma
Straw colored, nonliving
part of blood.
90% Water
Helps to regulate body
temperature
Contains Electrolytes
Plasma transports blood
cells, products of
digestion and hormones
throughout the body.
Plasma proteins
There are three main groups of proteins in
plasma :
1-the blood coagulation proteins.
2- albumin.
3 -globulins.
The globulins can be divided in to :
*alpha globulins
*beta globulins
*gamma globulins
(mainly immunoglobulins).
Cont.
The plasma proteins are nearly all derived
from synthesis in the liver , with the exception of
the immunoglobulins which are synthesised by
plasma cells .
Major Blood Cell Types:
Microscopic examination of a stained blood
smear reveals the major blood cell types :
1- Erythrocytes :
or red blood cells are nonnucleated cells and are the
most numerous blood cells.
Erythrocytes remain in the blood and perform
their major functions within the blood vessels.
Cont.
2- leukocytes,
or white blood cells, are nucleated and subdivided into
granulocytes and agranulocytes, depending on the
presence or absence of granules in their cytoplasm
.
Granulocytes
are the neutrophils, eosinophils, and
basophils.
Agranulocytes
are the monocytes and lymphocytes.
Leukocytes perform their major functions outside of the
blood vessels. They migrate out of the blood vessels
through capillary walls and enter the connective tissue,
lymphatic tissue, and bonemarrow.
Cont.
The primary function of leukocytes is to defend the
body against bacterial invasion or the presence of foreign
material.
Consequently, most leukocytes are concentrated in the
connective tissue.
3- Platelets:
or thrombocytes are not blood cells. Instead, they are
the smallest, nonnucleated formed elements in the
blood and appear in the blood of all mammals.
Cont.
Platelets are produced when small, uneven portions
of the cytoplasm separate or fragment from the
peripheries of the megakaryocytes , are extruded into
the blood stream.
Like the erythrocytes, platelets perform their major
functions within the blood vessels. Their main function
is to continually monitor the vascular system and to
detect any damage to the endothelial lining of the
vessels.
If the endothelial lining breaks, the platelets adhere
to the damaged site and initiate a highly complex
chemical process that produces a blood clot.
1- erythrocytes :
Mature erythrocytes are specialized to transport
oxygen and carbon dioxide. This specialization is
attributable to the presence of the protein
hemoglobin in their cytoplasm.
Iron molecules in hemoglobin bind with oxygen
molecules.
As a result, most of the oxygen in the blood
is carried in the combined form of
oxyhemoglobin
,
which is responsible for the bright red color of
arterial blood.
Cont.
Carbon dioxide diffuses from the cells and tissues
into the blood vessels.
It is carried to the lungs partly dissolved in the
blood and partly in combination with hemoglobin
in the erythrocytes as
carbaminohemoglobin
, which
gives venous blood its bluish color.
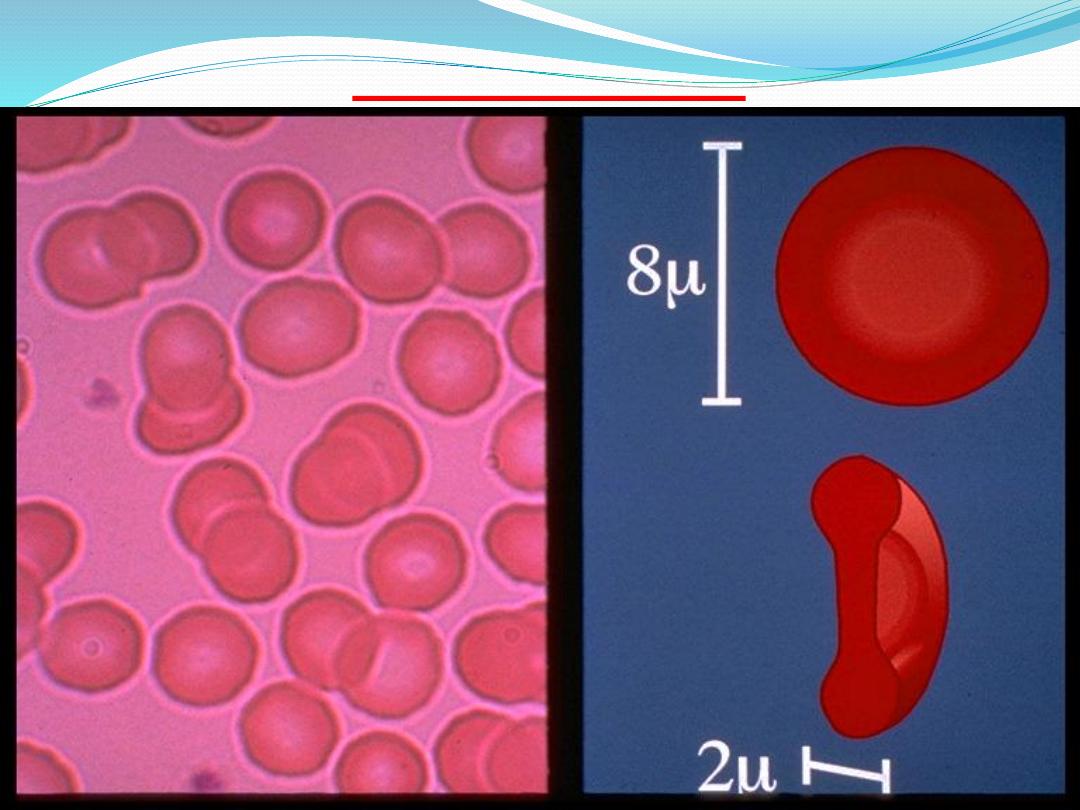
Cont.
During differentiation and maturation in the bone
marrow, erythrocytes synthesize large amounts of
hemoglobin.
Before an erythrocyte is released into the systemic
circulation, the nucleus is extruded from the cytoplasm,
and the mature erythrocyte assumes a biconcave shape.
This shape provides more surface area for carrying
respiratory gases.
Thus, mature erythrocytes in the circulation are
nonnucleated biconcave disks that are surrounded
by a membrane and filled with hemoglobin and some
enzymes.
Cont.
The life span of erythrocytes is approximately
( 120) days, after which the worn-out cells are
removed from the blood and phagocytosed by
macrophages in the spleen, liver, and bone marrow.
Woman usually have ( 4-5 million )erythrocytes per
cubic millimeter of blood, men have (5-6 million).
If this number is considerably higher, polycythemia
may be the cause. If the number is considerably
less, the person has anemia.
CONT
.
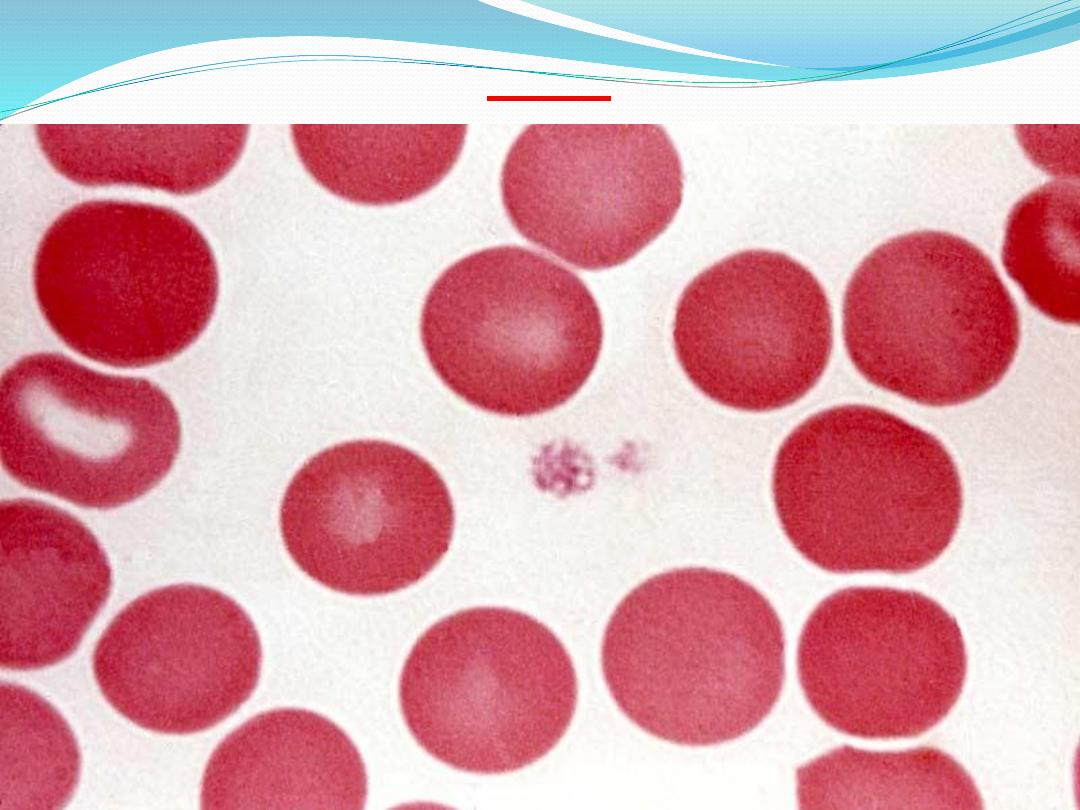
Sickle cell anemia is an inherited condition which
results in some erythrocytes being malformed.
