Neonatal Sepsis
Neonatal sepsis is a common cause of morbidity and mortality
Neonatal sepsis is a clinical syndrome of systemic illness
accompanied by bacteremia in the first month of life
Early Onset Sepsis (EOS): Culture proven infection within the first 72 hours of life
Late Onset Sepsis (LOS):
Culture proven infection after 72 hours of life
Sepsis, UTI, pneumonia, meningitis, osteomyelitis, NEC
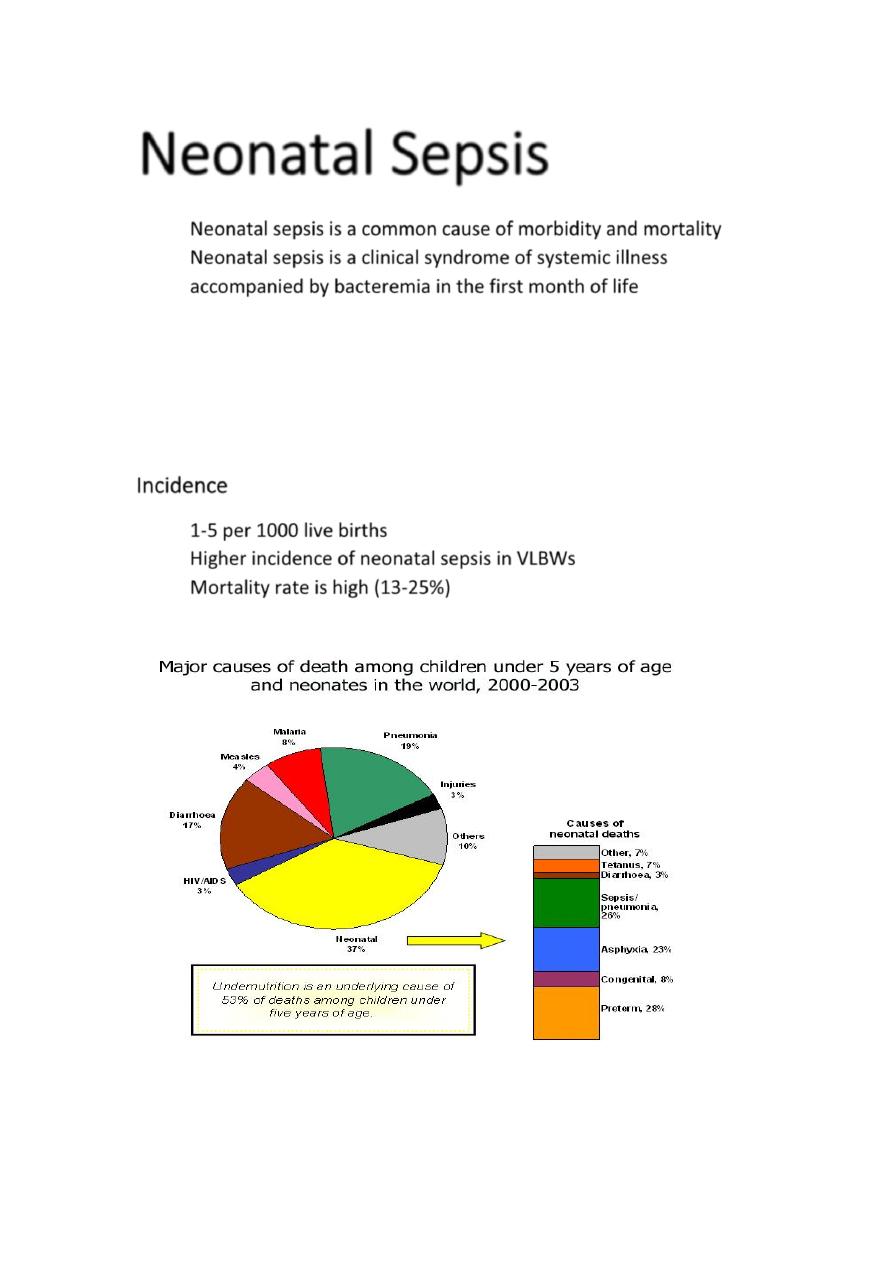
Incidence
1-5 per 1000 live births
Higher incidence of neonatal sepsis in VLBWs
Mortality rate is high (13-25%)
Etiology: EOS
Early Onset Sepsis (EOS):
–
Group B Streptococcus (GBS)
–
E. Coli
–
Listeria monocytogenes
–
Streptococcus species ie. Viridans
Due to maternal or perinatal factors
Etiology: LOS
Late Onset Sepsis (LOS):
–
Coagulase-negative staphylococcus
–
Staphylococcus aureus
–
Gram negative bacilli ie. Klebsiella
–
Candida spp.
