1
|
P a g e
Bleeding disorders
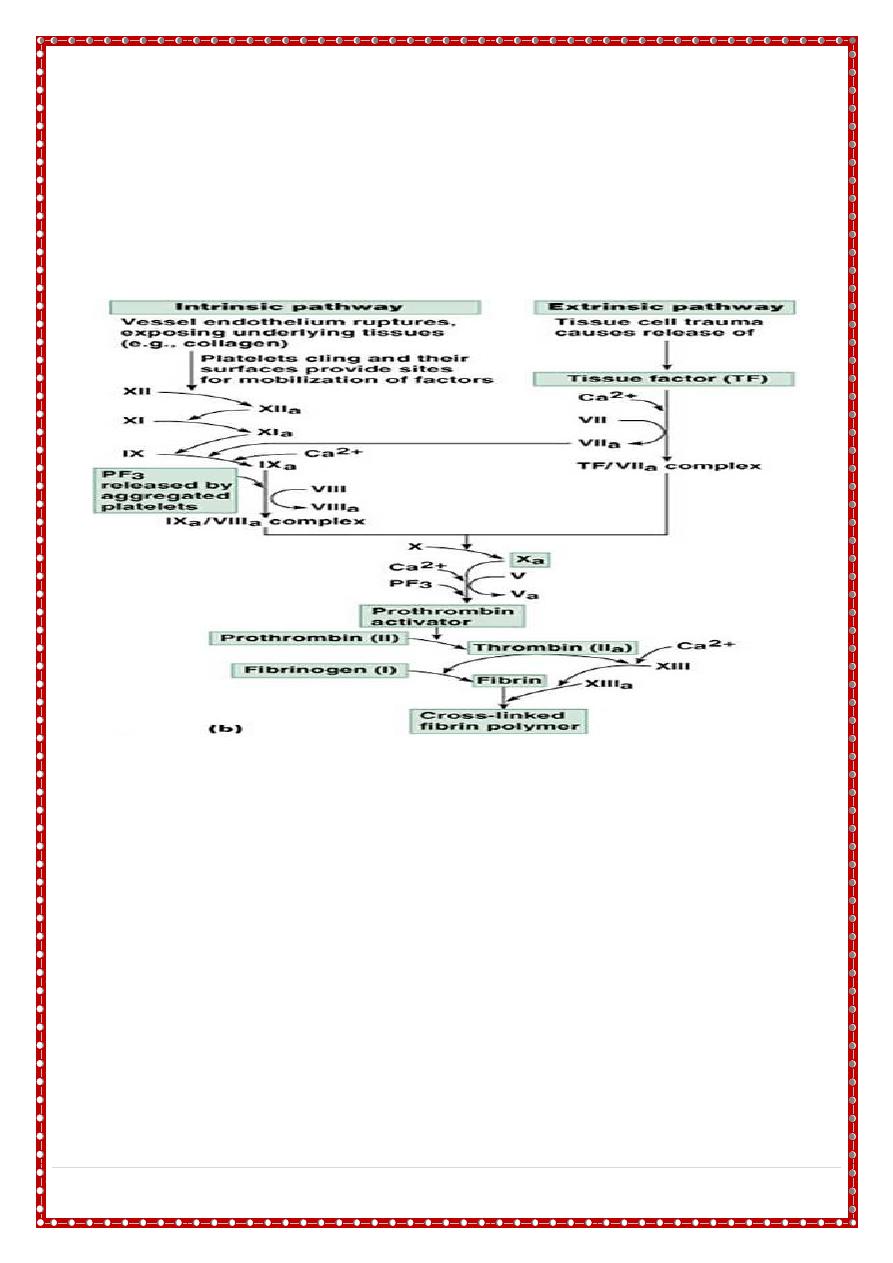
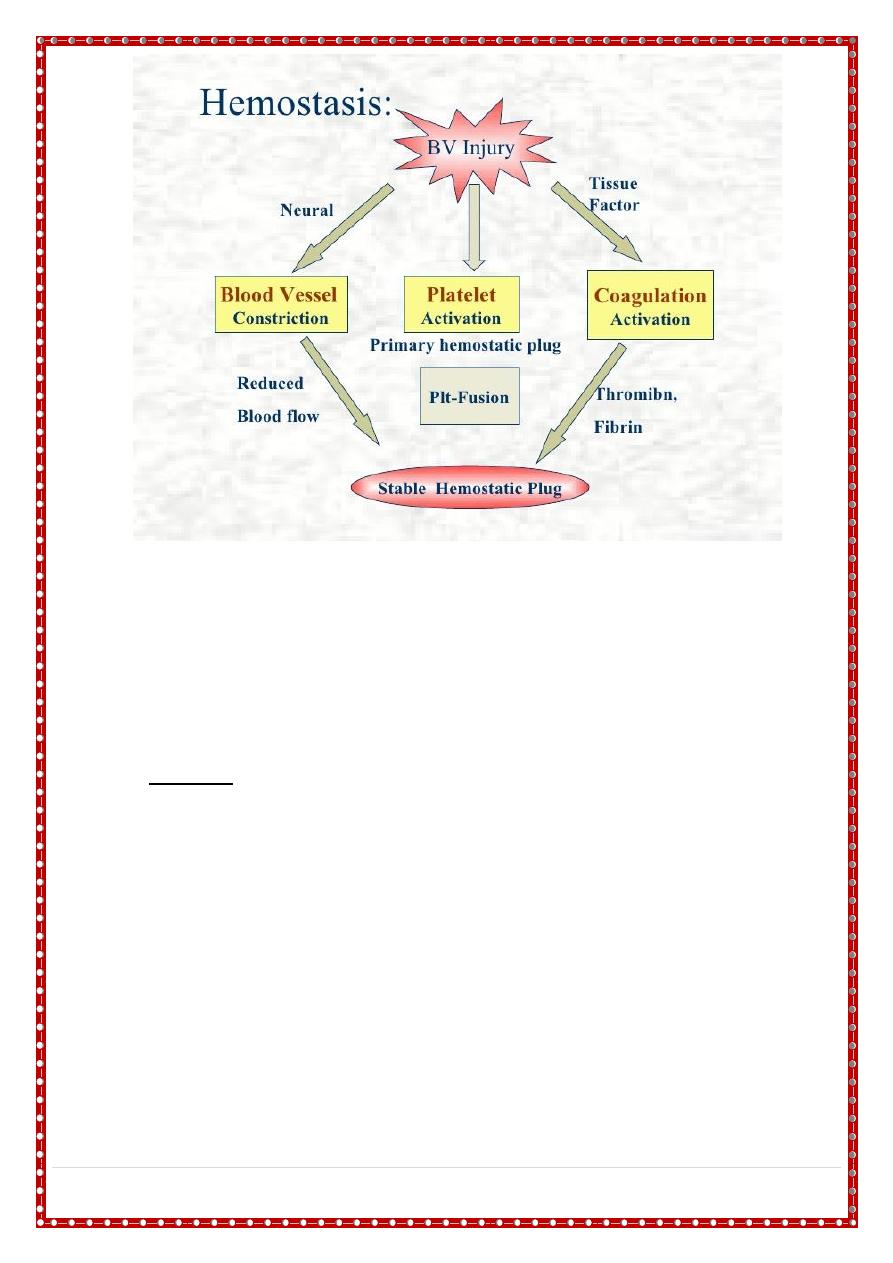
• Haemostasis describes the normal process of blood clotting. It takes place
via a series of complex, tightly regulated interactions involving cellular and
plasma factors
There are five main components:
• Blood vessels - both initiate and limit coagulation. Intact vascular endothelium.
Damaged endothelium).
• Platelets - are vital for haemostasis as they aggregate at sites of vessel injury to form
the primary haemostatic plug which is then stabilised by fibrin.
• Coagulation factors - are produced (mainly by the liver) in an inactive form and are
activated when coagulation is initiated (usually by tissue factor which is released by
vessel injury).
• Coagulation inhibitors - these either circulate in plasma or are bound to endothelium
and are necessary to prevent widespread coagulation throughout the body once
coagulation has been initiated.
