1
Medicine Dr. Sabah
CONGENITAL HEART DISEASE
CYANOTIC
1. TETRALOGY OF FALLOT
2. PULMONARY ATRESIA WITH- VSD & WITH INTACT IVS
3. DOUBLE OUTLET RT.V(BOTH AORTA & PA)
4. TRANSPOSITION OF GREAT VESSELS WITH VSD OR INTACT IVS
5. TOTAL ANOMALOUS PULM.VENOUS RETURN
6. EBSTIEN DIS.
7. TRUNCUS ARTERIOUS
8. SINGLE VENTRICLE
9. HYPOPLASTIC LEFT HEART
10. PULMONARY AV FISTULA
LITTLE OR NO CAYNOSIS
1) WITH LEFT TO RIGHT SHUNT =VSD=ASD=PDA=CORRECTED TRANSPOSITION=AORTO-
PULMONARY DEFECT
2) WITHOUT SHUNT=COARCTATION=PULMONARY STENOSIS=AORTIC STENOSIS=MITRAL STENOSIS
2
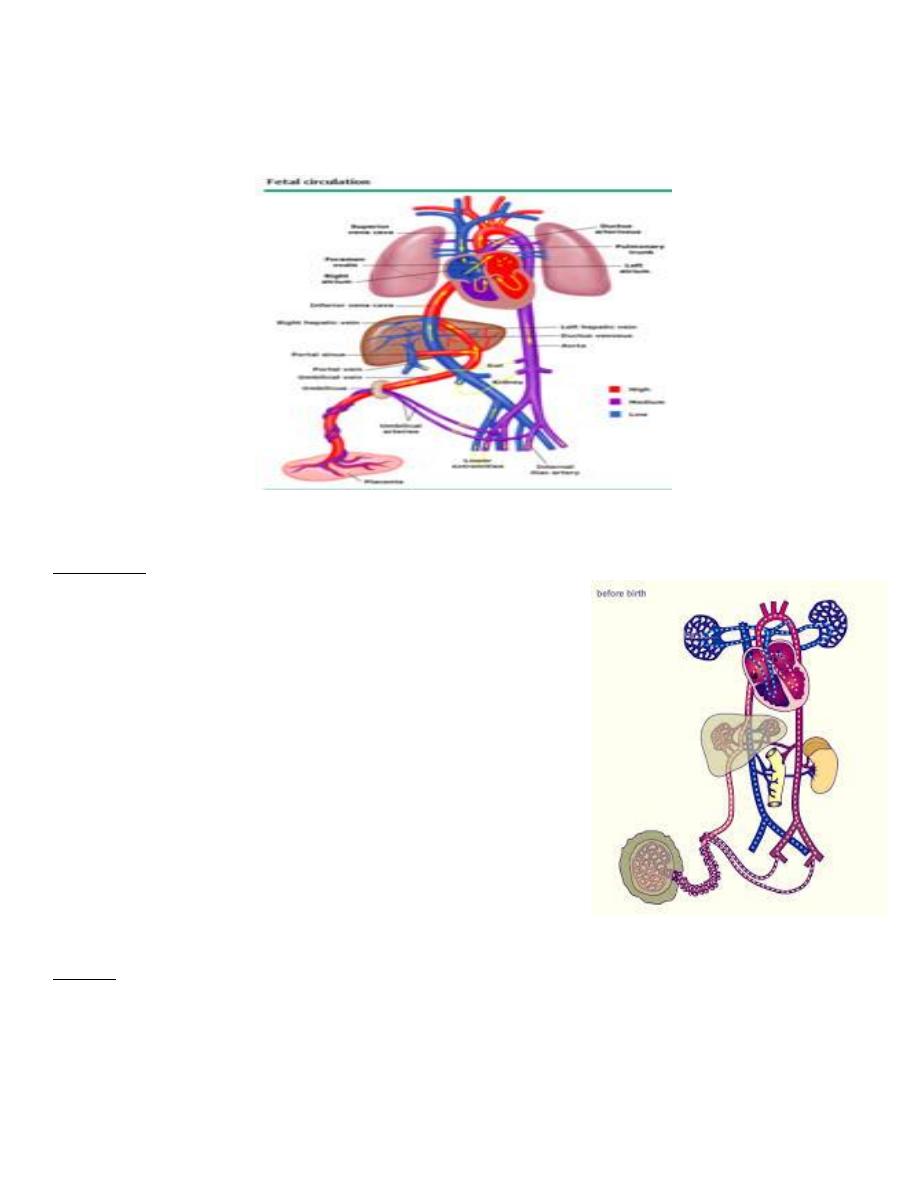
Fetal circulation
fetus has only a small flow of blood through lungs
fetal circulation allows oxygenated blood from placenta => pass directly to left side of heart
(foramen ovale) without lungs
Changes in the circulation at birth
In the fetus
Oxygenated blood umbilical vein => inferior VC(via DV)
Oxygenated blood streams => right atrium ( open foramen
ovale )=> left atrium and (via the left ventricle )=> aorta.
