
Obstetrical shock & maternal collapse
Shock:
Is a critical condition & life threatening medical emergency . It results from
acute, generalised, inadequate perfusion of blood (Oxygen and nutrients) to
tissues resulting in cellular injury and inadequate cell function .
Aetiology of shock:
●
Hypovolaemic:
hemorrhage, protracted vomiting(hyperemesis),
diarrhea, DKA & burns.
Septic :
sepsis, endotoxaemia
●
●
Cardiogenic:
massive pulmonary embolism, cardiomyopathy ,
obstructive non structural (cardiac tamponade, constictive pericarditis),
obstuctive structural (AS, MS), dysrhthmia, regurgitant lesions, blunt
cardiac trauma.
●
Distributive:
neurogenic due to spinal injury, regional anaesthesia or
anaphylaxis
Stages of shock:
Stage 1(compensated) :
changes in BP & COP compensated by adjustment
of homeostatic mechanism. In healthy patient this type of shock may not
require fluid replacement if cause is removed.
Stage 2(decompensated) :
maximal compensatory mechanism but tissue
perfusion is reduced & vital organ function are impaired.

Stage 3 (irreversible) :
vital organ function is impaired , acute tubular
necrosis, sever acidosis, decreased myocardial perfusion &decreased
myocardial contractility, decrease in perfusion lead cellular damage &
death
Initial management:
* Diagnosis require high index of suspicion, physical signs of inadequate
tissue perfusion , initial mx does not depend on the knowledge of
underlying cause.
*Airway: patent airway, high flow oxygen 15 L\min, tracheal intubation if
potential compromise
Breathing should be checked & supported if inadequate
*
* Circulation: insert 2 wide bore peripheral iv cannulas, sample should be
drawn for CBC, coagulation screen, electrolyte , urea, cross matching.
Start crystalloid ,blood may be required (O-ve or group specific uncrossed
matched blood in massive hge).
* Left lateral tilt or a wedge or manual replacement of uterus to avoid
aortocaval compression.
* Response to therapy can be monitored with monitoring of pulse BP pulse
oximetry & urin out put.
* After initial resuscitation , underlying cause should be identified &
treated

Causes of haemorrhagic shock in pregnancy:
Antenatal:
ruptured ectopic pregnancy, incomplete abortion, Placenta
Previa, Placental Abruption, uterine rupture.
Postpatum:
uterine atony, laceration to genital tract, chorioamnionitis,
large placental size (twin), acute uterine inversion , uterine fibroid,
puerperal sepsis
Haemodynamic consideration during pregnancy :
♫
Pregnancy produce a hyperdynamic, hypervolemic maternal
circulation this protect mother against haemorrhage to some degree.
♫
Greater fluid losses ˃30% of blood volume can occur before anything
other than maternal tachycardia. At this point peripheral vasoconsriction ,
hypotension develop. Aortocaval compression aggrevate the instability
seen in haemorrage.
♫
In antepartum period uteroplacental hypoperfusion cause abnormal
FHR pattern before maternal signs become evident
♫
Fluid resuscitation in obstetric hge is conservative because of under
estimation of volume & rapidity of blood loss , symptoms of hypovolemia
are delayed because of compensatory mechanism, moreover concern that
fluid overload cause pulmonary oedema
♫
A loss of 1 litre of blood requires replacement with 4 litre of crystalloid
until cross matched blood is available
♫
Emergency measures should be initiated if estimated blood loss more
than one third of women blood volume (bl.vol=wt X 80) or more than
1000 ml or change in hemodynamic state

♫
Golden hour is the time at which resuscitation must be started to ensure
best chance of survival, the probability of survival is decreases sharply
after 1
st
hr if pt is not effectively resuscitated.
