A wide range of organic agents may cause respiratory disorders.
Disease results from a local immune response to animal proteins (e.g. bird
fancier's lung) or fungal antigens in mouldy vegetable matter.
Hypersensitivity pneumonitis is the most common of these conditions.
Hypersensitivity pneumonitis (HP)
Hypersensitivity pneumonitis (also called extrinsic allergic alveolitis) results from
the inhalation of a wide variety of organic antigens which give rise to a diffuse
immune complex reaction in the walls of the alveoli and bronchioles.
Common causes include farm worker's lung and bird fancier's lung.
Examples of lung diseases caused by organic dusts
Pathogenesis and pathology :
The pathology of HP is consistent with both type III and type IV immunological
mechanism.
Precipitating IgG antibodies may be detected in the serum and a type III Arthus
reaction is believed to occur in the lung,
where the precipitation of immune complexes results in activation of complement
and an inflammatory response in the alveolar walls,
characterised by the influx of mononuclear cells and foamy histiocytes.
The presence of poorly formed non-caseating granulomas in the alveolar walls
suggests that type IV responses are also important.
Chronic forms of the disease may be accompanied by fibrosis.
For reasons that remain uncertain, there is a lower incidence of HP in smokers
compared to non-smokers.
Clinical features
The acute form of the disease should be suspected when anyone who is exposed to
organic dust complains, within a few hours of re-exposure to the same dust, of
influenza-like symptoms such as headache, myalgia, malaise, pyrexia, dry
cough and breathlessness.
Chest auscultation reveals widespread end-inspiratory crackles and squeaks.
Lung diseases due to organic dusts
Disorder
Source
Antigen/agent
Farmer's lung*
Mouldy hay, straw, grain Micropolyspora faeni
Aspergillus fumigatus
Bird fancier's lung* Avian excreta, proteins
and feathers
Avian serum proteins

In cases attributable to chronic low-level exposure (as may be the case with an
indoor pet bird), the presentation is more often insidious and established fibrosis
may be present by the time the disease is recognised.
If unchecked, HP may progress to cause severe respiratory disability, hypoxaemia,
pulmonary hypertension, cor pulmonale and eventually death.
Investigations:
The classical chest X-ray shows upper zone diffuse micronodular shadowing.
HRCT is more sensitive and the appearances may provide information on the stage
of disease.
Acute forms are characterised by ground glass shadowing and areas of
consolidation superimposed on small centrilobar nodular opacities; the
distribution is typically bilateral with upper and middle lobe predominance.
In more chronic disease, features of fibrosis such as volume loss, linear opacities
and architectural distortion appear.
Pulmonary function tests show a restrictive ventilatory defect with reduced lung
volumes and impaired gas transfer, dynamic tests may detect oxygen desaturation
and, in more advanced disease, type I respiratory failure is present at rest.
Predictive factors in the identification of hypersensitivity pneumonitis
1. Exposure to a known offending antigen
2. Positive precipitating antibodies to offending antigen
3. Recurrent episodes of symptoms
4. Inspiratory crackles on examination
5. Symptoms occurring 4-8 hours after exposure
6.
Weight loss
Diagnosis :
The diagnosis of HP is usually based on the characteristic clinical and radiological
features,
together with the identification of a potential source of antigen at the patient's
home or place of work.
It may be supported by a positive precipitin test or by more sensitive serological
tests based on the enzyme-linked immunosorbent assay (ELISA) technique.
However, the great majority of farmers with positive precipitins do not have
farmer's lung, and up to 15% of pigeon breeders may have positive serum
precipitins yet remain healthy.
Where HP is suspected but the cause is not readily apparent, a visit to the
patient's home or workplace should be arranged.
Occasionally, such as when an agent not previously recognised as causing HP is
suspected, provocation testing may be necessary to prove the diagnosis;
inhalation of the relevant antigen is followed by pyrexia and a reduction in VC and
gas transfer factor after 3-6 hours, if positive.

BAL fluid usually shows an increase in the number of CD8
+
T lymphocytes.
Transbronchial biopsy can occasionally provide sufficient tissue for a confident
diagnosis, but open lung biopsy may be necessary.
Management:
Whenever possible, the patient should cease exposure to the inciting agent.
However, in some cases this may be difficult to achieve, because of either
implications for livelihood (e.g. farmers) or addiction to hobbies (e.g. pigeon
breeders).
Dust masks with appropriate filters may minimise exposure and may be combined
with methods of reducing levels of antigen (e.g. drying hay before storage).
In acute cases prednisolone should be given for 3-4 weeks, starting with an oral
dose of 40 mg per day.
Severely hypoxaemic patients may require high-concentration oxygen therapy
initially.
Most patients recover completely, but the development of interstitial fibrosis is
usually accompanied by permanent disability.
Lung diseases due to inorganic dusts
COAL WORKER'S PNEUMOCONIOSIS
Prolonged inhalation of coal dust overwhelms the alveolar macrophages, which
aggregate to form macules in or near the centre of the secondary pulmonary
lobule.