Venous blood from superior vena cava crosses under main
blood stream => right atrium ( partly mixed with oxygenated
blood ) => right ventricle and pulmonary artery.
( pulmonary vasculature has a high resistance and so little
blood passes to lungs;)most blood passes( through
ductusarteriosus ) =>descending aorta.
aortic isthmus =constriction in aorta lies in aortic arch before
junction with ductusarteriosus
limits the flow of oxygen-rich blood to the descending aorta. =
less oxygen-rich blood is supplied to organ systems that take
up their function mainly after birth (kidneys and int. tract.)
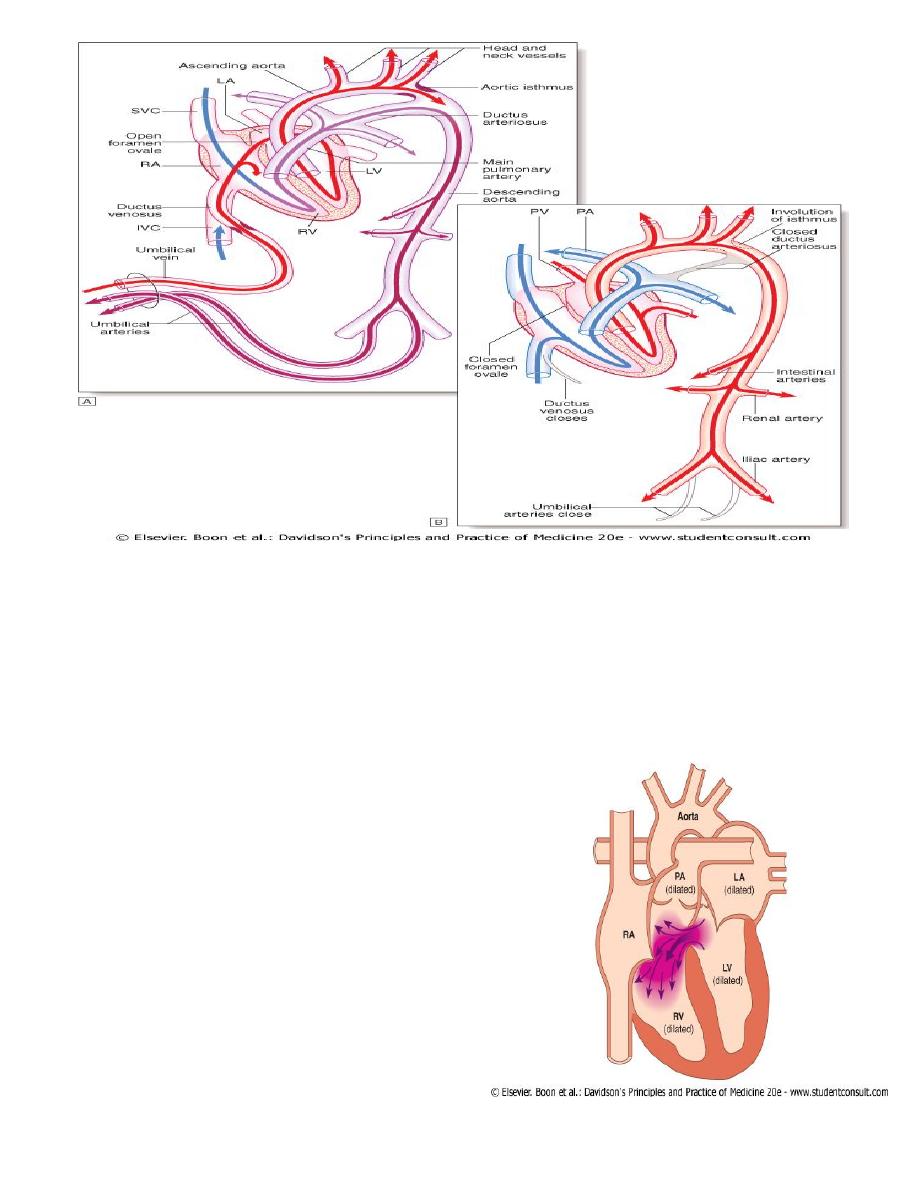
At birth
1- lungs expand with air and pulmonary vascular resistance falls ==>
blood flows to lungs and back Left atrium.
