1
Medicine Dr. Sabah
CORONARY ARTERY DISEASE (ANGINA)
ASYMPTOMATIC------SUDDEN DEATH
1.
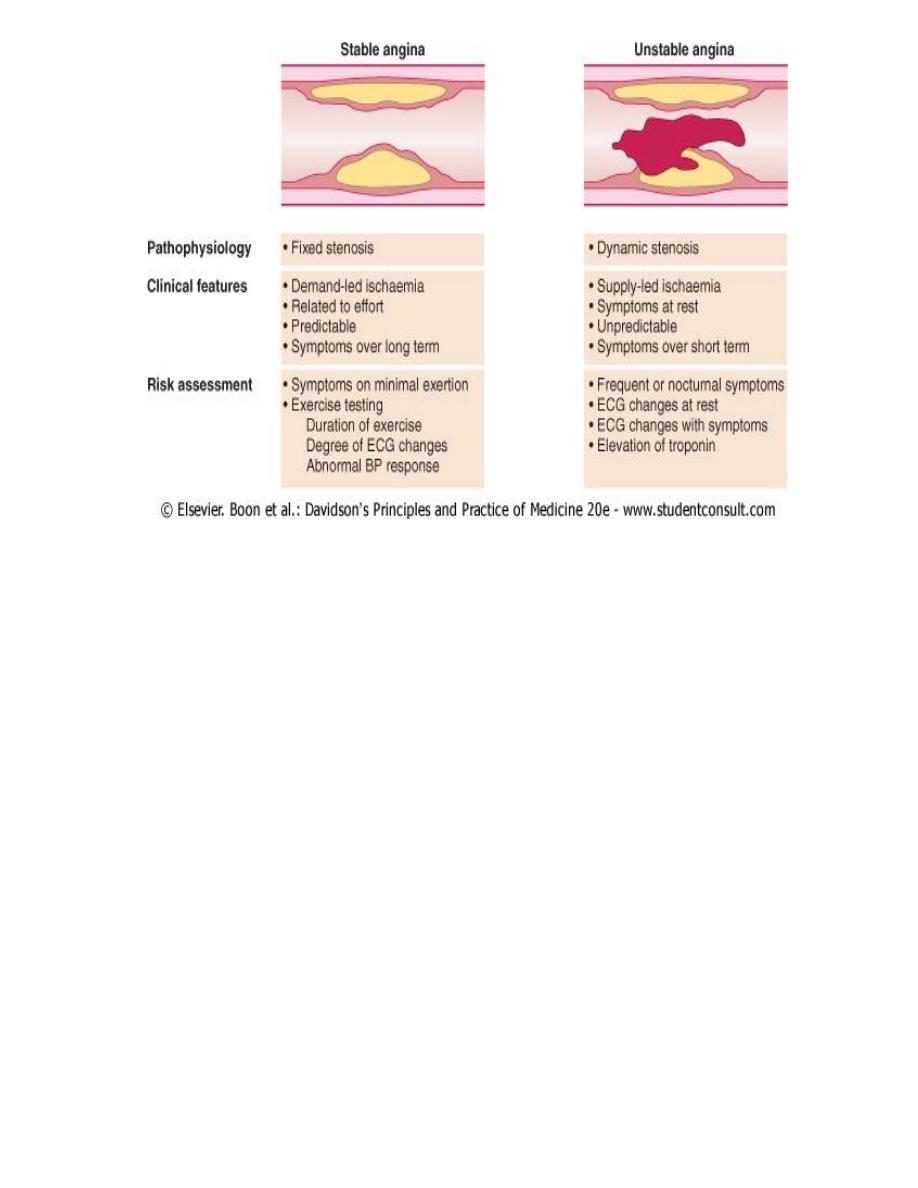
Stable angina
= Ischaemia =fixed atheromatous stenosis
2.
Unstable angina
= dynamic obstruction of CA =plaque rupture or erosion with superimposed
thrombosis
3.
Myocardial infarction
Myocardial necrosis =acute occlusion of a CA (plaque rupture or
erosion with superimposed thrombosis)
4.
Heart failure
= Myocardial dysfunction (infarction or ischaemia)
5.
Arrhythmia
Altered conduction ( ischaemia or infarction)
6.
Sudden death
// Ventricular arrhythmia// Asystole or// Massive MI
Epidemiology of Coronary heart disease (CHD)
Incidence= most common form of heart disease
In UK (population 59 million) yearly 330 000 people have a myocardial infarct
1.3 million people have angina.
Death and CAD
1) single most important cause of premature death( in Europe, Baltic states, Russia, North and
South America, Australia and New Zealand(.
2) major cause of death in all regions of the world by 2020
In the UK ,1 in 3 men and 1 in 4 women die from CHD Death rates from CHD in UK are amongst
highest in Western Europe (>140 000 people) but are falling, particularly in younger age groups;
last 10 years CHD mortality has fallen by 42% among UK men and women aged 16-64.
Aetiology
Almost always = Atheroma (and its complications, particularly thrombosis) Occasionally other
disorders : Aortiti, Polyarteritis , Connective tissue dis
ANGINA PECTORIS
O Epidemiology &Aetiology
O Types- Stable angina -unstable angina -variant angina (coronary spasm) -syndrome X
O Clinical manifestations
O Diagnosis—ECG --Angiography
2
O Management –Medical
