Pediatrics Lec 2
1
GROWTH AND DEVELOPMENT
Growth: increase in the size of the body as whole or the increase in its
separated parts.
Development: changes (complexity) in function including those influenced
by emotional and social environments.
Within a broad limits that characterized normal development; every
individual paths of growth and development through the life cycle is
unique.
Stages of Growth and Development
Neoborn- 0 to 1 month
Infant- 1 month to 1 year
Toddler- 1 year to 3 years
Preschool- 3 years to 6 years
School age- 6 to 11 or 12 years
Adolescence- 11 or 12 years to 21 years
Normal growth pattern:
Deviations in the growth pattern are important indicator of serious
medical disorders.
Accurate measurement of height, weight, head circumference should
obtained at each health visit, serial measurement are much more useful
than single measurement.
Normal growth have spurt and plateaus, so one can expect some shifting
on percentile.

Pediatrics Lec 2
2
Rules of thumb for growth:
Weight:
Weight loss in the 1st few days of life about 5-10%.
Regain body weight at 7-10 days of age.
Double birth weight at 4-5 months.
Triple birth weight at 1 year.
Quadrupled birth weight by 2nd year.
3-12 months: weight is equal to {age ( in months)+9}/2
1-6 years: age (in year) ×2 +8
7-12 years: {age (in years) × 7 – 5}/2
Height:
At birth 50 cm
Double birth height at 4 years.
Height at 1 year: 75 cm.
2-12 years: age in years × 6 + 77
Head circumference:
At birth: 35 cm.
Increase by 1 cm per month for 1st year.
Increase 10 cm for the rest of life.
Variability in the body proportion occurs from fetal to adult life; also there
is variation between normal children often following familial pattern.
Certain growth disturbance result in characteristic changes in the
proportional size of trunk, extremities, and head.
The growth of some body organ and systems correlate closely with their
function
Ex. Growth of nervous system is most rapid in the 1st 2 years. While growth of
lymphoid tissue peaks at about 12 years
Pediatrics Lec 2
3
Assessment of growth:
Growth assessment is essential component of pediatric health surveillance,
because almost any problem within the physiological, interpersonal, and social
domain can adversely affect growth
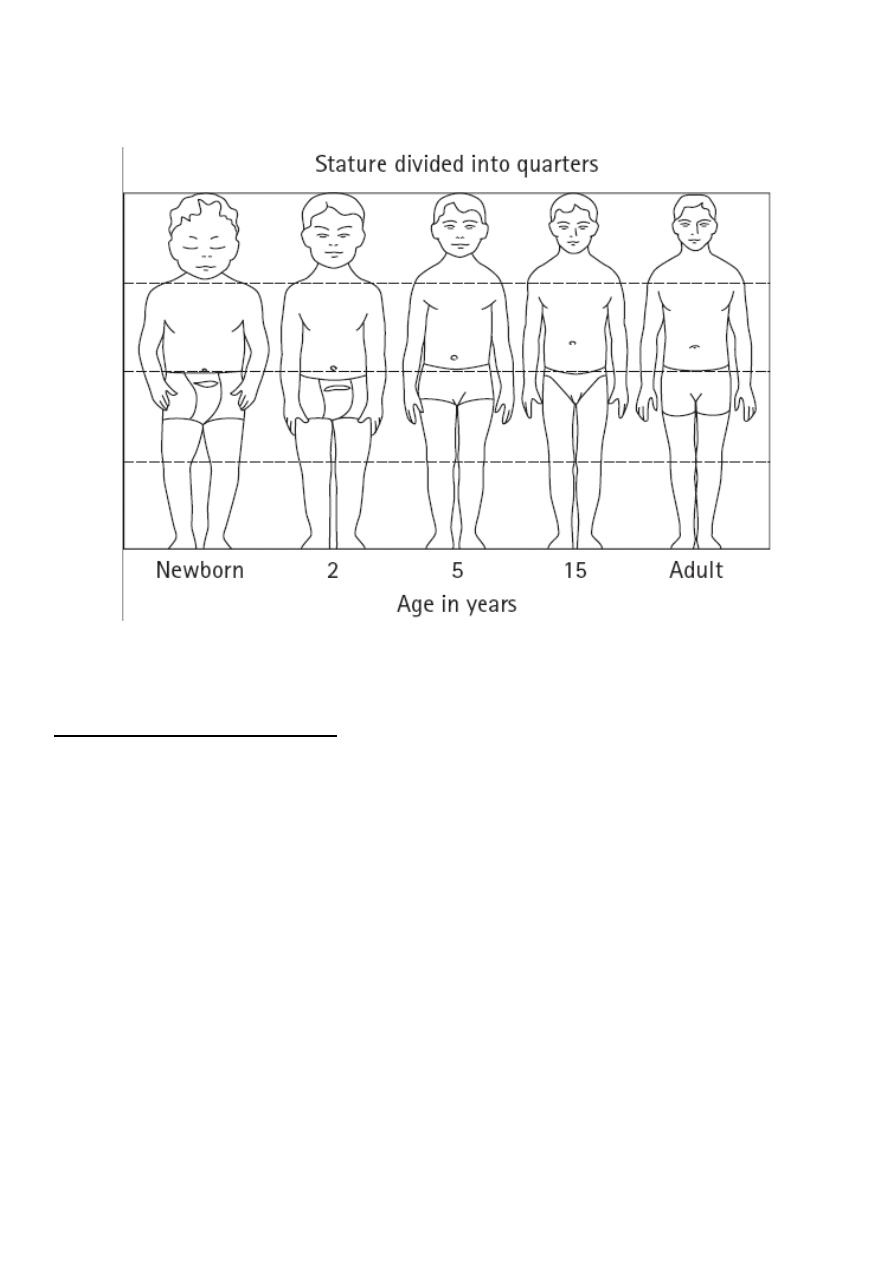
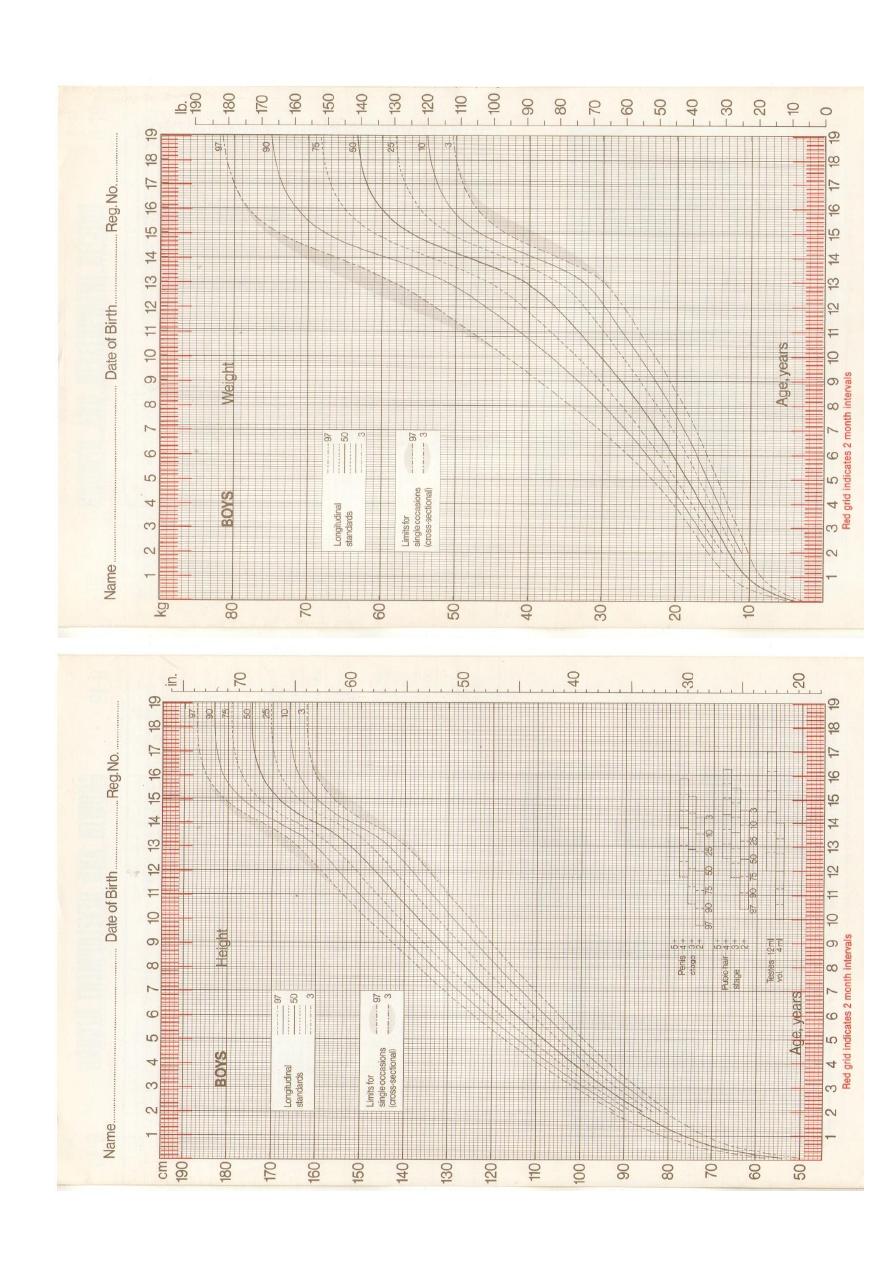
The most powerful tool in growth assessment is growth chart.
