Obstetrics Dr. Eman
Hypertensive disease
in pregnancy,
preeclampsia &
eclampsia
PE (pre-eclampsia)
•
Hypertension of at least 140\90 mmHg on at least 2 separate
occasions , at least 4 hr apart & in presence of at least 300 mg
protein in 24 hr collection of urine , arising after 20
th
week of
pregnancy in a previously normotensive women & resolving
completely by the 6
th
postpartum week.
Chronic hypertension
BP ˃140/90 mmHg before pregnancy or diagnosed before 20 weeks'
gestation or Hypertension first diagnosed after 20 weeks' gestation and
persistent after 6 weeks postpartum.
Chronic hypertension superimposed by preeclampsia:
New-onset proteinuria 300 mg/24 hours in hypertensive women after
20 weeks' gestation. Chronic HT even in absence of superimposed PE
can lead to maternal & fetal morbidity, so pregnancy in women with
chronic HT should be regarded as high risk pregnancy.
Gestational hypertension
• Systolic BP˃ 140 or diastolic BP ˃90 mm Hg for first time during
pregnancy
• No proteinuria
• BP returns to normal before 6 weeks postpartum
1

Obstetrics Dr. Eman
•
Final diagnosis made only postpartum
•
Not associated with adverse outcome, effort should be done to
differentiate it from PE.
Preeclampsia:-
Risk factors for PE
•
First pregnancy
•
Multiparous with: PE in any previous pregnancy, or 10 years or
more since last baby
•
Age more than 40 yr
•
BMI of 35 or more
•
Family history of PE in mother or sister
•
Booking diastolic blood pressure of 80 mmHg or more
•
Booking proteinuria of ≥ 1+ on more than one occasion or ≥ 0.3 g\
24 hr.
•
Multiple pregnancy
•
Underlying medical diseases:
➢ pre-existing HT
➢ pre-existing renal disease
➢ pre-existing DM
➢ antiphospholipid syndrome
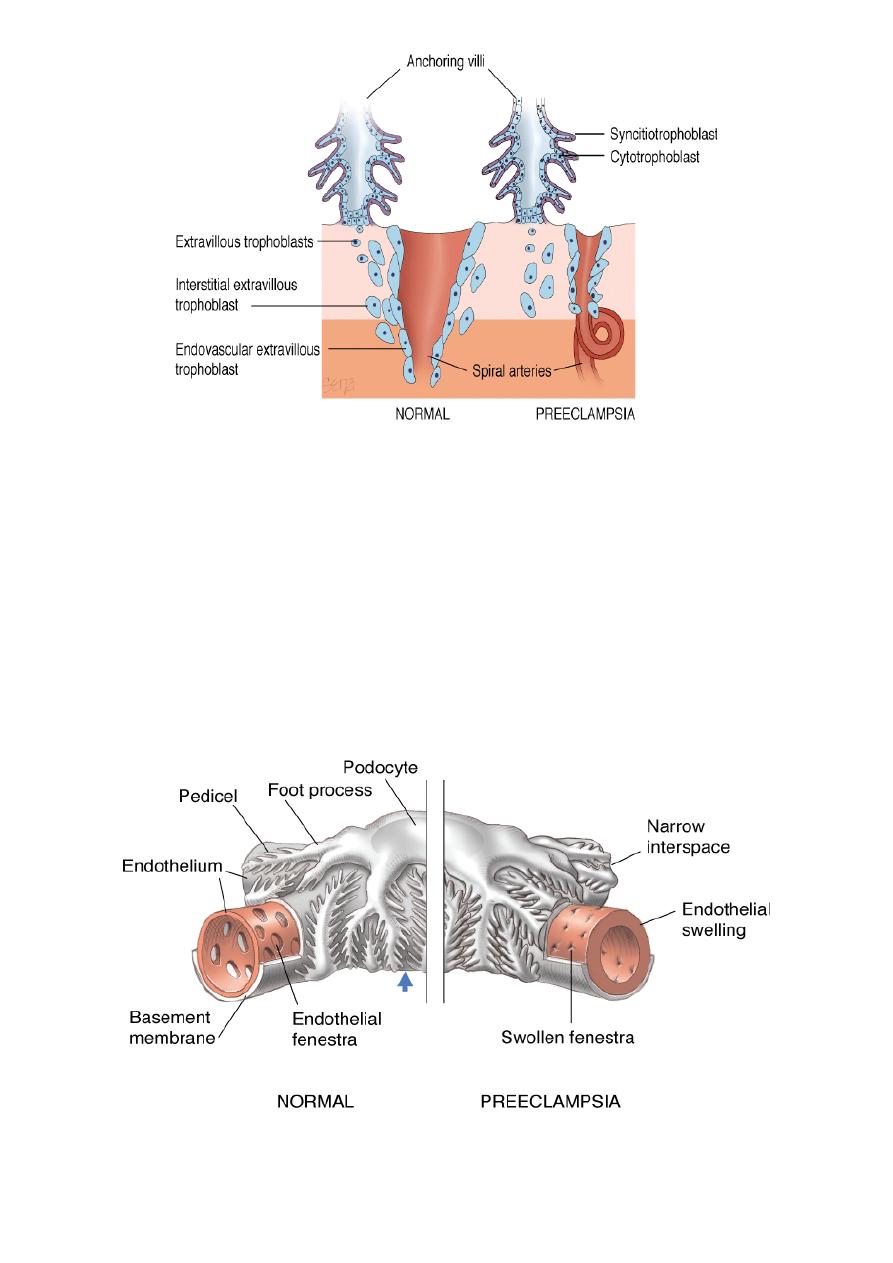
Aetiology :--
Genetic predisposition abnormal immunological
response defecient trophoblast invasion hypoperfused placenta
release of circulating factors activation of vascular endothelia
clinical manifestation of disease.
