Dr.Esraa
Amniotic fluid abnormalities
Physiology
In first trimester Amniotic fluid is transudate of plasma across maternal & fetal
surfaces.
From second trimester onward is produced almost exclusively from fetal urine, in
later gestation in addition to fetal urine production , there will be fetal lung secretion
it is functions :-
Protect the developing baby from pressure or trauma
Allow limb movement , hence normal postural development .
permitting the fetal lung to expand and develop breathing.
Volume of amniotic fluid
in early pregnancy is increased with gestation but this not maintained with
plateau at 770-800 ml between 24-37 wk .
By 40 wk ,the volume is less than 600 ml.
by 41 wk decreased to around 500 ml.
Volume is maintained by fetal urine & lung production being balanced by fetal
swallowing & absorption through GIT.
Oligohydramnios
Is defined by DVP( deepest vertical pool) less than 2 cm. Or AFI less than 5
th
centile
for gestation.Or AFI less than 5 at term.
Causes of oligo.
1.Preterm Premature rupture of membrane.
2.Placental insufficiency.
3.Congenital fetal abnormalities:
renal agenesis
urethral obstruction
renal dysplasia

Fetal & maternal risk:
1.Pulmonary hypoplasia.
2.Chorioamnionitis subsequent to PPROM.
3.Prematurity.
4.Perinatal mortality due to prematurity & congenital
malformation.
5.Potter syndrome: flattened facies, postural deformities & pulmonary
hypoplasia.
6.There are few maternal risk , unless fetal therapy is considered such as
placement of vesico amniotic shunt , these procedures carry the risk of
placental abruption & chorioamnionitis
Management
*Confirm aetiology of oligohydramnios, PPROM is apparent from history &
clinical examination. Clinical examination may revealed chronic hypertension
or pre-eclampsia.
*Amnio-infusion has been tried in past with no reduction in perinatal mortality.
*Exclude congenital anomalies or aneuploidy.
*Renal agenesis may be difficult to confirm because of large fetal adrenal
gland. However, inability to visualize fetal bladder on serial ultrasound or
bilateral absence of renal areteries using doppler us can increase sensitivity of
diagnosis.
*In cases of urinary outflow tract obstruction , vesico amniotic shunting may
improve fetal survival.
Polyhydramnios
DVP ≥ 8 cm. Or AFI above the 95
th
centile for the gestational age. Or an
amniotic fluid index (AFI) greater than 25 cm at term.
Causes :
1.Idiopathic
2.Diabetus mellitus
3.Intestinal obstruction ( oesophageal or duodenal atresia)
4.Impaired fetal swallowing ( aneuploidy, anencephaly, muscular dystrophy)

5.Fetal polyuria (twin- twin transfusion syndrome )
6.Cardiac failure secondary to lower fetal vascular resistance(fetal anaemia
due to maternal alloimmunoization or parvovirus B 19 infection).
Fetal & maternal risks
1.Preterm labour.
2.Abdominal discomfort.
3.Uterine atony postpartum
4.Unstable lie.
5.Placental abruption.
6.Perinatal mortality due to preterm delivery and congenital abnormality
Management
*History , attention to maternal symptoms such as diabetes , red cell
alloimmunization, recent viral infection.
*High resolution us to assess degree of polyhydramnios, identify multiple
pregnancy, assessment of fetal anomaly, fetal assessment include
examination of fetal CNS, gastrointestinal and renal system.
*Karyotyping should be offered in association of structural anomaly.
*If a viral infection is suspected , fetal & maternal samples should be obtained.
*If the polyhydramnios is associated with anaemia, the fetus is almost always
is hydropic , serial amniotransfusion can be done.
Treatment
:-- Aim of treatment is to reduce maternal discomfort and to prolong
pregnancy. Treatment is indicated when there is sever polyhydramnios ( AFI ≥
40 cm
or DVP ≥ 12 cm)
Treatment include :
1.Prostaglandin synthase inhibitors e.g indomethacin: decrease fetal urine
production & reduce polyhydramnios. Side effect include fetal renal failure,
premature closure of ductus arteriosus, necrotizing enterocolitis & intracranial
haemorrhage.