--interventional & surgical
TYPES
1) STABLE ANGINA
2) UNSTABLE ANGINA=(ACUTE CORNARY SYNDROM=MI+UA)
3) VARIANT ANGINA(CORONARY SPASM-Prinzmetal's angina )= (ANGINA WITH NORMAL
CORONARIES)- SYNDROME X VARIANT ANGINA
DFINITION
symptom complex caused by transient myocardial ischaemia
constitutes a clinical
syndrome (vs.disease).
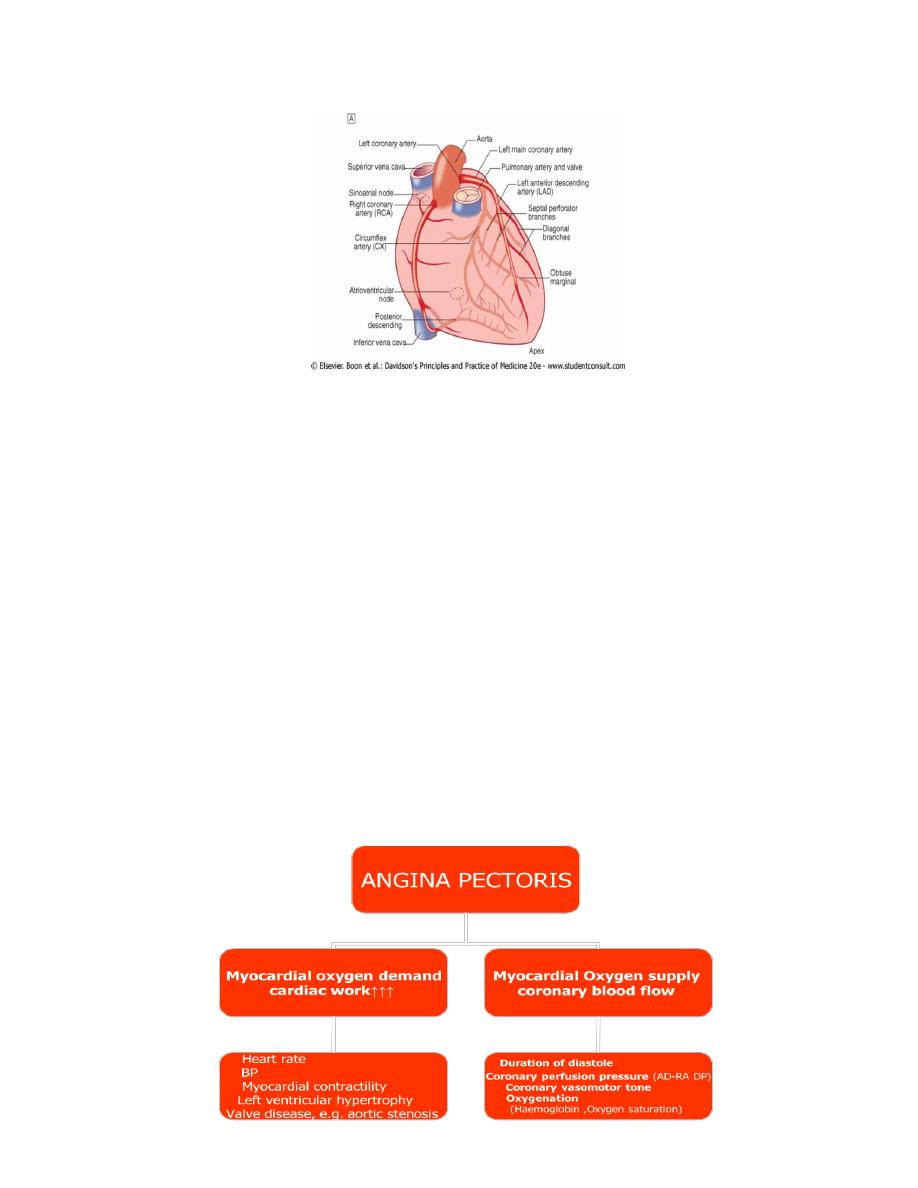
Mechanism=
imbalance between myocardial oxygen supply & demand
Aetiology:
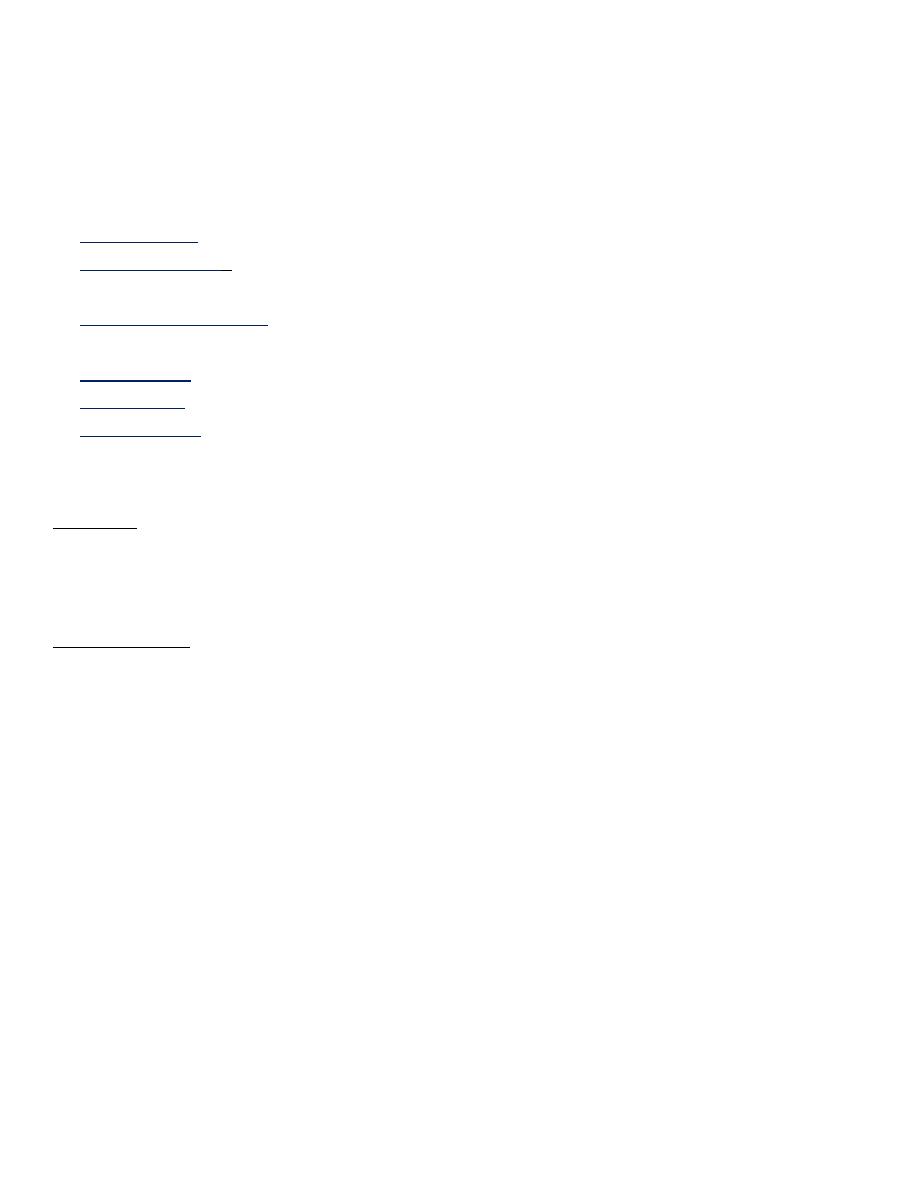
1. Coronary atheroma =most common cause of angina,
2. manifestation of other forms of heart disease, particularl aortic valve disease & hypertrophic
cardiomyopathy.
Mechanism

3
Clinical features
History
most important factor in making diagnosis.
1. characterised by central chest pain discomfort or breathlessness
2. precipitated by exertion or other forms of stress =
Common
Physical exertion
Cold exposure
Heavy meals
Intense emotion
Uncommon
Lying flat (decubitus angina)
Vivid dreams (nocturnal angina)
3. promptly relieved by rest .
Some patients -discomfort comes when they start walkin later it does not return despite greater
effort ('warm-up angina').
Physical examination
frequently negative.
1) evidence of valve disease (particularly aortic),
2) important risk factors (e.g. hypertension, diabetes),
3) LV dysfunction (e.g. cardiomegaly, gallop rhythm),
4) other manifestations of arterial disease e.g. carotid bruit peripheral vascular disease
5) unrelated conditions that may exacerbate angina e.g. anaemia, thyrotoxicosis
Investigations
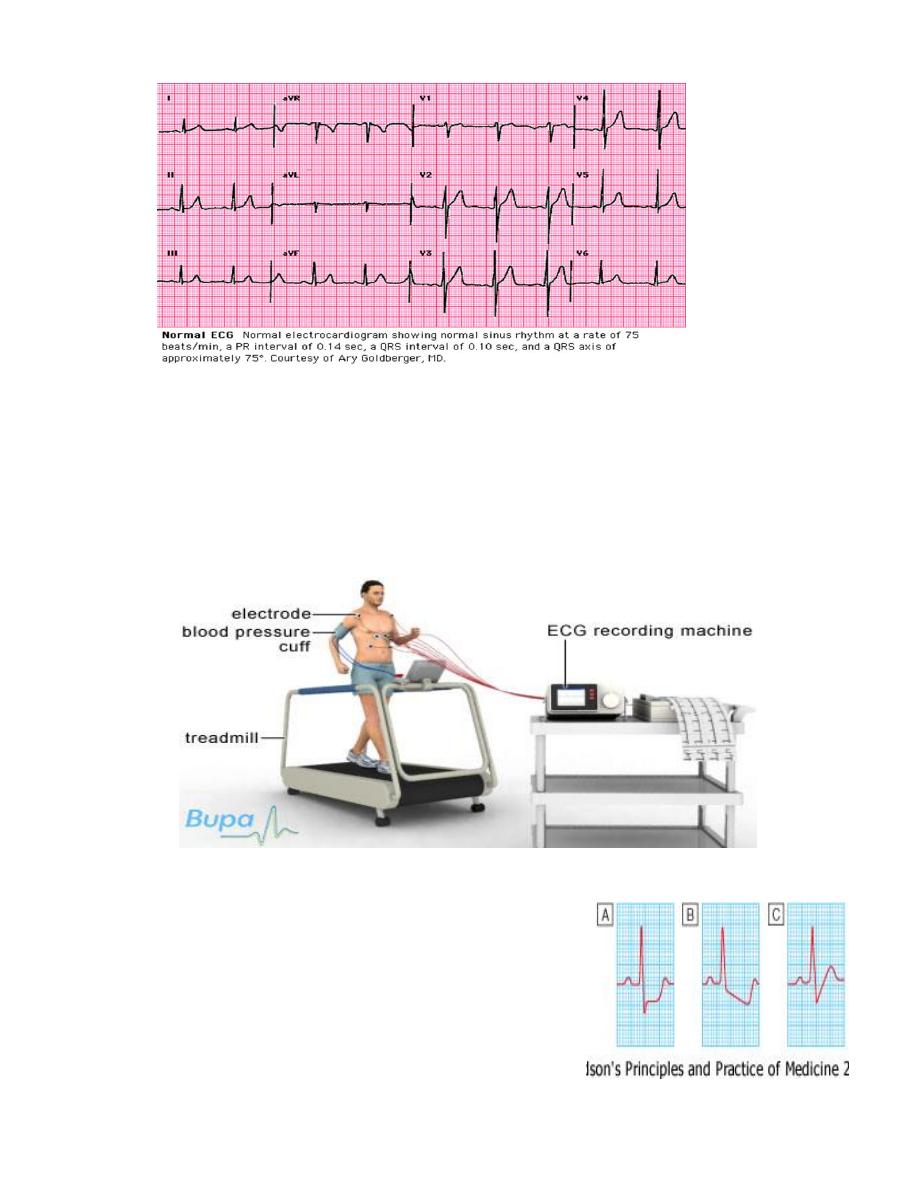
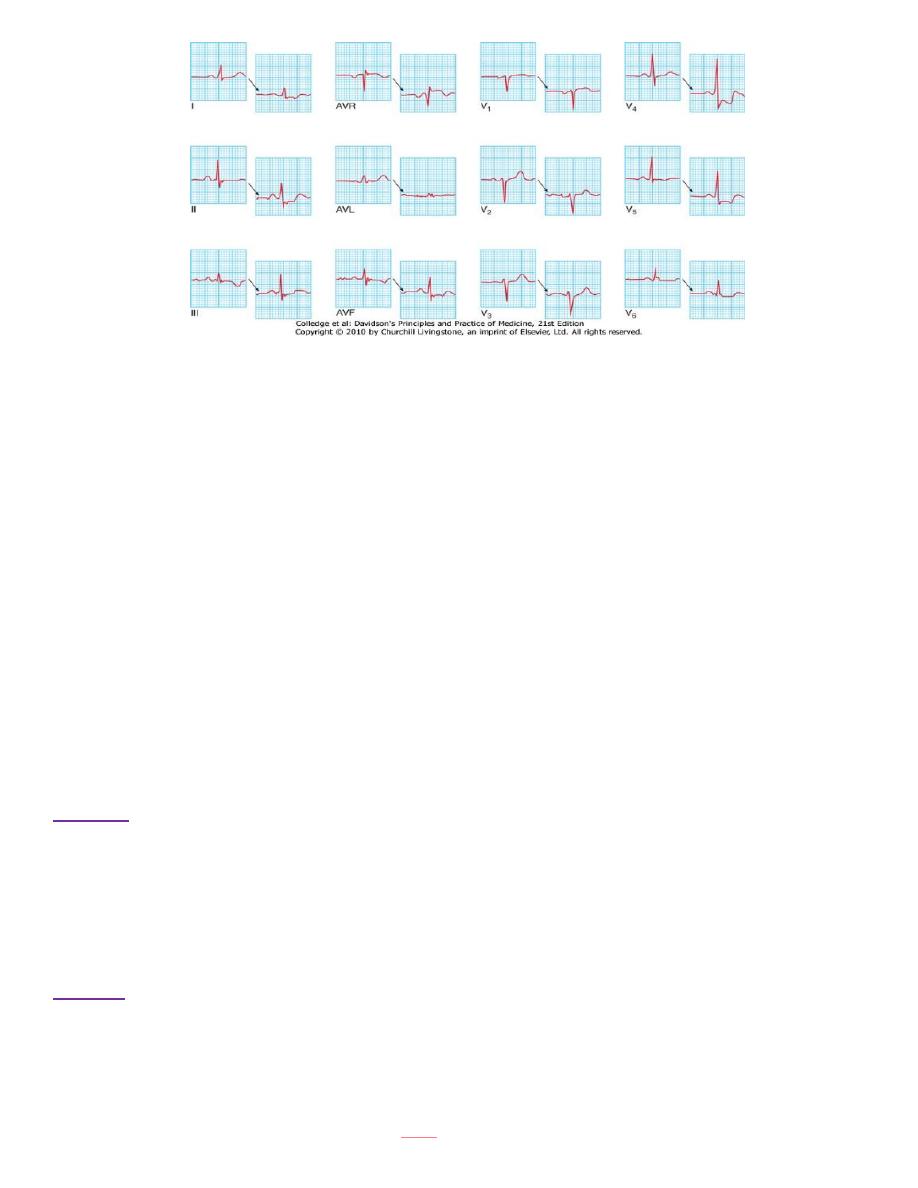
ECG
Resting ECG
Exercise ECG (Stress ECG)