The gene for this condition causes the hemoglobin
to be incorrectly formed, which in turn causes some
erythrocytes to take on a crescent shape.
These cells are not able to carry adequate amounts
of oxygen to cells.
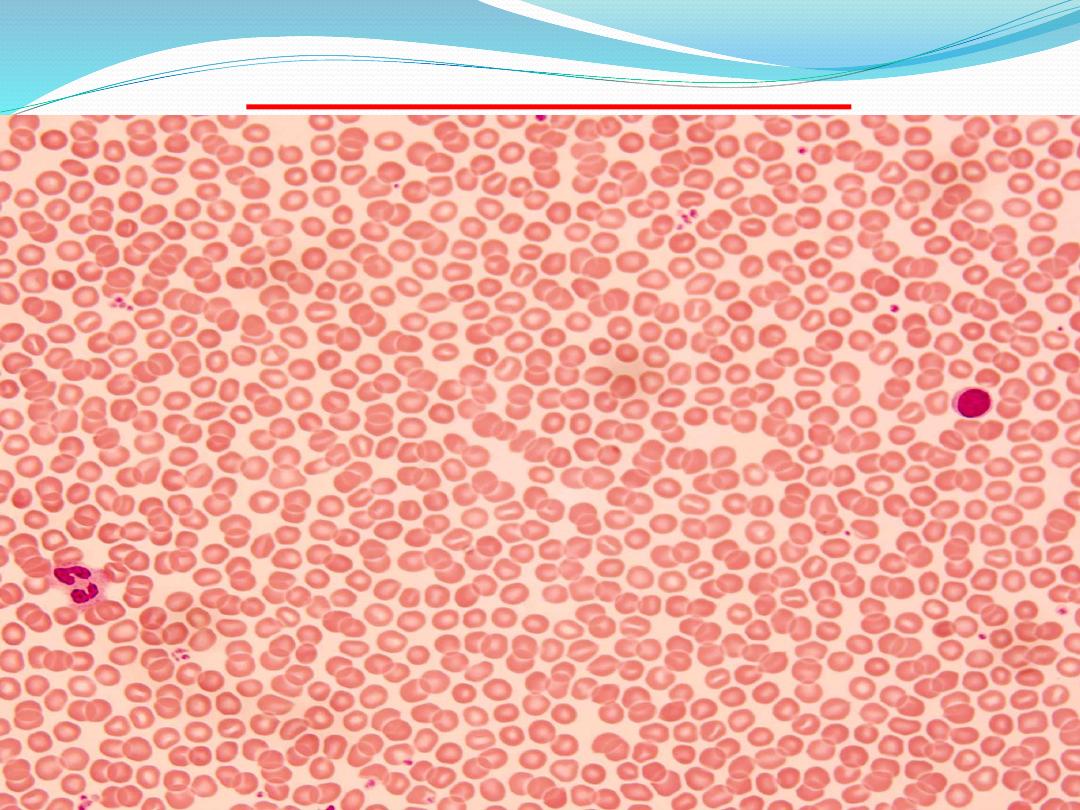
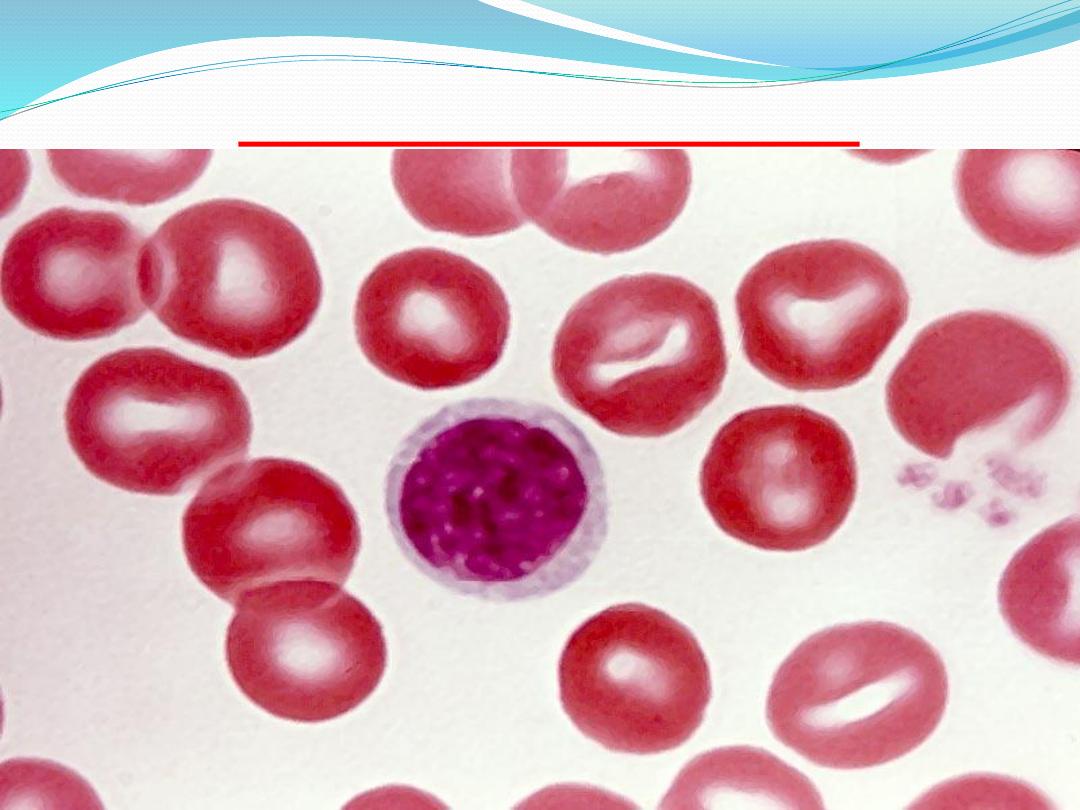
