1 |
P a g e
A
A
n
n
t
t
i
i
b
b
i
i
o
o
t
t
i
i
c
c
s
s
Antibiotic/Antimicrobial
Antibiotic: Chemical produced by a microorganism that kills or inhibits the growth
of another microorganism
Antimicrobial agent:
Chemical that kills or inhibits the growth of microorganisms
Bactericidal Kill bacteria
• Usually antibiotic of choice for infections in sites such as endocardium or
the meninges where host defenses are ineffective.
• Bacteriostatic
• Reversibly inhibit growth
• Duration of treatment sufficient for host defenses to eradicate infection
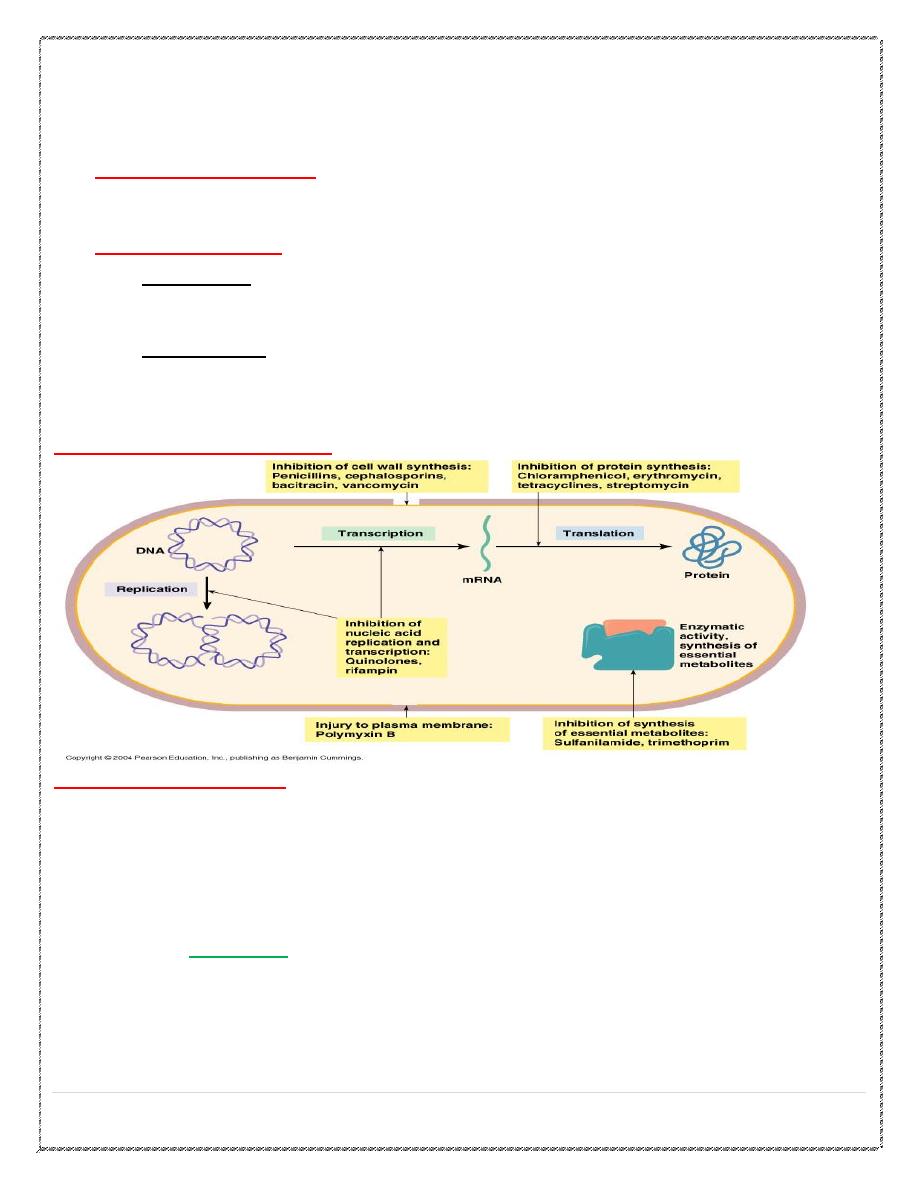
Modes of Antimicrobial Action
Principles and Definitions
•
Combination therapy
• Prevent emergence of resistant strains
• Temporary treatment until diagnosis is made
• Take advantage of antibiotic synergism
• Penicillins and aminoglycosides :inhibit cell wall synthesis and allow
aminoglycosides to enter the bacterium and inhibit protein synthesis.
