1
INFECTIVE ENDOCARDITIS
Definition:
Microbial infection of:
1-
Heart valve
(native or prosthetic)
2-
Lining
of cardiac chamber or blood vessel
3-
Congenital anomaly
(e.g. septal defect).
Aetiology:
Causative organism
usually
Bacteria
May be Rickettsia // Chlamydia // Fungus.
TYPES
-clinical presentations
1-SUB-ACUTE ENDOCARDITIS
On congenital or valvular heart dis.
2-ACUTE ENDOCARDITIS
On normal valves
3-POST-OPERATIVE ENDOCARDITIS
EARLY < 60 DAYS
LATE > 60 DAYS
Pathophysiology
HEART=
1-less virulent organism
pre-existing endocardial damage.
2-virulent or aggressive organisms
previously normal heart e.g., staphylococcal
endocarditis of the tricuspid valve is a common complication of intravenous drug
misuse.
Risk of Endocarditis
HIGH
= Areas of endocardial damage caused by
high-pressure jet
of blood,
haemodynamically insignificant. e.g.
ventricular septal defect,
mitral regurgitation
aortic regurgitation,
NEGLIGIBLE
at site of haemodynamically important low-pressure lesions (e.g. ) large
atrial septal defect) is minimal risk
2
Pathologic process
1-endothelial damage because thay attract deposits of platelets & fibrin thay are
vulnerable to
colonisation
by blood-borne organisms.
(avascular valve tissue + presence of fibrin aggregates to help
protect
proliferating
organisms
from host defense mechanisms).
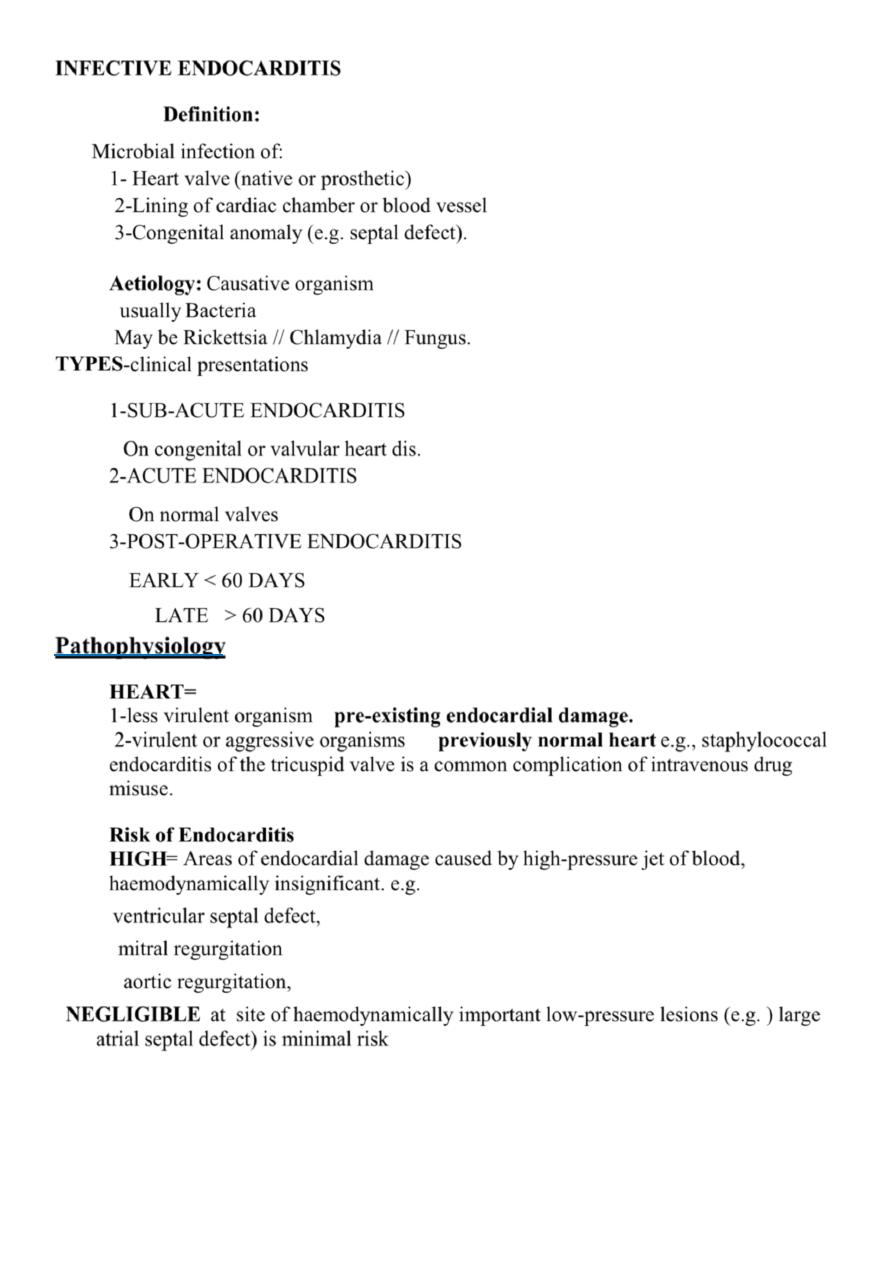
2- infection established
vegetations composed of
organisms+fibrin+platelets
Vegetations
=
grow and may be become large enough to cause obstruction
vegetations
=
break away
emboli
.