Other forms of stress testing
1-Myocardial perfusion scanning
2- Stress echocardiography
Coronary arteriography
1. Resting ECG =
A. often normal even in patients with left main or severe three-vessel coronary artery disease.
B. evidence of previous MI (Q-wave)
C. T-wave flattening or inversion in some leads, providing non-specific evidence of myocardial
ischaemia or damage-
4
2-Exercise ECG
most convincing ECG evidence of myocardial ischaemia obtained by
demonstrating
reversible ST segment depression or elevation
with or without T-wave inversion
at the time patient is experiencing symptoms (whether spontaneous or induced by exercise
testing).
Exercise tolerance test (ETT) = usually performed using standard treadmill or bicycle ergometer
protocol while monitoring patient's ECG, BP and general condition.
Interpretation
Planar or down-sloping ST segment depression of 1 mm or
more =of ischaemia
up-sloping ST depression i= less specific =often occurs in
normal individuals
5
Exercise ECG Indications :
1) confirm or refute diagnosis of angina
2) assessing severity of coronary disease and identifying high-risk individuals .e.g. amount of
exercise -tolerated and the extent and degree of ST segment change = useful guide likely
extent of CA disease.
Limitations
o Exercise testing is not infallible
o may produce false positive results in the presence of digoxin therapy,
o left ventricular hypertrophy
o left bundle branch block or Wolff-Parkinson-White syndrome.
o predictive accuracy of exercise testing lower in women than men.
o The test should be classed as inconclusive (and not negative) if the patient cannot achieve
an adequate level of exercise because of locomotor or other non-cardiac problems
A GUIDE TO RISK STRATIFICATION IN STABLE ANGINA
High risk
1. Post-infarct angina
2. Ischaemia at low workload
3. Poor LV function
4. Left main or three-vessel disease
5. Poor effort tolerance
Low risk
1) Good effort tolerance
2) Ischaemia only at high workload
3) Single-vessel or minor two-vessel disease
4) Good LV function
5) Predictable exertional angina
N.B.
Patients may fall between these categories.
6
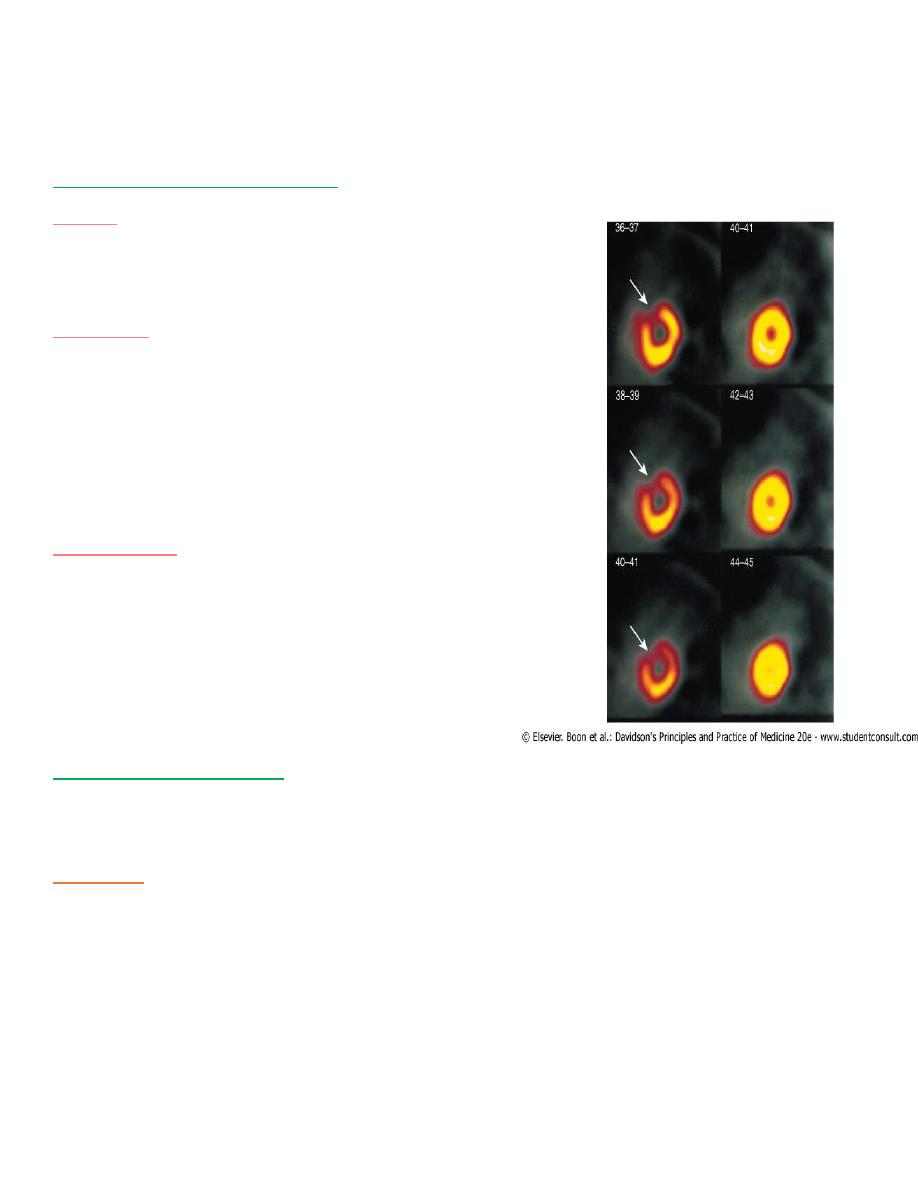
Other forms of stress testing
1) Myocardial perfusion scanning
2) Stress echocardiography
1-Myocardial perfusion scanning
Helpful
in evaluation of patients with
1- equivocal or uninterpretable exercise test
2- unable to exercise
Technique
$ obtaining scintiscans of myocardium at rest and
during stress afteradministration of IV radioactive
isotope(99technetium tetrofosmin.)
$ may be used in conjunction with conventional
exercise testing or pharmacological stress (
dobutamine.)
Interpretation
Thallium and tetrofosmin taken up by viable
perfused myocardium.
perfusion defect present during stress but not
rest provides
reversible myocardial ischaemia .
persistent perfusion defect seen during both
phases of the study
previous MI.
2-Stress echocardiography
Alternative to myocardial perfusion scanning achieve similar predictive accuracy (superior to
exercise ECG).
Technique
uses transthoracic echocardiography to identify ischaemic segments of myocardium and
areas of infarction.