•
CAUTION
: Antibiotic antagonism
• Penicillins and bacteriostatic antibiotics. Cell wall synthesis is not
• occurring in cells that are not growing.
2 |
P a g e
β- Lactam Antibiotics
1. Penicillins
2.Cephalosporins
3.Carbapenems ( Imipenems )
4. Monobactams ( Aztreonam)
β-lactam antibiotics antibiotic;
agents that contain a β-lactam ring in their molecular
structure
2 mechanism of resistance
1-Bacteria often develop resistance to β-lactam antibiotics by synthesizing a β-lactamase,
an enzyme that attacks the β-lactam ring rendering the antibiotic ineffective
2-Possession of altered penicillin-binding proteins.
some bacteria have changed the proteins to which β-lactam antibiotics bind. β-
lactams cannot bind as effectively to these altered PBPs, and, as a result,
the β-
lactams are less effective at disrupting cell wall synthesis.
examples of this mode of resistance include methicillin-resistant Staphylococcus
aureus (MRSA) and penicillin-resistant Streptococcus pneumoniae.
Penicillins
Classification
•
Narrow spectrum penicillins.
•
Antistaphylococcal penicillins.
•
Broad spectrum penicillins.
•
Extended –spectrum penicillins
( antipseudomonal penicillins).
Narrow spectrum penicillins
Penicillin G
•
Short duration.
•
Acid unstable.
•
Penicillinase sensitive.
Procaine penicillin
•
Long acting (every 12 h ).
•
Acid unstable.
•
Penicillinase sensitive.
•
Used to prevent subacute bacterial endocarditis due to dental extraction or
tonsillectomy in patients with congenital or acquired valve disease.
•
Mild streptococcal infection.
3 |
P a g e
Benzathine penicillin
Long acting (every 3-4 weeks).
Acid unstable.
Penicillinase sensitive.
Treatment of β-hemolytic streptococcal pharyngitis.
Used as prophylaxis against reinfection with β- hemolytic streptococci so prevent
rheumatic fever.
Once a week for 1-3 weeks for treatment of syphilis (2.4 million units I.M.).
Phenoxymethyl penicillin (P. V)
•
Less effective than penicillin G.
•
Acid stable.
•
Penicillinase sensitive.
•
Short acting.
•
Used in minor infections.
Penicillinase resistant to staphylococcal β-lactamase producer
Nafcillin,Meticilin, Oxacillin, Cloxacillin, Dicloxacillin.
Used in minor & severe Staph. Infections.
Broad &Extended spectrum penicillins
Aminopenicillins(Ampicillin&Amoxicillin)
Therapeutic uses:
•
1)Salmonella& Shigella infections.
•
2)Prophylaxis of infective endocarditis.
•
3) Urinary tract infections.
Carboxypenicillins (Ticarcillin) &Ureidopenicillin(Piperacillin)
Effective against pseudomonas aeruginosa & Enterobacter.
Penicillinase sensitive.
Can be given in combination with β-lactamase inhibitors as clavulanic acid ,
sulbactam, tazobactam.
Adverse effects
Hypersensitivity reactions.
High dose in renal failure ---seizure.
•
Naficillin (neutropenia).
•
Oxacillin (hepatitis).
•
Methicillin(nephritis).
•
B.S.P.(pseudomembraneous colitis ).
•
Secondary infections.
4 |
P a g e
Cephalosporins
First-Generation
•
Cefazolin, Cephalexin, cephradin.
•
They are very effective against gram- positive cocci.
Clinical uses
•
Urinary tract infections.
•
Minor Staph. infections or minor polymicrobial infections as cellulites or soft tissue
abscess.
•
Cefazolin is the drug of choice for surgical prophylaxis, also as alternative to anti
staph pencillin. In penicillin allergic patients.
Second -Generations
Cefaclor ,Cefamandole, Cefuroxime.
Less active against gram-positive bacteria than first generation.
They have extended gram –negative effect.
No effect on P-aeruginosa or E-cocci.
Clinical uses
H-influenza infections.
Mixed anaerobic infections as peritonitis.
Community acquired pneumonia.
Third -Generations
Cefoperazone, Cefixime, Ceftriaxone & cefotaxime.Cephtazidim.