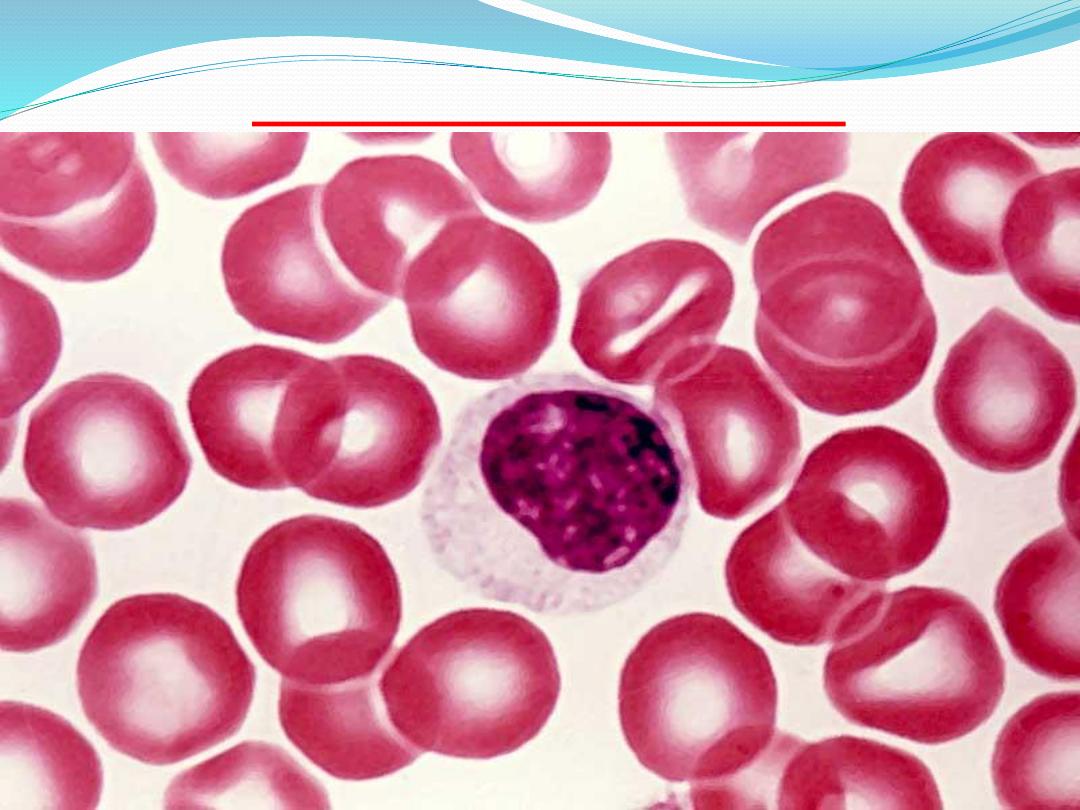
Blood smear - RBC
erythrocytes
RBC
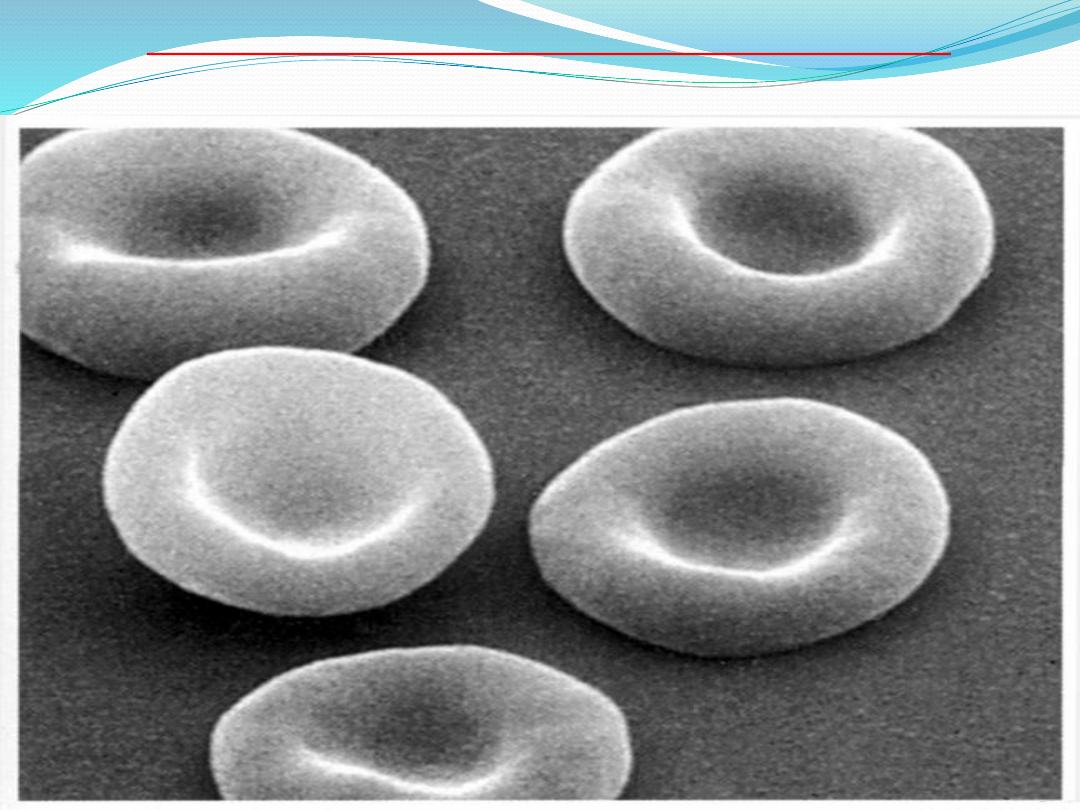
RBCs, scanning electron microscopy
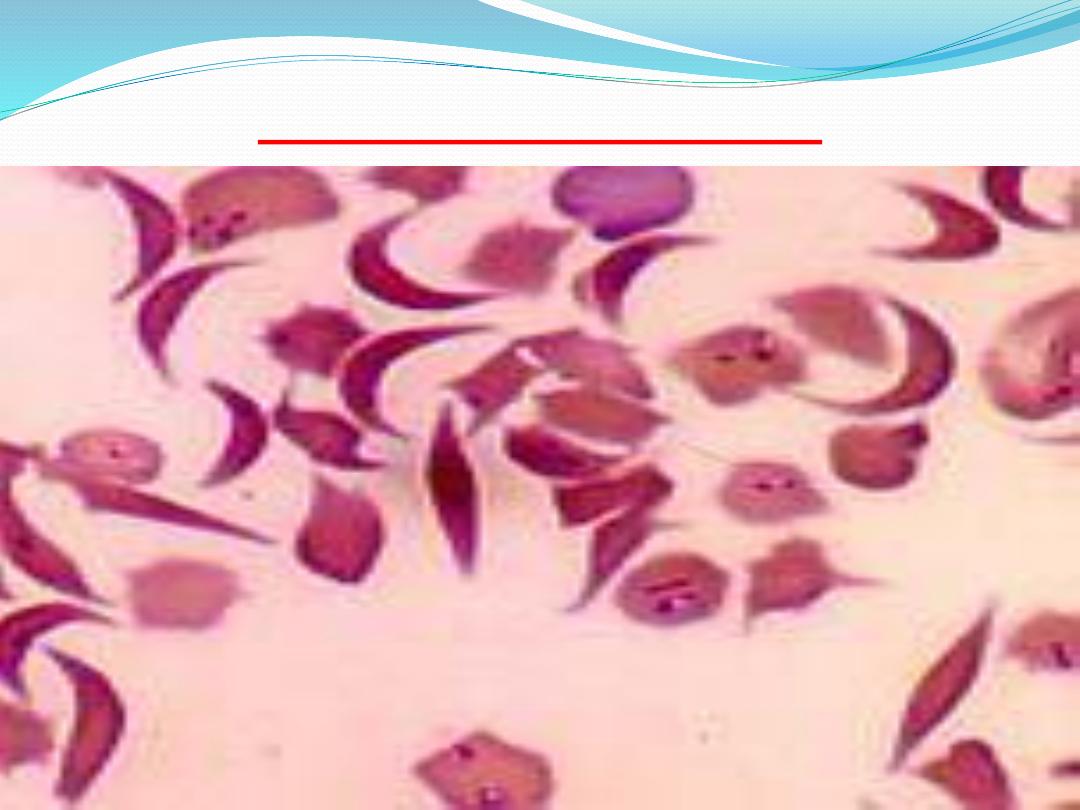
SICKLE CELL ANEMIA
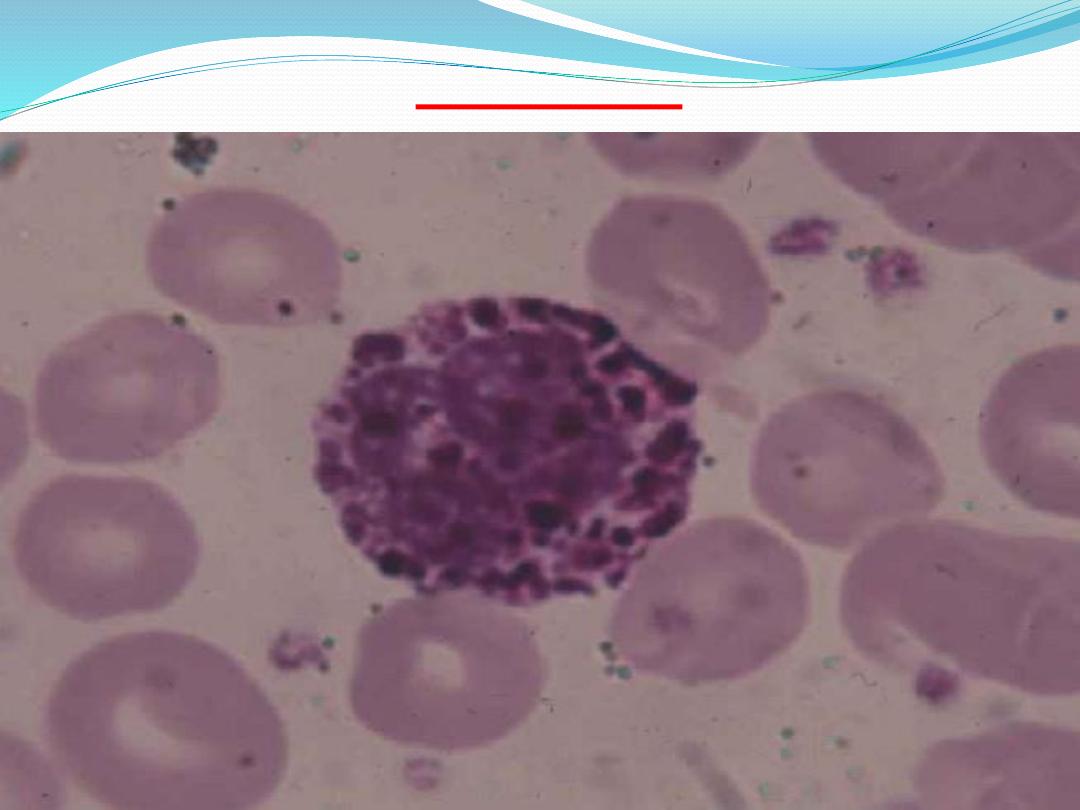
2- platelets
The main function of platelets is to promote blood
clotting.