2- lt. atrial pressure rises above RT. atrial pressure= flap valve of foramen ovale closes.
3- umbilical arteries and ductusvenosus= close.
4- ductus arteriosus = closes under influence of hormonal changes (particularly prostaglandins)
5- aortic isthmus== expands
3
1- VENTRICULAR SEPTAL DEFECT مهم
Aetiology
Congenital ventricular septal defect occurs as a result of incomplete septation of the ventricles.
Embryologically IV S = membranous +muscular portion MUSC.=inflow, trabecular and outflow
portions.
Most congenital defects = 'perimembranous', i.e. at junction of membranous and muscular portions
80% membraneous,20% muscular).
VSD –
Most common congenital C. defect
- once in 500 live births.
isolated or part of complex congenital heart
disease.
Acquired VSD -result from rupture as a
complication of acute MI or rarely from trauma
4
Clinical features
Flow from the high-pressure LV to the low-pressure RV during systole produces a pansystolic murmur
usually heard best at the left sternal edge but radiating all over the precordium . A small defect often
produces a loud murmur (maladie de Roger) in the absence of other haemodynamic disturbance.
Conversely, a large defect produces a softer murmur, particularly if pressure in the RV is elevated. This
may be found immediately after birth, while pulmonary vascular resistance remains high, or when the
shunt is reversed in Eisenmenger’s syndrome.
Congenital ventricular septal defect may present as cardiac failure in infants, as a murmur with only
minor haemodynamic disturbance in older children or adults, or rarely as Eisenmenger’s syndrome. In
a proportion of infants, the murmur gets quieter or disappears due to spontaneous closure of the
defect. If cardiac failure complicates a large defect, it is usually absent in the immediate postnatal
period and only becomes apparent in the first 4–6 weeks of life. In addition to the murmur, there is
prominent parasternal pulsation, tachypnoea and indrawing of the lower ribs on inspiration.
