CHRONIC DIARRHEA
Diarrhea is the reversal of the normal net absorptive status of water and
electrolyte absorption to secretion. It is due to an imbalance in the
physiology of the small and large intestinal processes involved in the
absorption of ions, organic substrates, and thus water.
Diarrhea often is subdivided in terms of pathophysiology.
Osmotic diarrhea,
secretary diarrhea,
motility disturbances
inflammatory processes
In many instances, more than one mechanism is at fault.
Osmotic diarrhea:
is relatively common in children. This term implies that malabsorption of an
absorbable solute creates an osmotic load in the distal small intestine and
colon, resulting in increased fluid losses. This commonly occurs with
carbohydrates. Malabsorption of carbohydrates usually is caused by:
1.
Diffuse mucosal injury:
occurs after viral or bacterial gastroenteritis
2.
Congenital defects
in carbohydrate absorption are relatively rare.
3.
Excess intake of hypertonic juices
by toddlers results in osmotic diarrhea.
In osmotic diarrhea, the diarrhea rapidly ceases when the offending substance
is withdrawn
.
Secretary diarrhea:
is diarrhea that continues even when the patient is not being fed
; it results from
enhanced secretion of water and electrolytes into the lumen relative to the amount of
fluid and electrolytes absorbed.
Pure secretary diarrhea typically does not manifest intestinal inflammation; occult blood and