Ischemic segmet reversible defects in contractility during exercise or pharmacological
stress with a dobutamine infusion;
Areas of infarction typically do not contract at rest or during stress
7
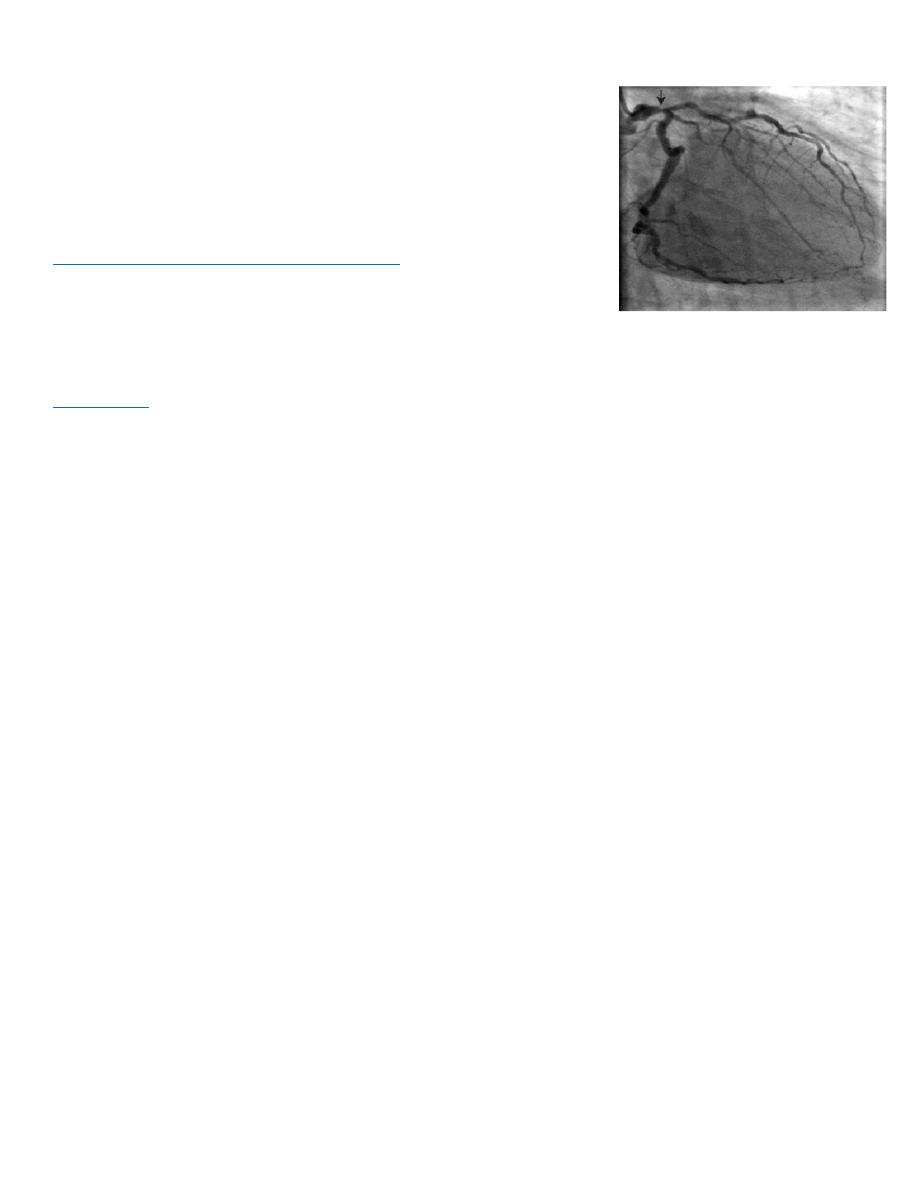
Coronary arteriography
Cardiac catheterisation
=passage of preshaped catheter via a
vein or artery into heart under X-ray guidance
1- measurement of pressure and oxygen saturation in cardiac
chambers and great vessels
2-performance of angiogram (injecting CM into chamber or BV )
coronary arteriography (cf. angioplasty)
q Provides detailed anatomical information about extent and
nature of CAD
q usually performed with a view to CABG or PCI .
Diagnostic
coronary angiography Indicated= non-invasive tests have failed to elucidate the cause
of atypical chest pain.
C procedure performed under local anaesthesia
C requires specialised radiological equipment, cardiac monitoring and an experienced operating
team.
ANGINA WITH NORMAL CORONARY ARTERIES
Approximately 10% stable angina on effort angiographically normal coronary arteries.
Many are women
mechanism of their symptoms is often difficult to establish.
Important to review the original diagnosis and explore other potential causes.
1-Coronary artery spasm
2-Syndrome X
1-Coronary artery spasm
=
Vasospasm =
% may coexist with atheroma, especially in UA
% occasionally (< 1% of all cases of angina) occur without angiographically detectable
atheroma=variant angina
% accompanied by spontaneous and transient ST elevation on the ECG (Prinzmetal's angina).
% Calcium antagonists, nitrates and other coronary vasodilators (e.g. nicorandil) =most useful
therapeutic agents = may be ineffective.
Syndrome X
= constellation of
1. typical angina on effort,
2. objective evidence of myocardial ischaemia on stress testing
3. 3-angiographically normal coronary arteries . poorly understood carries a good prognosis
may respond to treatment with anti-anginal therapy.
8
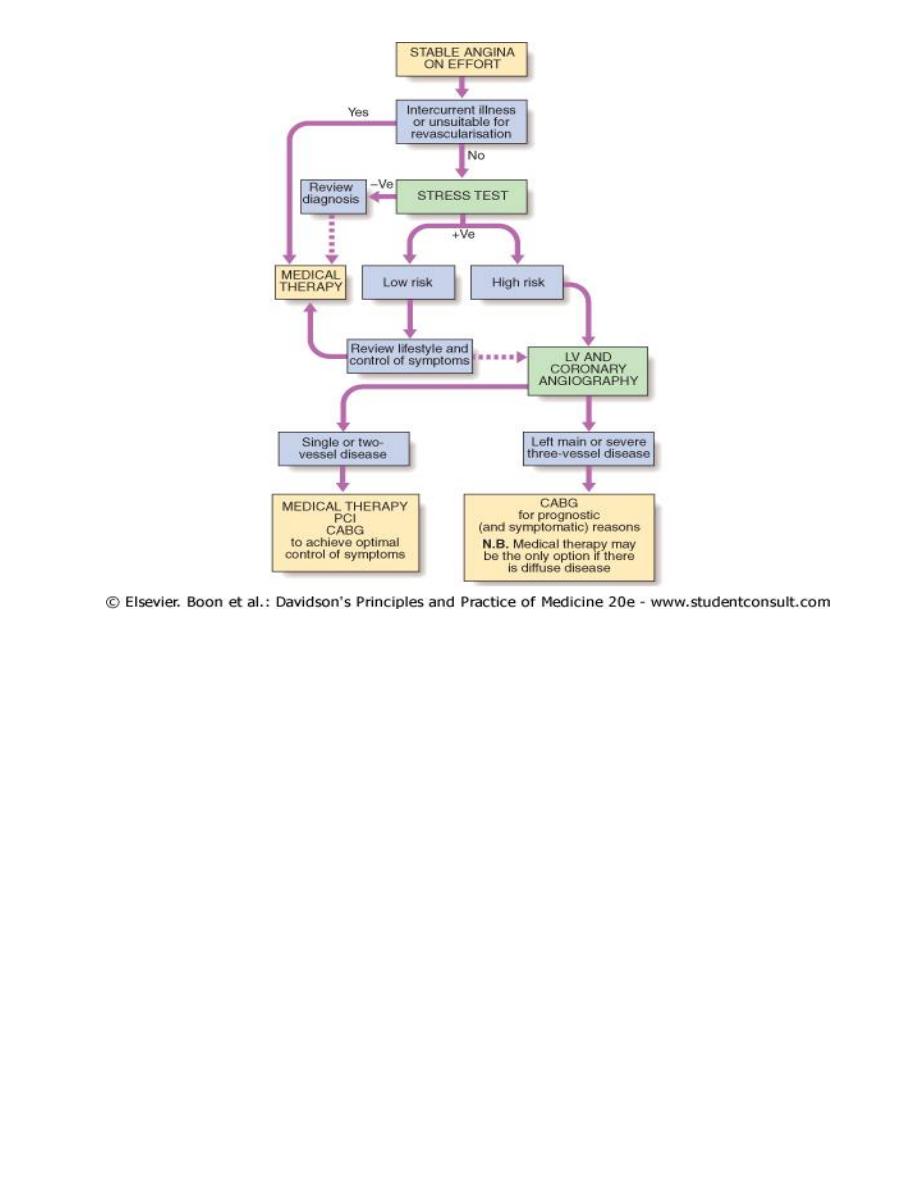
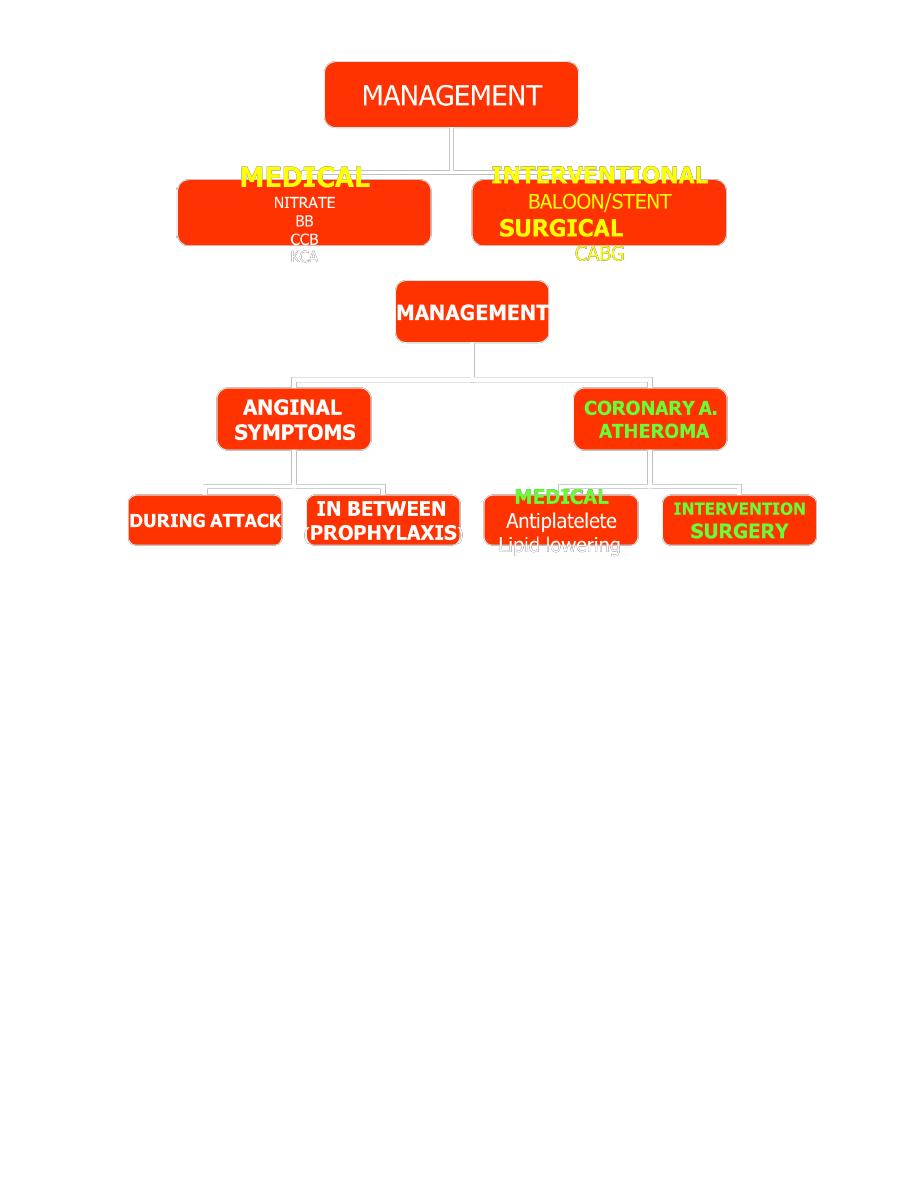
Management
a. assessment of likely extent and severity of arterial disease
b. identification and control of significant risk factors (e.g. smoking, hypertension,
hyperlipidaemia)
c. use of measures to control symptoms
d. identification of high-risk patients and application of treatments to improve life expectancy.
