Pediatrics Dr. Ziyad
1
Fatima Ehsan
HOSPITAL CARE OF THE
NEOBORN
BEFORE DELIVERY
a history of the mother should be elicited and her obstetric chart reviewed,
including:
● Pregnancy-related health issues
● Blood type, Rh antigen, and infant blood type, if known
● Prenatal laboratory values: hepatitis B, rubella, group B Streptococcus (GBS)
culture,, human immunodeficiency virus (HIV), hepatitis C (if obtained), sexually
transmitted disease screening, glucose tolerance test and drug screening
● Medications
● Lactation history and history of breast abnormalities or surgery
● Family/social history, if not obtained prenatally.
DELIVERY
A biophysical profile includes assessments of fetal breathing, heart rate, tone,
and amniotic fluid levels (fluid levels reflect fetal urinary output and, thus,
renal perfusion).
Approximately 10% of infants require some form of resuscitation; 20% of such
infants require aggressive intervention.
Most infants begin effective respirations following delivery and should establish
regular respirations by 1 minute of age.
An infant who has primary apnea and fails to respond to stimulation generally
responds to bag and mask ventilation.
Pediatrics Dr. Ziyad
2
Fatima Ehsan
Keeping the baby warm after delivery and during resuscitation minimizes heat
loss.
Newborns are at risk of heat loss due to their large surface area-to-body mass
ratio.
Cold stress can lead to depletion of important stores of the infant’s fat and
glycogen.
Healthy infants should be dried, covered with dry linen, and kept warm. Placing
infants skin-to-skin with the mother immediately after delivery may promote
bonding and breastfeeding success while keeping the baby warm.
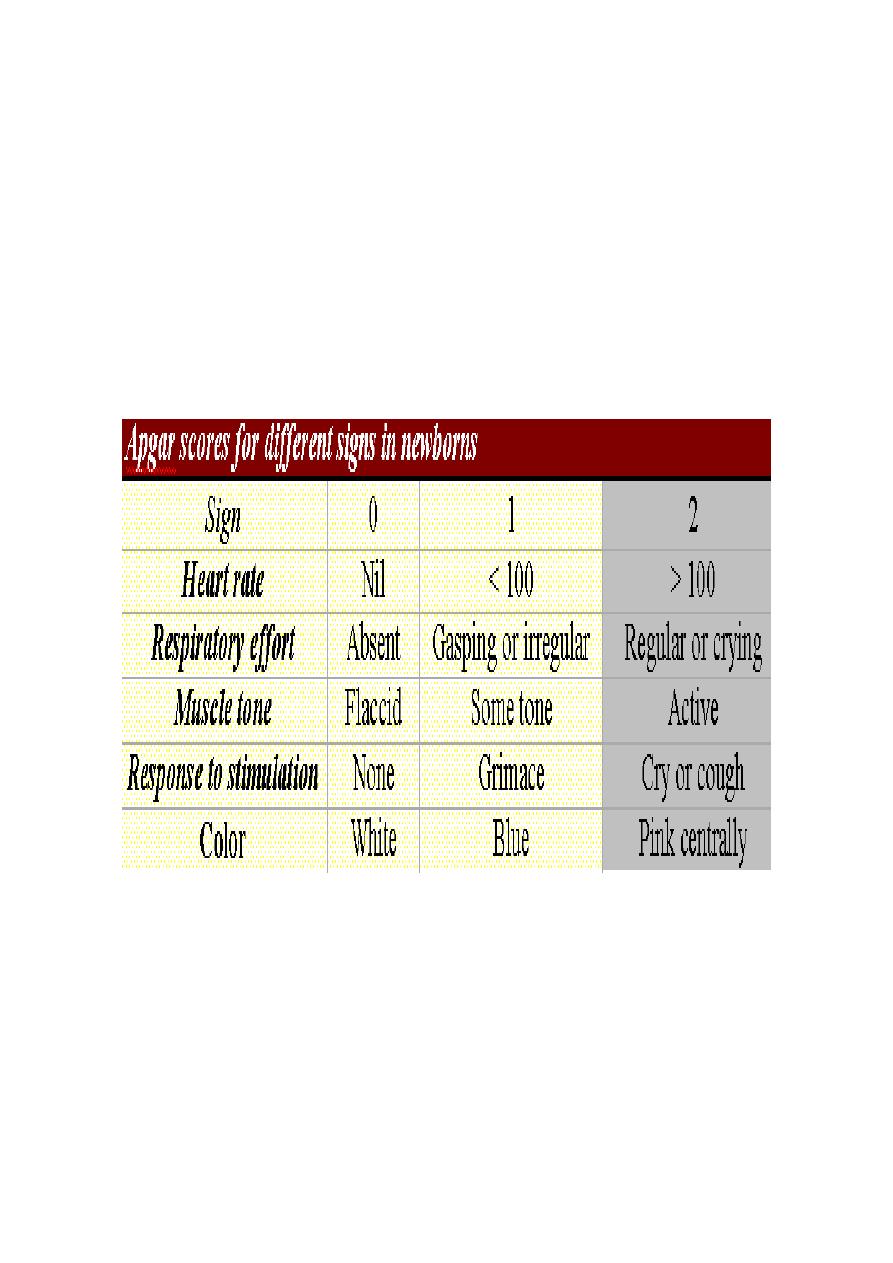
The Apgar score has been used for many years to assess an infant’s transition to
extrauterine life.
The 1-minute Apgar score reflects the infant’s intrauterine environment and
tolerance of the delivery process.
The 5-minute score reflects the success of the infant’s transition. The scores can