2.Serial amnioreduction ; may precipitate preterm delivery & lead rapid re-
accumulation of liquor.
3. Polyhydramnios associated with twin
–twin transfusion can be treated by
serial amnioreduction or altervatively distruption of communicating placental
vessels with laser therapy.
IUGR
IUGR: Is a failure of a fetus to achieve it is growth potential.
Small for gestational age SGA: means that the weight of the fetus below the
10th centile for it is gestation.
SGA are constitutionally small & not compromised while in IUGR there is a
pathological process.
Aetiology
*Intrinsic factors affecting fetal growth potential
1.Aneuploidy e.g trisomy 18.
2.Structural abnormalities e.g renal agenesis.
3.Intrauterine infection e.g CMV, toxoplasmsa.
*Extrinsic factors:
a.Maternal factors
1-Undernutrition such as poverty, eating disorder
2-Maternal hypoxia e,g living in high altitude, cyanotic heart disease
3-Drug e,g alcohol, smoking.
b.Placental factors
1-Reduced uteroplacental perfusion: inadequate trophoblast invasion, multiple
gestation
2-Reduced fetoplacental perfusion: single umbilical artery, TTTS.
Risk factors for IUGR
1.Multiple pregnancy 2.Previous pregnancy of IUGR
3.Current heavy smoker 3.Current drug users
4.Maternal medical diseases e,g HT,DM, CHD, APS.
5.Pregnancies with SFH is less than expected

Pathophysiology
*Symmetrical FGR : caused by factors directly affect fetal growth e,g
chromosomal disorders & fetal infection
*Asymmetrical FGR : caused by uteroplacental insufficiency which leads to
reduce O2 transfer to fetus & impair excretion of CO2 by placenta , this fall in
PO2 lead to vasodilatation in fetal brain, myocardium & adrenal gland with
vasoconstriction of renal, splanchnic vessels. Liver circulation is reduced
severely .
these changes result in :
1.Reduced abdominal girth with brain sparing
2.Renal vasoconstriction & leading to reduced urine output & oligphydramnios
3.Chronic FGR lead to metabolic & respiratory acidosis, which if prolong can
lead to IUFD.
4.Intrapartum hypoxia due to further compromise of uteroplacental circulation
by uterine contraction.
Fetal & neonatal problems
1.Perinatal hypoxia
2.Operative delivery
3.Neonatal encephalopathy
4.Neonatal hypoglycemia, hypocalcemia, hypothermia
5.Neonatal polycythemia
6.Perinatal morbidity & mortality
Management
1.Accurate assessment of gestational age by early US before 20
week(CRL˂14 & HC 14-20WK).
2.Assessment of fetal growth by US biometry (BPD, HC, AC, FL) at 2-4 wk
interval.
3.Determine whether the baby is constitutionally small or FGR.
4.US should be performed for fetal anatomy, even if the fetal anatomy is
normal the presence of symmetrical FGR should offer fetal karyotyping &
amniocentesis.
5.Currently no treatment available for FGR due to uteroplacental insufficiency
apart from stoping smoking, drug abuse and optimization of maternal health,
low dose aspirin may play role in pv but not effective in treating established
cases.
