Obstetrics Lec 15 Dr. Aseil
1
PPH
DEFINTION
Postpartum Hemorrhage: bleeding from genital tract in excess of 500 ml after
delivery. Types:-
*Primary pph occur within first 24 h
* Secondary pph occur between24h and 6-12w postpartum
ASSESSMENT OF BLOOD LOSS AFTER DELIVERY
Difficult, mostly visual & subjective.
For this reason it is more important to take into account any blood loss
that causes a haemodynamic change
As the risk of dying from pph depend not only on the amount and rate of
blood loss but also on the health of women.
Physiology of 3
rd
stage
Once the baby is born myometrial contraction is the main driving force for
placental separation &blood v.constriction .This hamostatic mechanism is
known as
Physiological suture or livinig ligature.
If the uterus does not contract normally, the blood vessels at the placental
site stay open & hemorrhage results.
Because the estimated blood flow to the uterus is 500 – 800 ml/min at
term a severe postpartum hemorrhage can happen within just a few
minutes.
Etiology of PPH
The causes of postpartum hemorrhage can be thought of as the four Ts:
tone,
tissue,
trauma,
thrombin

Obstetrics Lec 15 Dr. Aseil
2
Tone
Uterine atony
Multiple gestation , polyhydramnios
high parity,
prolonged labor
chorioamnionitis,
augmented, instrumental delivery
Tissue
1-Retained uterine contents
Placenta &products of conception,
blood clots
2-Placental abnormalities
Location : Placenta previa
Attachment : Accreta (Leiomyoa, previous surgery)
Peripartum : Placental abruption
Trauma
Lacerations and trauma