provide information about the initial status of the baby and the response to
interventions as well as help predict neonatal survival..
Pediatrics Dr. Ziyad
3
Fatima Ehsan
Infants who have 5-minute Apgar scores of less than 7 may require close
observation. Infants whose 5-minute Apgar scores are 3 or less need very
careful subsequent monitoring and observation, often requiring intensive care.
AFTER DELIVERY
Placing the healthy neoborn skin-to-skin on the mother’s chest immediately
after birth may facilitate breastfeeding by encouraging latch-on during the
baby’s early alert period.
Vitamin K and erythromycin eye drops administration, as well as weighing and
measuring the baby, can be delayed for 1 hour to allow this important mother-
child interaction.
FIRST EXAMINATION
The neoborn examination is essential in attempting to determine the integrity
of various organ systems and their ability to adapt successfully to extrauterine
life. Examination may reveal potentially correctable defects that may
significantly interfere with normal development.
There are three periods for consideration:
1. The baby should have a brief examination within the first few minutes of
life. Care must be taken to not unnecessarily expose the infant to
inappropriate cold stress. Attention should be given to the presence of
appropriate signs of successful transition to the extra-uterine
environment, correct sex determination and presence or otherwise of
significant congenital abnormalities. The healthy infant should then be
allowed time to be with parents.
2. A full and detailed examination should be performed within the first 48
hours of life.
3. A follow up examination should be performed later in the first week ;
focus given to current status and possible evolution of signs. like
nutritional status, cardiac examination (with reducing pulmonary
pressures), abdominal examination (food tolerance) jaundice assessment
and hip examination are all relevant and should be reassessed.