Adjacent tissues destroyed
abscesses
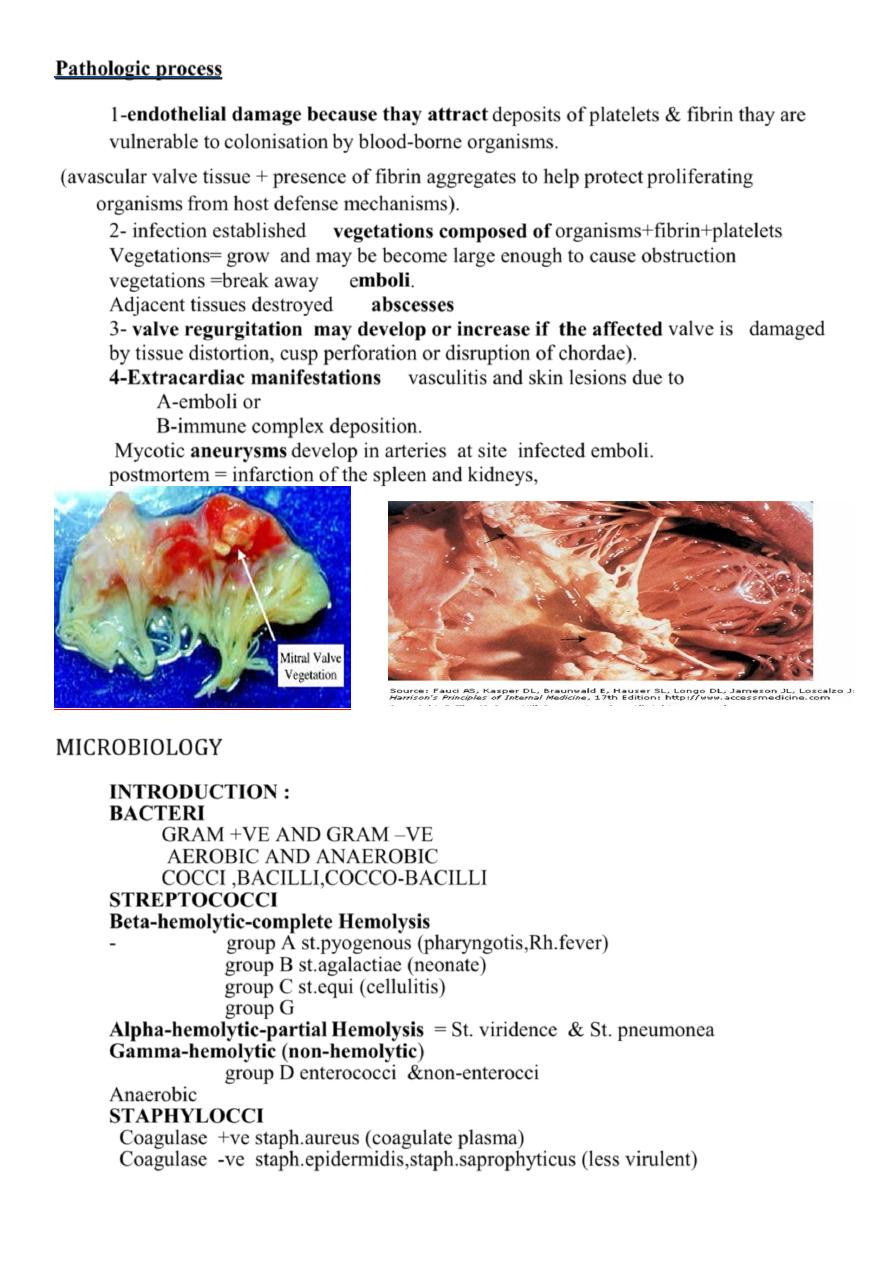
3-
valve regurgitation may develop or increase if the affected
valve is damaged
by tissue distortion, cusp perforation or disruption of chordae).
4-
Extracardiac manifestations
vasculitis and skin lesions due to
A-emboli or
B-immune complex deposition.
Mycotic
aneurysms
develop in arteries at site infected emboli.
postmortem = infarction of the spleen and kidneys,
MICROBIOLOGY
INTRODUCTION :
BACTERI
GRAM +VE AND GRAM –VE
AEROBIC AND ANAEROBIC
COCCI ,BACILLI,COCCO-BACILLI
STREPTOCOCCI
Beta-hemolytic-complete Hemolysis
- group A st.pyogenous (pharyngotis,Rh.fever)
group B st.agalactiae (neonate)
group C st.equi (cellulitis)
group G
Alpha-hemolytic-partial Hemolysis =
St. viridence & St. pneumonea
Gamma-hemolytic (non-hemolytic
)
group D enterococci &non-enterocci
Anaerobic
STAPHYLOCCI
Coagulase +ve staph.aureus (coagulate plasma)
Coagulase -ve staph.epidermidis,staph.saprophyticus (less virulent)
3
Microbiology
>3/4 =streptococci or staphylococci
1-Viridans
group of streptococci
= commensals in URT
enter blood stream on chewing or teeth-brushing, dental treatment, common causes of
subacute endocarditis .