Planned: Cesarean section, episiotomy
Unplanned: Vaginal/cervical tear, Uterine rupture, Haematoma
Thrombin
Coagulation disorders
Congenital: Von Willebrand's disease
Acquired: DIC(AP,IUD,PET,AFE) , Heparin, Massive transfusion
PREVENTION
Regular ANC
Correction of anaemia
Identification of high risk cases,who should deliver
in hospital with facility for Emergency Obstetric Care.
ACTIVE MANAGEMENT OF 3
RD
STAGE :-
Obstetrics Lec 15 Dr. Aseil
3
• Placenta delivered by controlled cord traction (CCT) with counter-traction to
the fundus.
• Fundal massage.
Prophylactic oxytocics should be offered routinely in the management of the
third stage of labour
Oxytocin 5 u iv, 10 u im
Syentometrin (5 u syentocinon+0.5 mg ergometrin)
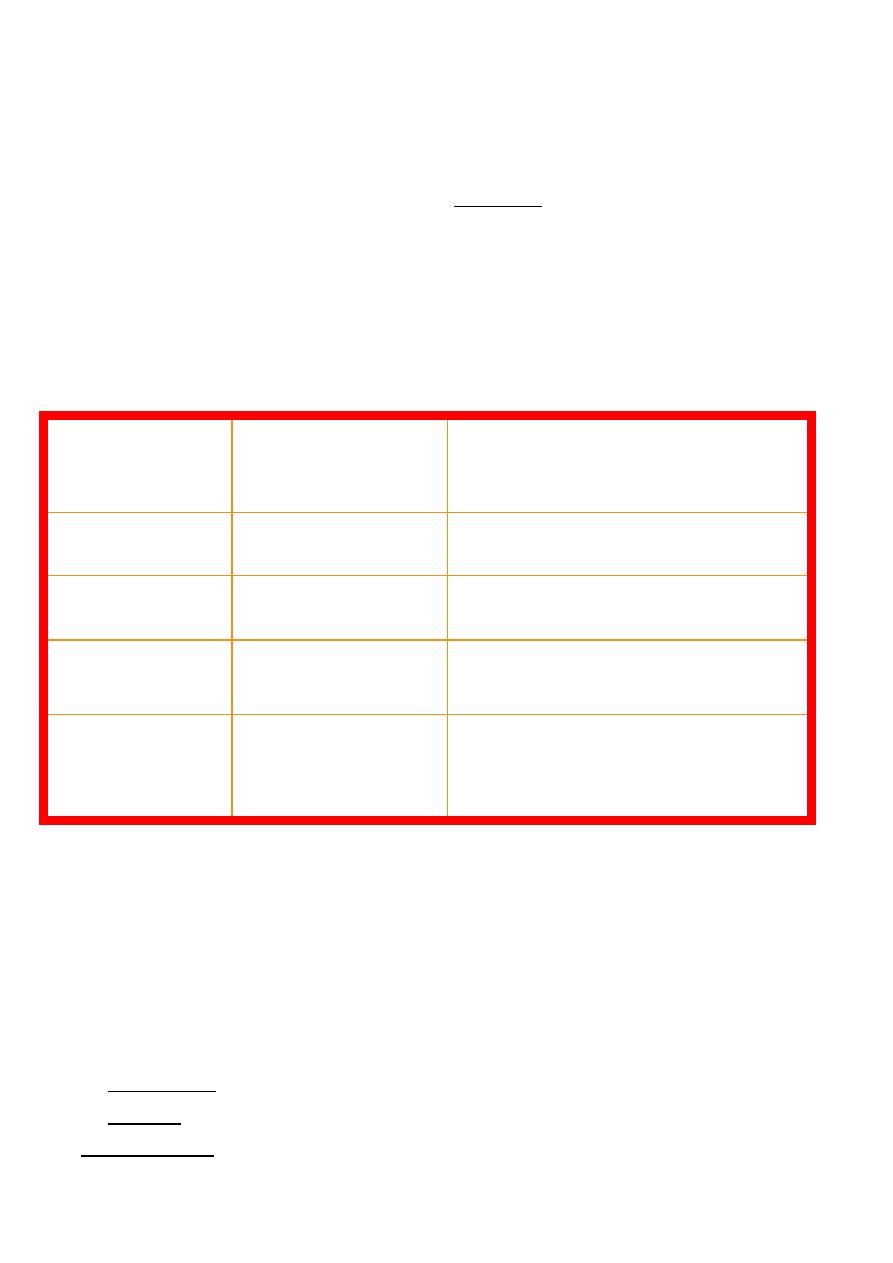
SYMPTOMS & SIGNS
Blood loss
(% B Vol)
Systolic BP
(mm of Hg)
Signs & Symptoms
10-15
Normal
postural hypotension
15-30
slight fall
PR, thirst, weakness
30-40
60-80
pallor,oliguria, confusion
40+
40-60
anuria, air hunger, coma,
death
Management
A-RESUSCITATE
TEAM(call for help)- Obstetrician, Anaesthetist ,midwife Haematologist
and Blood Bank
IV access with 14 G cannula X 2,Oxygen, head down
Transfuse
Crystalloid (eg Hartmann’s)
Colloid (eg Gelofusine)
GIVE ‘O NEG’ OR uncross-matched own-group If no cross-matched blood
available .
Obstetrics Lec 15 Dr. Aseil
4
Monitor
PR,BP,Foley catheter for UOP,CVP,oximeter
Investigate
Cross match 6 units of blood
FBC ,Clotting screen
RFT,LFT
B-STOP THE BLEEDING
First step(if placenta delivered)
Examine uterus for atonia, or inversion
ENSURE UTERINE CONTRACTION.