Pediatrics Dr. Ziyad
4
Fatima Ehsan
RESUSCITATION:
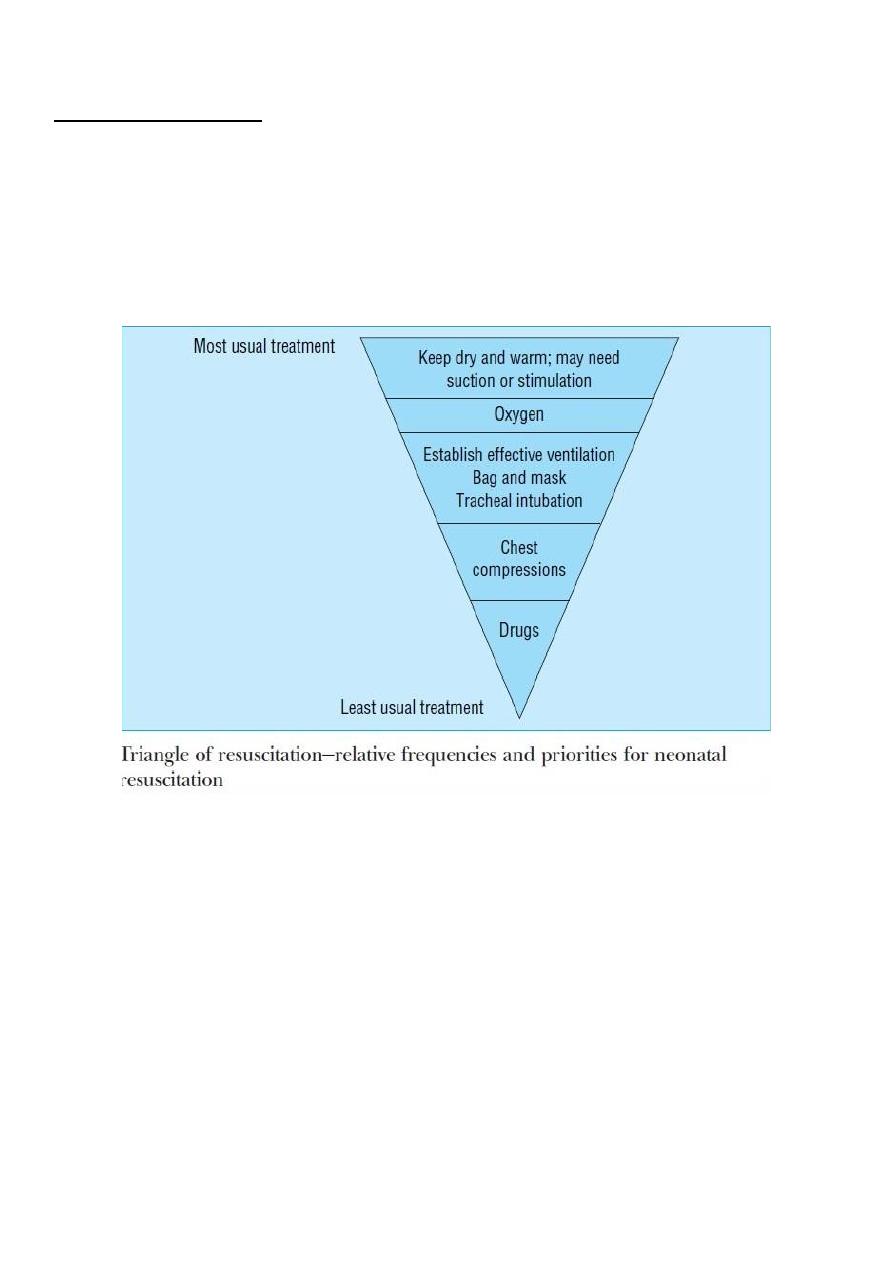
Most neoborn babies will establish normal breathing spontaneously. They need
only attention to the maintenance of their temperature and perhaps gentle
stimulation to start breathing; some may need suction of the airway, and a few
will need assisted lung inflation via a mask.
Fewer still need tracheal intubation, and very few indeed will need external
chest compression and intervention with drugs.
Before delivery it is important to check that the correct equipment is present
and functioning properly.
The room should be warm, the radiant heat source switched on, and
prewarmed towels available. The mother's case notes should be checked for
any relevant information, in particular any antenatal diagnosis made, any
relevant maternal condition, or any risk factors for infection.
Surgical gloves should be worn over clean hands to protect the baby and the
attending professional.