Investigation
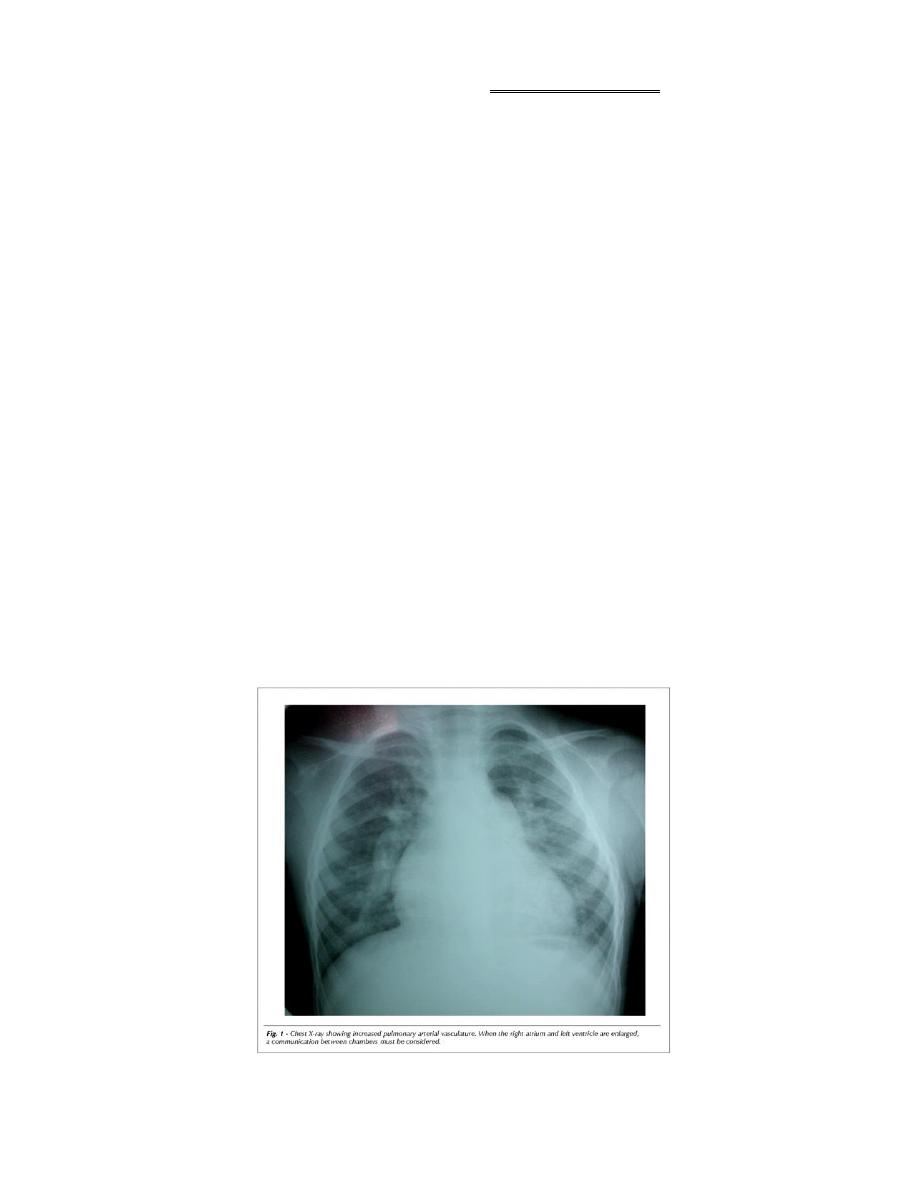
1) chest X-ray shows pulmonary plethora
2) ECG shows bilateral ventricular hypertrophy
Management
Small VSD require no specific treatment (endocarditis prophylaxis) most 50% close spontaneously
Cardiac failure =digoxin and diuretics. Persisting failure =surgical repair of the defect.
Percutaneous closure devices = under development.
o Doppler echocardiography =predict small septal defects likely to close spontaneously.
o
Eisenmenger's syndrome
= avoided by monitoring for signs of rising pulmonary resistance (serial
ECG and echocardiography) and carrying out surgical repair when appropriate.
o Surgical closure =contraindicated in fully developed Eisenmenger's
o heart-lung transplantation ?treatment.
Prognosis:
Except in the case of Eisenmenger's syndrome, long-term prognosis is very good in
congenital ventricular septal defect..
2- ATRIAL SEPTAL DEFECT
مهم
Aetiology
common congenital heart defects,
occurs twice as frequently in females.
1- 'ostiumsecundum' defects=fossa ovalis ( foramen ovale)
2- 'Ostiumprimum' defects =defect in the AV septum
associated with a 'cleft mitral valve' (split anterior leaflet).
