Dr..Ziyad
1
Chronic Diarrhea With Failure to Thrive
1.Intractable Diarrhea of Infancy IDI:
Persistent diarrhea after an acute episode of presumed infectious diarrhea is known
as intractable diarrhea of infancy (IDI). in IDI there is weight loss associated with
malabsorption and histologic evidence of enteropathy. IDI should be suspected in
any infant with persistent diarrhea after an acute gastroenteritis. Small bowel
biopsy may reveal patchy villous atrophy and inflammatory infiltrates in epithelial
and lamina propria layers.
Dr..Ziyad
2
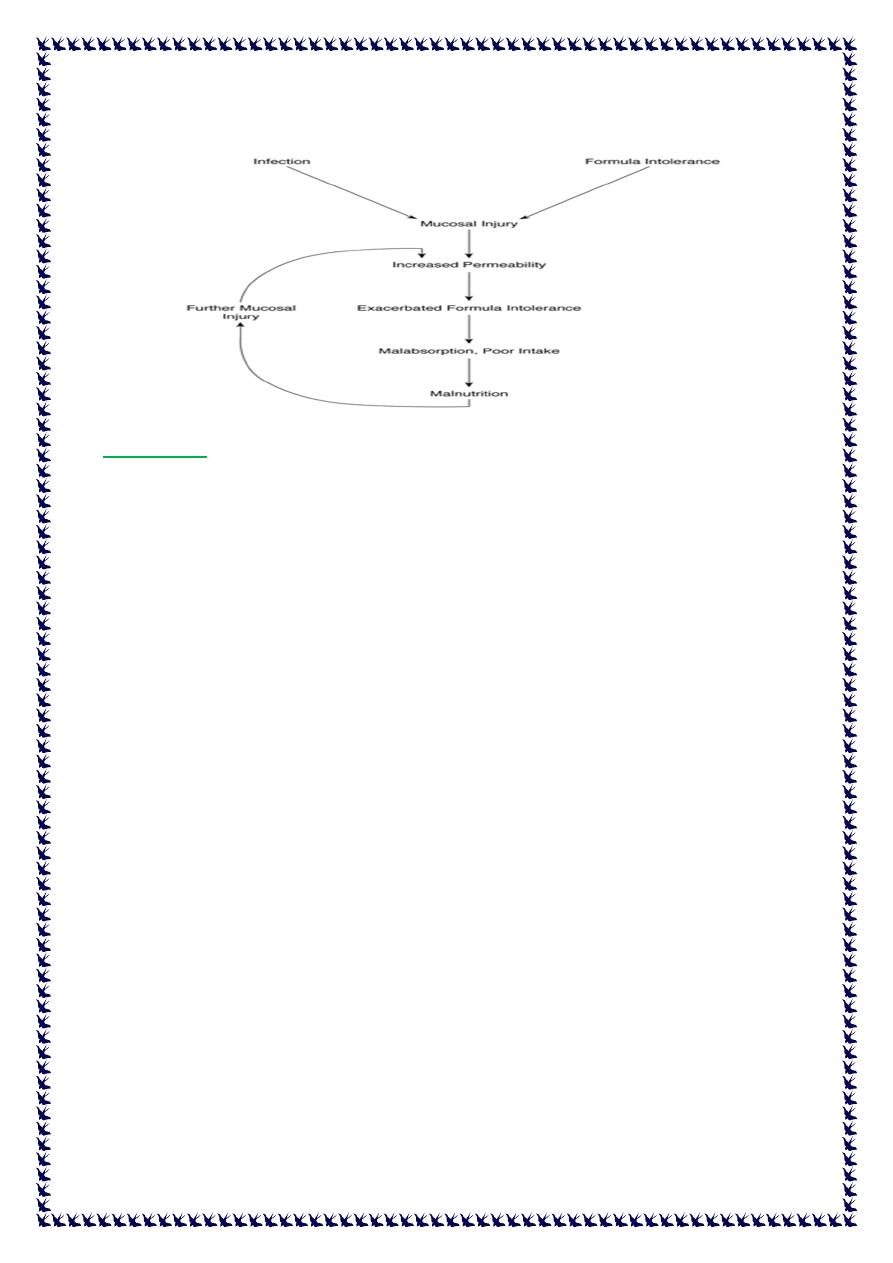
Vicious circle of pathophysiology in intractable diarrhea.
