
Pediatrics Lec 7 Dr. Ziyad
1
Fluid requirement
Fluid needs vary according to the gestational age, environmental condition, and
disease states.
Assuming minimal water loss in the stool of infant not receiving oral fluids, their
water need are equal to insensible water loss, excretion of renal solutes,
growth and any unusual water losses.
Insensible water loss are indirectly related to gestational age; very immature
preterm infant (<1000 g) may lose as much as 2-3 mL/kg/hr, partly because of
immature skin, lack of subcutaneous tissue, and a large exposed surface area.
Larger premature infants (2,000-2,500 g) nursed in an incubator may have an
insensible water loss of approximately 0.6-0.7 mL/kg/hr.
Insensible water loss is increased under radiant warmers, during phototherapy,
and in febrile infants. It is diminished when infants are clothed, breathe
humidified air, or are of advanced postnatal age.
Neoborn infants, especially those with VLBW, are also less able to concentrate
urine; their fluid intake required to excrete solutes increases.
Water intake in term infants is usually begun at 60-70 mL/kg on day 1 and
increased to 100-120 mL/kg by days 2-3.
Smaller, more premature infants may need to start with 70-80 mL/kg on day 1
and advance gradually to 150 mL/kg/day.
Daily weights, urine, and serum urea nitrogen and sodium levels should be
monitored carefully to determine water balance and fluid needs.
Clinical observation and physical examination are poor indicators of the state of
hydration of premature infants.
Conditions that increase fluid loss, such as glycosuria, the polyuric phase of
acute tubular necrosis, and diarrhea may lead to severe dehydration.
Alternatively, fluid overload may lead to edema, heart failure, patent ductus
arteriosus, and bronchopulmonary dysplasia.
Pediatrics Lec 7 Dr. Ziyad
2
Total Parenteral Nutrition:
Total intravenous alimentation may provide sufficient fluid, calories, amino
acids, electrolytes, and vitamins to sustain the growth of LBW infants before
complete enteral feeding has been established or when enteral feeding is
impossible for prolonged periods. Complications of intravenous alimentation
are related to both the catheter and metabolism of the infusate:
Coagulase-negative staphylococcus sepsis is the most important problem of
central vein infusions. Treatment includes appropriate antibiotics. If an infection
persists the line must be removed.
Thrombosis, extravasation of fluid, and accidental dislodgment of catheters
have also occurred.
Phlebitis, cutaneous sloughing, and superficial infection may occur.
Metabolic complications of parenteral nutrition include hyperglycemia, which
may lead to osmotic diuresis and dehydration; azotemia; hypoglycemia from
sudden accidental cessation of the infusate ; hyperlipidemia and
hyperammonemia. Metabolic bone disease and/or cholestatic jaundice and liver
disease may develop in infants who require long-term parenteral nutrition.
Feeding:
The process of oral alimentation requires, in addition to a strong sucking effort,
coordination of swallowing, epiglottal and uvular closure of the larynx and nasal
passages, and normal esophageal motility, a synchronized process that is usually
absent before 34 wk of gestation.
Oral feeding (nipple) should not be initiated or should be discontinued in infants
with respiratory distress, hypoxia, circulatory insufficiency, excessive
secretions, gagging, sepsis, central nervous system depression, severe
immaturity, or signs of serious illness.
These high-risk infants require parenteral nutrition or gavage feeding to supply
calories, fluid, and electrolytes.
Pediatrics Lec 7 Dr. Ziyad
3
Preterm infants at 34 week of gestation or more can often be fed by bottle or at
the breast. Smaller or less vigorous infants should be fed by gavage. The tube is
passed through the nose until approximately 2.5 cm (1 inch) of the lower end is
in the stomach; a measured amount of fluid is given by pump or by gravity.
Such tubes may be left in place for 3-7 days before being replaced by a similar
tube through the alternate nostril. The LBW infant may be fed with intermittent
bolus feeding or continuous feeding.
A change to breast or bottle-feeding may be instituted gradually as soon as
infant displays general vigor adequate for oral feeding
For infants under 1000 g the initial feedings are either breast milk or preterm
formula at 10 mL/kg/24 hr as a continuous nasogastric tube drip (or given by
intermittent gavage every 2-3 hr.)
if the initial feeding is tolerated, the volume is increased by 10 – 15 ml/ kg/24
hr. Once a volume of 150 ml/kg/24 hr achieved, the caloric content may be
increase to 24 or 27 kcal/oz.
Intravenous fluids are needed until feedings provide approximately 120
mL/kg/24. the feeding protocol for premature infants weighing over 1,500g is
initiated at a volume of 20-25 mL/kg/24 hr of full-strength breast milk or
preterm formula given as a bolus every 3 hr. thereafter increments in total daily
formula volume should not exceed 20 ml/kg/24 hr.