A fibrotic reaction ensues, resulting in the appearance of scattered discrete
fibrotic lesions that constitute simple coal worker's pneumoconiosis (SCWP).
This can be divided into three categories on the basis of the size and extent of
nodularity on the chest X-ray.
However, it does not cause pulmonary function abnormalities nor does it give rise
to symptoms or progress following cessation of exposure.
Complicated pneumoconiosis invariably develops against a background of simple
pneumoconiosis.
In this form of the disease, large dense masses appear mainly in the upper
lobes (also known as progressive massive fibrosis, PMF).
Cavitation may occur, raising important differential diagnoses such as lung cancer,
TB and Wegener's granulomatosis .
In contrast to SCWP, PMF is usually associated with cough, production of sputum,
that may be black (melanoptysis) and breathlessness.
It may progress to respiratory failure after cessation of exposure and right
ventricular failure.
Caplan's syndrome describes the coexistence of rheumatoid arthritis and rounded
fibrotic nodules 0.5-5 cm in diameter.
These are mainly in the periphery of the lung fields and show pathological
features similar to a rheumatoid nodule including central necrosis, palisading
histiocytes, and a peripheral rim of lymphocytes and plasma cells.
This syndrome may also occur in other types of pneumoconiosis.

SILICOSIS
Silicosis results from the inhalation of crystalline or free silica, usually in the form
of quartz.
The clinical and radiological features are similar to those of coal worker's
pneumoconiosis with multiple well-circumscribed 3-5 mm nodular opacities
predominantly in the mid- and upper zones.
As the disease progresses some of these may coalesce, particularly in the upper
lobes.
Enlargement of the hilar glands with an 'egg-shell' pattern of calcification is said
to be characteristic but is uncommon and non-specific.
Patients may be at increased risk of TB-silicotuberculosis.
Silica is highly fibrogenic and the disease is usually progressive (even when
exposure ceases).
The patient should, therefore, be removed from the offending environment as
soon as possible
Intense exposure to very fine crystalline silica dust can cause a more acute disease
similar to alveolar proteinosis with over-production of surfactant by type II
alveolar pneumocytes.
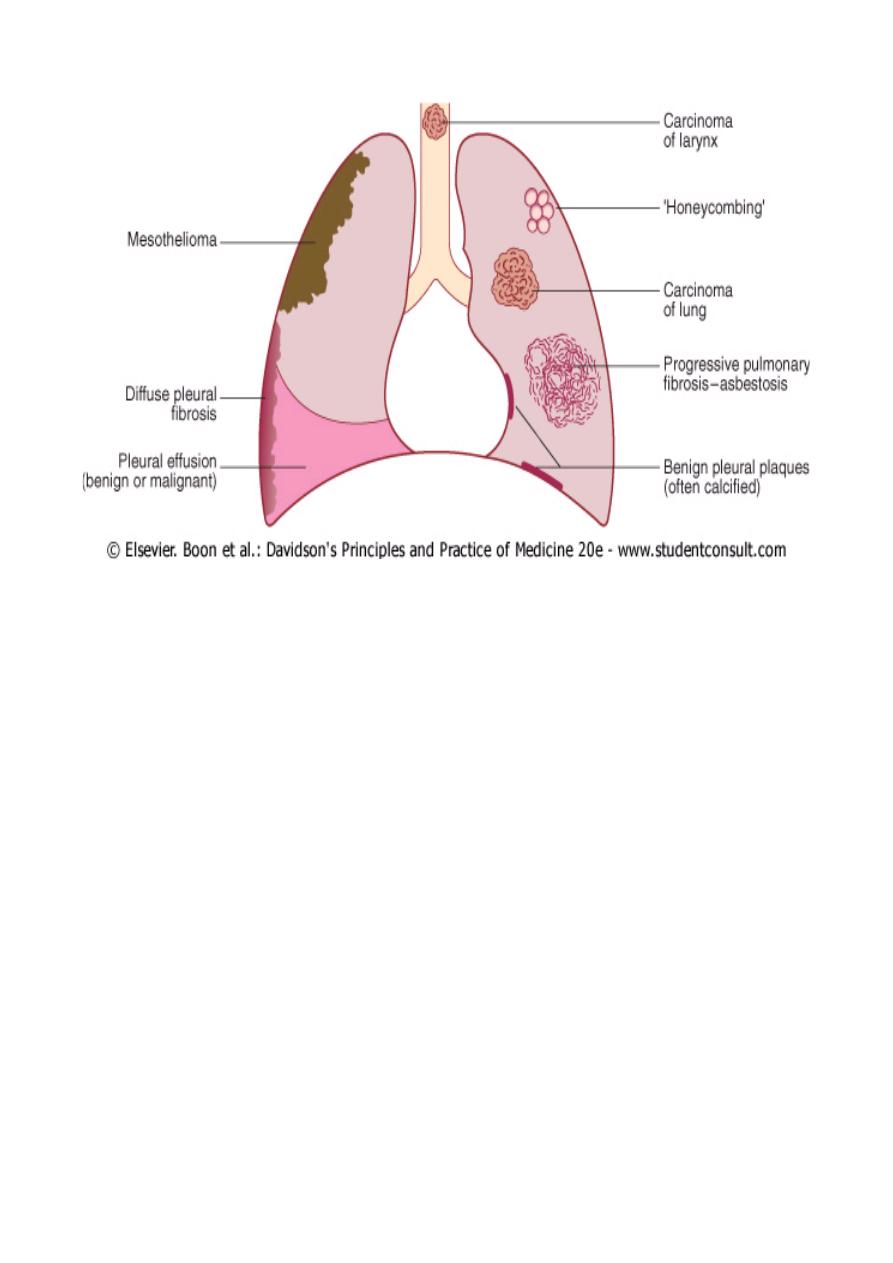
ASBESTOSIS
The main types of the fibrous mineral asbestos are chrysotile (white asbestos),
which accounts for 90% of the world's production, crocidolite (blue asbestos) and
amosite (brown asbestos).