Symptoms alone are a poor guide to the extent of coronary artery disease; exercise or
pharmacological stress testing is therefore advisable in all patients who are potential candidates
for revascularisation.
Treatment
1. careful explanation of the problem discussion of the potential lifestyle and medical
interventions that may relieve symptoms and improve prognosis .
2. Anxiety and misconceptions often contribute to disability; for example, some patients avoid
all forms of exertion because they believe that each attack of angina is a 'mini heart attack'
that results in permanent damage. Effective management of these psychological factors can
make a huge difference to the patient's quality of life.
9
ADVICE TO PATIENTS WITH STABLE ANGINA
N Do not smoke
N Aim at ideal body weight
N Take regular exercise (exercise up to, but not beyond, the point of chest discomfort
N beneficial and may promote collateral vessels)
N Avoid severe unaccustomed exertion, and vigorous exercise after a heavy meal or in very cold
weather
N Take sublingual nitrate before undertaking exertion that may induce angina
MANAGEMENT
8 MEDICAL---during the attack
---between the attacks-prophylactic
8 INVASIVE-INTERVENTIONAL-PCI(PTCA) - SURGERY
10
MEDICAL
1-TREAMENT OF ATHEROSCLEOSIS
2-ANTI-ANGINAL TREATMENT
A-DECREASE OXYGEN SUPPLY
B-BLOCKERS
NITRATES
B-INCREASE BLOOD SUPPLY-VASODILATERS
CCB
KCA
ICB
C-BOTH
Treatment of atherosclerosis
o Life style (smoking/diet/exercise/body weight)
o Treatment of hypercholesrolemia-Statins
o Treatment of hypertension-BB
o Antiplatelete
11
Low-dose (75-150 mg) aspirin
reduces the risk of adverse events such as MI
should be prescribed for all patients with CAD indefinitely
Clopidogrel
(75 mg daily) =
equally effective antiplatelet agent
can be prescribed if aspirin causes troublesome dyspepsia or other side-effects
Anti-anginal drug treatment
Five groups =relieve or prevent symptoms
nitrates,
β-blockers,
calcium antagonists
potassium channel activators and
If channel antagonist.
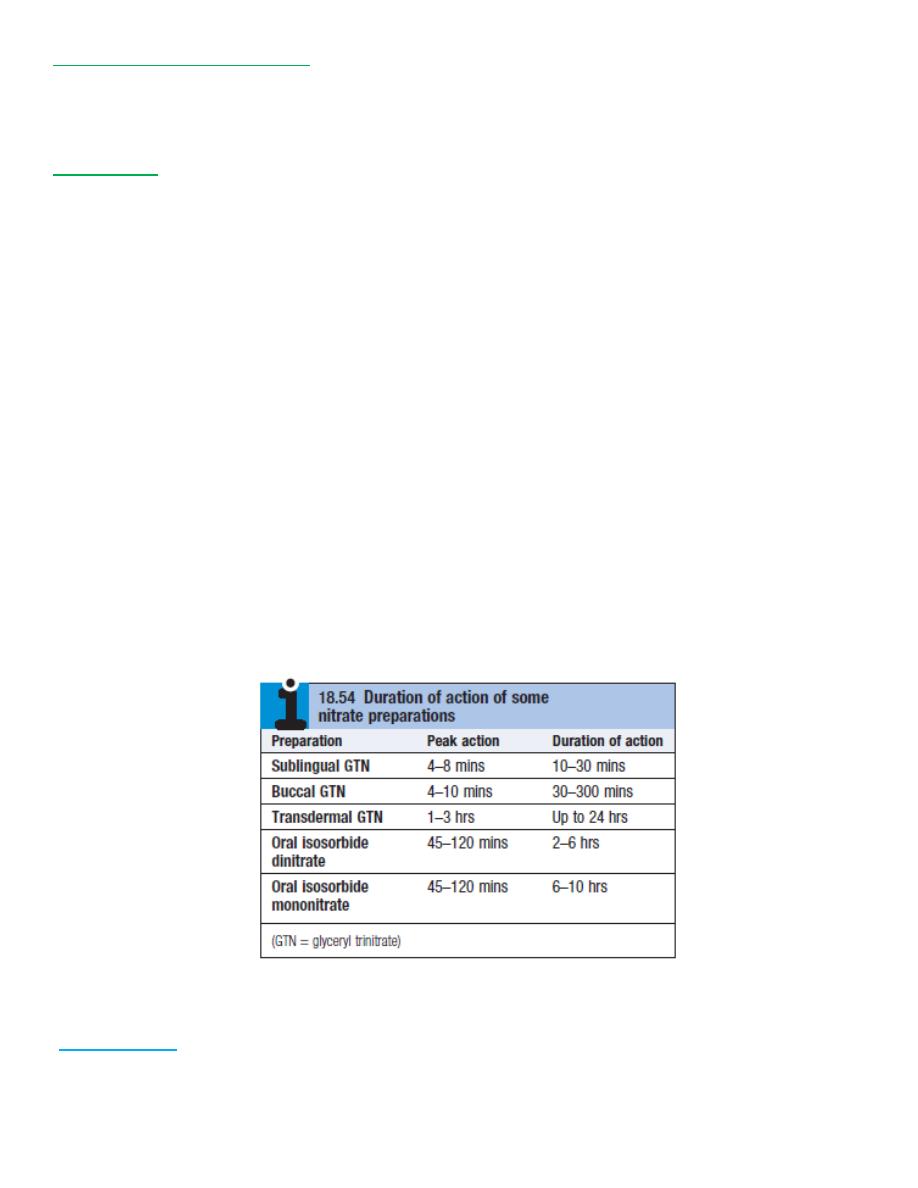
1-Nitrates
act directly on vascular smooth muscle produce venous and arteriolar dilatation;
Beneficial effects
1. reduction in myocardial oxygen demand (lower preload and afterload) and
2. increase in myocardial oxygen supply (coronary vasodilatation)
Glyceryl TriNitrate (GTN)
Administered
. from a metered-dose aerosol (400 μg per spray) or as a tablet (300 or 500 μg) allowed to
dissolve under the tongue or crunched and retained in the mouth will usually relieve an
attack of angina in 2-3 minutes.

12
Unwanted side-effects
1. headache (which may be more distressing than the angina), symptomatic hypotension and,
rarely, syncope.
2. To avoid these symptoms the tablet may be spat out as soon as the angina is relieved.
3. Patients often need to be reassured that GTN is not habit-forming and will not lose its effect if
used repeatedly.
USE
A. use the drug prophylactically before engaging in exercise that is liable to provoke symptoms.
Sublingual
B. Sublingual GTN has a short duration of action
C. variety of alternative nitrate preparations can provide a more prolonged therapeutic effect.
Transcutaneously GTN
as a patch (5-10 mg daily), or as a
Slow-release buccal
tablet (1-5 mg 6-hourly).
GTN is subject to extensive first-pass metabolism in the liver and is therefore virtually ineffective
when swallowed;
Long acting oral nitrates
1) isosorbide dinitrate (10-20 mg 8-hourly) and
2) isosorbide mononitrate (20-60 mg once or twice a day)
Headache common -tends to diminish if the patient perseveres with the treatment.
Continuous nitrate therapy pharmacological tolerance = avoided by using a regimen
that includes a nitrate-free period of 6-8 hours every day.
variety of once-daily proprietary preparations with a built-in nitrate-free period are
available.
schedule the medication so that drug levels are low during the night when the patient is
inactive;
if nocturnal angina is a prominent symptom, long-acting nitrates can be given at the end of
the day instead
2-Beta-blockers
E lower myocardial oxygen demand by reducing
E heart rate,
E blood pressure and
E myocardial contractility.
13
SIDE EFFECTS
A. exacerbate the symptoms of peripheral vascular disease may provoke bronchospasm in
patients with obstructive airways disease.
B. non-selective β-blockers may aggravate coronary vasospasm by blocking the coronary artery
β2-adrenoceptors and
C. A β-blocking drug should not be withdrawn abruptly because this may have a rebound effect
and precipitate dangerous arrhythmias, worsening angina or myocardial infarction (the β-
blocker withdrawal syndrome).