Pediatrics Dr. Ziyad
5
Fatima Ehsan
The baby should be assessed after birth. Even a vigorous neoborn baby may
have a marked fall in body temperature if exposed, and should be covered with
a warm, dry towel at all times
Most babies will breathe or cry within 90 seconds of birth; suction of the
pharynx is not usually necessary, nor is additional oxygen. These babies should
be handed direct to the mother.
If the baby is not breathing adequately, the ABC of resuscitation should be
followed.
Conditions in which neonatal resuscitation may be needed
1. Fetal distress
2. Thick meconium staining of amniotic fluid
3. Vaginal breech deliveries
4. Gestation of < 32 completed weeks
5. Serious congenital abnormality
6. Concern of attending staff
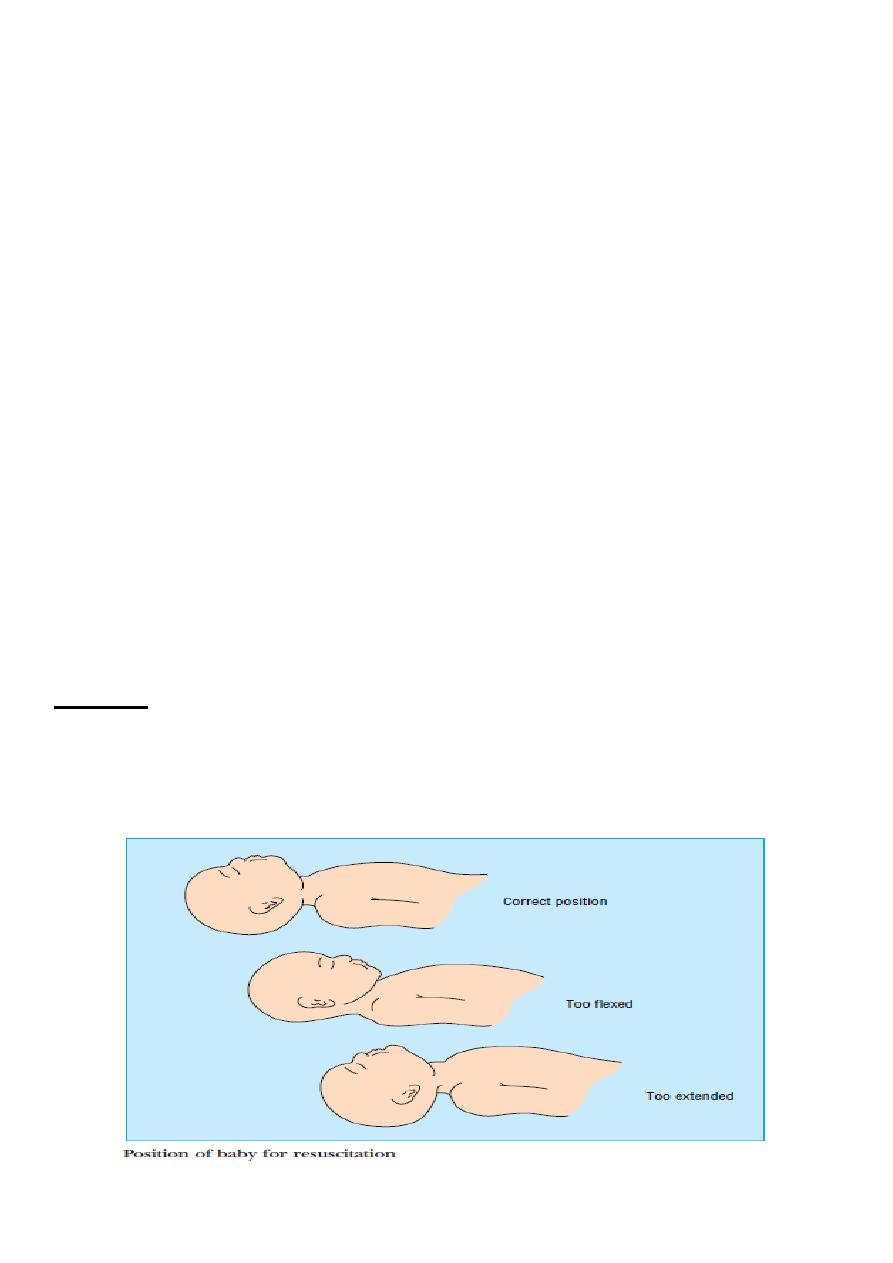
AIRWAY
The baby should be positioned face upwards with the head supported in the neutral
position. If respiratory efforts are vigorous but no breath sounds are heard, the
airway may be obstructed. Reposition the baby and gently suck out the mouth and
nostrils.