2-
Enterococcus
enter blood from
bowel or urinary tract
.
3-Staph. Aureus
common cause of
acute endocarditis
,
from
skin
infections, abscesses or vascular access sites or from
intravenous
drug misuse.
highly virulent and invasive organism, produce florid vegetations, rapid valve destruction
and abscess formation.
4-
Other =
Strep. pneumoniae
and
Strep. pyogenes
.
5-Gram-negative bacteria
slow-growing fastidious organisms
revealed after prolonged culture
may be resistant to penicillin.
6-
Brucella
history of contact with goats or cattle .often affects aortic V.
7-Yeasts and fungi
attack previously normal or prosthetic valves,
particularly in immuno-compromised or with indwelling IV lines.
Abscesses and emboli - common,
therapy is difficult (surgery is often required) and mortality is high.
Concomitant bacterial infection may be present.
Post-operative endocarditis
Native or prosthetic heart valves or other prosthetic materials.
Coagulase-negative staphylococcus
(Staph. epidermidis)
, =
normal skin
commensal. =
history of post-operative wound infection
Q fever endocarditis (
Coxiella burnetii
) –
patient often has a history of contact with farm animals
Incidence
Incidence =2-5 cases per 100 000 per annum.
Underlying condition =2/3 vs.1/3
1- rheumatic heart disease = 24% of patients
2-congenital heart disease =19%
3- other cardiac abnormality (e.g. calcified atrial valve, floppy mitral valve) = 25%.
4- remainder (32%)= No pre-existing cardiac abnormality.
Age
> 50% of patients with infective endocarditis > 60 years
4
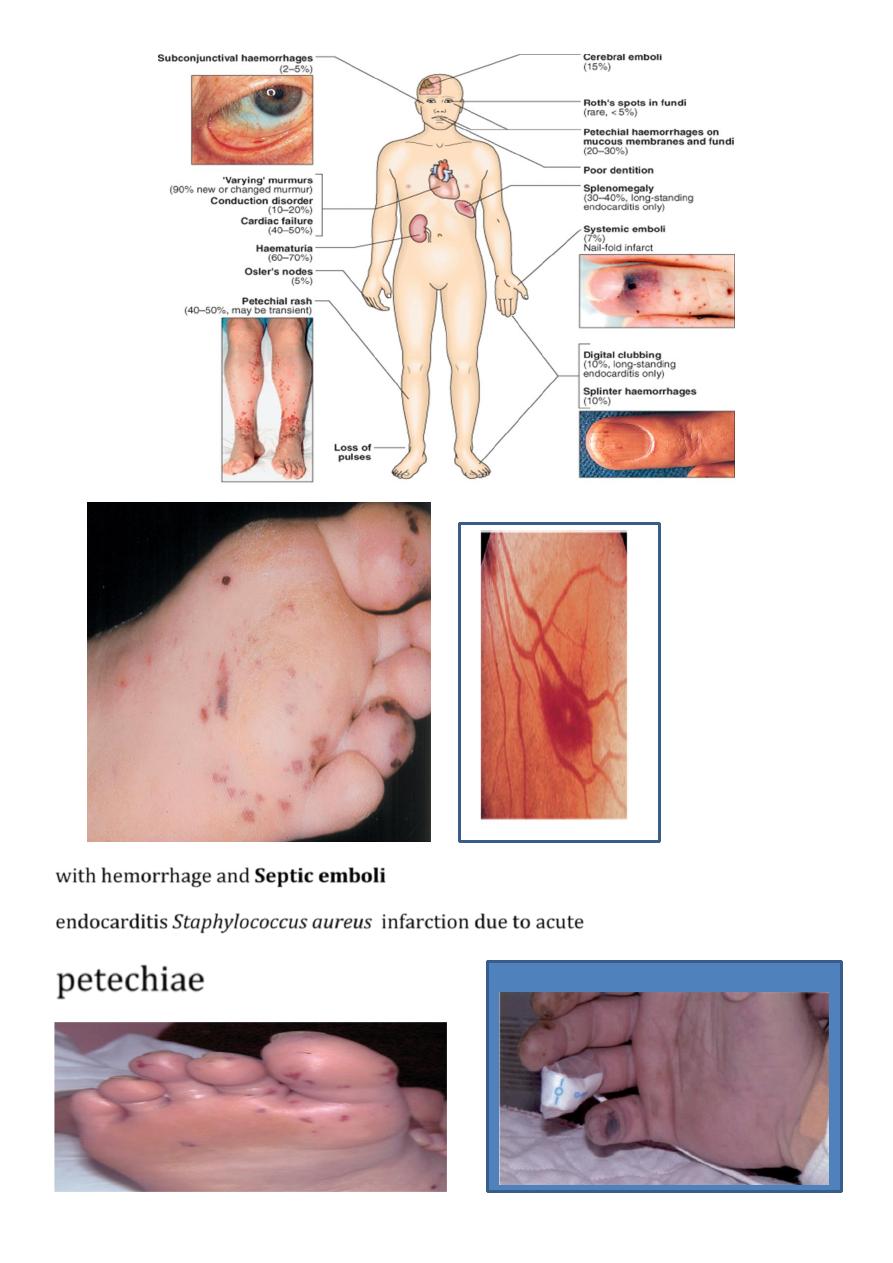
Clinical features
clinical course
1-
acute
2-
'
subacute
‘more insidious form.