When the wall and the endothelium of the blood
vessel are damaged, platelets aggregate at the site and
adhere to the damaged wall.
The platelets are activated and form a plug to occlude
the site of damage. The platelets in the plug release
adhesive glycoproteins that increase the plug size,
Cont.
The plug is then reinforced by a polymer fibrin
formed from numerous plasma proteins.
Fibrin forms a mesh around the plug, trapping
other platelets and blood cells to form a blood clot.
After blood clot formation and cessation of
bleeding, the aggregated platelets contribute to clot
retraction, which is later removed through
enzymatic action.
Cont.
platelets are small basophilic fragments,
often appearing in clusters. Small, biconvex disks,
2-3 µm in diameter. Each cubic millimeter of blood
should contain 250,000 to 500,000 of these.
If the number is too high, spontaneous
clotting may occur. If the number is too low,
clotting may not occur when necessary.
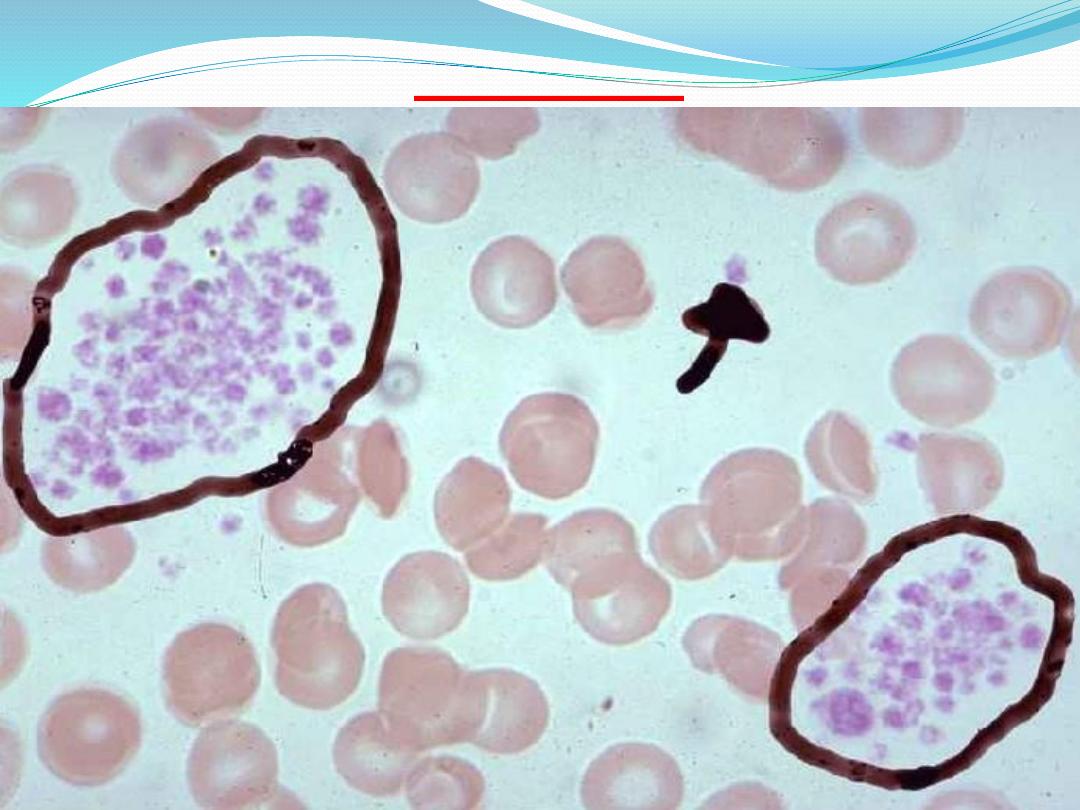
platelets
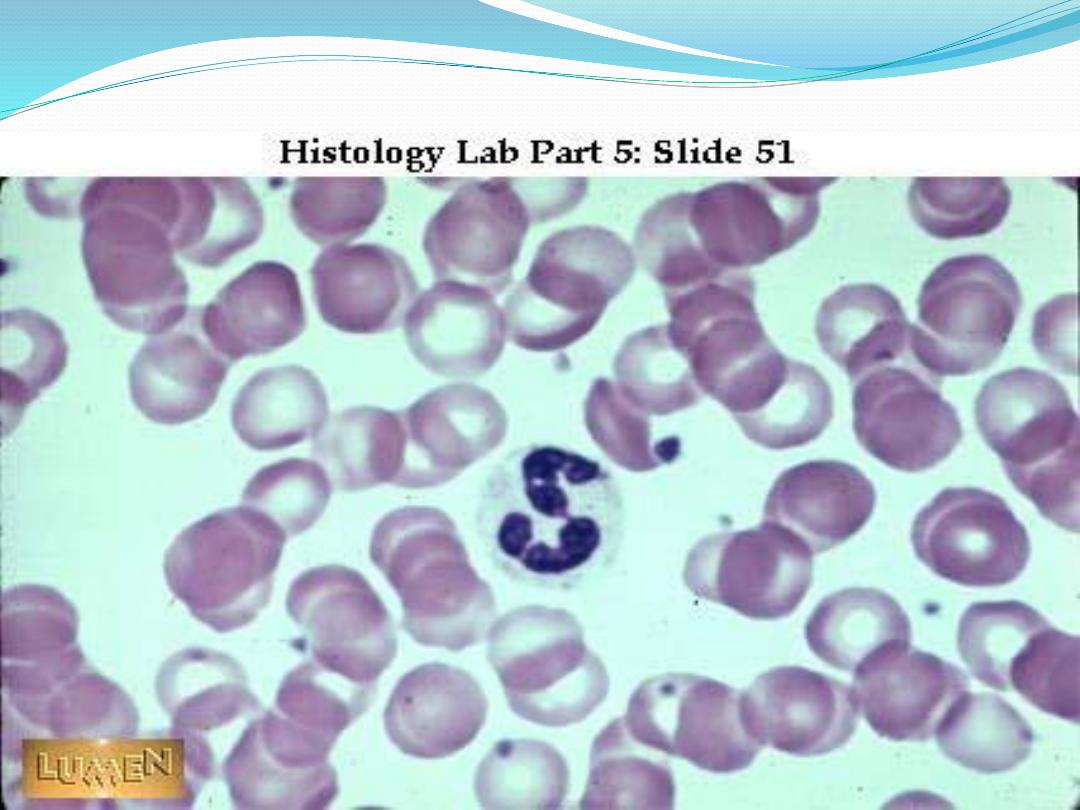
3- leukocytes - granulocytes
a-Neutrophils
have a short life span. They circulate in blood
for about ( 10 hours ) and then enter the connective
tissue, where they survive for another( 2 or 3 days).
Neutrophils are active phagocytes. They are
attracted by chemotactic factors (chemicals)
released by damaged or dead cells, tissues, or
microorganisms, especially bacterial, which they
phagocytose (ingest) and quickly destroy with
their lysosomal enzymes.
Cont.
Nucleus long and multi-lobed (usually 2-4 lobes).