Prevention:
avoiding formula dilution.
promoting early feeding that reduces intestinal permeability and illness duration and
improves nutritional outcomes.
Dietary protein and fat are important in recovery, but simple carbohydrates should be
minimized.
Breastfeeding should continue unless lactose malabsorption is strongly suspected.
Intravenous hydration may be necessary in treating IDI.
Tolerance of enteral feeds and resolution of diarrhea typically occur within 2 to 3 weeks.
2. Allergic Enteropathy
Allergic enteropathy is induced by food proteins with the most common being cow milk
and soy proteins.
associated with failure to thrive, vomiting, and diarrhea.
there is small intestinal mucosal damage resulting in malabsorption of protein,
carbohydrate, and fat.
Protein malabsorption may lead to hypoalbuminemia and diffuse swelling. Profuse
vomiting and diarrhea may lead to severe dehydration, lethargy, and hypotension,
mimicking sepsis in a young infant.
Serum IgE levels may or may not be elevated.
Dr..Ziyad
3
Protein hydrolysate or amino acid-based elemental formulas are necessary if breastfeeding
on a restricted diet is not possible.
Once the inciting dietary protein is removed, the enteropathy will resolve.
3. Celiac disease
is an immune-mediated enteropathy that occurs in the setting of gluten ingestion in a
genetically susceptible individual.
With its prevalence in adults and children approaching 1% worldwide, celiac disease has
become a more commonly diagnosed disorder .
The classic presentation (failure to thrive, diarrhea, and abdominal distension) is being seen
less frequently; Because of family screening, more sensitive and easily accessible testing, and
the recognition of the wide variety of presenting symptoms, identification of patients
presenting with atypical symptoms is on the rise.
Diagnosis should begin with establishing the presence of antiendomysial IgA antibodies,
which have near 100% specificity, or employing newer and less expensive techniques for
measuring enzyme-linked immunosorbent assay-based anti-TTG IgA antibodies.
Diagnosis is confirmed by particular histologic findings in the duodenum, including villous
blunting and prominent intraepithelial lymphocytosis.
Current treatment is with a diet free of wheat, rye, and barley.
New potential therapies are being sought, including the use of gliadin-digesting
recombinant enzymes .
4. Inflammatory Bowel Disease
Approximately 50% to 80% of children with Crohn disease will present with diarrhea, among
other symptoms. In Crohn disease, stool may contain microscopic blood but may not be
grossly bloody, especially in the absence of significant left-sided colonic disease. Diarrhea is
more common in colonic disease and may be absent altogether in cases of isolated small
bowel inflammation.
In ulcerative colitis, diarrhea is a more consistent presenting feature, often insidious in its
development but eventually developing hematochezia.
Dr..Ziyad
4
Nocturnal diarrhea with urgency may be a sign of left-sided colonic inflammation in either
Crohn disease or ulcerative colitis.
Diarrhea associated with IBD typically improves with therapy as mucosal inflammation
resolves.
5. Immunodeficiency States
Children with primary immunodeficiency states often present with chronic diarrhea.
X-linked agammaglobulinemia may result in diarrhea secondary to chronic rotaviral
infections or recurrent giardiasis.
IgA deficiency may lead to recurrent giardiasis and bacterial overgrowth, and is associated
with a 10- to 20-fold increased incidence of celiac disease.
Chronic diarrhea is common also in hyper-IgM and human immunodeficiency virus
syndromes and may be caused by infection with Cryptosporidium parvum in these diseases.