•
They have extended gram- negative spectrum.
•
Have an effect on P-aeruginosa . Main route I.V. I.M
•
Cefixime can be given orally.
•
Ceftriaxone has a long half- life (7-8h).can be given once every 24h.
•
Excreted through kidney (Ceftriaxone through bile).
4th Generation Cephalosporins
•
Cefepime.
•
Extended spectrum of activity:
• Gram-positives: similar to ceftriaxone
• Gram-negatives: similar to ceftazidime (including Pseudomonas aeruginosa),
also covers beta-lactamase producing Enterobacter spp.
5 |
P a g e
•
Stable against -lactamases.
'Next generation'
•
Ceftobiprole (i.v.)
•
Ceftaroline (i.v.)
•
Have a fourth-generation spectrum enhanced to include MRSA.
Adverse Effects
•
Allergy.
•
Thrombophilibitis.
•
Interstitial nephritis and tubular necrosis mainly with cephaloridine.
•
Cephalosporins that contain a methylthiotetrazole group as cefamandole ,cefperazone
cause hypoprothrombinemia and bleeding disorders .Vit.K twice weekly can prevent
this.
•
Diarrhea.
Carbapenems
Imipenem.
Bctericidal, inhibit bacterial cell wall synthesis.
Has a wide spectrum of activity.
Sensetive to -β lactamase.
Not absorbed orally, taken by I.V.I.
Inactivated by dehydropeptidases in renal tubules, so it is given with an inhibitor of
renal dehydropeptidases, (cilastatin) for clinical use.
Penetrates body tissues and fluids including CSF.
Clinical uses
Mixed aerobic and anaerobic infections.
Carbapenem is the β lactam of choice for treatment of enterobacter infections.
Pseudomonal infections.
Intraabdominal infections.
Febrile neutropenic patient.
Septicaemia.
Meropenem
Similar to imipenem but it is highly active against gram-negative aerobes.
Not degraded by renal dehydropeptidase.
6 |
P a g e
Adverse effects
•
Nausea,vomiting,diarrhea.
•
Skin rash and reaction at the site of infusion.
•
High dose with imipenem in renal failure cause seizure.
•
Patients allergic to penicillin may be allergic to carbapenems.
Monobactams
Aztreonam
•
Active only against gram-negative aerobic bacteria.
•
Given I.V.
•
Similar to β-lactam in mechanism of action and adverse effects.
Macrolides
•
Erythromycin.
•
Clarithromycin.
•
Azithromycin.
•
Act on 50S ribosome to block protein synthesis.
•
Hepatic excretion - no dose adjustment for renal failure.
•
Bacterostatic for most bacteria.
Macrolides - Spectrum of Activity
•
MSSA.
•
Streptococcus.
•
H. influenzae (Azithromycin best).
•
Mycoplasma pneumoniae.
•
Chlamydia spp.
•
Legionella (Azithromycin best).
•
Atypical mycobacteria (Clarithromycin and Azithromycin).
Erythromycin - Side effects
•
GI: abd. Cramps, nausea, vomiting, diarrhea - IV or PO.
•
Cholestatic hepatitis.
•
Rash, fever, eosinophilia - sometimes accompanies hepatitis.
•
Transient hearing loss - more common with high doses in elderly or renal insuf.
Clarithromycin/Azithromycin - Side effects
•
Much less than erythromycin.
•
GI: nausea, vomiting, abd. Cramps.
•
Abnormal liver functions.
7 |
P a g e
•
Head Ache, dizziness.
•
Reversible hearing loss at high doses.
Macrolides - Drug Interactions
•
Inhibit drug metabolism through the cytochrome P450 system.
•
Increases drug levels.
•
Erythromycin>Clarithromycin>Azithro
•
Erythromycin can cause serious, life-threatening drug toxicity.
•
Azithromycin has almost no drug-drug effect.
Tetracyclines
•
Tetracycline.
•
Doxycycline.
•
Minocycline.
•
Demeclocycline.
•
Bind to 30S ribosome to inhibit protein synthesis.
•
Bacterostatic against bacteria.
Tetracyclines - Drug of Choice :
•
Borrelia - Lyme Dz, relapsing fever.
•
Chlamydia - psittacosis, STD, pneumonia.
•
Rickettsia -, typhus, Q fever.
•
Brucellosis.
•
Vibrio – cholera.