Nosocomial or focal infection
Etiology: Viral Sepsis
Congenital
–
Enteroviruses (ie. Coxsackievirus A & B)
–
Herpes Simplex Virus
–
TORCH infections ie. CMV, Toxoplasmosis
–
Acquired
–
HIV
–
Varicella
–
Respiratory syncytial virus
–
Can be either early or late onset sepsis
Risk Factors
Prematurity
Low birthweight
Maternal peripartum fever or infection
Resuscitation at birth
Multiple gestation
Male sex
Clinical Signs and Symptoms
Lethargy
Hypo/hyperthermia
Feeding intolerance
Jaundice
Abdominal distention
Vomiting
Apnea
Differential Diagnosis
Respiratory
Cardiac
CNS
GI
Inborn errors of metabolism
Hematologic
Sepsis Work-Up
Blood cultures
Urine cultures
Lumbar puncture
Tracheal aspirates
CBC with differential
False negative Blood Culture
Maternal antibiotics
Small blood sample
in a prospective study of nearly 300 blood cultures drawn from
critically ill neonates, 55% of culture vials contained less than 0.5
ml of blood
Bacteria load, timing of sampling
Practical points
LP should be done in evaluation of sepsis even with negative
blood culture
Urine culture is not part of work up for EOS
Vesicoureteral reflux was present in 14% of VLBW infants with UTI
Serial CRP
elevated CRP on day 1 and/or day 2, identify most case of sepsis
–
sensitivity (90.2%)
-When CRP is normal on days 1 and 2 ,neonatal sepsis can be
confidently excluded and antibiotic therapy ceased
-negative predictive value (97.7%).
-Sensitivity of serial CRP testing is lower for bacteremia due to gram-
positive than to gram-negative bacteria
-Help in timing of discontinuation of antibiotics when CRP normalize
-Further studies is needed
PCR
–
Sensitivity 96%
–
Specificity 99.4%
–
positive predictive value 88.9%
–
negative predictive value 99.8%
Management : GBS Prophylaxis
All women screened at 35-37 weeks
Intrapartum antibiotics given to:
–
GBS bacteruria during pregnancy
–
GBS positive rectovaginal culture
–
GBS unknown with risk factors
Temp > 37.5
GA < 37 weeks
ROM >18 hours
Empiric Antibiotic Therapy
EOS
–
Penicillin and Aminoglycoside
–
Ampicillin and Gentamicin
–
LOS
–
Vancomycin and Aminoglycoside
–
Vancomycin and Gentamicin
Prognosis
Low birth weight and gram negative infection are associated with
adverse outcomes
Septic meningitis in preterm infants may lead to neurological
disabilities
–
May acquire hydrocephalus or periventricular leukomalacia
What is the major risk factor for neonatal sepsis?
–
A. Maternal GBS colonization
–
B. Male sex
–
C. Prematurity
–
D. ROM >18 hours
–
E. Low birthweight
If meningitis is suspected what antibiotic may be added for better
CNS penetration?
–
A. Vancomycin
–
B. Tobramycin
–
C. Cefotaxime
–
D. Ceftriaxone
–
E. Meropenem
What is the gold standard for diagnosing neonatal sepsis?
–
A. Blood culture
–
B. Lumbar culture
–
C. CBC
–
D. Chest X-ray
–
E. CRP
Of the following, the MOST appropriate antibiotic regimen for this infant
is
A
.
Ampicillin and an aminoglycoside

B
.
Clindamycin and a third-generation cephalosporin
C
.
Meropenem and an aminoglycoside
D
.
Piperacillin and an aminoglycoside
E
.
Vancomycin and a third-generation cephalosporin
You are called to labor and delivery to attend the vaginal delivery of a
37 weeks' gestation male to a 24-year-old primiparous mother. She
reports that her membranes ruptured 36 hours ago. She is afebrile.
Of the following, the maternal condition that is MOST likely to
require antibiotic therapy for this neonate is
A.
Chorioamnionitis
B. Diabetes mellitus
C. Group B streptococcal colonization
D. Preeclampsia
E. Urinary tract infection in the first trimester
