1
Pathophysiology
What Is Sickle Cell Disease?
An inherited disease of red blood cells
Affects hemoglobin
Polymerization of hemoglobin leads to a cascade of effects decreasing blood flow
Tissue hypoxia causes acute and chronic damage
Why Do Cells Sickle?
Glutamic acid is substituted for valine
Allowing the polymerization of sickle hemoglobin when deoxygenated
Normal Vs. Sickle Red Cells
Normal
1. Disc-Shaped
2. Deformable
3. Life span of 120 days
Sickle
1. Sickle-Shaped
2. Rigid
3. Lives for 20 days or less
4. Hemolysis and Vaso-occlusion
Vaso-occlusion:
Occurs when the rigid sickle shaped cells fail to move through the small blood vessels,
blocking local blood flow to a microscopic region of tissue. Amplified many times, these
episodes produce tissue hypoxia. The result is pain, and often damage to organs.
Hemolysis and Vaso-occlusion
(continued)
2
Acute Manifestations:
Bacterial Sepsis or meningitis*
Recurrent vaso-occlusive pain (dactylitis, muscoskeletal or abdominal pain)
Splenic Sequestration*
Aplastic Crisis*
Acute Chest Syndrome*
Stroke*
Priapism
Hematuria, including papillary necrosis
Chronic Manifestations:
Anemia
Jaundice
Splenomegaly
Functional asplenia
Cardiomegaly and functional murmurs
Hyposthenuria and enuresis
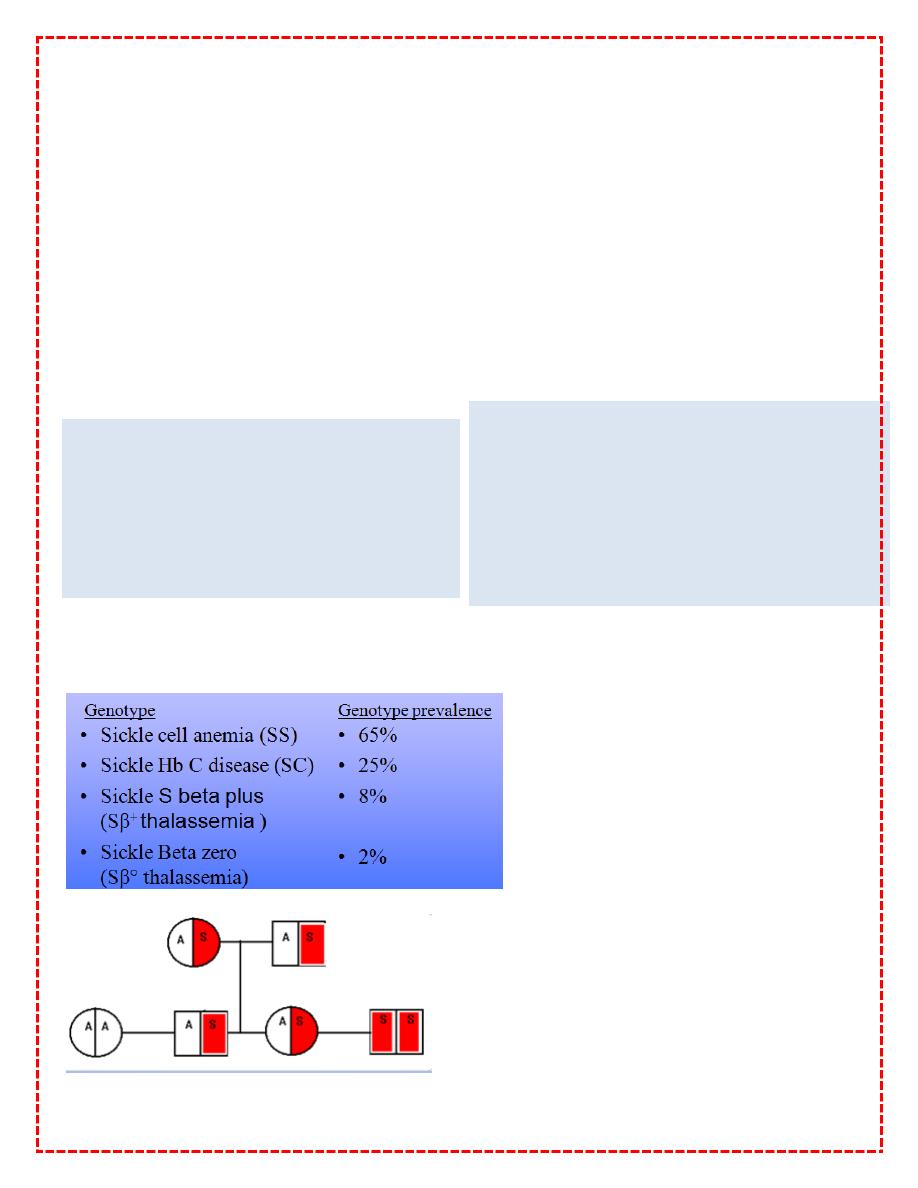
Sickle Cell Disease
SCD Genotype
Sickle Cell Pedigree
Cholelithiasis
Delayed growth and sexual maturation
Restrictive lung disease*
Pulmonary Hypertension*
Avascular necrosis
Proliferative retinopathy
Leg ulcers
Transfusional hemosiderosis*
3
Parents with sickle cell trait: hemoglobin AS
Probability of child with hemoglobin AA: 25%
Probability of child with sickle cell trait AS: 50%
Probability of child with sickle cell disease SS: 25%
Newborn Screening
Diagnosis
abnormal sickle-shaped cells in the blood microscope.