♫
Rule of 30 : if systolic BP falls by 30 mmHg, HR rises by 30 bpm , RR
increase to 30 b\m , Hb or pcv drop by 30% or UOP less than 30ml\hr ,
the patient is likely to have lost at least 30% of her blood volume & she is
in moderate shock (Shock index =HR\SBP)
Principles of resuscitation :
* One litre of fresh frozen plasma should be administered with every 6
unit of blood
* Platelets should be more than 50000\L or more than 80000\L if
surgical intervention is likely
* Cryoprecipitate may be required if there is DIC or if fibrinogen level less
than 10 g\l
Degrees of hypovolemic shock:
#
Mild shock when 20% of blood volume is lost, which result in decrease
perfusion to non vital organs like skin, fat, skeletal muscle, with pale , cool
skin
#
Moderate shock 20-40% of blood volume is lost with decrease
perfusion to vital organs like liver , kidneys, oliguria& \or an uria ,
mottling of skin in extremities.
#
Sever shock more 40% of blood volume is lost, with decreased tissue
perfusion to heart & brain leading to agitation ,coma, & cardic arrest
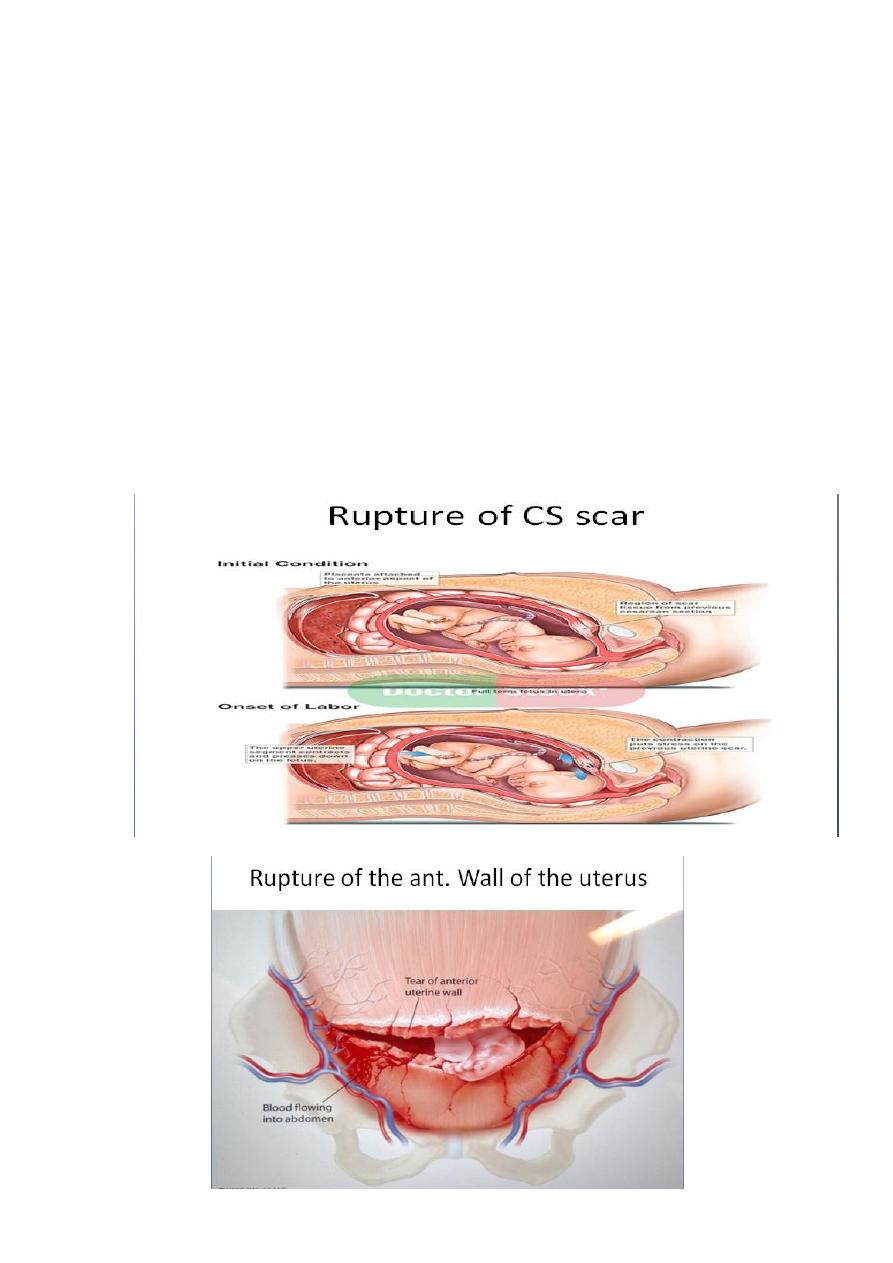
Uterine rupture :
* Uterine scarring due to previuos CS or myomectomy is most important
risk factor.