Cytoplasm has small, neutrally stained specific
granules. (fine violet or pink granules,they are
difficult to see with LM ,therefor,the cytoplasm
appear clear.). Normally, neutrophils account for
50-70% of all leukocytes.
If the count exceeds this amount, the cause is
usually due to an acute infection such as
appendicitis, smallpox or rheumatic fever. If the
count is considerably less, it may be due to a viral
infection such as influenza, hepatitis, or rubella.
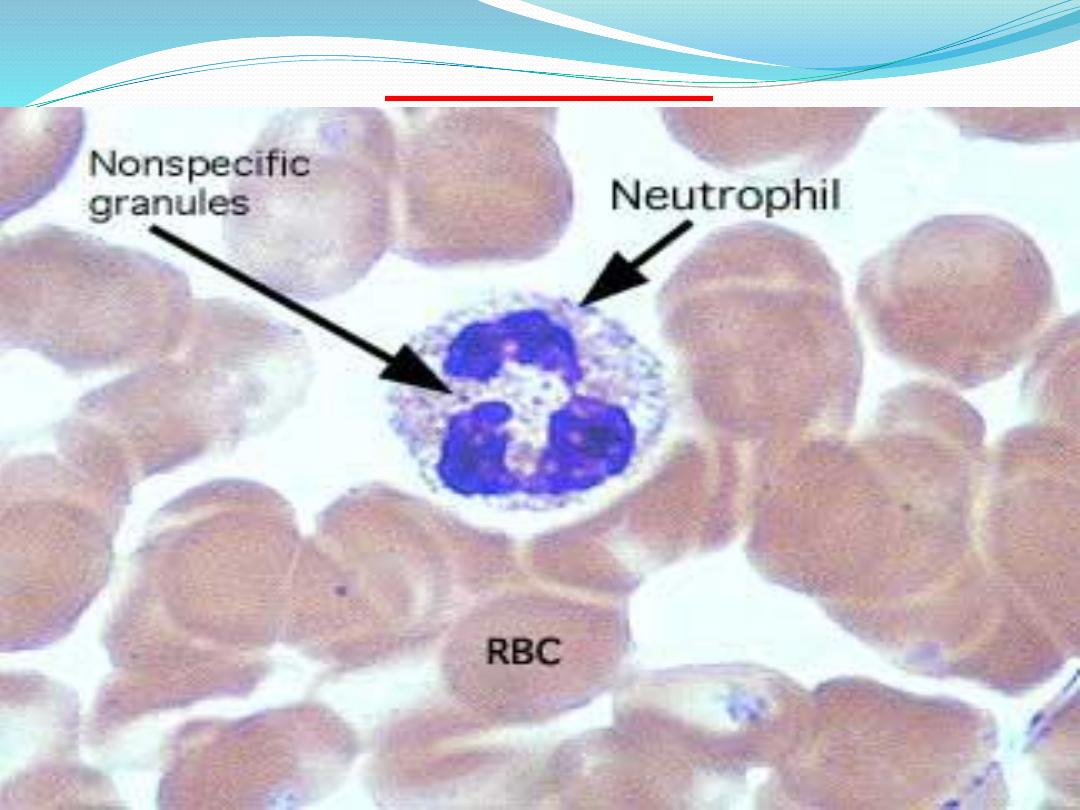
neutrophil
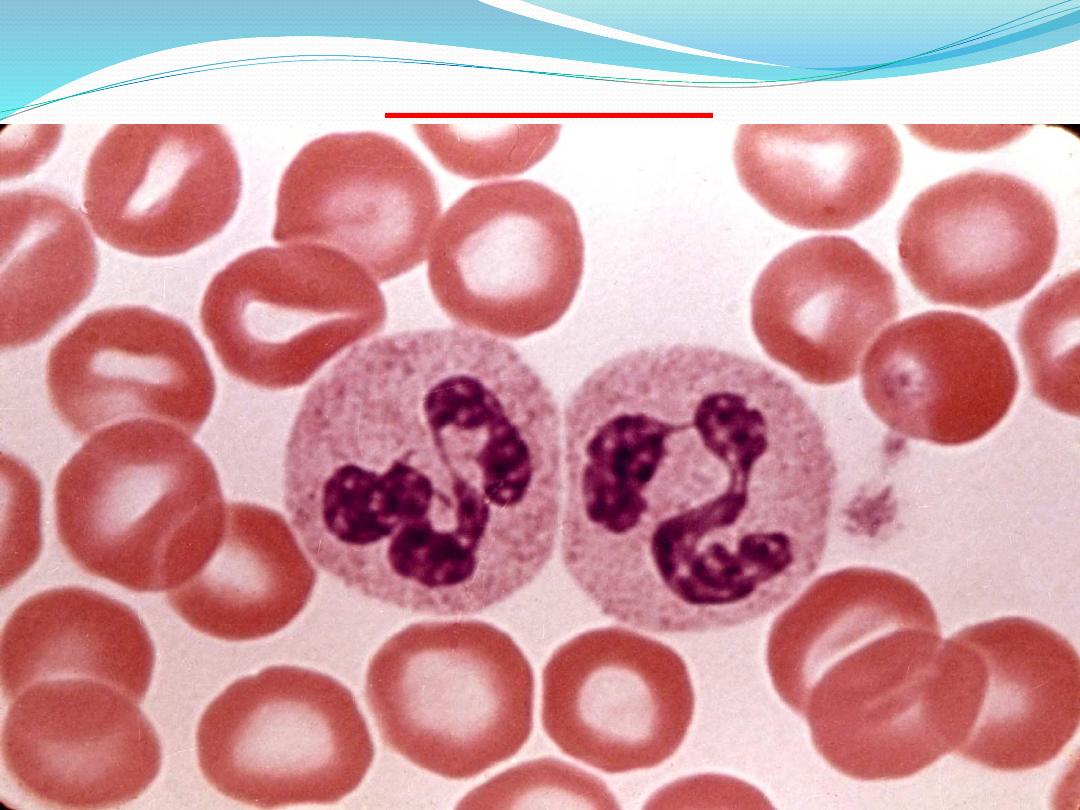
neutrophil
Leukocytes (cont.)
B-Eosinophils
also have a short life span. They remain in blood
for up to( 10 hours) and then migrate into the
connective tissue, where they remain for up to
( 10 days).
Eosinophils are also phagocytic cells with a
particular affinity for antigen–antibody complexes
that are formed in the tissues in allergic conditions.
Cont.
Esonophils have Bilobed nucleus. The
cytoplasm has prominent pink/red specific granules
(stained with eosin dye). If the smear is not stained
properly, the granules may be brownish. These cells
account for less than ( 5% of the WBC's ).
Increases beyond this amount may be due to
parasitic diseases, bronchial asthma or hay fever.
Eosinopenia may occur when the body is severely
stressed.

Esonophil
Esonophil
Cont.
The cells also release chemicals that neutralize
histamine and other mediators related to
inflammatory allergic reactions.
Eosinophils also increase in number during
parasitic infection and defend the organism against
helminthic parasites by destroying them.
Cont.
c-Basophils
have a short life span and their function is
similar to that of mast cells. Their granules contain
histamine(cause vasodilation) and heparin
(anticoagulant ).
Exposure to allergens results in release of
histamine and other chemicals that mediate and
intensify inflammatory responses. These reactions
cause severe allergic reactions, vascular changes
that lead to increased fluid leakage from blood
vessels, and hypersensitivity responses and
anaphylaxis.
Cont.
In a Differential WBC Count we rarely see these
as they represent less than (1% of all leukocytes).
If the count showed an abnormally high number
of these cells, hemolytic anemia or chicken pox
may be the cause.
Basophil
Basophil
Cont.
The nucleus is usually bilobed, but usually is
partially obscured by granules, which can lie over it.
The cytoplasm contains large, purple/black specific
granules (stained with the basic dye) that are larger
but not as numerous as those of eosinophils.