Sickling Testing is performed on a smear of blood using a special low-oxygen preparation.
a sickle prep. Sodium metabisulphite reduces the oxygen tension inducing the typical
sickle-shape RBC.
solubility tests Hb S is quite insoluble when in the reduced state in high phosphate buffer
solution. produce a turbid solution.
hemoglobin electrophoresis.
Health Maintenance
And
Management
Health Maintenance
Physical exam with attention to:
Growth and development, jaundice, liver/spleen size, heart murmur of anemia,
malocclusion from increased bone marrow activity, delayed puberty
Lab evaluations:
CBC with differential and reticulocyte count, urinalysis, renal & liver function
Current Recommendations
Penicillin Prophylaxis: SS, S ºThalassemia
2 months to 3 years: 125 mg PO BID
Over 3 years: 250 mg PO BID
When to discontinue is controversia
Vaccination.
4
Emergencies
1. Fever/infection
2. Acute chest syndrome
3. Eye trauma (hyphema)
4. Priapism
5. Stroke
6. Splenic sequestration
7. Severe pain
Fever and Infection
Fever > 38.5° C (101°F)
is an EMERGENCY
Basic laboratory evaluation:
CBC with differential and reticulocyte count, blood, urine, and throat cultures, urinalysis,
chest x-ray
Indications for hospitalization & IV antibiotics:
-Child appears ill
-Any temperature > 40°C
-Abnormal laboratory values
Start IV antibiotics IMMEDIATELY if child appears ill or temperature > 40°C (DO NOT WAIT
FOR LABS)
Splenic Sequestration
Sudden trapping of blood within the spleen
Usually occurs in infants under 2 years of age with SS
Spleen enlarged on physical exam, may not be associated with fever, pain, respiratory, or
other symptoms
Circulatory collapse and death can occur in less than thirty minutes
Treatments For Splenic Sequestion
Intravenous fluids
Maintain vascular volume
Cautious blood transfusion
Treat anemia, sequestered blood can be released from spleen
Spleen removal or splenectomy
5
Pain Management
Acute pain
Hand-foot syndrome (dactylitis)
Painful episodes: vasoocculsion
Splenic sequestration
Acute chest syndrome
Cholelithiasis
Priapism
Avascular necrosis
Right upper quadrant syndrome
Pain Management
Mild-moderate pain
Acetaminophen
Non-steroidal anti-inflammatory agents (NSAIDs)
-Contraindicated in patients with gastritis/ulcers and renal failure
-Monitor renal function if used chronically
Pain Management
Moderate-severe pain
Opioids are first-line treatment
Morphine sulfate or hydromorphone
Moderate or less severe pain
Acetaminophen or NSAID's in combination with opioids
Other adjuvant medications (sedatives, anxiolytics)
Hand Foot Syndrome - Dactylitis
Early complication of sickle cell disease
6 months to 2 years
Painful swelling of hands and feet
Treatment involves fluids and pain medication
Fevers treated as medical emergency
Genetic Counseling
Glucose-6-phosphate dehydrogenase deficiency
X-linked recessive hereditary disease characterized by abnormally low levels of glucose-6-
phosphate dehydrogenase, a metabolic enzyme involved in the pentose phosphate
6
pathway, especially important in red blood cell metabolism. G6PD deficiency is the most
common.
Signs and symptoms
Most are asymptomatic.
X-linked pattern of inheritance, but female carriers can be clinically affected due to
unfavorablelyonization
Abnormal red blood cell breakdown (hemolysis) in G6PD deficiency
Prolonged neonatal jaundice, possibly leading to kernicterus
Hemolytic crises in response to:
Illness (especially infections)
Certain drugs .
Certain foods, most notably broad beans, Favism
Certain chemicals
Diabetic ketoacidosis
Very severe crises can cause acute renal failure
Trigger drugs
Antimalarial drugs
Sulfonamides m
methylene blue, and naphthalene.
aspirin, phenazopyridine, and acetanilide) nalidixicacid, nitrofurantoin, INH dapsone, and
furazolidone)
Henna .
diagnosis
Complete blood count and reticulocyte count; in active G6PD deficiency, Heinz bodies can
be seen in red blood cells on a blood film, "bite cells”.
Liver enzymes .
Lactate dehydrogenase .
Haptoglobin (decreased in hemolysis);
A "direct antiglobulin test" (Coombs' test) –
Treatment
prevention – a
voidance of the drugs and foods that cause hemolysis.
Vaccination against some common pathogens ( hepatitis A and hepatitis B) may prevent
infection-induced attacks.
In the acute phase of hemolysis, blood transfusions might be necessary, or
even dialysis in acute renal failure.
Some patients may benefit from removal of the spleen (splenectomy0