• Fibrinolysis - this process limits fibrin deposition at the site of injury due to activity of
the key enzyme plasmin
2
|
P a g e
Initial screening tests
• full blood count and blood film
• (PT) - measures the activity of factors II, V, VII and X
• (APTT) - measures the activity of factors II, V, VIII, IX, X, XI and XII
• if PT or APTT is prolonged,
• Mixing study 50: 50 mix with normal plasma will distinguish between possible
factor deficiency or presence of inhibitor
• thrombin time - deficiency or dysfunction of fibrinogen
• quantitative fibrinogen assay
• biochemical screen including renal and liver function tests
Thrombocytopenia
• severe thrombocytopenia (platelets <20 × 10
9
/L - spontaneous bleeding
• moderate thrombocytopenia (platelets 20-50 × 10
9
/L) - at risk of excess bleeding
during operations or trauma but low risk of spontaneous bleeding
• mild thrombocytopenia (platelets 50-150 × 10
9
/L) - low risk of bleeding during
operations or trauma.
• bruising, petechiae, purpura and mucosal bleeding (e.g. epistaxis, bleeding from
gums ). Major haemorrhage in the form of severe gastrointestinal haemorrhage,
haematuria and intracranial bleeding is much less common.
3
|
P a g e
Causes
• Impaired production: aplastic anemia, bone marrow infilteration, B12 dif.,
osteopetrosis.
• Seqesteration: hypersplenism.
• DIC, Kasabach merritte syndrome.
• Infection.
• Immune thrombocytopenia: ITP, drugs
Idiopathic thrombocytopenic purpura
• is the commonest cause of thrombocytopenia in childhood.
• It has an incidence of around 4 per 100000 children per year.
• It is caused by immune-mediated destruction of circulating platelets due to anti-
platelet autoantibodies.
• The reduced platelet count is accompanied by a compensatory increase of
megakaryocytes in the bone marrow.
Clinical features
• Most children present between the ages of 2-10 years, with onset often 1-2
weeks after a viral infection.
• Affected children develop petechiae and purpura and superficial bruising .
• epistaxis and other mucosal bleeding but profuse bleeding is uncommon despite
the fact that the platelet count often falls to < 10 × 10
9
/L.
• Intracranial bleeding is a serious but rare complication, occurring in 0.1-0.5%,
mainly in those with a long period of severe thrombocytopenia.
•
Asymptomatic
•
Mild
•
Moderate
•
Sever.
Diagnosis
• ITP is a diagnosis of exclusion, so careful attention must be paid to the history,
clinical features and blood film.
• A bone marrow examination should also be performed if
1- atypical clinical features, hepatosplenomegaly or marked lymphadenopathy, (acute
leukaemia or aplastic anaemia)
2- the child is going to be treated with steroids since this treatment may temporarily mask
these diagnoses.
SLE should also be considered.
4
|
P a g e
diagnosis
Differential
• Peripheral
• Bone marrow
Treatment
• 80% of children, the disease is acute, benign and self-limiting, usually remitting
spontaneously within 6-8 weeks.
• Treatment is controversial. Most children do not need any therapy even if their
platelet count is <10 × 10
9
/L
• no therapy for asymptomatic, mild, moderate.
• Immunoglobulin infusions IVIG usually result in a more rapid rise in the platelet
count than steroids 0.8-1 gm/ kg/ day 1-2 day.
• Platelet transfusions are reserved for life-threatening haemorrhage as they raise
the platelet count only for a few hours.
• prednisolone 1-4 mg/kg/ 24hr 2-3 wk or raise no. to> 20x 109/l.
• Anti D infusion for RH +ve 50-75 mcg/kg.
Splenectomy acute LT bleeding
Chronic ITP , age> 4y.
Clotting factors deficiency
• Hereditary
• Haemophilia A, B, C.
• Bleeding may present at birth or in the fetus.
• Easy brusing, hemarthrosis, mouth ulceration, intramascular hematoma.
Lab
• PTT
• Mixing study
• Specific factor assay.
Treatment
• Factor 8
•
Cryoprecipitate
• FFP