2
Obstetrics Dr. Eman
preeclampsia is best described as a pregnancy- specific syndrome that
can affect virtually every organ system:
1.Cardiovascular system: in normal pregnancy there is peripheral
vasodilatation while in preeclampsia there will be marked
vasoconstriction, increased intravascular pressure & loss of endothelial
cell integrity result in increase vascular permeability & generalized
oedema.
2.Renal system : glomeruloendotheliosis is specific for PE characterize
by impaired glomerular filtration & proteinuria resulting in decrease in
plasma oncotic pressure that exacerbate development of oedema.
3.Haematological system : normally expected hypervolemia is severely
curtailed. Women of should have a blood volume of 5000mL during the
3
Obstetrics Dr. Eman
last several weeks of a normal pregnancy, compared with 3500 mL when
not pregnant. With PE much or all of the anticipated normal excess
1500 mL is lost. Such hemoconcentration results from generalized
vasoconstriction that follows endothelial activation and leakage of
plasma into the interstitial space because of increased permeability.
4.CNS: Headache and scotomata are thought to arise from
cerebrovascular hyperperfusion that has a predilection for the occipital
lobes. they are unique in that they usually improve after magnesium
sulfate infusion is initiated. Convulsions are diagnostic for eclampsia.
Blindness is rare with preeclampsia alone, but it complicates eclamptic
convulsions in up to 15 percent of women . Generalized cerebral edema
may develop and is usually manifest by mental status changes that vary
from confusion to coma. This situation is particularly dangerous because
fatal supratentorial herniation may result.
5.Liver: Symptomatic involvement, typically manifest by right-upper or
midepigastric pain and tenderness, is usually only seen with severe
disease.
Asymptomatic elevations of serum hepatic transaminase levels—AST and
ALT—are considered markers for severe preeclampsia. Hepatic
hemorrhage from areas of infarction may extend to form a hepatic
hematoma. These in turn may extend to form a subcapsular hematoma
that may rupture.
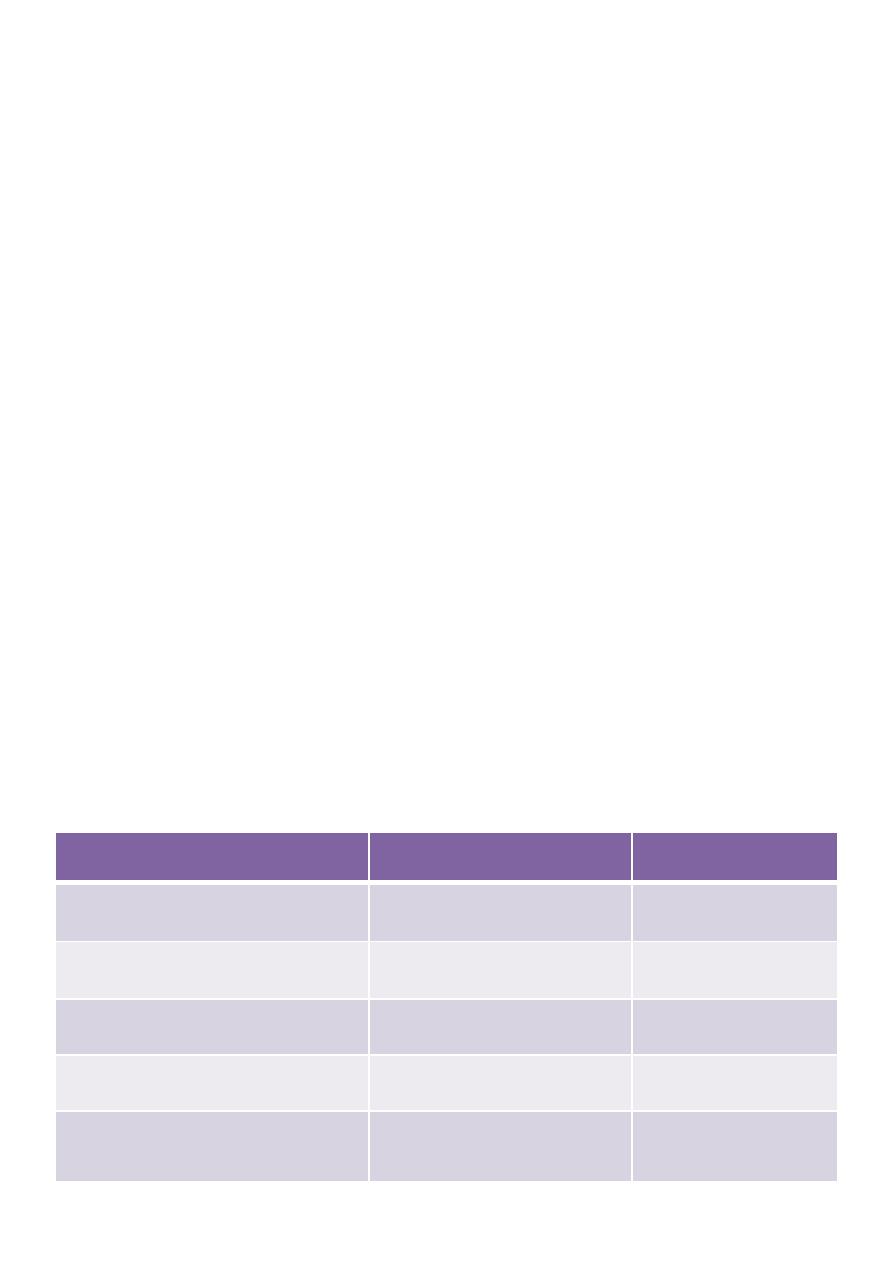
Indicators of severity in PE
Non sever
sever
Diastolic blood pressure
<110 mm Hg
≥110 mm Hg
Systolic blood pressure
<160 mm Hg
≥160 mm Hg
Proteinuria
≤2+
≥3+
Headache
Absent
Present
Visual disturbances(blurred
vision,flushing of light