Pediatrics Dr. Ziyad
6
Fatima Ehsan
BREATHING
If respiratory efforts are shallow or slow and no meconium is present, stimulate
gently and offer supplementary oxygen if the baby is cyanosed.
If the heart rate is < 100 beats/minute or decreasing, start lung inflation via a mask. If
there is no response, prepare to perform tracheal intubation and call for help if
necessary.
CIRCULATION:
Assess the circulation by evaluating the heart rate and the color of the baby.
Monitor the heart rate by auscultation or palpation of the base of the cord.
If it is > 100 beats/minute continue assessment, but if it is < 100 beats/minute
and decreasing, start or continue positive pressure ventilation.
If the heart rate is less than 60 beats/minute, start external chest compression
and consider drugs and volume expansion.
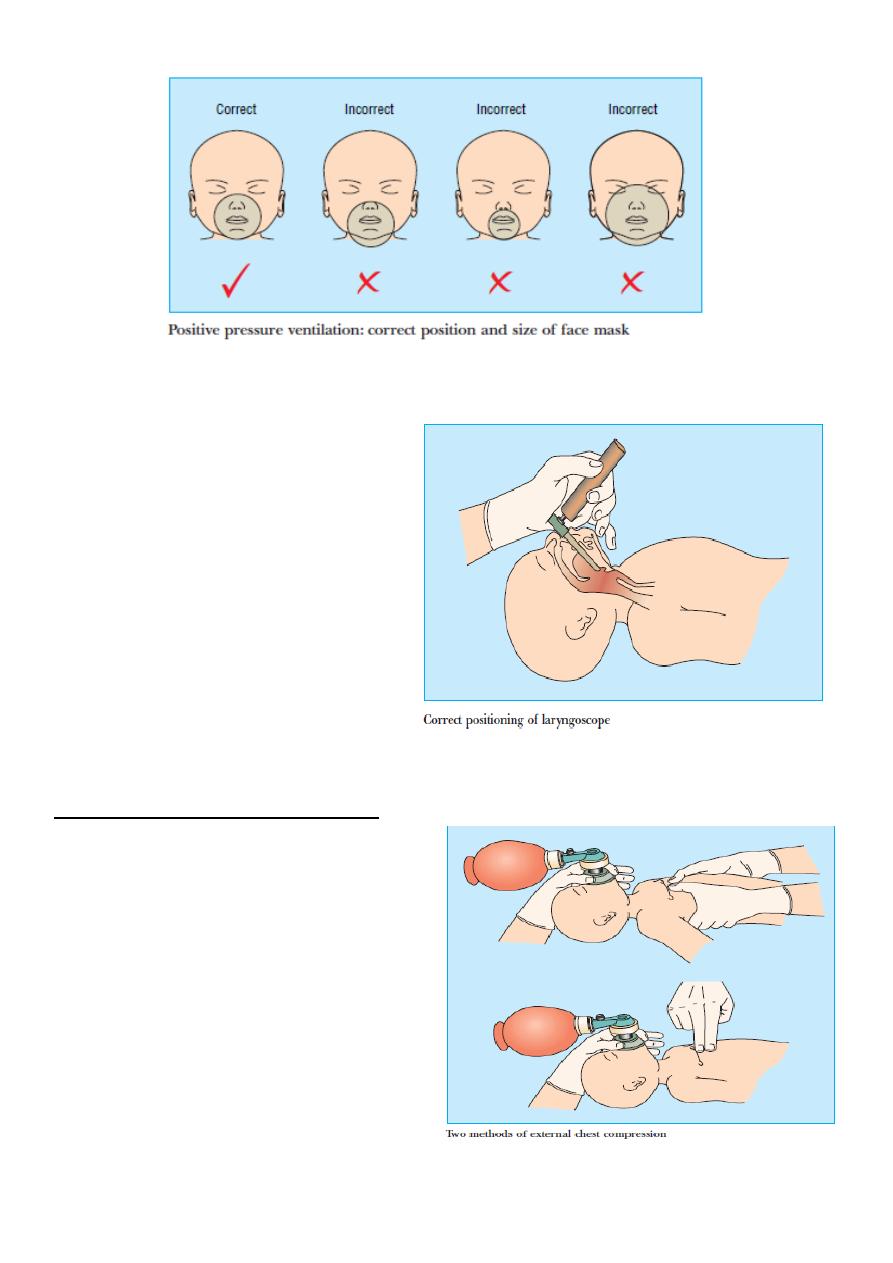
POSITIVE PRESSURE VENTILATION:
1. VIA A FACE MASK: Apply the right size face mask holding the chin gently
forward. Ventilate the lungs at a rate of 30-40 breaths per minute. See
that the chest wall moves with each inflation and listen for breath and
heart sounds.
Pediatrics Dr. Ziyad
7
Fatima Ehsan
2. TRACHEAL INTUBATION: Lift the
straight bladed laryngoscope