* Uterine rupture cause acute fetal distress, cessation of uterine
contraction , scar tenderness suggest but it is not a constant feature,
vaginal bleeding may occur, high head which was low in birth canal
earlier.
* Stop oxytocin if running , emergency laparotomy & CS hysterectomy
need to be performed if there is uncontrollable hge.
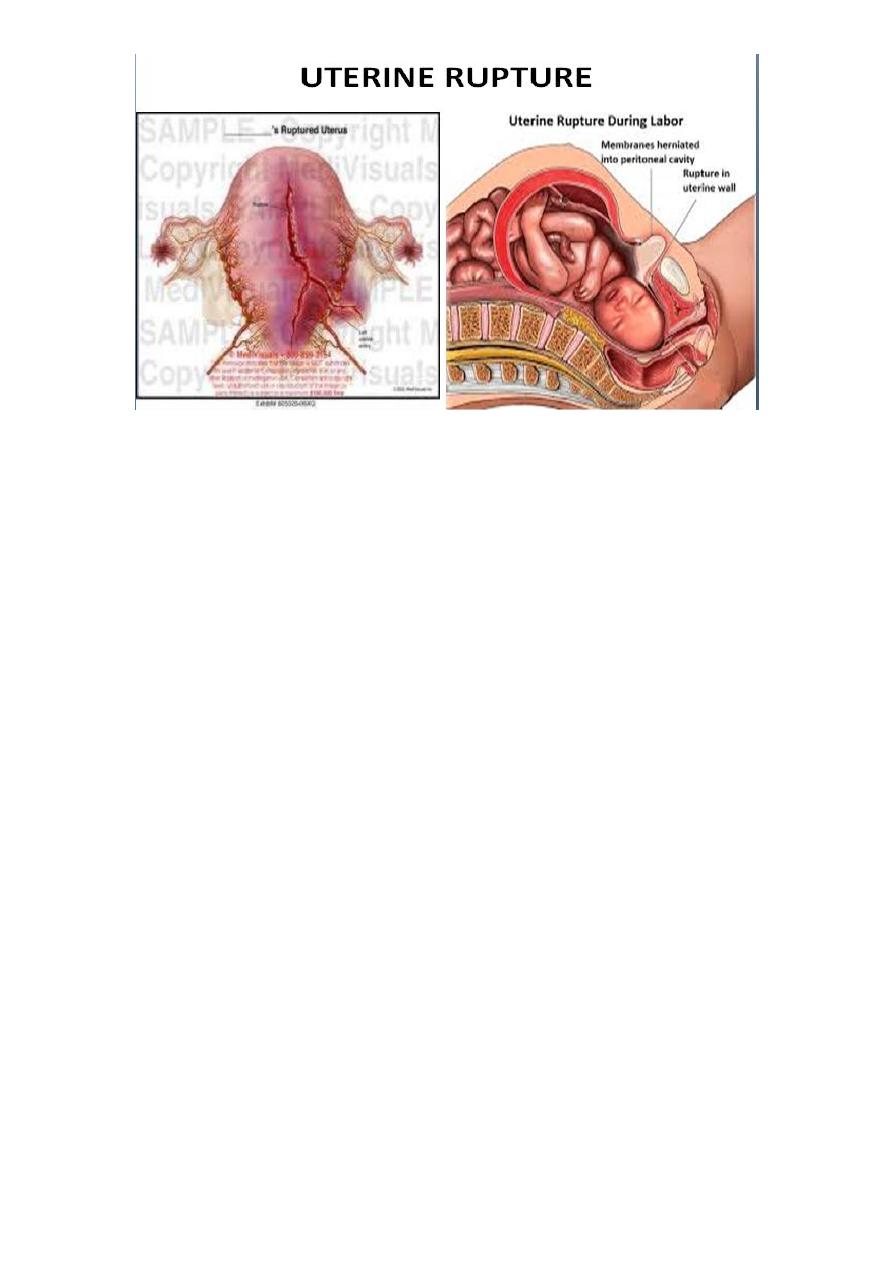
Complications:
Hemorrhage , shock, post operative infection, urethral damage,
thrombophilibitis, DIC, pituitary damage & death
Pregnancy after uterine rupture:
If the site of the rupture scar is confined to the lower segment the rate of repeat
rupture Is 6% in contrast upper segment is 32% . therefore women with prior
uterine rupture are should delivered by CS. As soon as the fetus maturedor at
36-37 week of gestation befor the onset of labour.
Uterine inversion :
Predisposing factors:
Short umbilical cord
#
Excessive traction on cord
#
Excessive fundal pressure
#
Fundal implantation of placenta
#
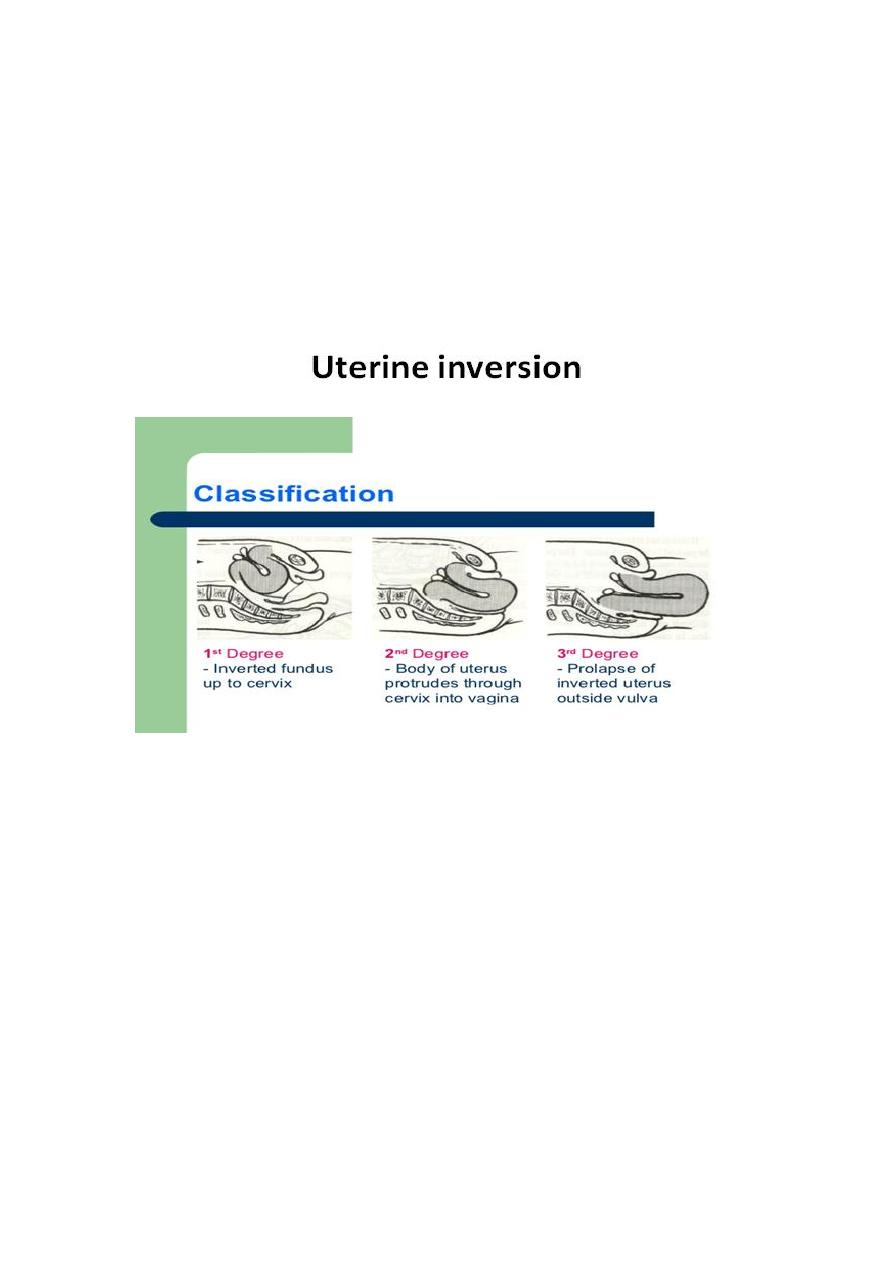
Retained placenta& abnormal placental adherence.