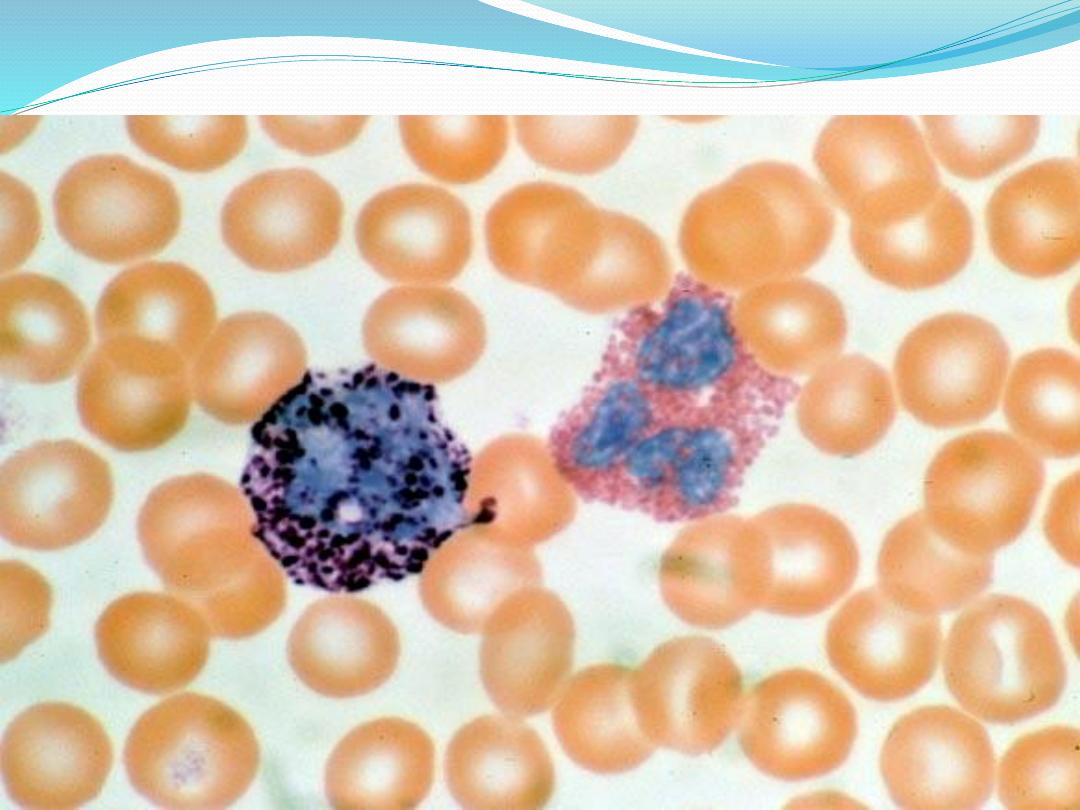
Basophil & esonophil
Leukocytes - agranulocytes
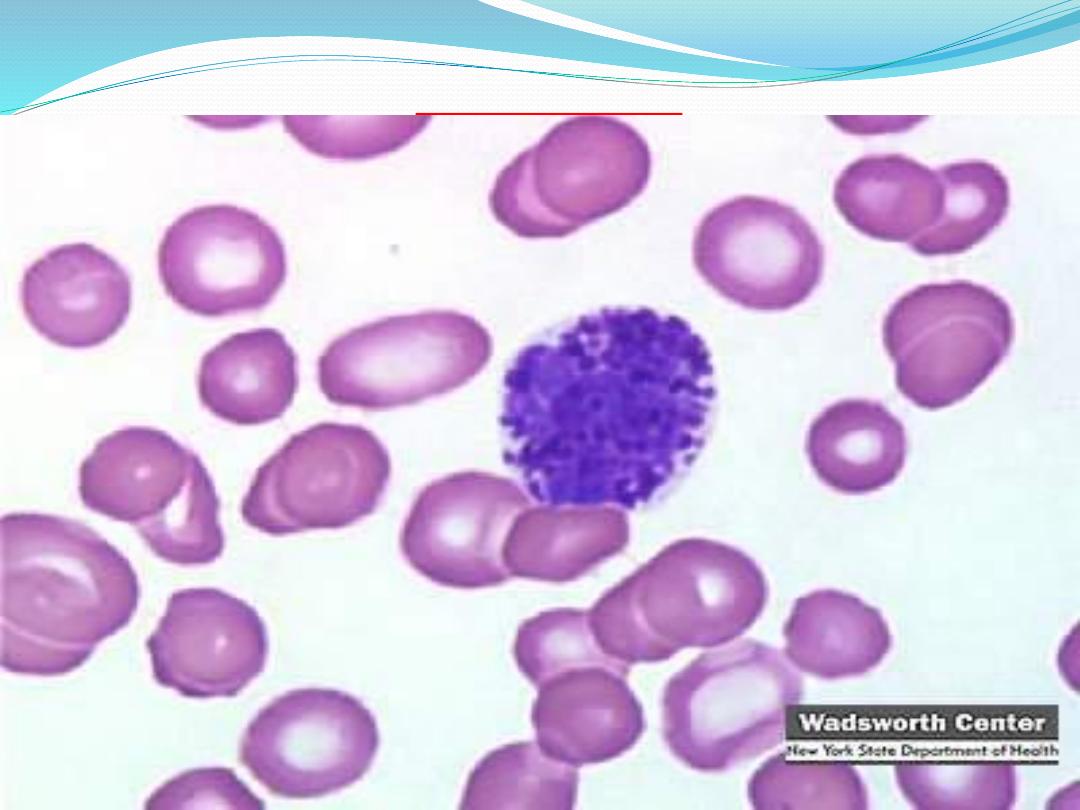
a-Lymphocytes
have a variable life span, from days to months,
and show size variability.
The difference between small and large
lymphocytes has a functional significance. Large
lymphocytes represent the cells that were activated
by specific antigens.
Lymphocytes are essential for immunologic
defense of the organism. Some lymphocytes (B
lymphocytes), when stimulated by specific
antigens, differentiate into plasma cells in the
connective tissue and produce antibodies to
destroy the invading organisms.
Cont.
The nucleus is surrounded by a thin rim of
lightly basophilic cytoplasm in the smaller types.
The cytoplasm is more abundant in the larger
lymphocytes. When the number of these cells
exceeds the normal amount, one would suspect
infectious mononucleosis or a chronic infection.
Patients with AIDS keep a careful watch on their
T-cell level, an indicator of the AIDS virus' activity.
Cont.
Two major subtypes of usually
morphologically indistinguishable lymphocytes can
be identified (by lifespan, function, surface
receptors, site of differentiation) –
T cells and B
cells
. A third type of lymphocyte is referred to as
natural killer (NK) cells
.
Cont.
1-B-lymphocytes
these cells play a central role in humoral or
antibody-mediated immunity. Some divide and
differentiate into plasma cells in tissue. Some are
memory cells. They are immunologically
characterized by immunoglobulin on their cell
membrane.
Cont.
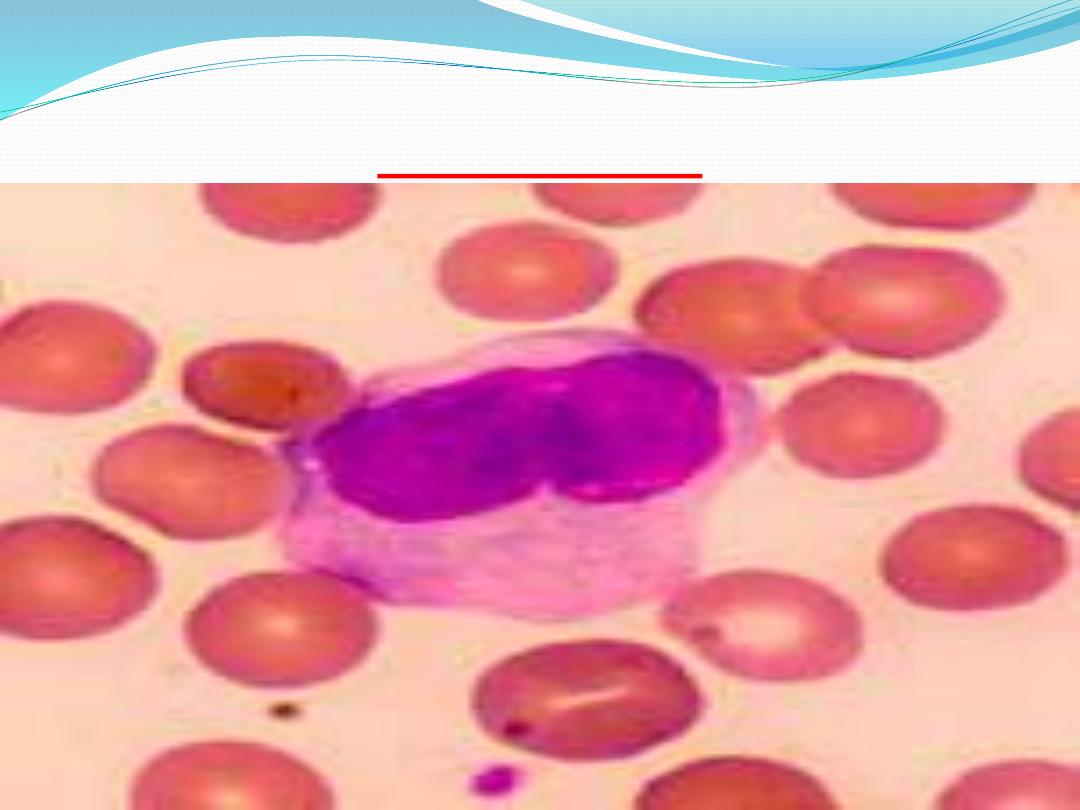
Plasma cells
Derive from B-lymphocytes. They have an
eccentrically placed nucleus, contain abundant
amounts of RER whose cisternae can be filled
with antibody, and have a well-developed Golgi.