overlap clinical pattern influenced by
organism
site of infection,
prior antibiotic therapy and
the presence of a valve or shunt prosthesis.
subacute form may abruptly develop acute life-threatening complications such as
valve disruption or emboli
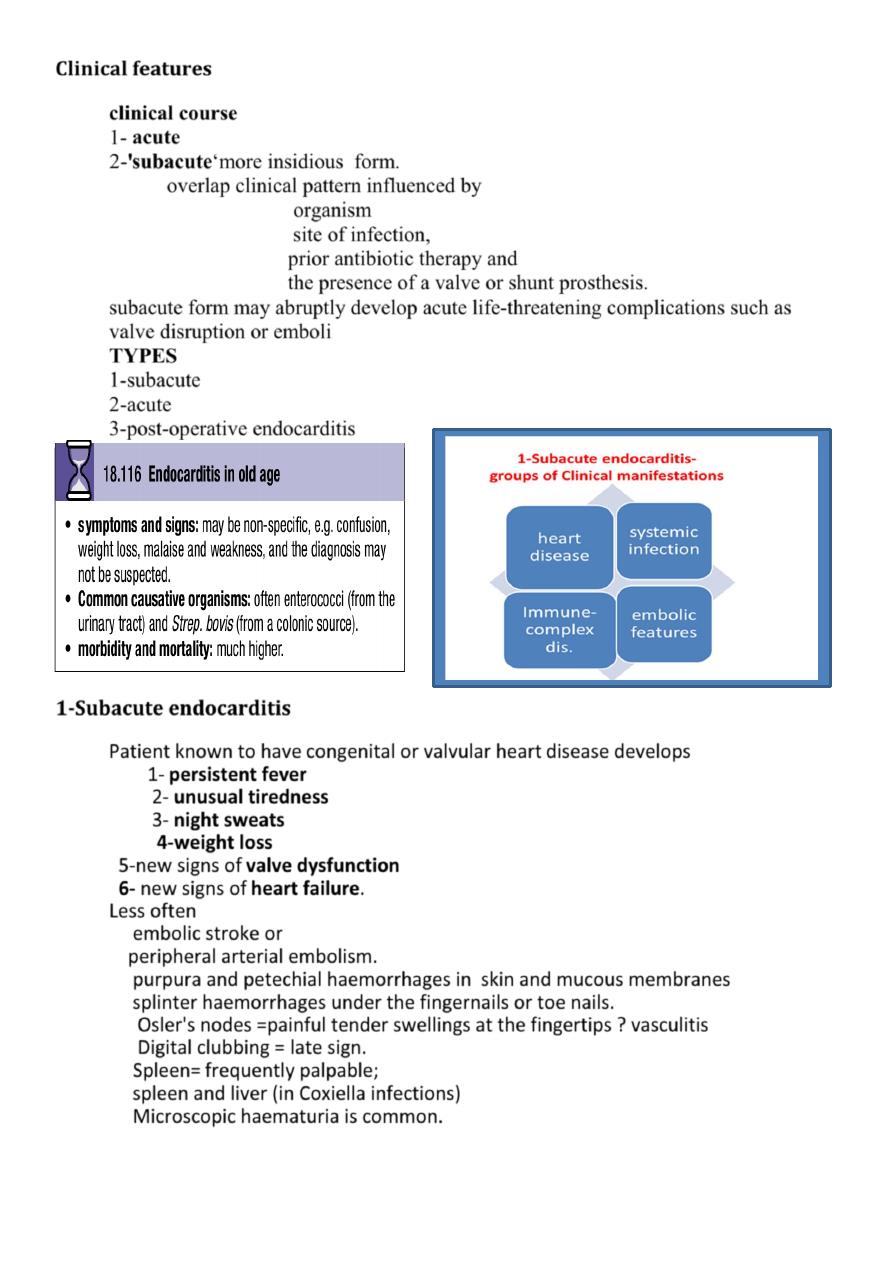
TYPES
1-subacute
2-acute
3-post-operative endocarditis
1-Subacute endocarditis
Patient known to have
congenital or valvular heart
disease develops
1-
persistent fever
2- unusual tiredness
3- night sweats
4-weight loss
5-new signs of
valve dysfunction
6- new signs of
heart failure.
Less often
embolic stroke or
peripheral arterial embolism.