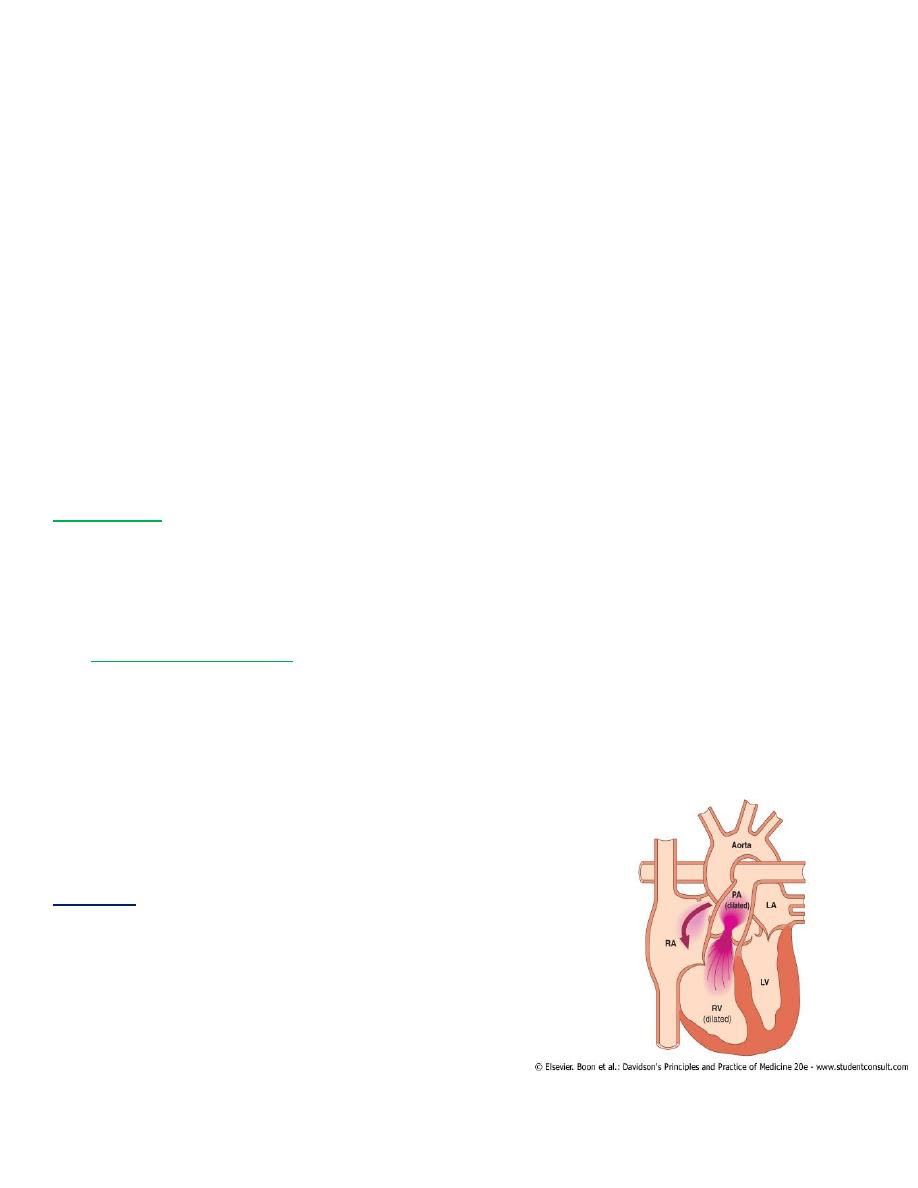
HAEMODYNAMICS
5
normal RV more compliant than left
large volume of blood shunts through defect from left to right atrium=> right ventricle and
pulmonary arteries gradual enlargement of right side of heart and PA
Pulmonary hypertension and shunt reversal(less common and tend to occur later in life than with
other types of left-to-right shunt.)
Clinical features
Most children = free of symptoms for many years
detected - routine clinical exam. or following a chest X-ray.
Dyspnoea, chest infections, cardiac failure and arrhythmias, especially atrial fibrillation.
Physical signs = volume overload of RV
wide fixed splitting of the second heart sound:
wide –RV ejection (increased stroke volume and right bundle branch block
fixed =septal defect equalises left and right atrial pressures throughout respiratory cycle
systolic flow murmur over the pulmonary valve.