Absent
Present
4
Obstetrics Dr. Eman
Investigation for PE
• MATERNAL
FBC, Clotting study : if platelets count are normal additional clotting
study is not indicated, RFT & LFT.
• FETAL
US assesment of fetal size, AFI, doppler
Antenatal CTG: loss of baseline variability or deceleration may indicate
fetal hypoxia.
Treatment
The basic management objectives for any pregnancy complicated by
preeclampsia are:
•
Termination of pregnancy with the least possible trauma to mother and
fetus.
• Birth of an infant who subsequently thrives
• Complete restoration of health to the mother.
A diagnosis of pre-eclampsia require admission. Patient with mild pre-
eclampsia & normal haematological and biochemical measures can be
monitored as out patient with frequent attendance for fetal &maternal
assessment.
Upper abdominal pain
Absent
Present
Oliguria
Absent
Present
Convulsion (eclampsia)
Absent
Present
Serum creatinine
Normal
Elevated
Thrombocytopenia
Absent
Present
Serum transaminase
elevation
Minimal
Marked
Fetal-growth restriction
Absent
Obvious
Pulmonary edema
Absent
Present
5

Obstetrics Dr. Eman
Patient with sever disease require inpatient management.
The aim of antihypertensive is to lower blood pressure , reduce the risk
of maternal CVA without reducing uterine blood flow.
•
Methyl dopa:
centrally acting antihypertensive agent.
safe in pregnancy.
oral tablets.
Takes 24 hr to act.
SE: depression & sedation
•
Labetalol :
alpha & non selective beta blocker.
Safe in pregnancy
Can be given orally or intravenously.
•
Nefidipine :
Calcium channal blocker.
Given orally
SE : sever headache that mimic worsening disease.
In sever disease intravenous hydralazine or labetalol can be used.
•
Hydralazine:
Direct vasodilator
Dose :- bolus 5 mg iv followed by further boluses of 5 mg every 15 min,
up to a cumulative dose of 15 mg, once BP is 140\90, infusion of 10 mg
\hr is started , doubling if necessary at 30 min interval , until a
satisfactory response or a dose of 40 mg\hr
Side effect :- headache, tachycardia, flushing, vomiting
•
Labetalol:-
Bolus of 20 mg iv , followed at 10 min interval by 40, 80, 80 mg boluses,
once BP 140\90 infusion of 40 mg\ hr is started , doubling at 30 min
interval , until a satisfactory response or a dose of 160 mg\hr
Whenever i.v antihypertensive is given BP should be monitored every
10-15 minute with continuous electronic fetal heart rate monitoring.