DOSAGE
a) advisable to use a once-daily cardioselective preparation e.g.
o slow-release metoprolol 50-200 mg daily,
o bisoprolol 5-10 mg daily).
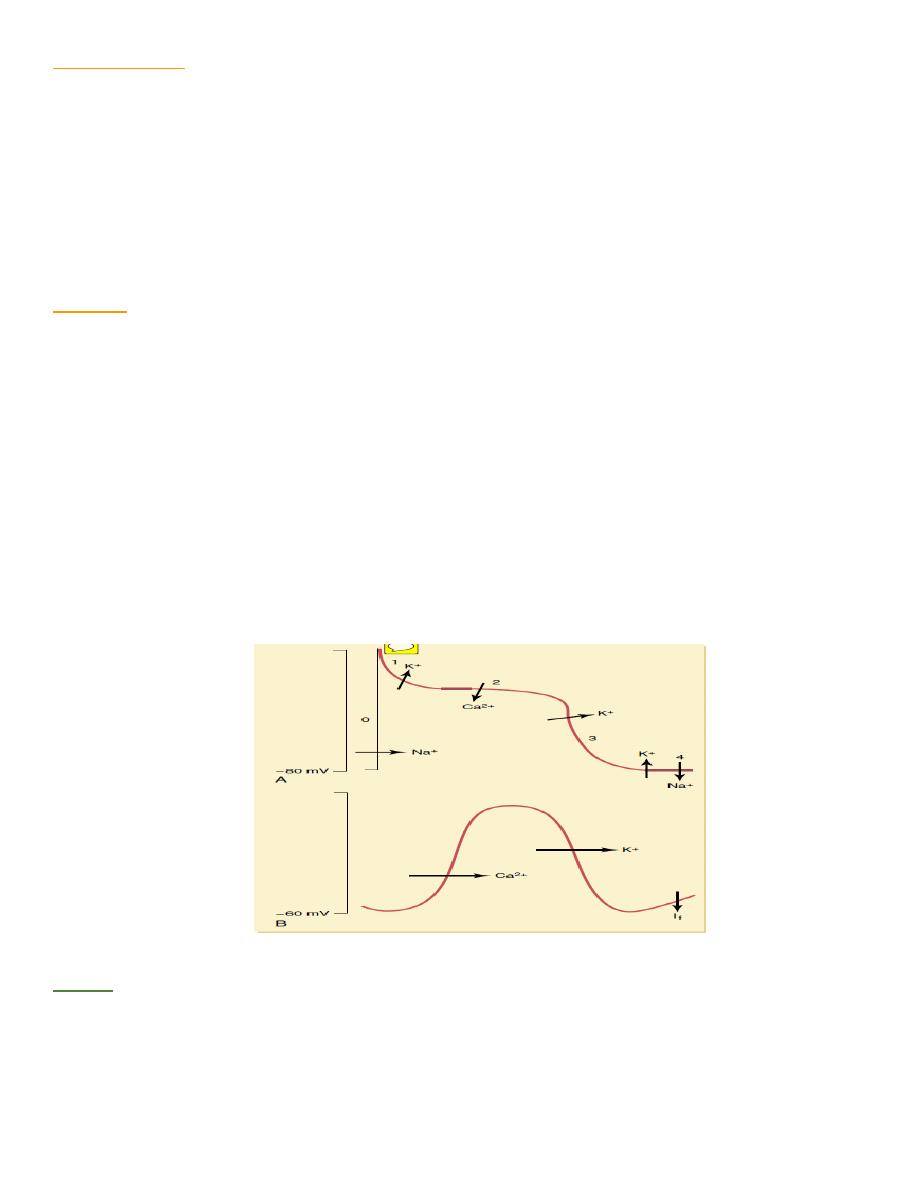
Calcium channel blockers
3-Calcium antagonists
inhibit slow inward current caused by entry of extracellular calcium through cell membrane of
excitable cells, particularly cardiac and arteriolar smooth muscle, and lower myocardial oxygen
demand by reducing blood pressure and myocardial contractility.
TYPES
1- Dihydropyridine calcium antagonists, e.g. nifedipine and nicardipine, often cause a reflex
tachycardia; this may be counterproductive and it is often best to use these drugs in combination
with a β-blocker.
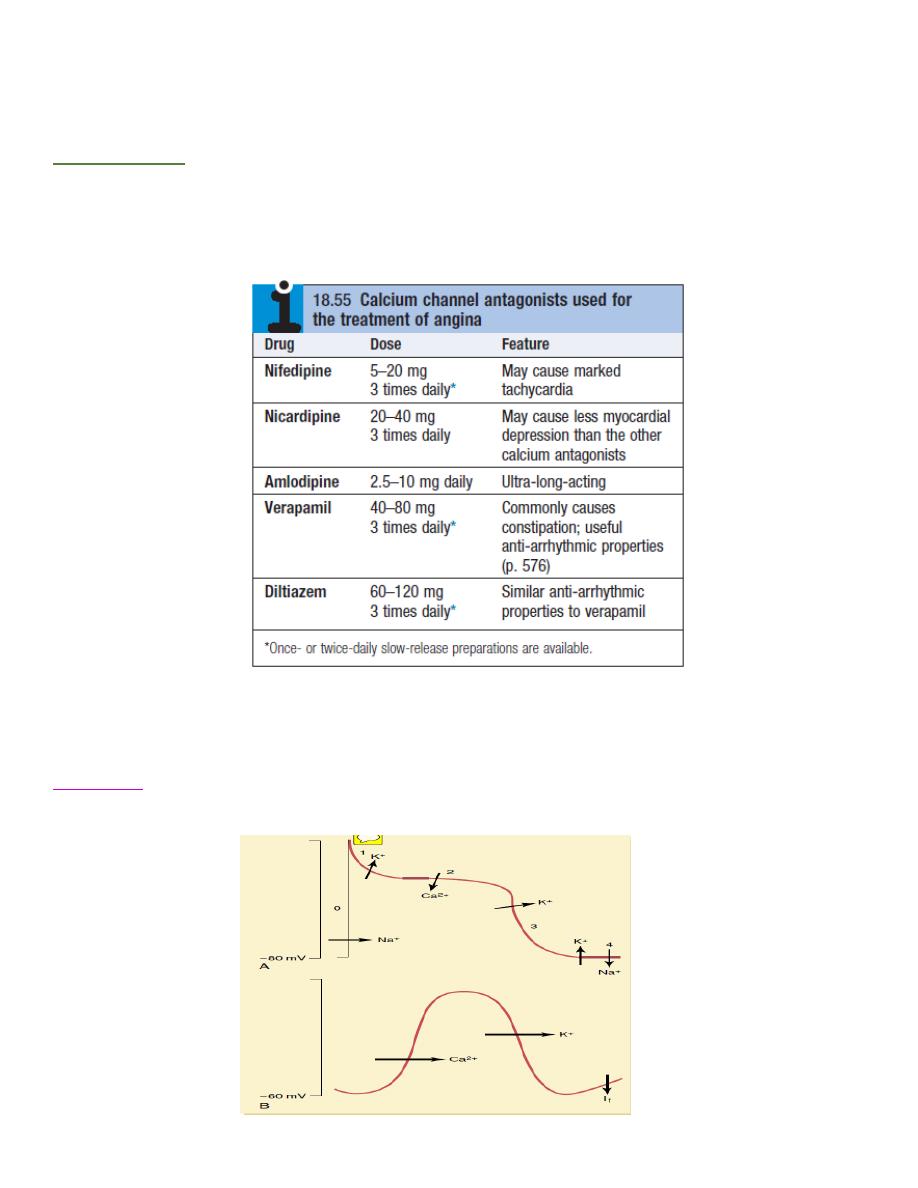
14
2- verapamil and diltiazem -particularly suitable for patients who are not receiving a β-blocker (
inhibit conduction through the AV node and tend to cause a bradycardia or even AV block in
susceptible individuals.)
SIDE EFFECTS
b) may reduce myocardial contractility and can aggravate or precipitate heart failure.
c) peripheral oedema,
d) flushing, headache and dizziness.
4-Potassium channel activators
has arterial and venous dilating properties does not exhibit tolerance seen with nitrates.
Nicorandil
(10-30 mg 12-hourly orally) = tonly drug in this class currently available for clinical
use.

15
5. If channel antagonist
Ivabradine
3 first of this class of drug.
3 It induces bradycardia by modulating ion channels in sinus node.
3 In contrast to β-blockers and rate-limiting calcium antagonists, it does not have other
cardiovascular effects.
3 Appears to be safe to use in patients with heart failure.
Guidelines
. each of these groups of drug has been shown to be superior to placebo in relieving the
symptoms of angina== little convincing evidence that one group is more effective than
another.
. many commonly used combinations of anti-anginal drugs have not been evaluated in well-
controlled clinical trials.
1-conventional to start therapy with low-dose aspirin+ sublingual GTN +a β-blocker,
2-add a calcium channel antagonist or a long-acting nitrate l
Goal
control of angina with minimum side-effects and the simplest possible drug regimen.
little or no evidence that prescribing multiple anti-anginal drugs is of benefit, and
revascularisation =considered if an appropriate combination of two drugs fails to achieve a
symptomatic response.