white blood cells are absent from the stool.
Secretary diarrheas may occur in congenital disorders of fluid and electrolyte metabolism
such as congenital chloridorrhea, mucosal disorders such as microvillus inclusion
disease, and certain tumors such as ganglioneuroblastoma.
Motility disorders:
may cause diarrhea, but they rarely cause malabsorption. The absorptive capacity
of the small intestine is sufficient to absorb most nutrients, even when
transit is rapid. the most common motility-induced diarrhea in the pediatric
age group is irritable colon of infancy or chronic nonspecific diarrhea.
Disorders that result in decreased intestinal motility, such as Hirschsprung
disease, may result in severe bacterial overgrowth in the small intestine,
with mucosal injury and inflammatory diarrhea.
Inflammatory diarrhea:
is relatively common in the pediatric age group, especially associated with acute
diarrheal disorders that are likely to be infectious. Chronic inflammatory
conditions such as ulcerative colitis and Crohn disease also occur in the
pediatric age group.
Exudation of mucus, protein, and blood into the gastrointestinal lumen may
contribute to fecal water, electrolyte, and protein loss.
Inflammatory diarrheas often are accompanied by secretary, osmotic, and even
motility-induced components.
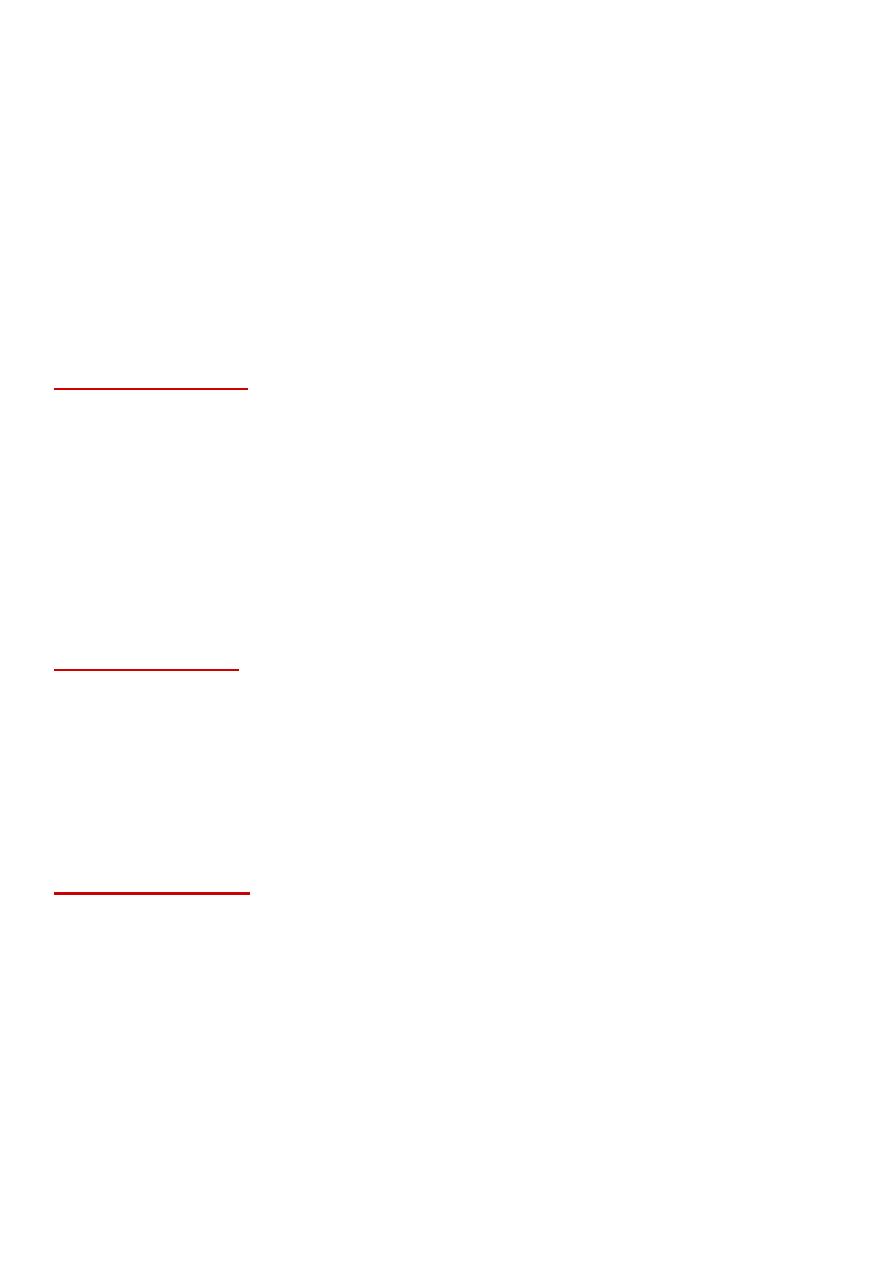
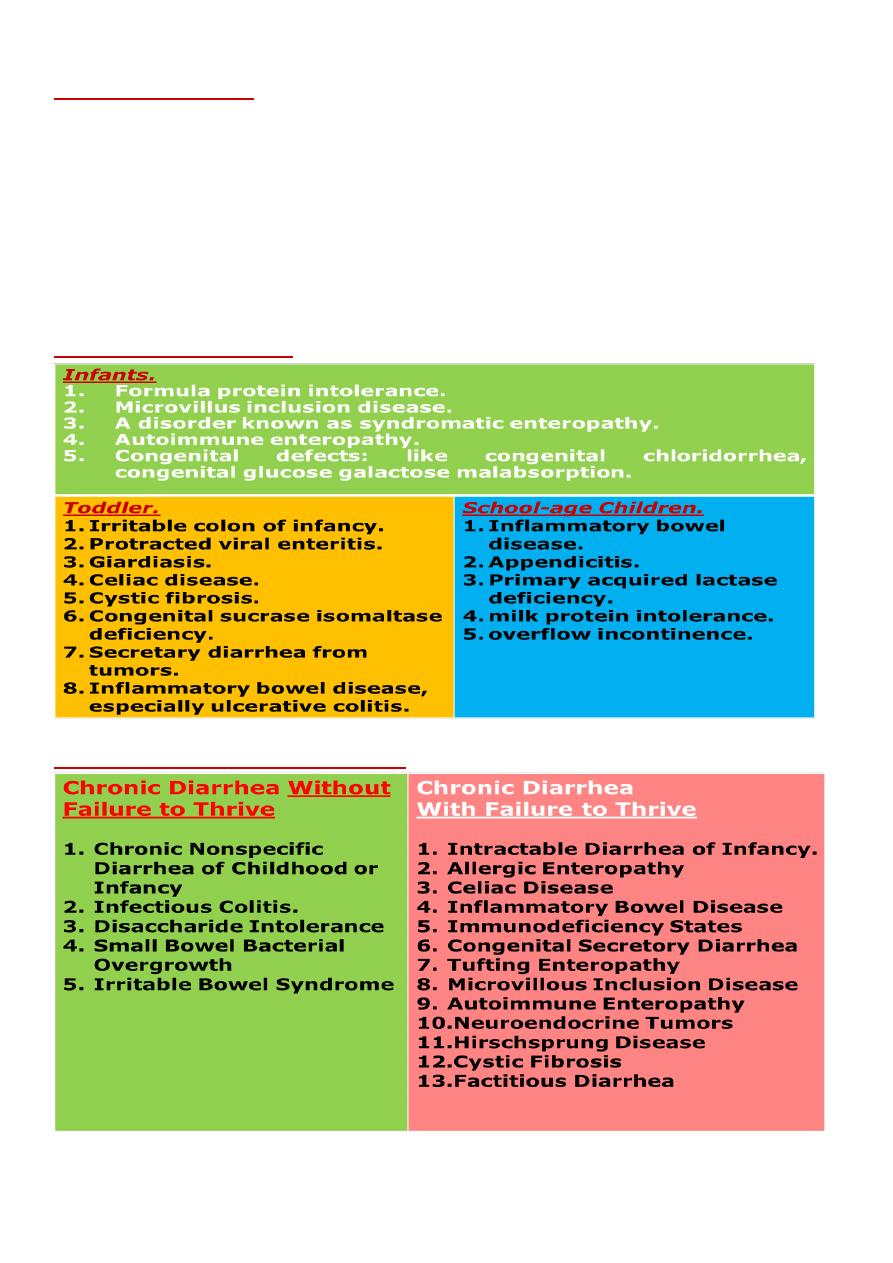
Chronic diarrhea --Causes:
!