Exposure occurs in a variety of occupations and is a recognised risk factor for
several respiratory diseases , including carcinoma of the lung and larynx.
The law in many countries now enforces improvements in standards of industrial
hygiene and provides compensation for asbestos-related disease.
Asbestosis is a diffuse interstitial fibrosis of the lungs that may or may not be
associated with fibrosis of the parietal or visceral layer of the pleura.
The condition seldom develops less than 20 years after the start of exposure and
usually follows substantial and prolonged asbestos exposure over many years.
The risk increases with the amount inhaled.
Asbestos fibres are cleared by mucociliary clearance, by pulmonary macrophages
and by dissolution.
Incomplete phagocytosis of fibres by macrophages triggers a fibrotic process that
is typically most marked in the lower lobes.
Patients usually present with exertional breathlessness and fine, late inspiratory
crackles over the lower zones.
Digital clubbing (reported in 40% of patients) is an adverse prognostic feature.
The chest X-ray shows bi-basal reticular nodular shadowing and asbestos-related
pleural disease is usually present.
HRCT scanning is more sensitive than plain radiography and typically shows
basal, subpleural, curvilinear opacities, band-like opacities and occasionally
'honeycombing'.
Pulmonary function tests typically show a restrictive defect with decreased lung
volumes and reduced gas transfer factor.
The diagnosis is usually established by a history of substantial asbestos exposure
with the clinical, radiological and pulmonary function abnormalities.
Asbestos bodies may be identified in sputum or BAL and confirm asbestos
exposure.
Lung biopsy is rarely necessary but may be required to exclude other causes of
interstitial lung disease.
If a history of exposure is uncertain, asbestos fibre counts may be performed on
lung biopsy material.
Management
No specific treatment is available. Asbestosis usually progresses very slowly.
In advanced cases respiratory failure and cor pulmonale may develop and should
be treated appropriately.
About 40% of patients (who usually smoke) develop carcinoma of the lung and 10%
may develop mesothelioma.
Patients should be provided with appropriate legal advice if asbestos exposure
occurred as a result of negligent exposure.
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
This describes the acute, diffuse pulmonary inflammatory response to either
direct (via airway or chest trauma) or indirect blood-borne insults that originate
from extrapulmonary pathology.It is characterised by:
1. neutrophil sequestration in pulmonary capillaries,
2. increased capillary permeability,

3. protein-rich pulmonary oedema with hyaline membrane formation,
4. damage to type 2 pneumocytes leading to surfactant depletion,
5. alveolar collapse
6. and reduction in lung compliance.
•
If this early phase does not resolve with treatment of the underlying cause, a
fibroproliferative phase ensues and causes progressive pulmonary fibrosis.
•
It is frequently associated with other organ dysfunction (kidney, heart, gut,
liver, coagulation) as part of multiple organ failure.
The term ARDS is often limited to patients requiring ventilatory support on the
ICU, but less severe forms, conventionally referred to as acute lung injury (ALI)
and with similar pathology, occur on acute medical and surgical wards.
The clinical symptoms and signs are not specific, sharing many features with other
pulmonary conditions.
The criteria defining ARDS are:
hypoxaemia
chest X-ray showing diffuse bilateral infiltrates
absence of a raised left atrial pressure: PAWP < 15 mmHg
impaired lung compliance.
CONDITIONS PREDISPOSING TO ARDS:
Inhalation (direct)
1. Aspiration of gastric contents
2. Toxic gases/burn injury
3. Pneumonia
4. Blunt chest trauma
5. Near-drowning
Blood-borne (indirect)
1. Sepsis
2. Necrotic tissue (particularly bowel)
3. Multiple trauma
4. Pancreatitis
5. Cardiopulmonary bypass
6. Severe burns
7. Drugs (heroin, barbiturates, thiazides)
8. Major blood transfusion reaction
9. Anaphylaxis (wasp, bee, snake venom)
10.Fat embolism
11.Carcinomatosis
12.Obstetric crises (amniotic fluid embolus, eclampsia)