Invasive treatment
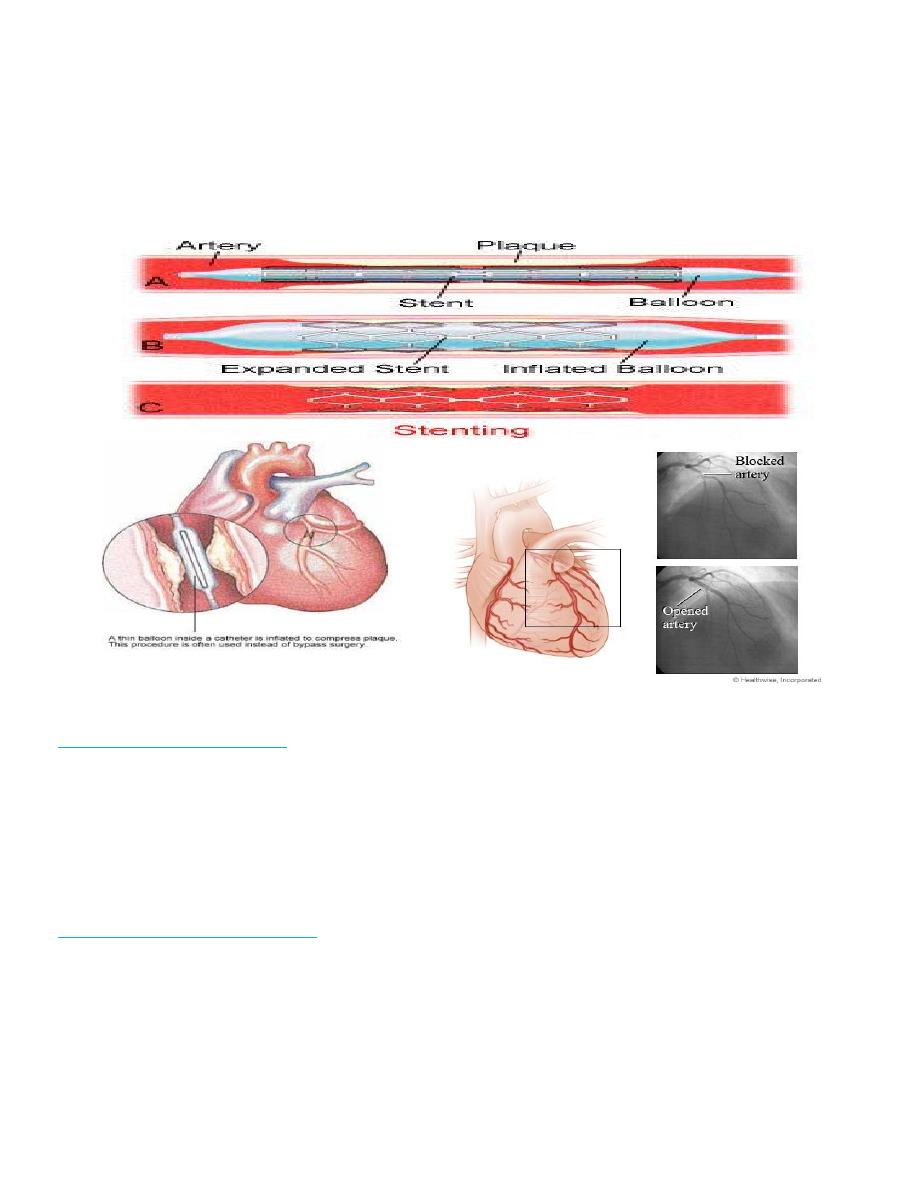
1) percutaneous coronary intervention (PCI = percutaneous transluminal coronary angioplasty,
PTCA)
2) coronary artery bypass graft (CABG) surgery.
Percutaneous coronary intervention (PCI)
3 passing a fine guidewire across coronary stenosis under radiographic control and using it to
position a balloon which is then inflated to dilate the stenosis
3 Coronary stent =piece of coated metallic 'scaffolding' = deployed on a balloon and used to
maximise and maintain dilatation of stenosed vessel. use of stents in appropriate vessels
reduces both acute complications and incidence of clinically important restenosis .+ Drug-
eluting stents
16
3 PCI provides an effective symptomatic treatment no evidence that it improves survival in
patients with chronic stable angina.
3 PCI is mainly used in :
1. single or two-vessel disease;
2. stenoses in bypass grafts +native coronary arteries=Dilated
+ palliative therapy for recurrent angina after CABG.
COMPLICATIONS OF PTC
acute complications of PCI
¥ occlusion of target vessel or a side branch by thrombus or a loose flap of intima (coronary
artery dissection), and consequent myocardial damage. 2-5% . often corrected by deploying a
stent +/-emergency CABG i
¥ Minor myocardial damage, as indicated by elevation of sensitive intracellular markers
(troponins), occurs in up to 10% of cases.
long-term complication of PCI
* restenosis = occurs in up to one-third of cases(elastic recoil + smooth muscle proliferation
(neo-intimal hyperplasia) =within 3 months.
* Stenting substantially reduces the risk of restenosis, ( allows operator to achieve more
complete dilatation in first place).
* Drug-eluting stents can reduce this risk even further by allowing an antiproliferative drug,
such as sirolimus or paclitaxel, to elute slowly from the coating and prevent neo-intimal
hyperplasia and in-stent restenosis.
17
* Recurrent angina ( 15-20% of patients receiving an intracoronary stent at 6 months) may
require further PCI or bypass grafting
Risk of complications and likely success of the procedure are closely related to
a. morphology of the stenoses,
b. experience of the operator and
c. presence of important comorbidity (e.g. diabetes, peripheral arterial dis).
Good outcome is less likely if target lesion is
1. complex,
2. long,
3. eccentric or
4. 4-calcified,
5. lies on a bend or within a tortuous vessel,
6. involves a branch or
7. contains acute thrombus.
In combination with aspirin and heparin, adjunctive therapy with potent platelet inhibitors,
such as clopidogrel or glycoprotein IIb/IIIa receptor antagonists, has been shown to improve
the outcome of PCI, with lower short- and long-term rates of death and myocardial infarction.
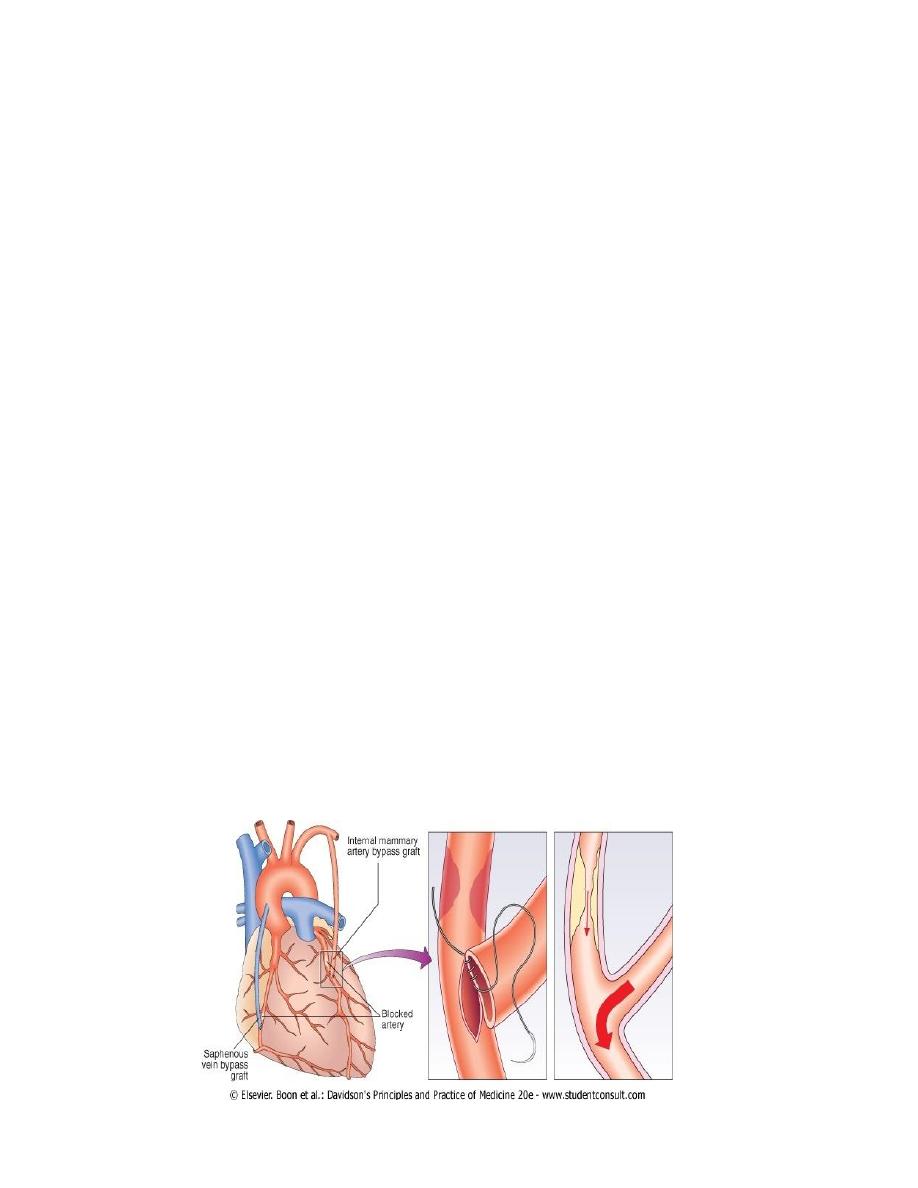
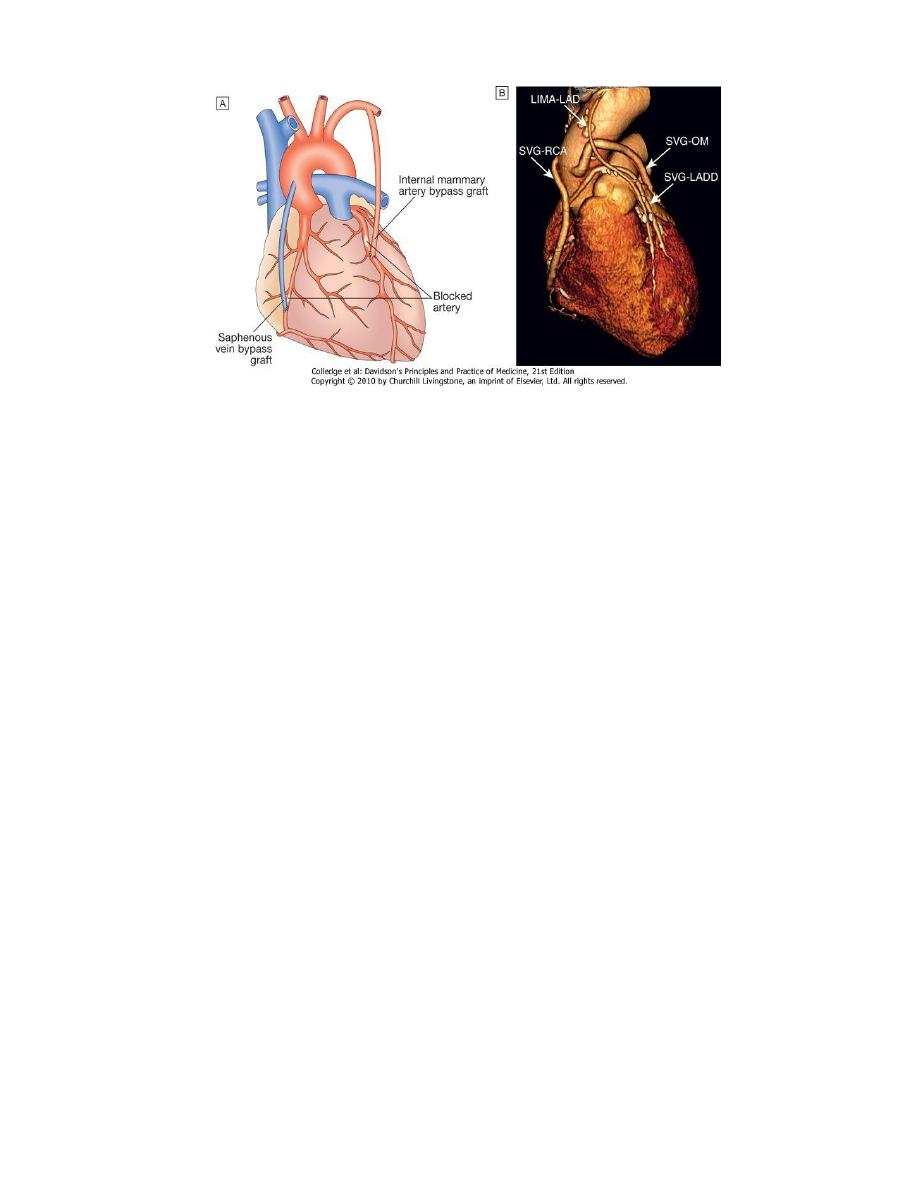
Coronary artery bypass grafting (CABG)
Internal mammary arteries, radial arteries or reversed segments of patient's own saphenous
vein =used to bypass coronary artery stenoses involves major surgery under
cardiopulmonary bypass, but in some cases, grafts can be applied to the beating heart: 'off-