Prevention of Infection:
Premature infants have an increased susceptibility to infection, and thus meticulous
attention to infection control is required. Prevention strategies include:
1. Strict compliance with hand washing and universal precautions.
2. Limiting nurse-to patient ratios and avoiding crowding.
3. Minimizing the risk of catheter contamination, meticulous skin care
4. Encouraging early appropriate advancement of enteral feeding.
5. Education and feedback to staff.
6. Surveillance of nosocomial infection rates in the nursery.
Pediatrics Lec 7 Dr. Ziyad
4
PROGNOSIS:
Infants born weighing 1,501-2,500 g have a 95% or greater chance of survival,
but those weighing less still have significantly higher mortality.
Intensive care has extended the period during which a VLBW infant is at
increased risk of dying of complications of prematurity, such as
bronchopulmonary dysplasia, necrotizing enterocolitis, or nosocomial infection.
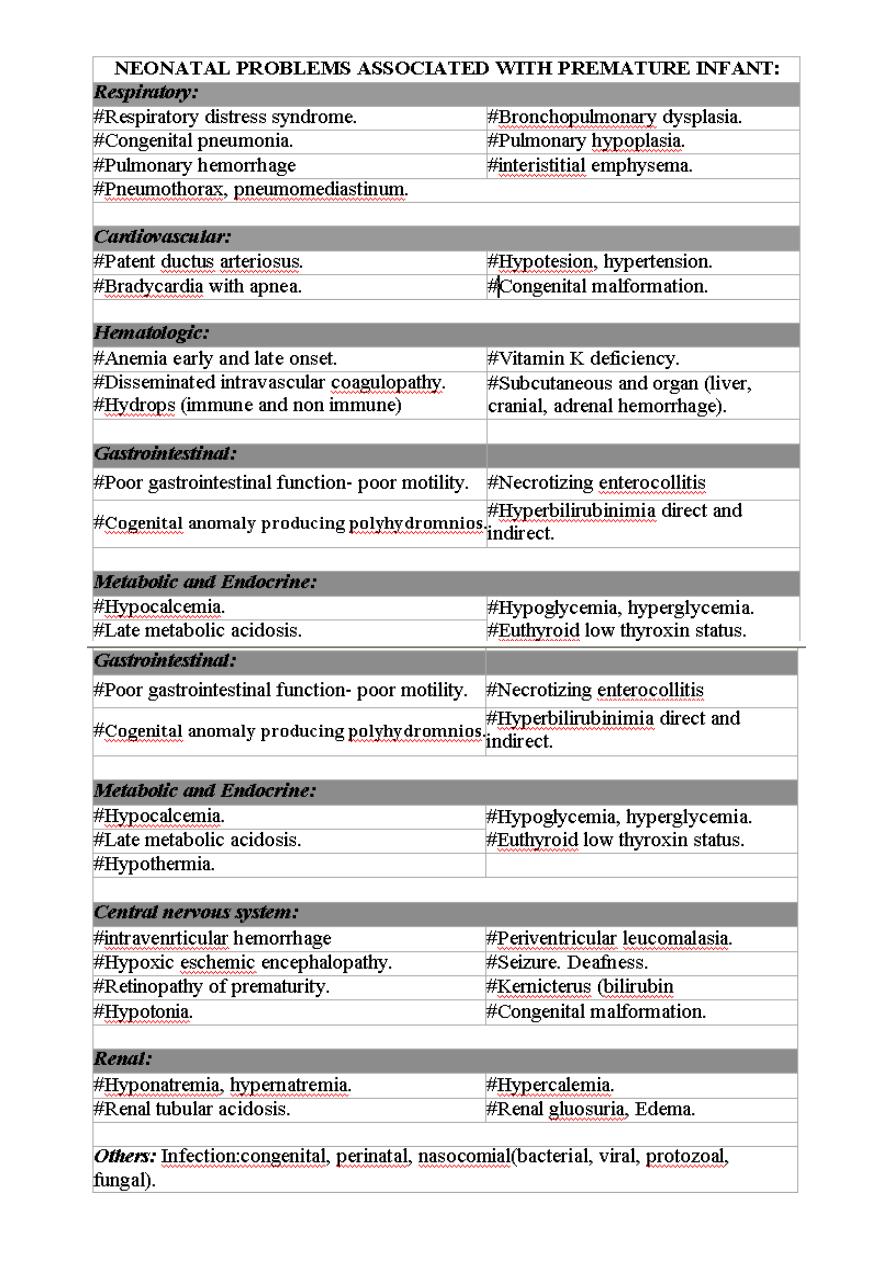
SEQUELAE OF LOW BIRTH WEIGHT
IMMEDIATE
Hypoxia, ischemia
Intraventricutlar hemorrhage Sensorineural injury
Respiratory failure
Necrotizing enterocolitis.
Cholestatic liver disease.
Nutrient deficiency
Social stress
.
Other
LATE
Mental retardation, spastic diplegia, mictocephaly, seizure, poor school
performance, spasticity, hydrocephalus
Hearing, visual impairment, retinopathy of prematurity myopia
Bronchopulmonary dysplasia, core pulmonale, bronchospasim
Short bowel syndrome, malabsorbtion, malnutrition
Cirrhosis, hepatic failure, hepatic carcinoma Growth, failure, osteopenia,
anemia,Child abuse or neglect, failure to thrive
Sudden infant death syndrome, infection, inguinal hernia
Pediatrics Lec 7 Dr. Ziyad
5
