Failure to thrive
• objectives :-♣ To define failure to thrive (FTT).♣ To identify major classification of FTT.♣ To discuss diagnostic work up of FTT.♣ To discuss treatment of FTT.♣ To discuss complications of FTT.
♣ definition :- -physical growth that is significantly less than that of peers .
Growth Parameters
weightlength
Head
circumference
Weight
height
Does all these parameters fall at one time ?
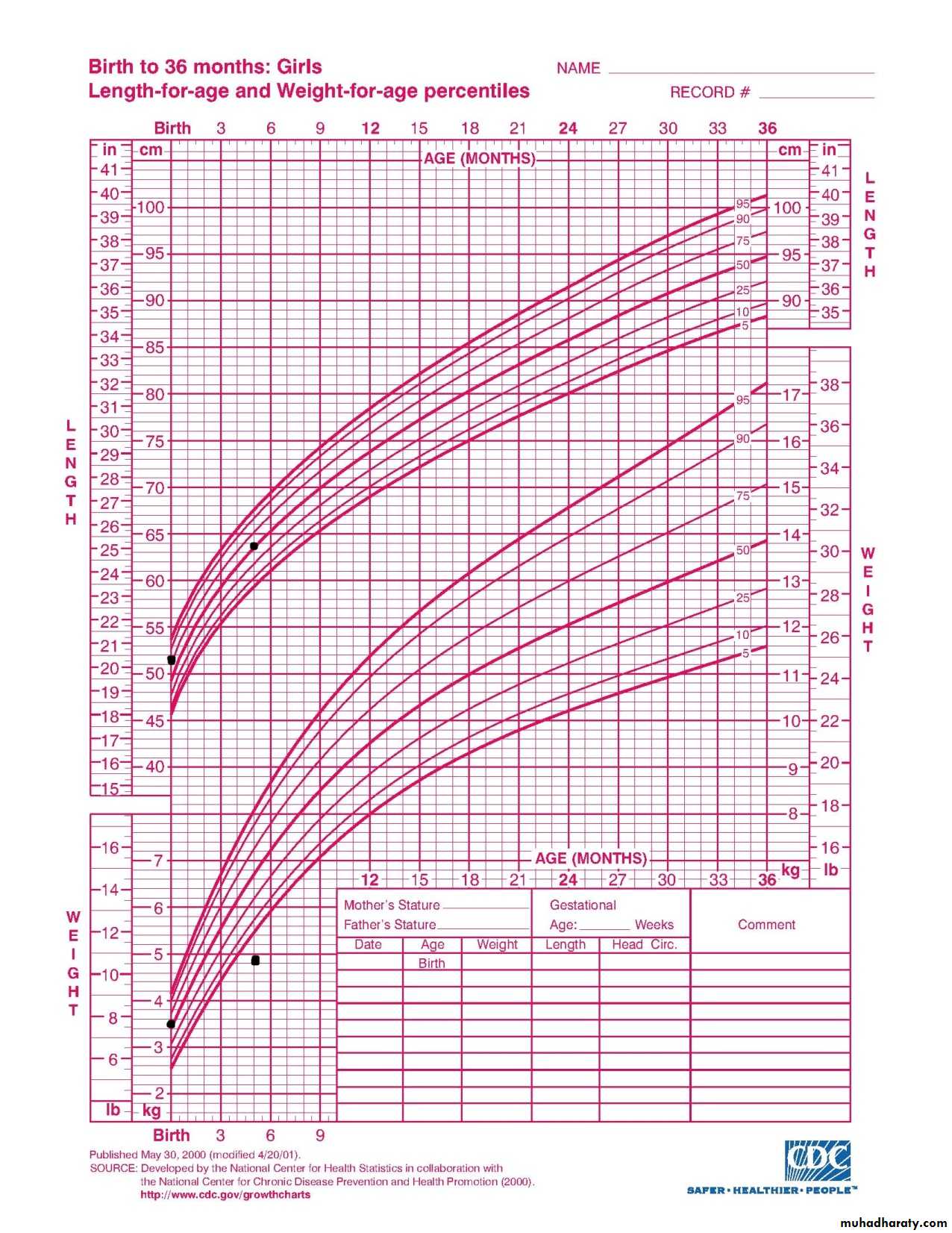
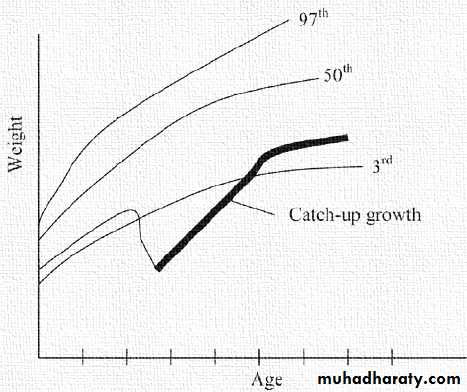
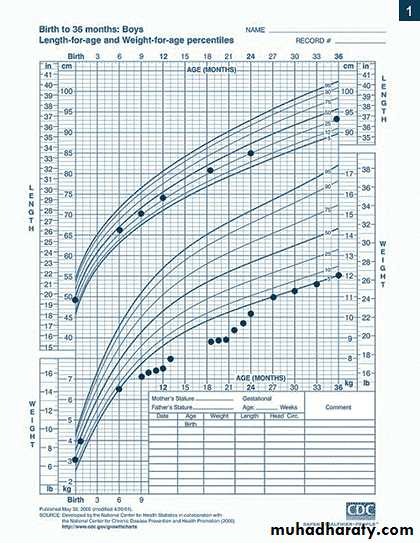
► in children FTT, malnutrition initially results in wasting (deficiency in weight gain) , ► stunting (deficiency in linear growth) generally occurs after months of malnutrition , ►head circumference is spared except with chronic severe malnutrition .♣ criteria :- ● weight below the 5th percentile for age on the growth chart . OR ● weight that deceases, crossing two major percentile lines on the growth chart over time . OR ● weight that is less than 80% of the median weight for height of the child .
♣ Epidemiology :- ● FTT affect 5-10% of young children and approximately 3-5% of children admitted to the teaching hospitals .
♣ Classification :-
Causes of organic failure to thriveMechanism
disorder
Decrease nutrient intake
Cleft lip or palate, cerebral palsy, gastroesophageal reflux, pyloric stenosis
malabsorption
Celiac disease, cystic fibrosis
Inflammatory bowel disease
Impaired metabolism
Galactosemia, fructose intolerance
Down syndrome and turner syndrome
Increase excretion
Diabetes mellitus, proteinuria
Increased energy requirements
Infections, heart failure, hyperthyroidism
Non organic failure to thrive
- Its due to poverty, psychosocial problems in the family, improper formula preparation, improper mealtime environment, unusual parental nutritional beliefs . .