pump' surgery.
Operative mortality is approximately 1.5%, risks are higher in elderly patients poor LV
function significant comorbidity (renal failure)
18
Three-dimensional reconstruction of multidetector CT of the heart
a CABG =improve survival in patients with left main coronary stenosis
a symptomatic patients with three-vessel coronary disease (i.e. involving left anterior
descending, circumflex and right coronary arteries, two-vessel disease involving the proximal
left anterior descending coronary artery.
a Improvement in survival is most marked in those with impaired left ventricular function or
positive stress testing prior to surgery and those who have undergone left internal mammary
artery grafting.
Neurological complications
Z common, 1-5% risk of perioperative stroke.
Z Between 30% and 80% of patients develop short-term cognitive impairment that is often mild
and typically resolves within 6 months.
Z Reports of long-term cognitive decline that may be evident in more than 30% of patients at 5
years.
OUTCOME OF CABG
` 90% of patients =free of angina 1 year after surgery
` 60% =asymptomatic 5 or more years after CABG.
` Early post-operative angina =due to graft failure arising from technical problems during
operation or poor 'run off' (dis. in distal native coronary v.
` Late recurrence of angina =due to progressive disease in native coronary arteries or graft
degeneration.
` Less than 50% of vein grafts are patent 10 years after surgery.
` arterial grafts have a much better long-term patency rate with more than 80% of internal
mammary artery grafts patent at 10 years. => total arterial revascularisation (TAR) during
CABG surgery.
19
`
Aspirin
(75-150 mg daily) and clopidogrel (75 g daily) have both been shown to improve graft
patency-one prescribed indefinitely if well tolerated.
` Intensive lipid-lowering therapy =slow the progression of disease in native coronary arteries
and bypass grafts, and to reduce clinical cardiovascular events;
` serum LDL cholesterol <3.2 mmol/l (∼120 mg/dl).
` excess cardiovascular morbidity and mortality in patients who continue to smoke after bypass
grafting..
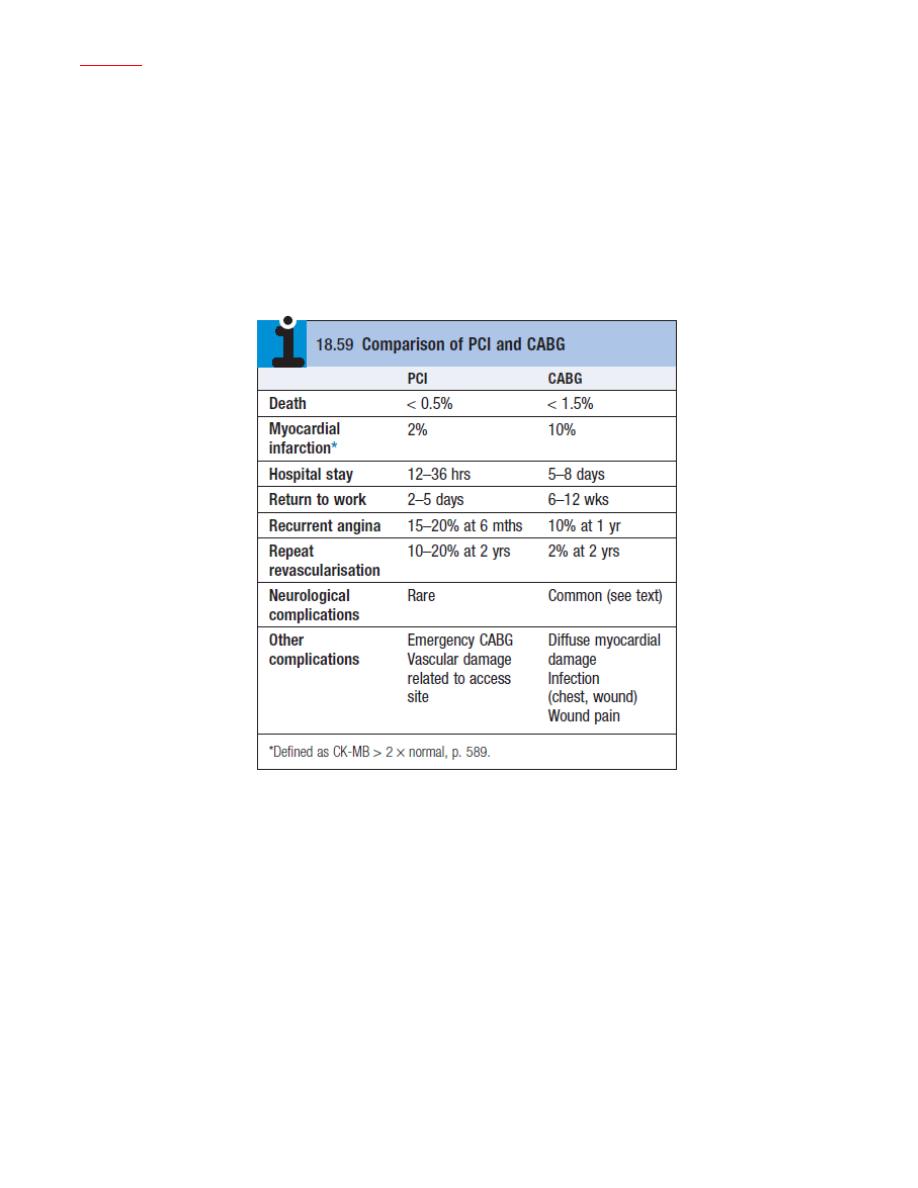
COMPARISON OF PERCUTANEOUS CORONARY INTERVENTION (PCI) AND CORONARY ARTERY
BYPASS GRAFTING (CABG)
Prognosis
z Symptoms are a poor guide to prognosis; 5-year mortality of patients with severe angina
(NYHA class III or IV, ) is nearly double that of patients with mild symptoms.
z Exercise testing and other forms of stress testing are much more powerful predictors of
mortality; Prognosis of coronary artery disease is related to number of diseased vessels (one-
, two- or three-vessel coronary artery disease) and degree of left ventricular dysfunction.
z Patient with single-vessel disease and good LV function has an excellent outlook (5-year
survival > 90%), patient with severe LV dysfunction and extensive three-vessel disease has a
poor prognosis (5-year survival < 30%) without revascularisation.
z Spontaneous symptomatic improvement due to the development of collateral vessels is
common.