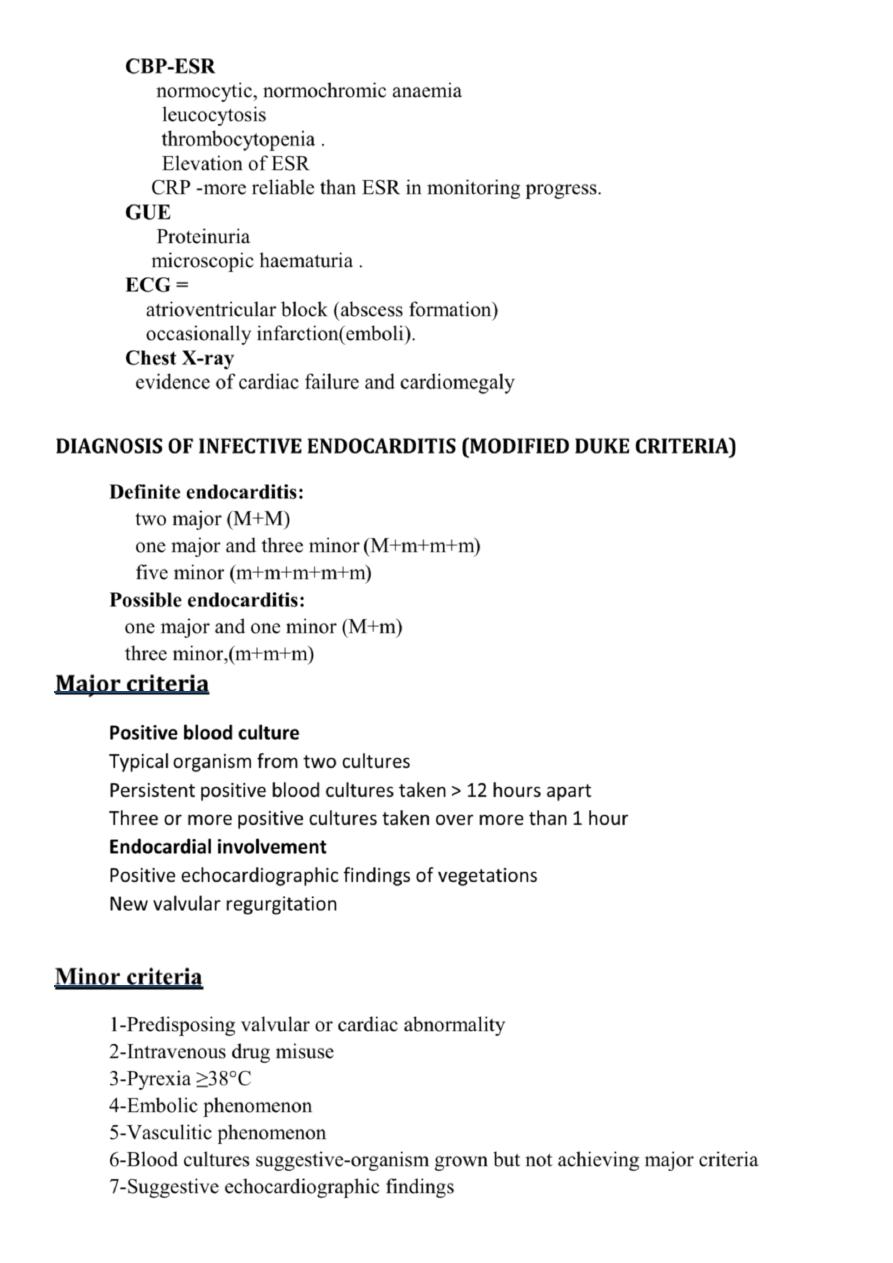
purpura and petechial haemorrhages in skin and mucous membranes
splinter haemorrhages under the fingernails or toe nails.
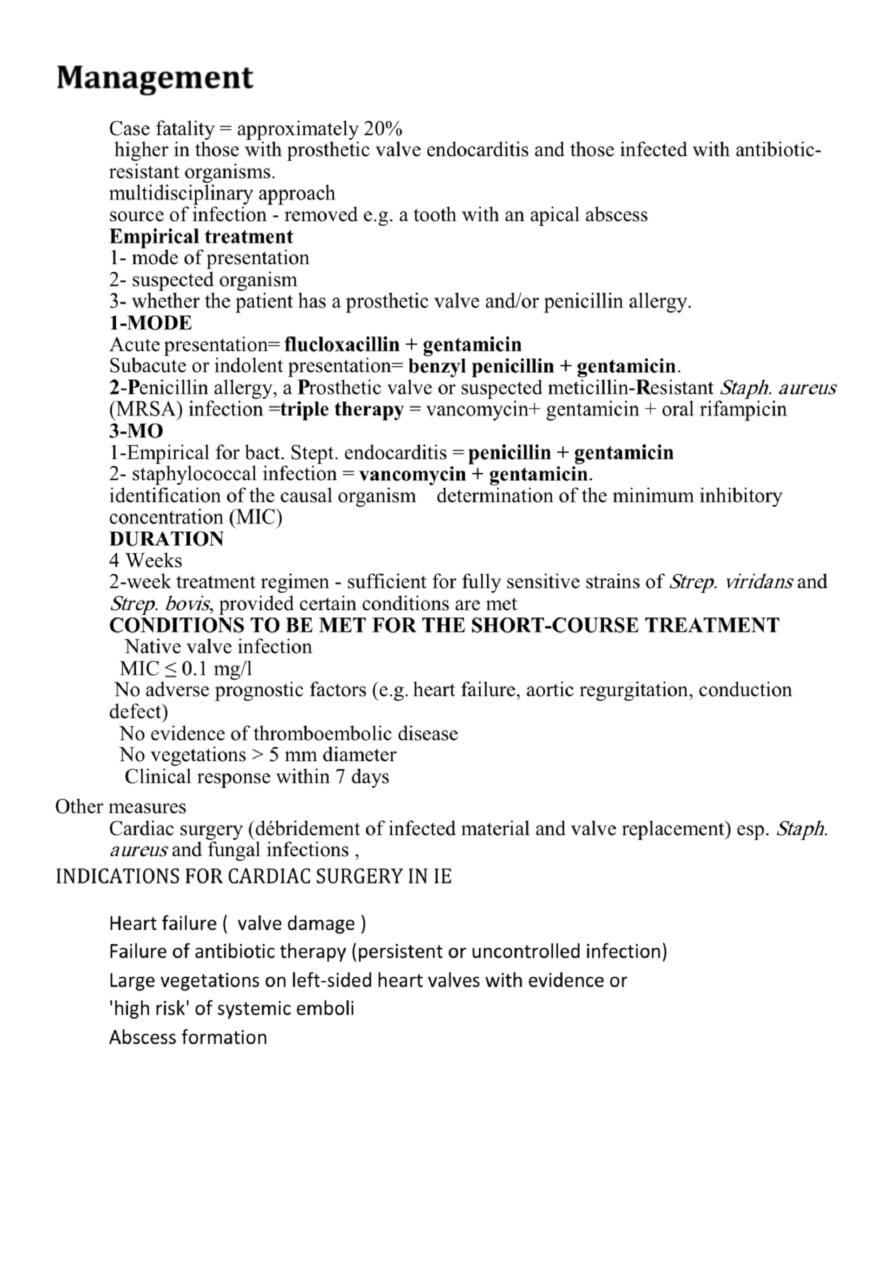
Osler's nodes =painful tender swellings at the fingertips ? vasculitis
Digital clubbing = late sign.
Spleen=
frequently palpable;