Growth data are represented in 5 five standard charts:
Weight for age.
Height for age.
Head circumference for age.
Weight for height.
Body mass index.
Separated charts are provided for boys and girls.
Pediatrics Lec 2
4
Pediatrics Lec 2
5
For infant the measure of linear growth is (length) taken by 2 examiners, with
the child supine on a measuring board
For older children the measure is (stature) taken with the child standing on
stadiometer.
Each chart composed of 7-8 percentile curve, the percentile curve indicate the
percentage of children at a given age on the X axis whose measured value falls
below the corresponding value on the Y axis.
50 percentile - by the definition- is the median; also called the standard value.
Specialized chart have also been developed for children with various condition;
including down, turner, klinefelter syndrome, and achondroplasia.
Worrisome sign that warrant attention during follow-up include:
Large shift on percentile graphs.
Large discrepancies among height weight, and head circumference.
When the caloric intake is inadequate; weight percentile fall 1st, then the
height, and last the head circumference.
Increase in the weight in the face of falling height suggests hypothyroidism.
Increase in the head circumference may suggest familial megalencephaly,
hydrocephalus.

Pediatrics Lec 2
6
Other indices of growth:
Body mass index: BMI
Body mass index: BMI Calculated as wieght/height
2
According to center of disease control and prevention (CDC):
BMI>95% indicate overweight.
BMI 85-95% risk of overweight
BMI <5 indicate underweight
BMI may not provide an accurate index for adiposity because it does not
differentiate lean tissue and bone from fat.
Measurement of skinfold thickness over triceps and subscapular region give a
better estimation of adiposity.
Body proportion:
can be assessed by measuring the lower body segment (length from symphysis
pubis to the floor) and the upper body segment (height - lower segment)
At birth U/L segment is about 1.7
At 3 years U/L segment is about 1.3
After 7 year U/L segment is about 1
High upper to lower body ratio is characteristic of short limb dwarfism or bone
disorders such as rickets
Bone age: (osseous maturation):
is determined from X ray on the bases of:
No. and size of epiphyseal center.
Size, shape, density and sharpness of outline of the end of bone.
Distance separating epiphyseal center from the zone provisional
calcification.
Bone age correspond more closely to sexual maturity (which is dependant of
growth and development of endocrine system) than chronological age.

Pediatrics Lec 2
7
Bone age correlate well with stage of pubertal development and can be
helpful in predicting adult height
In familial short stature the bone age is normal (comparable to chronological
age), in endochrinological short stature, constitutional short stature, and
undernutrition the bone age is low and comparable to height age.
Dental development:
include: mineralization, eruption, and exfoliation.
Initial mineralization begins as soon as 2nd trimester and continues through
3rd year of age for primary teeth (deciduous) and 25 years of age for
permanent teeth.
Mineralization begins at crown and progress towered the root.
Eruption begins at central incisor and progress laterally.
Delayed eruption is usually considered when there are no teeth by 13 months
of age; common causes include hypothyroidism, hypoparathyroidisim,
familial, and (most common) idiopathic.
Individual teeth may fail to erupt because of mechanical blockage (crowding,
gum fibrosis)
Exfoliation begins at about 6 years of age, and continues through 12 years.
Causes of early exfoliation include: trauma, idiopathic, histiocytosis x and
cyclical neutropenia.
The timing of dental development is poorly correlated with other process of
growth and maturation.

Pediatrics Lec 2
8
physiological & structural growth:
every organ and structure undergoes sequence of structural and functional
changes or both during development. Physiological and structural changes of
particular relevance to general pediatrics include the following:
Respiratory and pulse arte decrease shapely during the 1st 2 year.
Blood pressure rises steadily begging at approximately 6 year of age.
Development of paranasal sinuses continue through out childhood, the
ethmoid, maxillary, and sphenoid sinuses are present from birth, the frontal
sinuses 1st appear around 6 year of age the ethmoid sinus reach their
maximum size in early childhood(7-14), the other reach their maximum size
after puberty.
Lymphoid tissue develops rapidly, reaching adult size during 6 years, and
continuing to hypertrophy during childhood and early adolescence before
receding to adult size.
The metabolism of medications and the child’s response to them changes
rapidly in the 1st months of life and again under the hormonal influences in
puberty.
Nutritional need and biochemical and hematological values
undergo marked developmental changes. (Alkaline phosphatase
level increases during period of rapid growth, hemoglobin has a
physiological nadir at approximately 2 months of age.