Children with common variable immunodefiency often present with diarrhea and significant
malabsorption along with severe recurrent life-threatening infections during the first
months after birth.
Intractable diarrhea with neonatal insulin-dependent diabetes should raise suspicion for the
syndrome of immune dysregulation, polyendocrinopathy, and enteropathy (autoimmune(
Glycogen storage disease type 1B and chronic granulomatous disease may present very
similarly to Crohn disease, likely related to defective intestinal mucosal immunity.
6. Microvillous Inclusion Disease
rare cause of chronic secretory diarrhea in the neonatal period.
Microvillous inclusion disease is the second most common cause of severe, protracted diarrhea
in the first week after birth, after infectious causes.
presenting with diarrhea so watery that it may be mistaken for urine.
Histology reveals small bowel villous atrophy but without inflammation. Villin substance can be
seen by immunostaining in affected cell cytoplasm, creating the “microvillous inclusions
Aggressive intravenous rehydration and electrolyte replacement are necessary to maintain life
during infancy, followed by lifelong parenteral nutrition in most cases.
Dr..Ziyad
5
7. Autoimmune Enteropathy
Children with autoimmune enteropathy usually develop secretory diarrhea after the first 8
weeks after birth. Another autoimmune disease, such as insulin-dependent diabetes, may be
present in the setting of chronic diarrhea and poor growth.
autoimmuneenteropathy may exist without extraintestinal manifestations.
Diagnosis is made by documenting antienterocyte, anticolonocyte, or antigoblet cell
antibodies in the blood.
Treatment is difficult but may be accomplished with immunosuppressive agents such as
corticosteroids, 6-mercaptopurine, tacrolimus, and infliximab.
8. Neuroendocrine Tumors
These tumors produce symptoms by the systemic effect of their secretory products. The
neuroendocrine tumors produce secretory diarrhea and include vasoactive intestinal
polypeptide-secreting tumor, or VIPoma; Zollinger-Ellison syndrome (ZES); tumors secreting
prostaglandin E2; and carcinoid syndrome.
the classic presentation of VIPoma is with profuse watery diarrhea (usually >20 cc/kg per
day), hypokalemia, and achlorhydria.
Most VIPomas in children are ganglioneuromas or ganglioneuroblastomas, which can be
identified radiographically. Operative resection is imperative but not always curative if the
tumor has metastasized.
9. Hirschsprung Disease
Diarrhea is present in approximately one-third of neonates born with Hirschsprung disease.
The diarrhea usually is a consequence of enterocolitis that occurs in the setting of bacterial
stasis in the lumen.
Children may present with fever, diarrhea, and abdominal distension.
Some children may appear acutely ill with explosive diarrhea, vomiting, rectal bleeding, and
lethargy, whereas others may present with only loose stools and perianal excoriation.
Dr..Ziyad
6
10. Cystic Fibrosis
Diarrhea occurs in CF most commonly as a result of pancreatic insufficiency.
Approximately 90% of patients with CF have pancreatic insufficiency.
Loss of exocrine pancreatic function leads to malabsorption of carbohydrates, fat, and
protein because of dysfunctional amylases, lipases, and proteases, respectively.
Patients with CF also have an increased incidence of small bowel bacterial overgrowth
secondary to altered motility and thickened secretions.
Fecal elastase can be used as a predictor of pancreatic exocrine function, with low levels
indicating possible pancreatic insufficiency. Pancreatic enzyme replacement therapy may
improve malabsorptive diarrhea in patients with CF.
11. Factitious Diarrhea
Laxative ingestion is the most common cause of factitious diarrhea, the ingestion of osmotic
agents may induce diarrhea.
Patients also may dilute stool to create the appearance of diarrhea.
Munchausen by proxy syndrome in which the caregiver creates the child's illness, often
includes factitious diarrhea induced with stimulant laxatives or even by syrup of ipecac
poisoning.