spleen and liver (in Coxiella infections)
Microscopic haematuria is common.
5
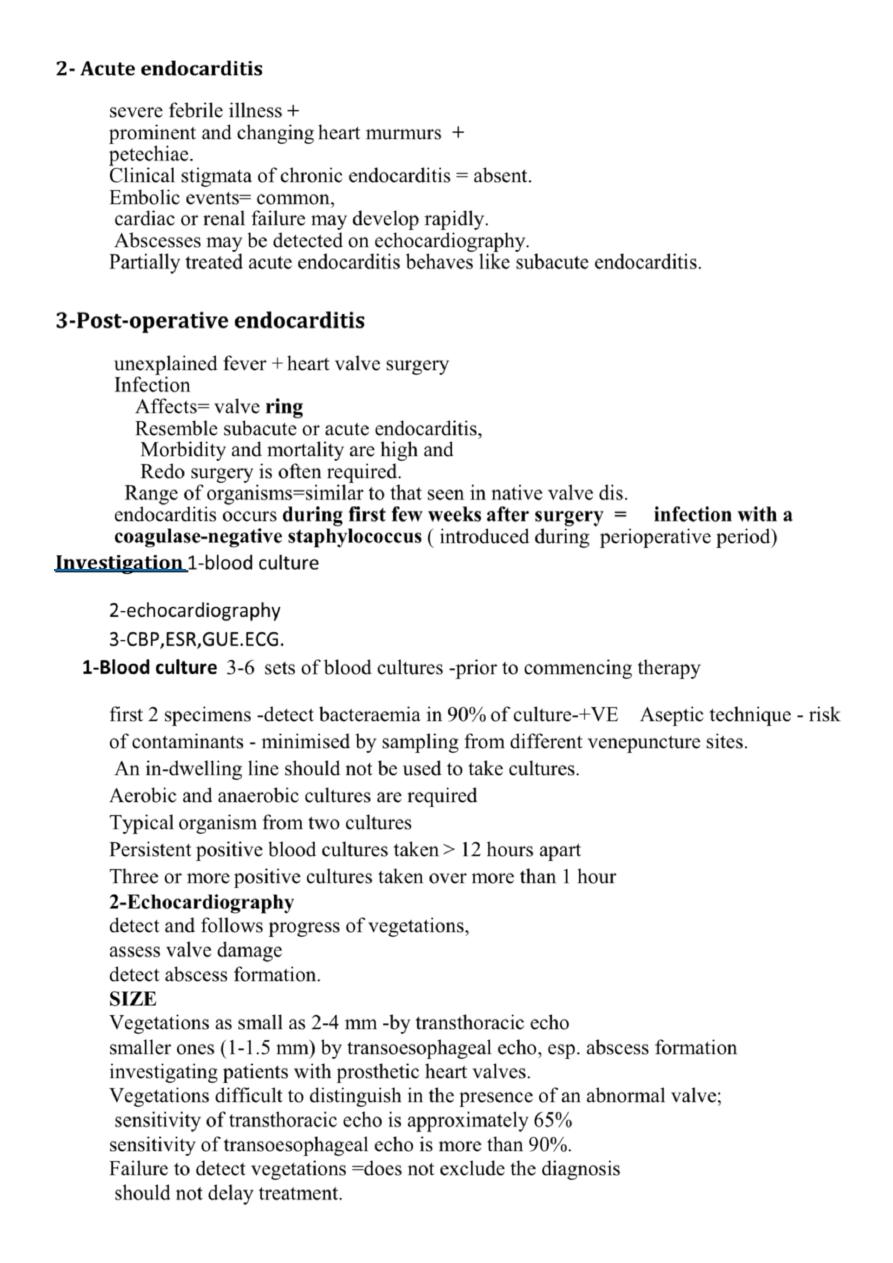
Septic emboli
with hemorrhage and
infarction due to acute
Staphylococcus aureus
endocarditis
petechiae
Osler’r node
6
Acute endocarditis
2-
severe febrile illness
+
prominent and changing
heart murmurs
+
petechiae.