Evaluation of a child with FTT
♣ Review of systems
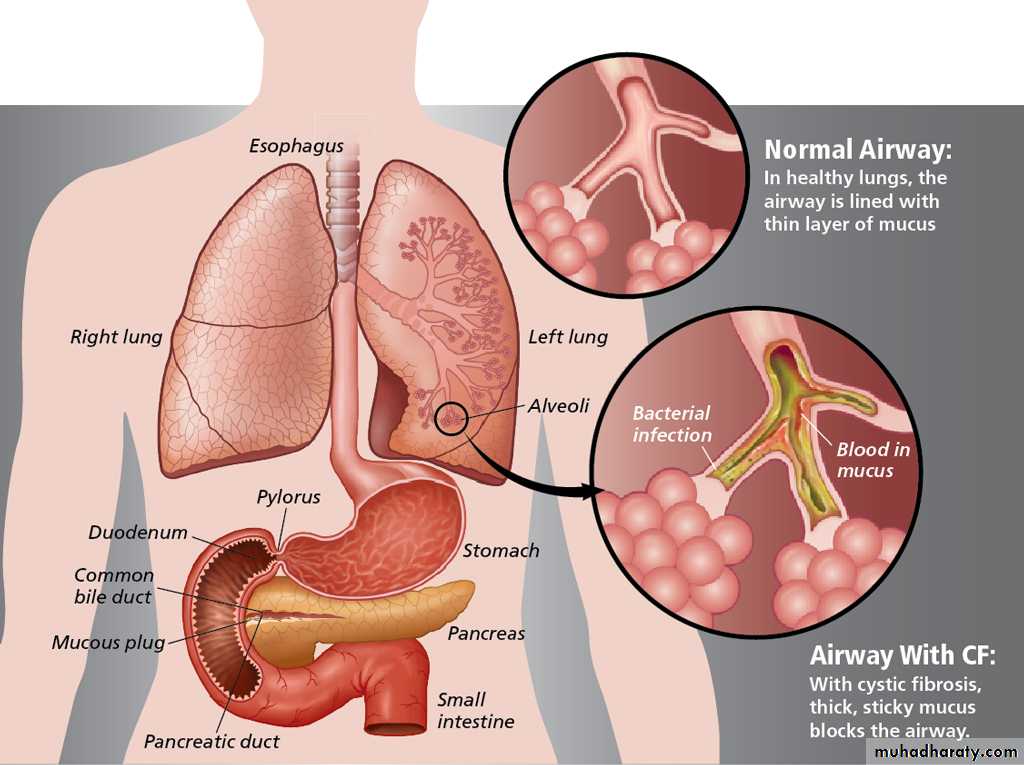
Clues to organic diseases( Dyspnea, Cough, Sputum, Hemoptysis ) Cystic fibrosis
1.respiratory►lungs :Decrease mucociliary clearance result in build up mucus within the bronchial tree causing airway obstruction and superadded infection
►increase mucus that obstruct the ducts of the exocrine glands which produce the digestive enzymes, causing malabsorption.
2.Cardiovascular
( Dyspnea, orthopnea, cyanosis, palpitation ) congenital heart disease►hypoxia and breathlessness may lead to feeding problems .
►peripheral anoxia and acidosis may lead to insufficient utilization
of nutrients.
►increase basal metabolic rate that require increase energy intake.
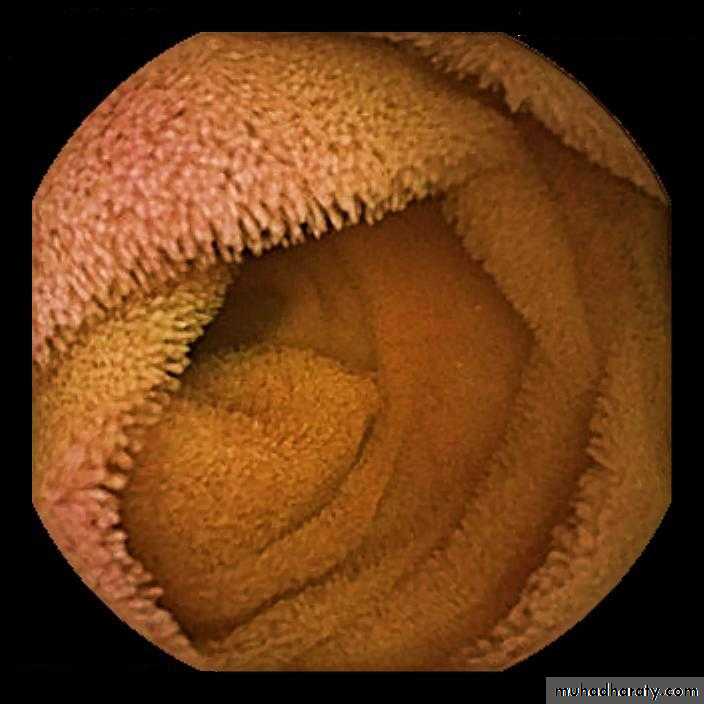
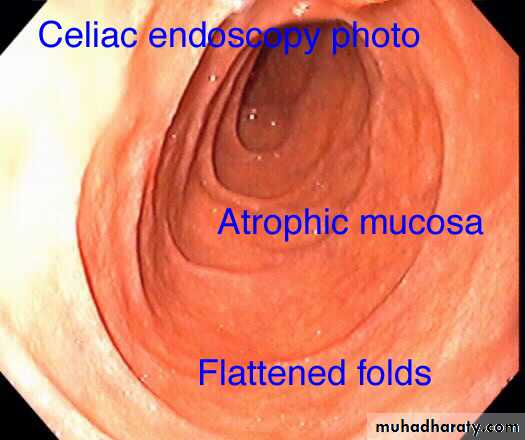
(Decrease appetite, chronic diarrhea, chronic constipation, abdominal distention, vomiting ) celiac disease.