Plasma cells produce
antibodies(immunoglobulins
).
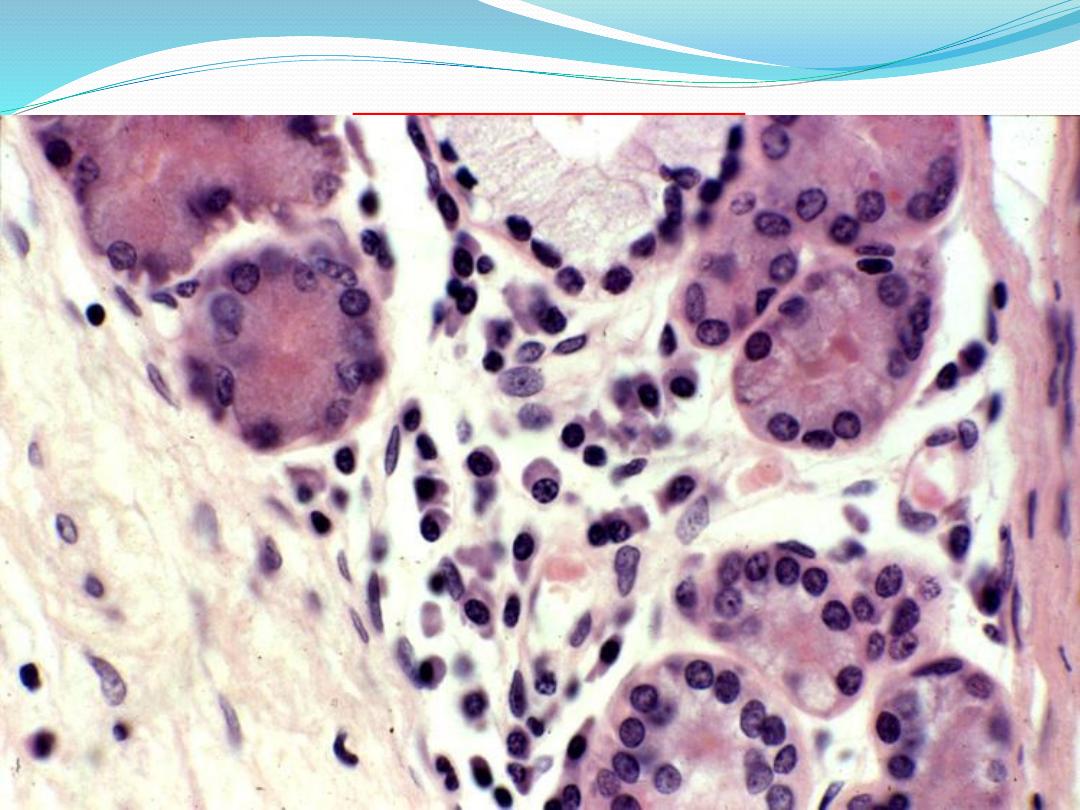
Plasma cells
Cont.
2- T-lymphocytes
Processed by the thymus and participate in
cell-mediated immunity (such as graft rejection).
Some T-cells (cytotoxic) can elaborate cytotoxic
agents. They can make lymphokines (including
interferon, macrophage migration inhibitor factor,
chemotactic factors for basophils). There are also
memory T-cells that survive for years or decades.
Cont.
3- NK cells
NK cells lack the surface antigens of T and B
cells and do not require prior stimulation to
attack virus-infected cells or tumor cells.
Lymphocyte (small)
Lymphocyte (large)
Cont.
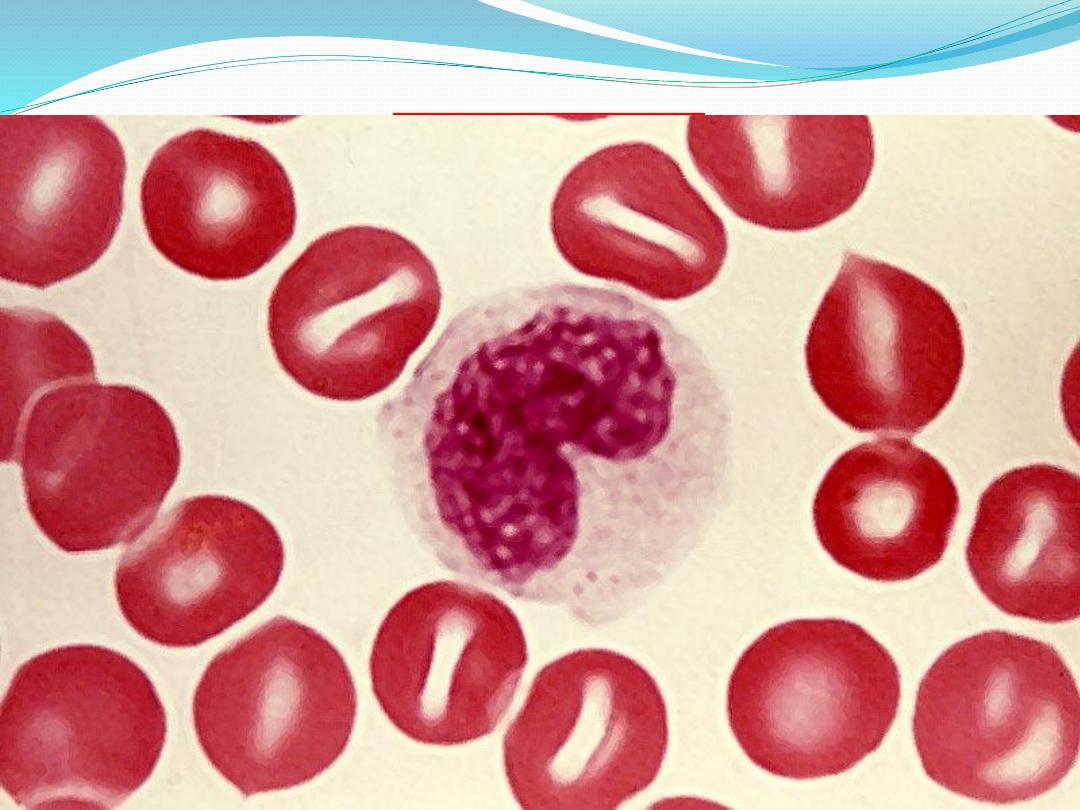
b-Monocytes :
can live in the blood for( 2 to 3 days), after
which they move into the connective tissue, where
they may remain for a few months or longer.
Blood monocytes are precursors of the
mononuclear phagocyte system. After entering the
connective tissue, monocytes become powerful
phagocytes.
At the site of infection, monocytes
differentiate into tissue macrophages and then
destroy bacteria, foreign matter, and cellular debris.
Cont.
They contain a fairly large nucleus which is ovoid,
kidney- or horseshoe-shaped, often located in an
eccentric position. They are the largest cell in the
peripheral blood.
These cells account for ( 3-9% )of all leukocytes. In
people with malaria, endocarditis, typhoid fever,
monocytes increase in number.