upwards and forwards in the
direction of the handle and keep
the vocal cords in view while
inserting an uncuffed tracheal
tube. The shoulder of the tube or
the intubation mark should be
positioned just above the cords.
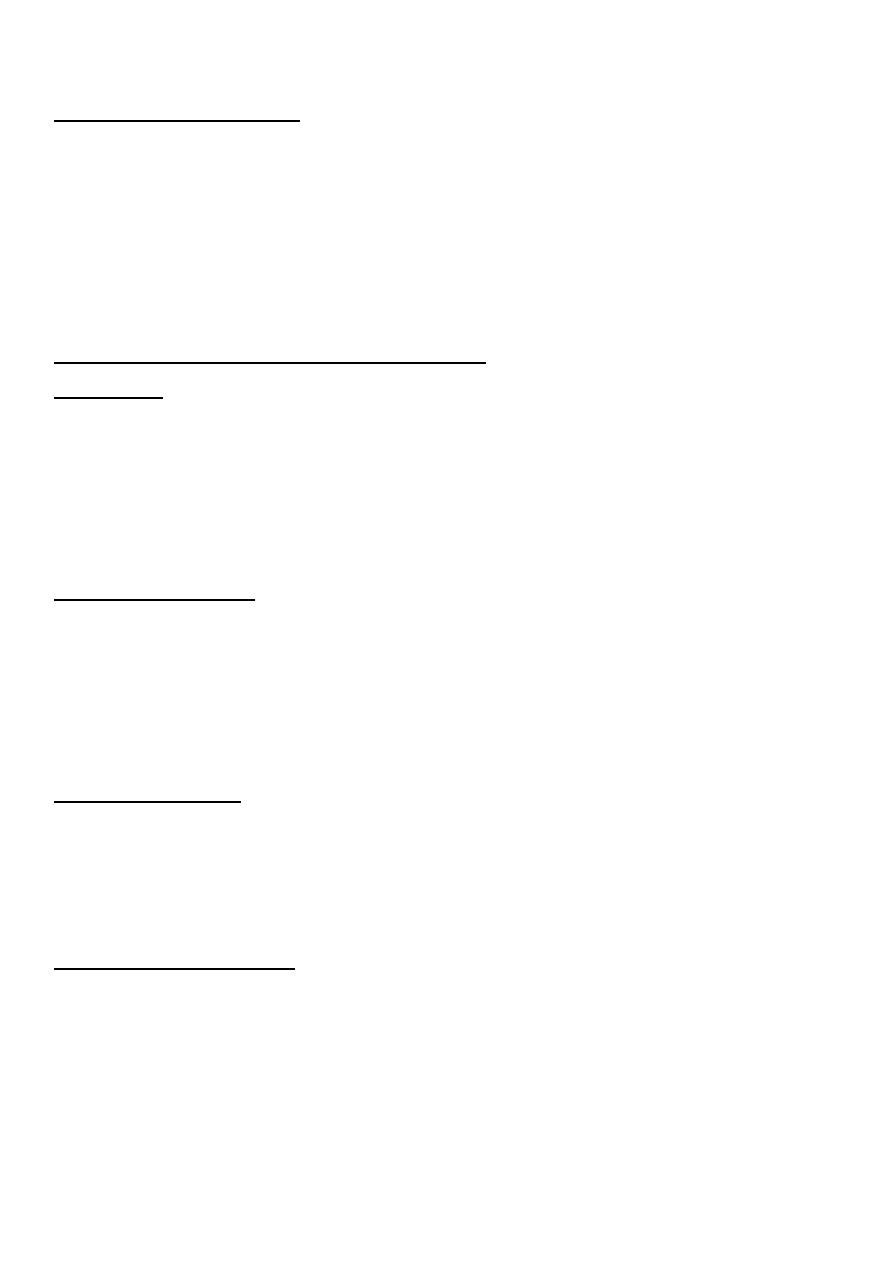
EXTERNAL CHEST COMPRESSION
Place the thumbs over the lower third
of the sternum with the hands around
the chest, or apply pressure with two
fingers. The sternum should be
compressed by about 23 cm in a term
baby at a rate of about 2
compressions per second, and the
lungs should be reinflated with oxygen
after every 3 compressions.
Pediatrics Dr. Ziyad
8
Fatima Ehsan
DRUGS AND FLUIDS
Adrenaline should be given initially, followed by sodium bicarbonate if
necessary. Hypovolaemia should be considered when there is evidence of acute
bleeding or poor response to adequate resuscitation.
Naloxone should be reserved for the apnoeic baby whose mother has received
opiate analgesia 24 hours before delivery. It is not a substitute for resuscitation.
Drugs for use in neonatal resuscitation
Adrenaline
Preparation 1 in 10 000 dilution (100 microg/ml).
Dose 1st and 2nd dose 10 microg/ml /kg (0.1 ml/kg); 3rd dose 100 microg/ml
/kg (1 ml/kg)