3.Gastrointestinal
►autoantibodies cause damage to the villi result in
malabsorption .
( oliguria, hypertension, headache, nausea and vomiting ) chronic renal failure
4.Genitourinary system► creating an imbalance of sodium, potassium, and acid-base levels in the blood, also called acidosis. When blood is not balanced, the body slows growth to focus energy on restoring the balance.
►decreasing appetite, nausea, vomiting .
►decrease production of erythropoietin so the child develop anemia.
( seizures, intellectual impairment, abnormal posture, abnormal movement, communication and behavior difficulties ) cerebral palsy
5.Nervous system
►Unable to suck, swallow or chew .
1.General obstetrical history2. Recurrent miscarriages
3.Use of medications, drugs, cigarettes.prenatal
1.Neonatal asphyxia
2.Prematurity
3.Birth weight
4.Congenital malformations or infections
5.Breast feeding support
6.Feeding difficulties during neonatal period .
Delivery, postnatal
Nutritional history
● Details of feeding (breast feeding or formula feeding, formula preparation, volume consumed, who feeds the infants, position and placement of the infant for feeding, timing and introduction of solids, stool or vomiting patterns associated with feeding, strength of suck. Accurate measurement of caloric intake )●Vitamin and mineral supplements ●Weaning and introduction of solid food● food likes and dislikes, allergies
●family history of failure to thrive in previous sibling ●family history of congenital diseases.●source of water supply
Family history
Social history
general examination :-1.degree of malnutrition . 2.dysmorphic features may suggest genetic cause.3.clues for psychosocial etiology .4.signs of possible child abuse ( skin rash, injuries, fractures ) .5.signs of parents neglect ( neglected hygiene, diaper rash, unwashed skin, dirty fingernails ).6.vital signs 7.growth chart
systemic examination ♦ Suggested by the
To detect the underlying
Tests :-1.complete blood count (cbc)2.serum electrolytes 3.urinalysis and urine culture .4.hormone studies, include thyroid function test5.x-ray to determine bone age ..
♦ other investigations done according to the history and examination :-►cystic fibrosis -sweat test (sweat chloride > 60 mmol/L).►celiac disease -tTG-IgA (anti-tissue transglutaminase antibody)- small intestine biopsy to confirm the diagnosis.►congenital heart disease -echocardiography►chronic renal failure- RFT, ultrasound, VCUG, biopsy .►cerebral palsy-CT, MRI, DTI(diffusion tensor imaging), FT(fiber tractography)
guidelines :- 1.improve the child's diet and eating pattern .2.improvement in the care-givers skills .3.treat the underlying disease .4.regular and effective follow up .
admit or not :-►children with mild malnutrition can be managed by the primary care physician in the outpatient setting .►children with severe malnutrition require hospitalization for evaluation and proper treatment .
