1
ANEMIA
Anemia is defined as a hemoglobin below the 5th percentile of healthy population.
Most studies showed this cutoff point to be around 11 g/dl (-2SD below the mean).
A
A
n
n
a
a
e
e
m
m
i
i
a
a
Reduced production
Hereditary defect (e.g. Thalassaemias)
Acquired problem (e.g. Aplastic Anaemia,
Iron deficiency)
S
S
y
y
s
s
t
t
e
e
m
m
a
a
t
t
i
i
c
c
A
A
p
p
p
p
r
r
o
o
a
a
c
c
h
h
IRON DEFICIENCY & IRON DEFICIENCY ANEMIA
Iron is among the abundant minerals on earth; of the 87 elements in the earth’s crust, Iron
constitutes 5.6% and ranks fourth behind Oxygen (46.4%), Silicon (28.4%) and Aluminum
(8.3%).
In soil, Iron is 100 times more than Ca, Na & Mg and1000 times more than Zinc and 100,000
times more than Iodine.
Iron deficiency is the most common micronutrient deficiency in the world affecting 1.3
billion people i.e. 24% of the world population.
Iron deficiency can range from subclinical state to severe iron deficiency anemia.
I
I
r
r
o
o
n
n
f
f
u
u
n
n
c
c
t
t
i
i
o
o
n
n
s
s
Oxygen carriers
haemoglobin
Oxygen storage
Increased destruction
Hereditary (abnormal red cells):
Membrane defect
Cytoplasmic defect (Hb or enzymes)
Acquired (abnormal environment)
Hypersplenism
AIHA, DIC, HUS
2
Myoglobin
Energy Production
Cytochromes (oxidative phosphorylation)
Krebs cycle enzymes
Other
Liver detoxification (cytochrome p450)
IRON DEFICIENCY ANEMIA
AT RISK GROUPS
Infants.
Under 5 children.
Children of school age.
Women of child bearing age.
ETIOLOGY
1. Inadequate intake of iron & of food, which enhances iron absorption.
2. High intake of inhibitors of iron absorption
3. Hookworm infestation.
4. Blood loss (heavy menses & use of aspirin & NSAID).
5. High fertility rate in women.
6. Low iron stores in newborns.
DIETARY IRON
There are 2 types of iron in the diet; haem iron and non-haem iron
Haem iron is present in Hb containing animal food like meat, liver & spleen
Non-haem iron is obtained from cereals, vegetables & beans
Milk is a poor source of iron, hence breast-fed babies need iron supplements
IRON ABSORPTION
Occurs in the duodenum
1 – 2 mg iron are absorbed each day
(iron in balance 1 – 2 mg iron leaves the body each day)
Taken up as ionic iron or haem iron
Dietary iron usually in excess either not absorbed, or kept in enterocytes and shed into the
gut
Haem iron is not affected by ingestion of other food items. It has constant absorption rate
of 20-30% which is little affected by the iron balance of the subject.
The haem molecule is absorbed intact and the iron is released in the mucosal cells.
3
The absorption of non-haem iron varies greatly from 2% to 100% because it is strongly
influenced by:
1. The iron status of the body
2. The solubility of iron salts
3. Integrity of gut mucosa
4. Presence of absorption inhibitors or facilitators.
IRON ABSORPTION REGULATION
Increased:
Low dietary iron
Low body iron stores
Increased red cell production.
Low haemoglobin.
Low blood oxygen content.
INHIBITORS OF IRON ABSORPTION
Food with polyphenol compounds
Cereals like sorghum & oats
Vegetables such as spinach and spices
Beverages like tea, coffee, cocoa and wine.
A single cup of tea taken with meal reduces iron absorption by up to 11%.
Food containing phytic acid i.e. Bran, cereals like wheat, rice, maize. Legumes like soya
beans, black beans & peas.
Cow’s milk due to its high calcium & casein contents.
