Obstetrics Dr. Aseil
1
MultiplePregnancy
MULTIPLE PREGANCIES any pregnancy in which two or more fetuses exist
simultaneously .
TWINS make up the vast majority (98%) of multiple gestations.
Pregnancies with three or more fetuses (Triplets , Quadruplets) referred
to as ‘higher multiples’.
Risk factors for multiple gestation include:
Reproduction Techniques (Both ovulation induction and in-vitro
fertilization or IVF)
Increasing maternal age
High parity
Black Race
Maternal family history
Incidence
In UK,twins currently account for 1.5% of all pregnancies.
The incidence is increasing due to two overlapping trends , increased maternal
age at conception & increased use of infertility treatments often by older
women
Classification
o
Number of fetuses: twin, triplets,etc.
o
Number of fertilized eggs :zygosity.
o
Number of placentae :chorionicity.
Number of amniotic cavities : amnionicity
Obstetrics Dr. Aseil
2
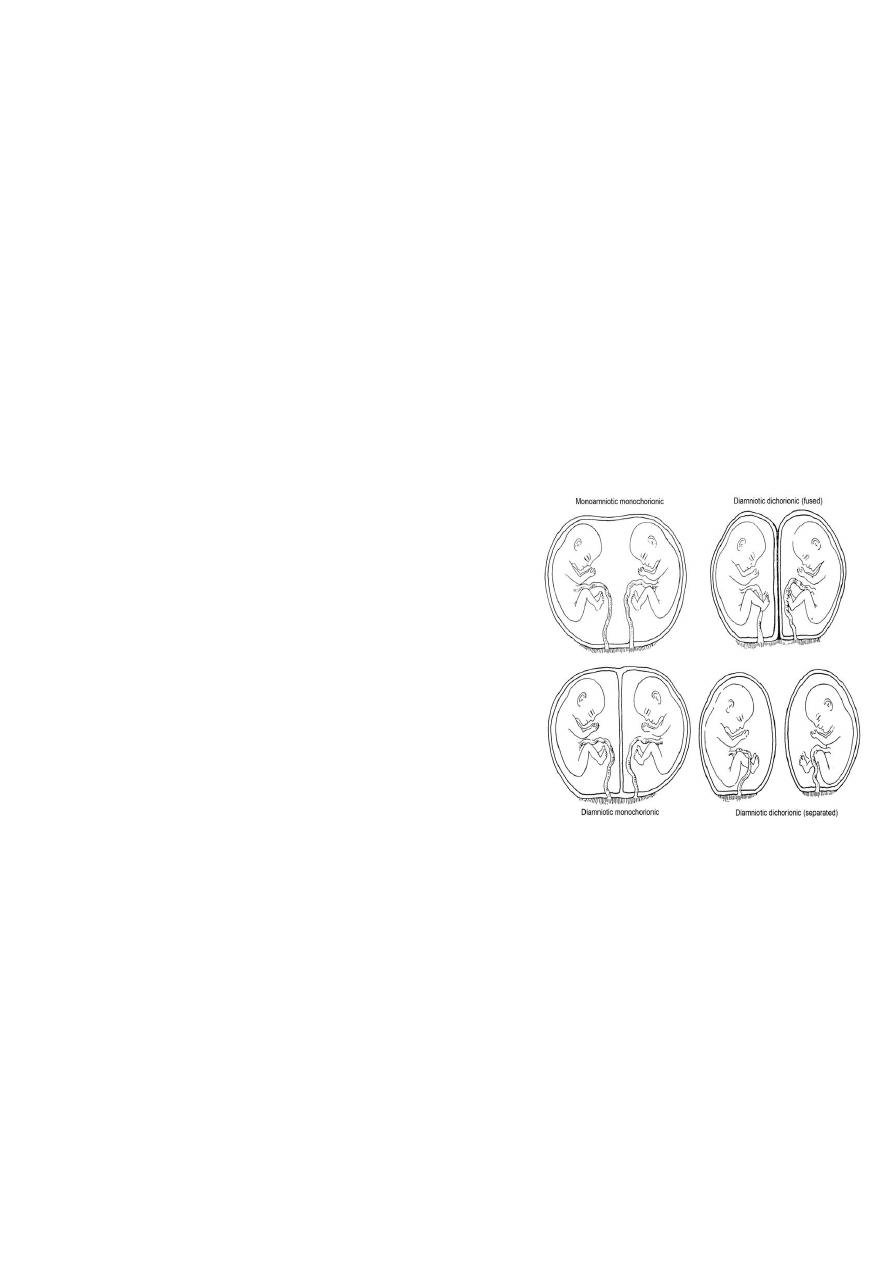
Fraternal Twin(Non-identical)
Fertilization of two separate ova (Dizygotic)
Have 2 functionally separated placentae (Dichorionic)
2 separated amniotic cavities (Diamniotic)
Fetuses either same sex or different
Identical Twins
from single fertilized ovum (monozygotic). single
placenta(monochorionic)or dichorionic
Monochorionic either diamniotic or share a single sac(monoamniotic)
always same sex
Monozygotic twin
(33% of US twins)
Ova division:
< 72 hours: Dichorionic, diamniotic
4-8 days: Monchorionic, diamniotic
9-12 days: Monochorionic, monoamniotic
12 days: conjoined “Siames”twins
Aetiology:
MONOZYGOTIC
• - relatively constant1:250
• - largely independent of race,
heredity, age and parity
• assisted reproductive therapy
DIZYGOTIC
• heredity
• increasing maternal age&parity
• Racial
• infertility therapy
• assisted reproductive therapy
Obstetrics Dr. Aseil
3
Maternal Complication
1- Gestational diabetes.