Route 1st dose, tracheal tube (provided that lungs are inflated); 2nd and 3rd
doses, umbilical venous catheter.
Sodium bicarbonate
Preparation 4.2% (0.5 mmol/ml) or 8.4% (1 mmol/ml) solution with equal
volume of dextrose.
Dose 12 mmol/kg (24 ml/kg of 4.2% solution) via umbilical venous catheter; 2
doses may be given.
Volume expanders
Preparations Plasma, or group O Rh negative blood that is not cross matched; 4-
5% human albumin
Dose 1020 ml/kg via umbilical venous catheter over 510 minutes (may be
repeated).
Naloxone hydrochloride
Dose 100 ìg/kg (0.25 ml/kg) intramuscularly.
Vitamin K
All babies should receive vitamin K at birth to prevent haemorrhagic disease of
the newborn.

Pediatrics Dr. Ziyad
9
Fatima Ehsan
Discharge
Most infants are ready for discharge at 48 hours after a vaginal delivery and 72
to 96 hours after a cesarean section delivery.
The infant is medically ready for discharge when:
1. he or she has stable vital signs for at least 12 hours.
2. appears healthy and has normal results on physical examination.
3. has stooled and voided.
4. is feeding well (or will be sent home after additional lactation evaluation
with a feeding plan in place).
5. has completed all screening tests.
6. and has appropriate follow-up care planned.