children with a large shunt=diastolic flow murmur over the tricuspid valve=high-pitched(cf.MS)
Investigation
The chest X-ray =
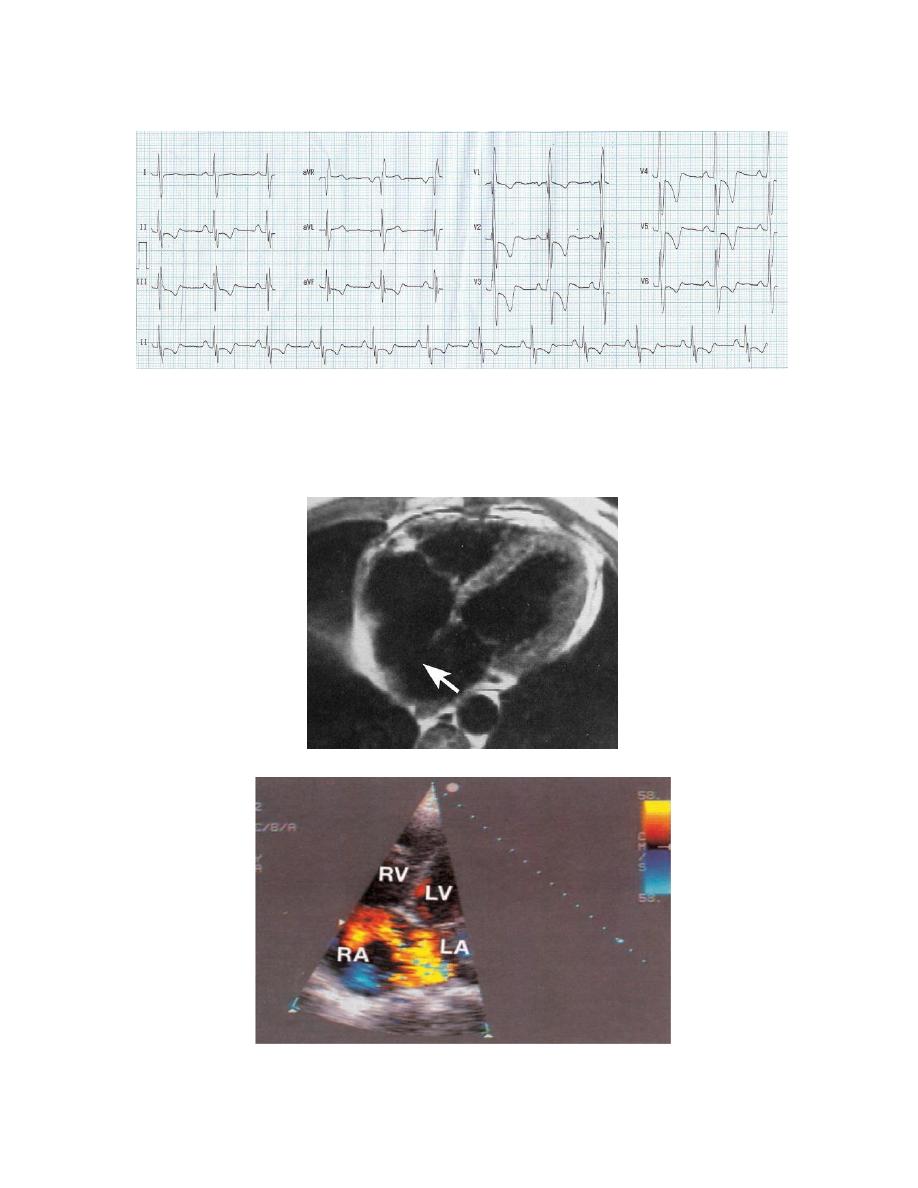
The ECG
Echocardiography =
**enlargement of heart and pulmonary artery +pulmonary plethora.
6
**
incomplete right bundle branch block
( right ventricular depolarisation is delayed as a result of
ventricular dilatation)
(with a 'primum' defect there is also left axis deviation).
demonstrate defect + RV dilatation,
RV hypertrophy & @PA dilatation.
precise size and location of defect = transoesophageal echocardiography.