2-Anemia.
3-Abnormal placentation.
4-Amniotic fluid volume abnormalities.
5-Preeclampsia.
6-Operative vaginal delivery and C-section.
7-Premature rupture of membrane.
8-Postpartum hemorrhage.
9-Umbilical cord prolapse.
10-Hyper emesis gravidarum&pressure symptoms
Complications of twin pregnancy
A_Miscarriage& Severe Preterm Delivery
Average GA at delivery is37w therefore about half of all twins deliver preterm.
In MC twins the chance for birth before viability & severe preterm(24-32)is increased.
B_Perinatal Mortality In Twins
The perinatal mortality rate for twins is around six times higher than for
singletons due to preterm birth.As preterm delivery is most common in
monochorionic , their perinatal mortality secondary to this is twice as high as in
dischorionic twins.
C_Death of one fetus in a twin pregnancy
the intrauterine death of one fetus in a twin pregnancy may be associated with
a poor outcome for the remaining co-twin.In MC ,acute hypotensive episodes,
secondary to placental vascular anastomoses between the two fetuses, result in
haemodynamic volume shifts from the live to the dead fetus.
D_Intrauterine Growth Restriction
The risk of poor growth is higher in each individual twin.The chance of poor fetal
growth for monochorionic twins is almost double that for dichorionic twins
E_Fetal abnormalities
Twins carry twice the risk of the birth of a baby with an anomaly.Each fetus in
MC twin carries 4 times risk of abnormality due to risks of vascular events
during embryonic development.
F_Chromosomal defects
In DZ twins maternal age releated risk of at least 1twin being affected is twice
while for MZ is the same as singleton.

Obstetrics Dr. Aseil
4
Complications Unique To Monochorionic Twinning
Twin-to-twin transfusion syndrome (TTTS).
The donor fetus suffers from both hypovolaema due to blood loss and
hypoxia due to placental insufficiency, and may become growth-restricted
and oliguric.& develops oligohydramnios.
The recipient fetus becomes hypervolaemic, leading to polyuria and
polyhydramnios& cardiac failure.
Diagnosis of Multiple Fetuses
History: risk factors,symtoms.
Examination: Large for date uterus
D.Diagnosis:
Inaccurate menstrual history.
Hydramnios.
Hydatidiform mole.
Elevation of the uterus by distended bladder.
Uterine myomas.
Fetal macrosomia (late in pregnancy).
Antenatal management
_ More frequent antenatal care visits with screening for hypertension and
gestational diabetes as these conditions occur more frequently in twin
pregnancies and there is also a higher risk of other problems (e.g APH,
thromboembolic disease).
_Iron &folic acid supplementation due to increased demand.
Threatened preterm labour
_ Screening& treatment for bacterial vaginosis
_ maternal steroid therapy to enhance fetal lung maturation.
A_Determination of chorionicity
Late 1st trimester US shows V shaped extension of placental tissue into the base
of inter twin membrane(lambda or twin peak sign) in DC
B_Screening for fetal abnormalities
The optimal method of screening twins is by 2nd trimester ultrasound.
Both amniocentesis and chorion villus sampling (CVS)
C_ Monitoring fetal growth & well-being
Ultrasound scan including fetal measurement & BPP.
Doppler assessment of the fetal circulations and CTG.

Obstetrics Dr. Aseil
5
Intrapartum Management
A_Analgesia during labour
Epidural analgesia is recommended.
B_Fetal well-being in labour
FH rate monitoring should be continuous using a speciallized twin monitor.
An abnormal FH rate pattern in twin 1 may be assessed using fetal scalp
sampling.However, a non-reassuring pattern in twin 2 will usually necessitate
delivery by Caesarean section.
The 2nd twin monitord after delivery of 1st, as acute complications such as cord
prolapse and placental separation are well recognized
C_ Vaginal delivery of vertex-vertex
Delivery of the first twin is undertaken in the usual manner
After the delivery of the first twin, abdominal palpitation should be performed
to assess the lie of the second twin.
If the lie is longitudinal with a cephalic presentation, one should wait until the
head is descending and then perform amniotomy with a contraction. If
contractions do not ensue within 5-10 minutes after delivery of the first twin, an
oxytocin infusion should be started.
Delivery of vertex-non-vertex
IF 2nd twin was breech ARM done once breech is fixed.
Breech extraction done if fetal distress occur or if footling .
if 2nd twin was transverse , external cephalic version can be done & if failed
internal podalic version followed by breech extraction.
Non-vertex first twin
When twin 1 presentation as a breech, clinicians usually recommend delivery by
elective C/S because of increase risk associated with breech vaginal delivary.
and the rarely seen phenomenon of ‘locked twins’.