#
Chronic endometritis
#
Rapid or long labour
#
#
Previous ut inversion
Drugs: mg sulphate
#
●
Dx :
prolapsed uterus stretching cervix causes vagal stimulation with
signs of cardiovascular collapse , although hge is present the symptoms
will be out of proportion to estimated blood loss , inverted uterus may be
obvious at introitus with lack of palpable uterus in abdomin or feeling of
dimple in fundus on examination
Rx :
●
-resuscitate pt using ABC approach
-not remove placenta if still attached
-immediately replace uterus through cervix by manual compression
-if failed hydrostatic pressure can
be applied pouring warmed NS to
vagina
-tocolysis may be used to relax
cervical ring
-surgery to reposition uterus from
above is last resort
-after replacement, uterine contraction is maintained with oxytocic
Septic shock :
Systemic inflammatory response syndrome : recognized by presence of 2 or
more of following
1. temp˂ 36C or ˃ 38C.
2. PR ˃90 bpm
3. RR ˃ 20 breath\ min
4. WBC ˃ 12 000 \mm3
Sepsis : SIRS + evidence of infection
Septic shock: evidence of infection + refractory hypotension despite of fluid
resuscitation
Sepsis with multiorgan failure.
Predisposing factors for sepsis :
Post vaginal or caesarean delivery endometritis
*
Prolonged rupture of membrane
*
* Cerclage with ruptured membrane
* Septic abortion
* Retained product of conception
* Intramniotic infection pregnancy with retained IUCD
Instrumentation of genital tract
*
* UTI
* Isolated MO: E.coli, group A&B streptococcal, klebsiella , staph aureus
General mx of septic shock :
* Rapid volume expansion, in pregnancy mother is the 1
st
priority . Fetal
compromise in sepsis directly due to maternal cardiovascular
decomposation so improvement of maternal condition have a positive
effect on the fetus. Delivery of fetus by CS in an unstable mother will end
in poor outcome
Transfer to ICU
*
Invasive monitoring may be required
*
* Obtain blood, urine, wound culture& start iv broad spectrum antibiotic initiall
* Removal of infected tissue after initial resuscitation e,g evacuation of
uterus, delivery in chorioamnionitis, drainage of abscess.

* In critically ill septic pt there may be relative adrenal insufficiency &
adrenal gland not respond to ACTH, low dose hydrocortisone may be
beneficial
Anaphylaxis :
- Caused by pharmacological agent, insect bite, foods & latex.
- There is exaggerated immunological response to antigen to which
individual has been sensitized. It is IgE mediated hypersensitivity reaction
causing breakdown & degranulation of mast cell & basophils releasing
mediator like histamine , serotonin into plasma . These substances cause
increased mucus secretion , increase capillary permeability, marked
vasodilatation & bronchospasm
Special aspects in mx of anaphylactic shock :
Call for help & stop administration of suspected agent.