7
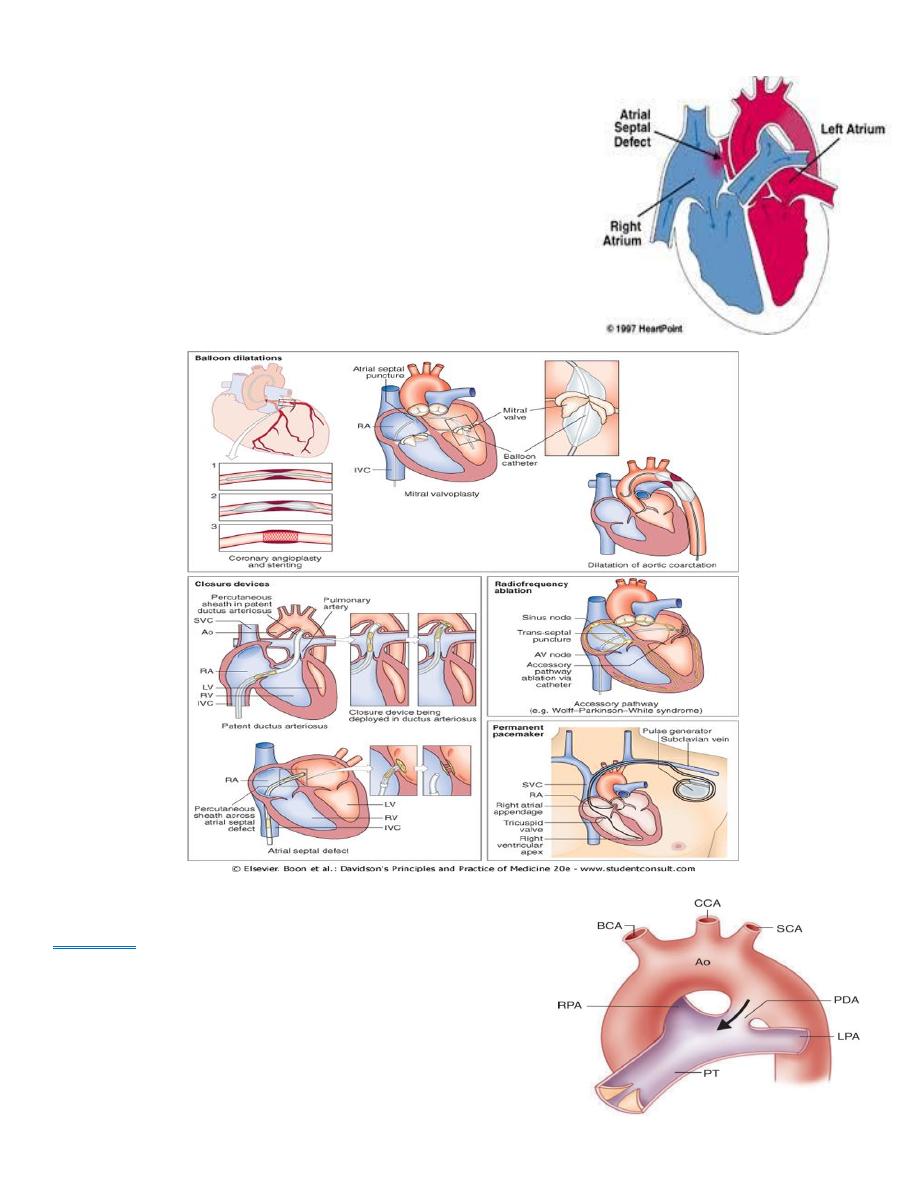
Management
Defects less than 8 mm.=rarely significant
Atrial septal defects +pulmonary flow is increased 50% above
systemic flow (i.e. flow ratio of 1.5:1) =large enough to be
clinically recognisable
should be closed surgically.
Closure =implantable closure devices .
long-term prognosis thereafter= excellent (unless pulmonary
hypertension).