Clinical stigmata of chronic endocarditis = absent.
Embolic events
=
common,
cardiac or renal failure may develop rapidly.
Abscesses
may be detected on echocardiography.
Partially treated acute endocarditis behaves like subacute endocarditis.
3-Post-operative endocarditis
unexplained fever +
heart valve surgery
Infection
Affects=
valve ring
Resemble subacute or acute endocarditis,
Morbidity and mortality are high and
Redo surgery is often required.
Range of organisms=similar to that seen in native valve dis.
endocarditis occurs during
first few weeks
after surgery =
infection with a
coagulase-negative staphylococcus
( introduced during perioperative period)
blood culture
-
1
Investigation
2-echocardiography
3-CBP,ESR,GUE.ECG.
1-Blood culture
3-6
sets of blood cultures -prior to commencing therapy
first 2 specimens -detect bacteraemia in
90%
of culture-+VE Aseptic technique - risk
of contaminants - minimised by sampling from different venepuncture sites.
An in-dwelling line should not be used to take cultures.
Aerobic and anaerobic cultures are required
Typical
organism from two cultures
Persistent
positive blood cultures taken
> 12 hours apart
Three or more
positive cultures taken over more than
1 hour
2-Echocardiography
detect and follows progress of vegetations,
assess valve damage
detect abscess formation.
SIZE
Vegetations as small as 2-4 mm -by transthoracic echo
smaller ones (1-1.5 mm) by transoesophageal echo, esp. abscess formation
investigating patients with prosthetic heart valves.
Vegetations difficult to distinguish in the presence of an abnormal valve;
sensitivity of transthoracic echo is approximately 65%
sensitivity of transoesophageal echo is more than 90%.
Failure to detect vegetations =does not exclude the diagnosis
should not delay treatment.
7
CBP-ESR
normocytic, normochromic anaemia
leucocytosis
thrombocytopenia .
Elevation of ESR
CRP -more reliable than ESR in monitoring progress.
GUE
Proteinuria
microscopic haematuria .
ECG =
atrioventricular block (abscess formation)
occasionally infarction(emboli).
Chest X-ray
evidence of cardiac failure and cardiomegaly
DIAGNOSIS OF INFECTIVE ENDOCARDITIS (MODIFIED DUKE CRITERIA)
Definite endocarditis:
two major (
M+M)
one major and three minor
(M+
m+m+m
)
five minor (
m+m+m+m+m
)
Possible endocarditis:
one major and one minor (
M
+
m
)
three minor,(
m+m+m
)
criteria
Major
Positive blood culture
Typical
organism from two cultures
Persistent
positive blood cultures taken
> 12 hours apart
Three or more
positive cultures taken over more than
1 hour
Endocardial involvement
Positive echocardiographic findings of vegetations
New valvular regurgitation
Minor criteria
1-Predisposing valvular or cardiac abnormality
2-Intravenous drug misuse
3-Pyrexia ≥38°C
4-Embolic phenomenon
5-Vasculitic phenomenon
6-Blood cultures suggestive-organism grown but not achieving major criteria
7-Suggestive echocardiographic findings
8
Management
Case fatality = approximately 20%
higher in those with prosthetic valve endocarditis and those infected with antibiotic-
resistant organisms.
multidisciplinary approach
source of infection - removed e.g. a tooth with an apical abscess
Empirical treatment
1- mode of presentation
2- suspected organism
3- whether the patient has a prosthetic valve and/or penicillin allergy.
1-MODE
Acute
presentation=
flucloxacillin + gentamicin
Subacute or
indolent presentation=
benzyl penicillin + gentamicin
.
2
-
P
enicillin allergy, a
P
rosthetic valve or suspected meticillin-
R
esistant
Staph. aureus
(MRSA) infection =
triple therapy
=
vancomycin+ gentamicin + oral rifampicin
3-MO
1-Empirical for bact. Stept. endocarditis =
penicillin + gentamicin
2- staphylococcal infection =
vancomycin + gentamicin
.
identification of the causal organism
determination of the minimum inhibitory
concentration (MIC)
DURATION
4 Weeks
2-week
treatment regimen - sufficient for fully sensitive strains of
Strep. viridans
and
Strep. bovis
, provided certain conditions are met
CONDITIONS TO BE MET FOR THE SHORT-COURSE TREATMENT
Native valve infection
MIC ≤ 0.1 mg/l
No
adverse prognostic factors (e.g.
heart failure, aortic regurgitation, conduction
defect)
No evidence of thromboembolic disease
No vegetations > 5 mm diameter
Clinical response within 7 days
Other measures
Cardiac surgery (débridement of infected material and valve replacement) esp.