PROMOTERS OF IRON ABSORPTION
Foods containing ascorbic acid like citrus fruits, broccoli & other dark green vegetables
because ascorbic acid reduces iron from ferric to ferrous forms, which increases its
absorption.
Foods containing muscle protein enhance iron absorption due to the effect of cysteine
containing peptides released from partially digested meat, which reduces ferric to ferrous
salts and form soluble iron complexes.
Some fruits inhibit the absorption of iron although they are rich in ascorbic acid because of
their high phenol content e.g strawberry banana and melon.
IRON TRANSPORT
Transferrin is the major protein responsible for transporting iron in the body: Transferrin
receptors, located in almost all cells of the body, can bind two molecules of transferrin.
Both transferrin concentration & transferrin receptors are important in assessing iron
status.
Decreased:
Systemic inflammation.
4
STORAGE OF IRON
Tissues with higher requirement for iron ( bone marrow, liver & placenta) contain more
transferrin receptors. Once in tissues, iron is stored as ferritin & hemosiderin compounds,
which are present in the liver, RE cells & bone marrow.
The amount of iron in the storage compartment depends on iron balance (positive or
negative).
Ferritin level reflects amount of stored iron in the body & is important in assessing iron
deficiency
35 – 45 mg / kg iron in adult male body. Total approx 4 g.
Red cell mass as haemoglobin - 50%.
Muscles as myoglobin – 7%
Storage as ferritin in,reticuloendothelial cells, liver - 30%.
bone marrow - 7%
Other Haem proteins - 5%
In Serum - 0.1%
Iron Loss
Physiological Cell loss:
Gut desquamation.
Menstruation (1mg/day).
Pregnancy, lactation.
Stages of iron deficiency:
1. Reduced iron stores
2. Iron deficient erythropoiesis
3. Iron deficient anaemia.
DIAGNOSIS OF IDA
Clinical: symptoms (fatigue, dizziness , palpitations..etc) & signs (pallor, smooth tongue,
Koilonychia, splenomegaly & dysphagia in elderly women).
Laboratory