6.Surveillance of FGR fetus:
*Serial biometry & AFV at not less than 2 wkly interval
*Umbilical artery doppler
*Fetal CTG
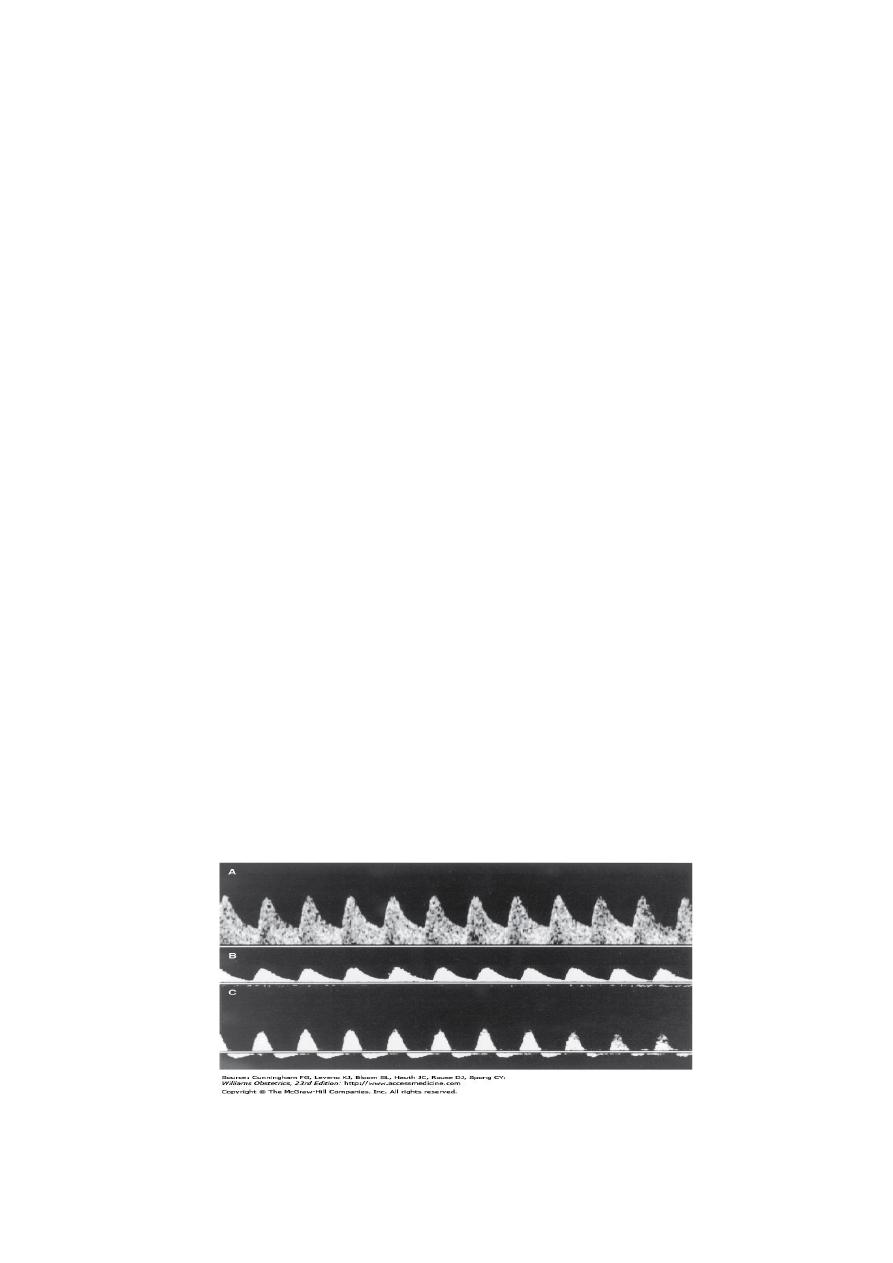
Doppler us in IUGR:
In fetuses with IUGR there are several adaptive vascular
changes:
Umbilical artery (UA) is low resistance vessel with both systolic & diastolic flow in
normal fetus suggesting continuous placental perfusion.
In pregnancy affected by IUGR , UA shows increasing resistance that initially blunt
forward flow during diastole & ultimately reverses at later stage
Once reversal of diastolic flow is identified, steroid should be administered in
premature fetus & delivery should be considered.
Middle cerebral artery MCA is high resistance vessel in normal fetus compared to
UA , in hypoxic fetus there will be vasodilatation & decreased in resistance
Mx of abnormal doppler indices
In mature fetus, little is gained by continuing pregnancy, & time course to
decompensate is shorter , therefore delivery is recommended. Induction of labour
would be possible in those with reassuring FHR.
In premature fetus , once AEDF in UA is demonstrated :
1.Twice weekly BPP
2.Repeat of doppler indices
3.Daily kick count
4.Growth scan every 2 wk
In premature fetus with REDF:
1.Hospitalization with continuous O2 therapy
2.Bed rest
3.Daily BPP
4.Daily doppler
5.Steroid
6.REDF & pulsatile DV pattern will not tolerate labour
Sama Adeeb