diet and eating pattern :-● children with FTT may require more than 1.5 times the expected calorie and protein intake for their age for catch-up growth .● children with FTT who are anorexic may not be able to consume this amount of food and require energy-dense foods .● for formula-fed infants, the concentration of formula can be changed from 20 cal/oz to 24 or 27 cal/oz ●for toddlers adding butter, oil, peanut butter, or other high-calorie foods .●In addition, vitamin and mineral supplementation is needed, especially during catch-up growth .
follow up :- ● the first priority is to achieve an ideal weight-for-age .● the second goal is to attain a catch-up in length expected for the child age .● depend on the severity of malnutrition initiation of catch-up growth may take 2 weeks .● for children with chronic, severe malnutrition, many months are needed to reverse all trends in growth .● Although many children with FTT eventually reach normal size, they continue to be at risk for developmental, learning, and behavioral problems .
1.malnutrition-infection cycle2.refeeding syndrome 3.psychsocial short stature
Malnutrition-infection cycle :--malnutrition causes defects in host defenses. Conversely, infection increases the metabolic needs of the patient and is often associated with anorexia. Children with FTT may suffer from a malnutrition-infection cycle, in which recurrent infections exacerbate malnutrition, which leads to greater susceptibility to infection. Children with FTT must be evaluated and treated promptly for infection and followed closely .
refeeding syndrome :-- etiology:- during starvation, the body slows the metabolic processes and growth to minimize the need for nutrients, also the body maintains homeostasis and normal serum concentration of electrolytes. With rapid reinstitution of feeding fluid and electrolyte homeostasis may be lost.-these changes may include :fluid retention, hypophosphatemia, hypomagnesaemia, hypokalemia .-can result in life-threatening cardiac, pulmonary, or neurological problems .-can be avoided by slow institution of nutrition, close monitoring of serum electrolytes during initial days of feeding, and proper replacement of depleted electrolytes.
Psychosocial short stature -children who live in psychosocial deprivation develop short stature .Etiology : endocrine dysfunction is often identified in affected children, who may have decrease growth hormone secretion and muted response to exogenous growth hormone.-Signs and symptoms : polyphagia, polydipsia, vomiting .The affected children are often shy and passive and are typically depressed and socially withdrawn. -treatment : removal of the child from the adverse environment result in rapid improvement in endocrine function and subsequent rapid somatic and pubertal growth of the child.
Case study :--A 20-month-old boy presented to his primary physician with a history of failure to thrive. He was born full term at 3.1 kg and was breast-fed, with diet advanced to solids at appropriate times. Poor weight gain was first noticed around 9 months. At that time, a complete blood count (CBC) was normal, as were electrolytes, liver enzymes, and thyroid stimulating hormone. Stool cultures for bacteria were negative, and ova and parasites were not done. Feeding practices were reviewed, and the home environment was assessed. At 12 months, the child’s diet was supplemented with PediaSure, due to continued poor growth. He experienced a slight, but transient improvement in growth rate. Consequently, he was referred to gastroenterologist.
-By history, the child was an active boy, he had a good appetite and enjoyed all table foods. There was no history of vomiting or diarrhea. He passed three to four large stools per day, which smelled quite badly. He did not attend day care and the family had no pets. His parents were non-consanguineous . He had a 10-year-old healthy brother who was growing properly. However, his brother had been treated for a Giardia infection several years ago. The family lived in a rural community and use municipal water for drinking.-Examination revealed normal vital signs, a weight of 8.9 kg (significantly below the 5th percentile) and a height of 82 cm (25th percentile).
-His physical examination revealed a small, but adequately nourished child, with clear lungs, no cardiac murmurs, a soft, mildly protuberant abdomen without masses nor organomegaly, normal bowel sounds, and no cutaneous lesions. Laboratory tests revealed a normal CBC, erythrocyte sedimentation rate (ESR), electrolytes, liver function test, total protein, albumin, and a normal urinalysis.