Stainable iron in bone marrow
Response to iron supplements
LAB FINDINGS IN IDA:
Low iron (poor specificity)
Low ferritin (excellent specificity)
Elevated Transferrin: High iron binding capacity (TIBC).
Low transferrin saturation
Pathological
Bleeding: Gut, menorrhagia, surgery, gross haematuria
5
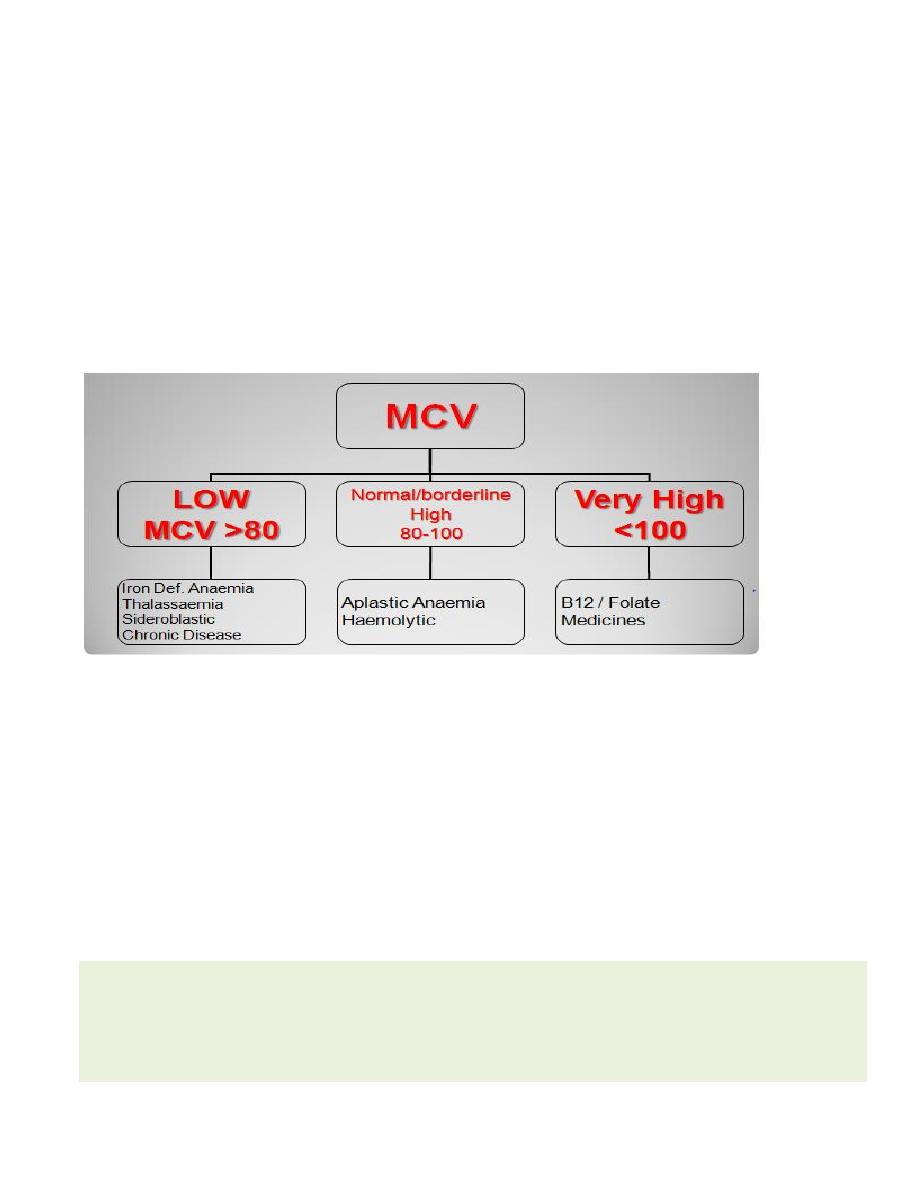
Anaemia: Microcytic hypochromic anaemia(< 11.0 g/dl)
Low MCV, MCH, MCHC. High RDW.
High erythrocyte protoporphyrin
Normal Blood Film Vs MICROCYTES
HYPOCHROMIA
Serum iron is a routine blood test:
Low levels:
Iron deficiency
Other: acute or chronic inflammation; pre-menstrual.
Ferritin – Measurement:
reflects iron stores
Low serum levels: Indicate Iron deficiency (high specificity).
High serum levels:
Iron overload
Tissue release (hepatitis, leukaemia, lymphoma)
Acute phase response (tissue damage, infection, cancer)
CONSEQUENCES OF IRON DEFICIENCY
Increase maternal & fetal mortality.
Increase risk of premature delivery and LBW.
Learning disabilities & delayed psychomotor development.
Reduced work capacity.
Impaired immunity (high risk of infection).
Inability to maintain body temperature.
Associated risk of lead poisoning because of pica.
MANAGEMENT OF IDA:
Blood transfusion if heart failure is eminent.
IV or IM iron in pregnant women.
Oral iron 3-5 mg Fe/kg/day.
Treat underlying cause.
Dietary education
Different iron preparations (salts) contain different amounts of elemental iron.
Fumarate - 33%
Sulfate - 20%
Gluconate - 12%
PREVENTION OF IDA
1. Dietary modification
2. Food fortification
3. Iron supplementation.
High levels:
Iron Overload
Other: pregnancy, recent iron
ingestion.
COMMON PRACTICE
Ferrous sulphate is commonly used in Rx &
prevention of IDA because of good absorption &
high bioavailability, but it has its drawbacks:
GIT disturbances & staining of teeth are frequent
Effects on fortified foods may include: Fat
oxidation & rancidity, Color changes, Metallic
taste, and Precipitation.

6
4. 4.Diet & nutrition education