Chronic diarrhea –Deferential diagnosis
!

Chronic Nonspecific Diarrhea of Childhood or Infancy CNSD
:
Most common form of persistent diarrhea in the first 3 years after birth.
The typical time of onset may range from 1 to 3 years of age and can last from infancy
until age 5 years.
Affected children may pass 4 to 10 loose bowel movements per day without blood or
mucus.
Patients pass stools only during waking hours
, typically beginning with a large formed
or semiformed stool after awakening. As the day progresses, stools become more
watery and smaller in volume.
Parents frequently describe undigested food remnants in the stool.
Children with CNSD maintain their weights and heights.
Potential pathophysiologic mechanisms for CNSD include increased intestinal motility
and osmotic effects of intraluminal solutes.
Excessive intake of fruit juices, particularly those containing sorbitol or fructose may
contribute to the stool osmotic load, thus causing or worsening diarrhea.
Reassurance is the cornerstone of therapy for CNSD. Parents should be reassured that
their child is growing well and is healthy.
Although no precise treatment for CNSD has been established, dietary intervention
may be prudent. Fruit juice intake should be minimized or changed to types of juice
with low sucrose and fructose loads.
possible helpful changes may be to liberalize fat to encourage normal caloric intake
and to slow intestinal transit time, not to restrict fiber, and to assure adequate but not
overhydration.
Infectious Colitis:
Viruses rarely cause diarrhea lasting more than 14 days.
some pathogenic bacteria and parasites may cause chronic diarrhea.
Nontyphoidal Salmonella organisms.
Yersinia enterocolitica and Y pseudotuberculosis. Escherichia coli, Campylobacter,
Aeromonas, and Plesiomonas.
Enteropathogenic E coli is a leading cause of chronic diarrhea in developing countries.
The protozoa Giardia intestinalis and Cryptosporidium may affect immunocompetent
as well as immunodeficient children and adolescents.
Disaccharide Intolerance
Secondary lactase deficiency results from small intestinal mucosal injury when
lactase enzyme is lost from the tips of the villi. Causes include rotaviral
infection, parasitic infection, celiac disease, Crohn disease, and other
enteropathies.
Incompletely digested lactose reaches the dense colonic microbial population,
which ferments the sugar to hydrogen and other gases, thereby causing
gassy discomfort and flatulence. The nonabsorbed lactose serves as an
osmotic agent, resulting in an osmotic diarrhea. Diagnosis can be made by
a successful lactose-free diet trial of 2 weeks or by hydrogen breath-testing.

Primary acquired lactase deficiency
May present in the school-age child. lactase levels begin to drop between the
ages of 3 and 5 years in children destined to become lactose-intolerant. The
child gradually develops flatulence, abdominal pain, and loose stools
following ingestion of milk. The condition is extremely rare before 5 years
of age and is a more common cause of abdominal pain than diarrhea.
Small Bowel Bacterial Overgrowth
Various conditions such as short bowel syndrome, pseudoobstruction, bowel
strictures, and malnutrition may result in overgrowth of aerobic and
anaerobic bacteria in the small bowel. Symptoms of abdominal pain and
diarrhea arise as bile acids are deconjugated and fatty acids hydroxylated
by bacteria. These processes lead to an osmotic diarrhea.
The diagnosis can be made by an early and late rise in breath hydrogen with
lactulose testing as the undigested lactulose reaches the small bowel and
then the colon.
Treatment is with metronidazole or with nonabsorbable rifaximin
Irritable Bowel Syndrome
The Rome III criteria define IBS as abdominal pain or discomfort at least 3
days per month in the last 3 months associated with two or more of the
following features: improvement with defecation, onset associated with a
change in frequency of stooling, and onset associated with change in the
form of the stool.
These patients do not have rectal bleeding, anemia, weight loss, or fever
Treatment is often challenging. Antispasmodic agents, tricyclic
antidepressants, and selective serotonin-reuptake inhibitors may improve
symptoms.