The aim is gradual lowering of BP with DBP to 90mmHg to avoid fetal
distress due to sudden drop in maternal BP that cause reduction in
uterine blood flow
6

Obstetrics Dr. Eman
Timing of delivery
Depend on:
1. Gestation
2. Severity of disease.
3. Presence of other complication
4. Stability of condition of the
patient.
Gestational age less than 34 wk steroid should be given to improve lung
maturity , recent studies indicate that steroid can benefit the mother
also
Mode of delivery
•
Delivery before term or unfavorable cx at term is by cs.
•
If labour start spontaneously or induced in presence of normal
clotting study , epidural analgesia can be used, it helps the BP to
decrease.
•
clotting disorders should be corrected before delivery regardless of mode of
delivery
•
Post partum women with sever preeclampsia are at risk of thrombo-
embolism, thromboprophylaxis should be given.
•
Ergometrine is contraindicated in the management of 3
rd
stage of
labour.
•
In majority BP & PU will resolve post natally , in minority one or
both persist for more than 6 wk indicating chronic HT or renal
disease.
•
Sever PE before 34 wk require careful medical assessment
Screening
Doppler US of uterine artery waveform can identify women at risk, in
pregnancies with incomplete trophoblast invasion, a notch can be seen
in doppler US. This may of value in women at high risk because of
medical or past obstetrical history but of no value in low risk women .
Prevention
•
Low dose aspirin 75 mg daily can lower risk moderately.
•
Calcium supplementaion.
•
Vitamins E & C does not reduce the risk of preeclampsia.
7

Obstetrics Dr. Eman
Eclampsia
• Is a generalized tonic-clonic convulsions,it may occur antepartum
(40%), intrapartum (20%), or postpartum(40%).
• Any convulsion in pregnancy should be considered eclamptic until
proved otherwise
• Eclampsia is most common in the last trimester and becomes
increasingly more frequent as term approaches.
Management
• ABC: airway, breathing should be secured, large bore intravenous
cannulae should be sited & blood taken for full blood count,
clotting studies, renal & liver function test & cross matching.
• Seizure due to eclampsia are self limiting & short lasting, the
patient shuld be moved to her side & oxygen applied.
• Termination of pregnancy regardless of gestational age
• Control of convulsions using intravenouse loading dose of
magnesium sulfate. This is followed by a continuous infusion of
magnesium sulfate
• Intermittent administration of antihypertensive medication to
lower blood pressure whenever it is considered dangerously high
• Avoidance of diuretics unless there is obvious pulmonary edema,
limitation of intravenous fluid administration unless fluid loss is
excessive, and avoidance of hyperosmotic agents
• Delivery of the fetus to achieve a "cure."
Magnesium sulphate
should be given that can be lower BP in addition to
anticonvulsant properties, initial loading dose of 4 g followed by infusion of 1 g\hr,
it is important to recognize mg overdose that can be reversed by calcium
gluconate. Assess deep tendon reflexes, UOP, RR periodically , measure serum
magnesium level at 4–6 hr and adjust infusion to maintain levels between 4 and 7
meq/L (4.8 to 8.4 mg/dL). Magnesium sulfate is discontinued 24 hr after delivery
Antihypertensive
should be given especially when systolic BP greater than 160
mmHg or diastolic greater than 110 mmHg:
-
i.v hydralazine.............................
-
i.v or oral labetalol.............
-
Oral nifidipine .......................
Whenever antihypertensive is given BP should be monitored every 10-15 minute
with continuous electronic fetal heart rate monitoring. The aim is gradual
lowering of BP with DBP to 90mmHg to avoid fetal distress due to sudden drop in
maternal BP that cause reduction in uterine blood flow
8

Obstetrics Dr. Eman
Management of fluid balance :
in pre eclampsia there is intense peripheral
vasoconstriction, decrease in plasma volume with redistribution of extracellular
fluid , so there will be risk of fluid over load & pulmonary oedema requiring strict
fluid input & output balance. In absence of bleeding 80 ml\hr of fluid( oral or iv)
should be given
HELLP syndrome
•
This condition is seen in 5-10% of cases of severe PE.
•
It is more common in multipara
•
It may associate with DIC, placental abruption or fetal death
Indication for delivery in PE
Maternal: Persistent severe headache or eclampsia
•
Shortness of breath; chest tightness, pulmonary edema
•
Uncontrolled severe hypertension despite treatment
•
Oliguria < 500 mL/24 hr or serum creatinine >1.5 mg/dL
•
Persistent platelet counts <100,000/L
•
Suspected abruption, progressive labor, and/or ruptured
membranes
Fetal: Severe growth restriction < 5th percentile for EGA
•
Persistent severe oligohydramnios AFI <5 cm
•
Biophysical profile 4 done 6 hr apart
•
Reversed end-diastolic umbilical artery flow
•
Fetal death
9