Staph.
aureus
and fungal infections ,
INDICATIONS FOR CARDIAC SURGERY IN IE
Heart failure ( valve damage )
Failure of antibiotic therapy (persistent or uncontrolled infection)
Large vegetations on left-sided heart valves with evidence or
'high risk' of systemic emboli
Abscess formation
9
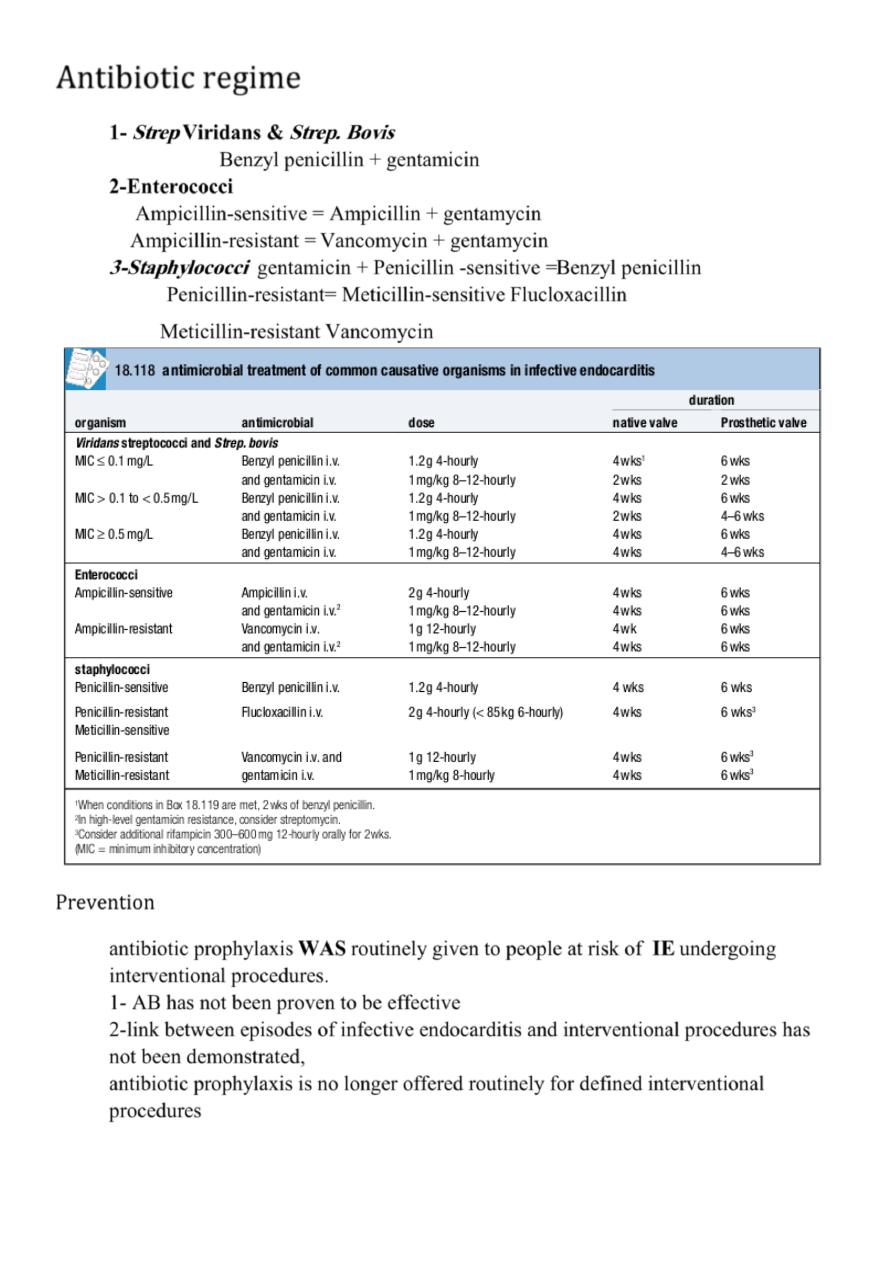
Antibiotic regime
1-
Strep
Viridans &
Strep. Bovis
Benzyl penicillin + gentamicin
2-Enterococci
Ampicillin-sensitive
= Ampicillin + gentamycin
Ampicillin-resistant =
Vancomycin + gentamycin
3-Staphylococci
gentamicin +
Penicillin -sensitive =
Benzyl penicillin
Penicillin-resistant= Meticillin-sensitive
Flucloxacillin
Meticillin-resistant
Vancomycin
Prevention
antibiotic prophylaxis
WAS
routinely given to people at risk of
IE
undergoing
interventiona
l procedures.
1- AB has not been proven to be effective
2-link between episodes of infective endocarditis and interventional procedures has
not been demonstrated,
antibiotic prophylaxis is no longer offered routinely for defined interventional
procedures