MONOCYTE
monocyte

monocyte
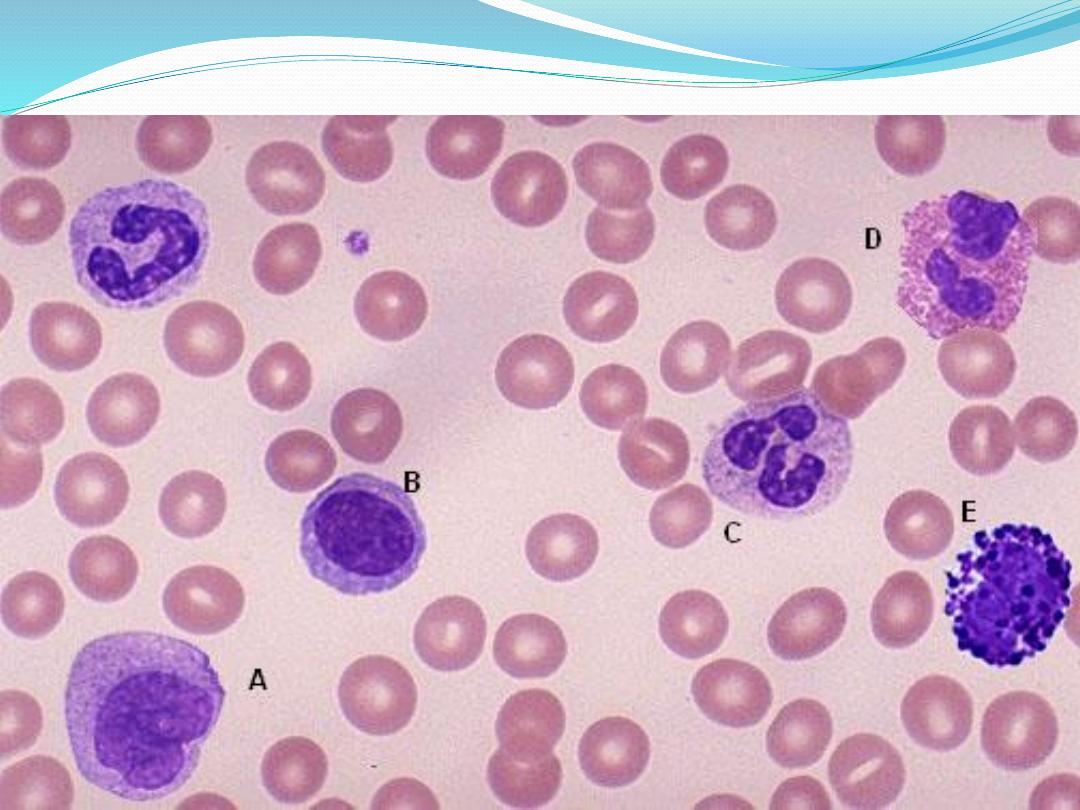
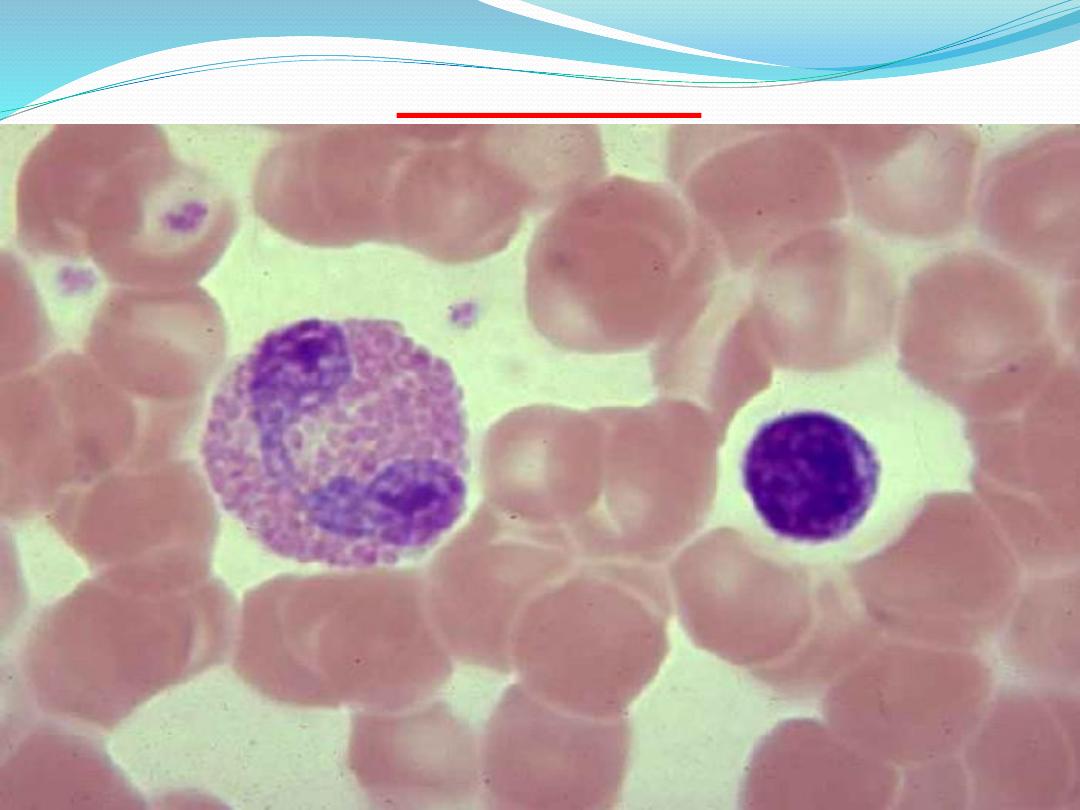
Name the cells below ?
Name the cells ?
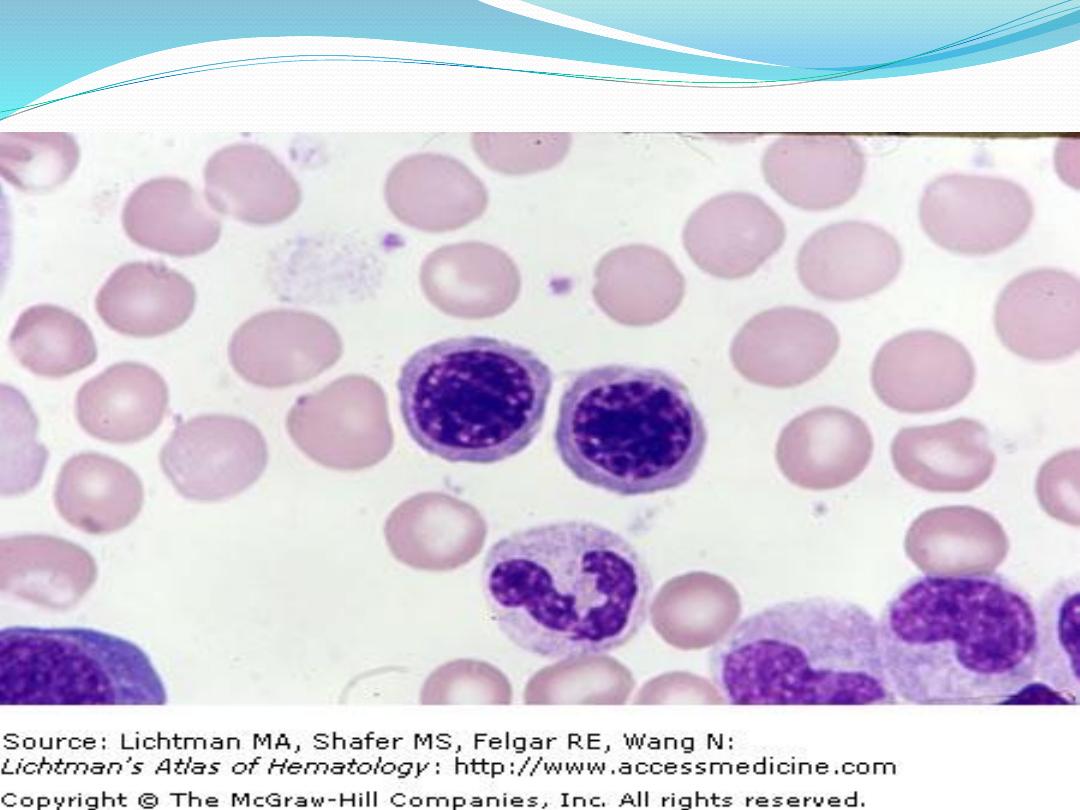
Name the cells ?

Medical Histology
Cell Counts
Cytosis: increased
Leukocytosis, neutrophilia, lymphocytosis,
erythrocytosis
Cytopenia: decreased
Pancytopenia = all
Leukopenia = Low WBC count
Neutropenia = Low neutrophil count
Lymphocytopenia

Thank you