•
Mycoplasma/Ureaplasma.
Tetracyclines - Side Effects
•
Skin - allergic rash, photosensitivity.
•
Teeth & Bones - yellow discoloration in kids (don’t use in pregnancy or kids <8 yrs).
•
GI - N/V/D, esophageal ulcerations
• decreased side effects with food, but food also decreases absorption.
•
Liver and kidney toxicity rare, but reported.
•
Minocycline – vertigo.
Chloramphenicol
Released in 1949
Binds to 50S ribosome to inhibit protein synthesis
Only bacterocidal vs H. influenzae, S. pneumoniae, N. meningitidis, otherwise
bacterostatic
8 |
P a g e
Reversible bone marrow suppression
Common
Dose-related
Due to inhibition of mitochondrial protein synthesis
Indiosyncratic aplastic anemia
Usually fatal
Occurs 1 in 24,500 to 40,800 patients
Not dose related
Occurs more commonly occurs weeks to months after therapy
Aminoglycosides
•
Bactericidal antibiotics.
•
Inhibits protein synthesis by binding to 30S ribosomal subunits.
•
Active against gram negative aerobic organisms.
•
Poorly absorbed orally.
•
Given parenterally (I.M,I.V.).
•
Excreted mainly unchanged in urine.
•
Have common adverse effects :
•
Ototoxicity.
•
Nephrotoxicity.
•
Neuromuscular blocking effect.
•
CNS (not common).
Clinical uses
Streptomycin
T.B. in combination with other antituberculous drugs.
Enterococcal endocarditis with penicillin.
Severe brucellosis with tetracycline
Gentamicin
Severe infections caused by gram negative organisms as sepsis ,urinary tract
infections & pneumonia caused by pseudomonas.
Topically for the treatment of infected burns,wounds,skin lesions,ocular, ear
infections.
Tobramycin
More active against pseudomonas than gentamicin.
Less nephrotoxic and ototoxic than gentamicin.
Used in treatment of bacteremia, osteomyelitis and pneumonia.
Amikacin
Has the broadest spectrum.
Used for serious nosocomial infections by gram negative organisms.
In T.B. as alternative to streptomycin.
Atypical mycobacterial infections.
9 |
P a g e
Contraindications of aminoglycosides
•
Renal dysfunction.
•
Pregnancy.
•
Diminished hearing.
•
Myasthenia gravis.
•
Respiratory problems.
FLUOROQUINOLONES (Ciprofloxacin, ofloxacin, norfloxacin
•
Mechanism of action:
•
Block bacterial DNA synthesis by inhibiting bacterial topoisomerase11(DNA gyrase )
and topoisomerase 1V.
•
Antibacterial activity :
•
Highly active against gram-negative aerobic bacteria.
•
Active against gram-positive bacteria.
•
Mycoplasma, chlamydia, legionella, mycobacteria.
Clinical uses
•
U.T.I.caused by multidrug resistance organisms as pseudomonas.
•
Bacterial diarrhea.
•
Soft tissues,bones,joints,intra-abdominal, respiratory infections caused by multidrug
resistance organisms.
•
Gonococcal infections.
•
Legionellosis.
•
Chlamydial urethritis or cervicitis
•
T.B & atypical T.B.
Adverse effects
•
N.V.D.
•
Headache, dizziness,insomnia.
•
Skin rash ,abnormal liver enzymes.
•
QT prolongation.
•
Damage growing cartilage causing arthropathy.
•
Tendinitis in adults.
Contraindications
•
contraindicated in children ,adolescents ,pregnancy ,lactation ,epileptic patients.
10 |
P a g e
Other inhibitors to cell wall synthesis
Vancomycin
•
Bactericidal.
•
Active only on gram +ve bacteria.
•
Poorly absorbed orally.
•
Given by I.v.I.
•
Not freely cross BBB.
•
Excreted mainly through kidney.
Clinical uses
•
Endocarditis mainly caused by methicillin –resistant staphylococci.
•
Alternative to penicillin in enterococcal endocarditis( in combination with
gentamicin).
•
Meningitis( in combination with ceftriaxone or rifampin in highly resistant
pneumococcus strains).
•
Orally in antibiotic associated enterocolitis.
Adverse effects
•
Irritation at the site of injection.
•
Ototoxicity & nephrotoxicity.
•
Red man or red neck syndrome.
•
Gastric upset.