1- Ensure empty bladder
2-Give uterotonics)
*IV oxytocin 10 units bolus followed by 40U in500ml NS infusion 125ml/hr
*IV ergometrine 0.2-0.5 mg
*IV Syntometrine (5 unit oxytocin +ergometrine)
*IM or inramyometrial Carboprost or haemabate(PG F2 *
*Misoprostol (PG E1).(800 Mcg rectally or orally)
bronchoconstrive C.I. in asthma SE diarrhea,v omiting ,fever ,headache &
flushing
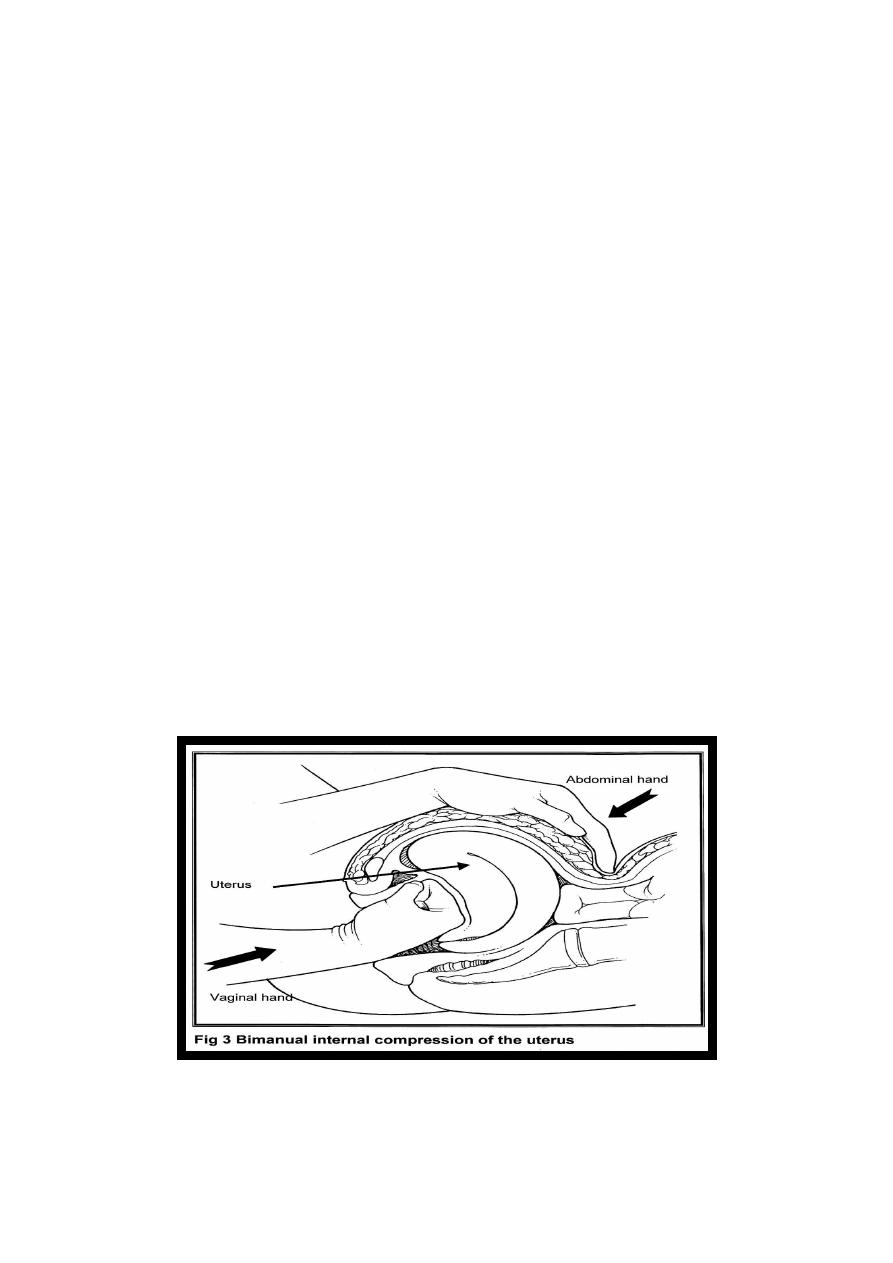
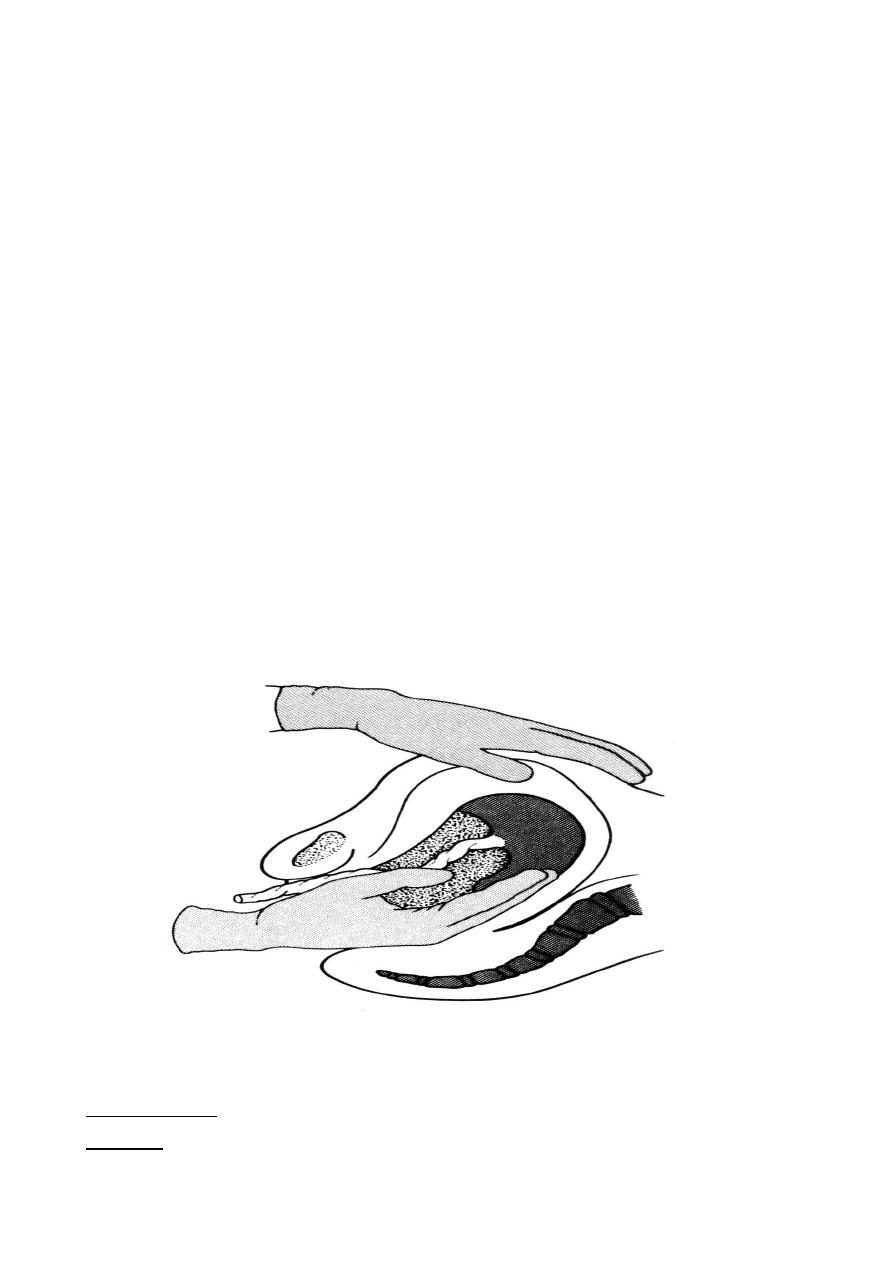
3-(uterine massage, Bimanual compression)
Second step
Exclude causes other than uterine atony
Obstetrics Lec 15 Dr. Aseil
5
Explore the uterine cavity for integrity , placenta debris and exclude clot
retention
*Examine lower genital tract for possible cervical,vaginal and perineal
tears.
*Exclude coagulopathies: bed side clotting test, clotting profile,fibrinogen
and FDP
Third step
EUA
SURGICAL TREATMENT
Repair of trauma if any
UTERINE PACKING
UTERINE TAMPONADE
Uterine A. ligation
Internal Iliac A. Ligation
Brace suturing of Uterus(B- Lynch)
Angiographic embolisation of U.A.
Hysterectomy
IF Placenta not delivered
EUA & MANUAL REMOVAL OF PLACENTA
Placenta Accreta
(1) Accreta vera,
in which the placenta adheres to the myometrium without invasion .
(2) Increta, in which it invades into the myometrium.

Obstetrics Lec 15 Dr. Aseil
6
(3) Percreta, in which it invades the full thickness of the uterine wall and
possibly other pelvic structures, most frequently the bladder.
UTERINE RUPTURE
Rupture of the uterus is described as complete or incomplete and dehiscence
of a cesarean section scar.
Management of Rupture Uterus
At this point, a decision must be made to perform hysterectomy or to
repair the rupture site. In most cases, hysterectomy should be performed.
repair of the rupture can be attempted (in dehiscent scar following C/S).
MORBIDITY & MORTALITY from PPH
Shock & DIC
Renal Failure
Puerperal sepsis
Blood transfusion reaction
Thrombo-embolism
Sheehan’s syndrome
>25% Maternal deaths are due to PPH
EDITED BY :TWANA NAWZAD