♫
♫
Early intubation of trachea should be considered bc upper airway
oedema make this problematic.
Epinephrine
♫
Rapid intravascular volume expansion with crystalloid
♫
Atropine if there is significant bradycardia
♫
If bronchospasm persist : nebulised or iv B2 agonist
♫
Iv histamine
♫
Iv hydrocotisone
♫

♫
Immediate IX: Elevated serum tryptase indicate that reaction due to
mast cell degranulation . Late refer to immunologist
Amniotic fluid embolism :
* The process is more similar to anaphylaxis than to embolism, so the term
anaphylactoid syndrome of pregnancy has been suggested.
* Amniotic fluid within pulmonary circulation produce intense pulmonary
vasospasm , pulmonary hypertension , hypoxia this initial response is
resolved within 15-30 min followed by a phase of hemodynamic
compromise caused by left heart failure
Clinical features:
Hypotension, dyspnea, seizure, cough, cyanosis, fetal bradycardia,
uterine atony & cardiac arrest
Management:
Basic shock mx
-Treat hypoension with crystalloid
-Women who survive initial event will require ICU bc heart failure & DIC
are late occurrence
-Treatment of coagulopathy
-Perform emergency CS in arrested mothers who are not responsive to
resuscitation

Distributive shock:
There is no loss in intavascular volume, the defect is due to massive
vasodilatation leading to relative hypovolemia.
Anaesthesia :
High spinal block
* Drug dose for subarachnoid anaesthesia in pregnancy is reduced, use of
standard non obstetric doses may lead to extensive block
* Excessive spread of intrathecal injection of appropriate dose of local
anaesthesia
* Accidental intrathecal injection of local anaesthesic dose intended for
epidural space. The cause may be drug passing through an unrecognised
dural puncture or migration of epidural catheter from epidural to
intrathecal space.
* Hypotension can be aggrevated by incorrect positioning especially in
absence of left lateral tilt.
Clinical features :
* Hypotension preceded by complaint of nausea or feeling unwell
* Bradycardia occur when sympathetic block reaches level of cardio
acceletory fibersT1-T4 causing unopposed vagal tone
* Difficulty in breathing as block progresses in cephaled direction as 1
st
intercostal muscle & diaphram are paralysed
* Upper limb neurological sign C5-T1 & tingling of fingersC6-T1

Special aspects in treatment of high block :
ABC
*
Vasopressor drugs
*
* Sedative agent to reduce risk of awareness once initial resuscitation has
been done
Local anaesthesia toxicity :
Occur due to high plasma concentration that occurs in accidental iv
injection , rapid absorption or absolute overdose. Accidental injection in
obstetric anaesthesia occur during subcutaneous infiltration , the
generous blood supply in this region encourages rapid absorption &
increase risk of toxicity
Clinical features :
* Central nervous system: light headedness, tinnitus, dizziness, circumoral
numbness, metallic test confusion , tonic clonic seizure, loss of
consciousness, coma
* Cardiovascular : hypertension, tachycardia, refractory cardiorespiratory
arrest
* CNS toxicity precedes CVS toxicity , in bupvicaine CVS toxicity may
occur in absence of CNS toxicity
Special aspect in treatment :
* Advanced life support with external cardiac massage & defibrillation
* Vasopressor drugs
* Seizure mx by diazepam
* CS may be considered to rescue the fetus.
* Sedative agent to reduce risk of awareness once initial resuscitation has
been done
New development :
* Blood is removed from operative site by heparinised tube & filter into
collecting reservoir & processed by washing , resulting blood have htc of
55-80% can be returned to patient quickly
Expensive
*
Not suitable for PPH in labour due to fecal contamination
*
Risk of transfusion of amniotic fluid
*
Recombinant factor VII
Forms a complex with tissue factor at site of endothelial damage
producing thrombin , Va, VIIIa, platelets with conversion of fibrinogen to
fibrin
Meral Cevdet