contraindications to surgery= Severe pulmonary hypertension
and shunt reversal
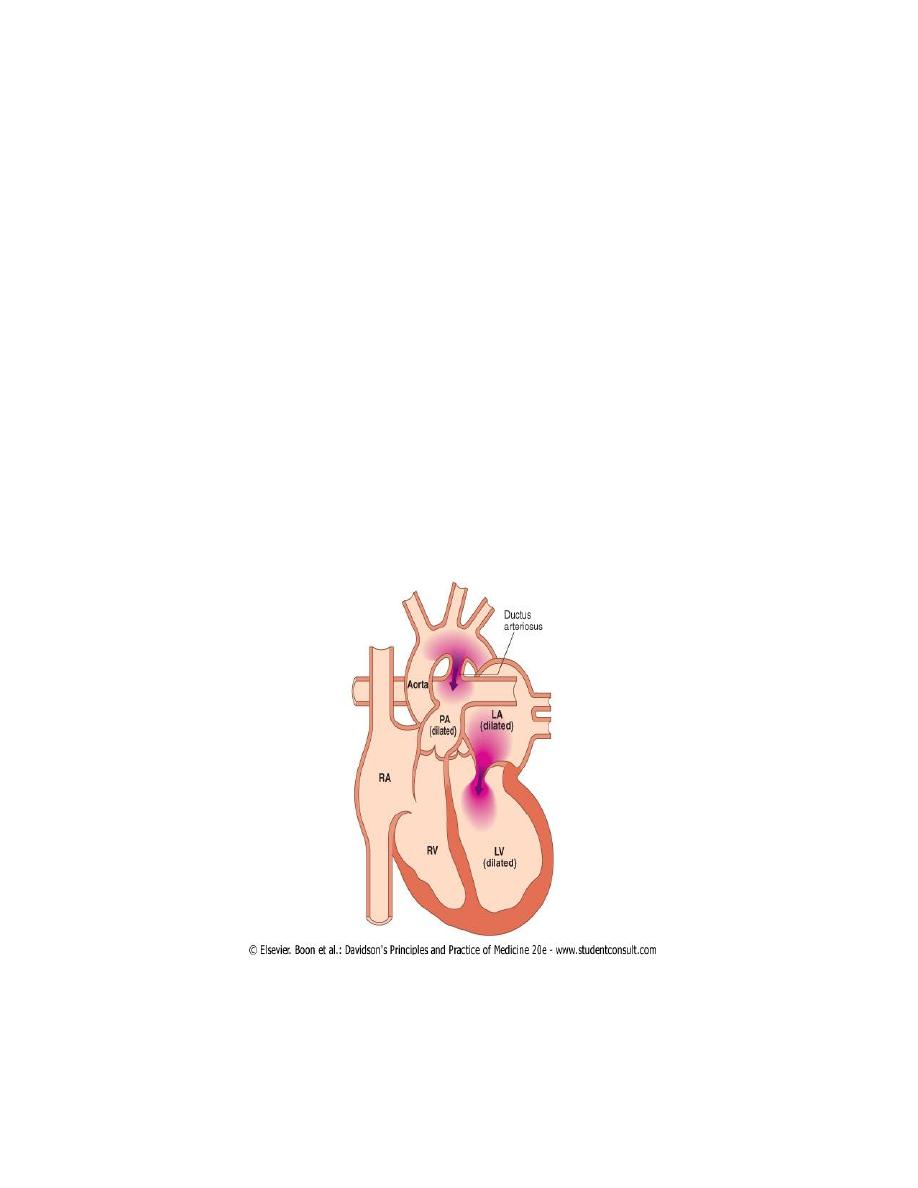
3-PERSISTENT DUCTUS ARTERIOSUS
Aetiology
During fetal life, before lungs begin to function
most of blood from pulm. a.passes through
ductusarteriosus into aorta .
Normally - ductus closes soon but sometimes it fails to do
so.
more common in females.
8
Pathophysiology
pressure in aorta is higher than pulmonary artery (PA) continuous arteriovenous shunt=
volume depends on size of ductus.
50% of LV output may be recirculated through lungs, with a consequent increase in the work of
heart
Functionally close several hours after birth and anatomocally within 4-8 weeks
Clinical features
small shunts = no symptoms for years,
Large ductus = growth and development may be retarded.
No disability in infancy
cardiac failure =dyspnoea.
A continuous 'machinery' murmur = with late systolic accentuation, maximal 2
nd
.left intercostal
space below the clavicle frequently accompanied by a thrill.
Pulses -increased in volume.
A large left-to-right shunt in infancy =considerable rise in pulmonary artery pressure =>leads to
progressive pulmonary vascular damage
CXR= Enlargement of the pulmonary artery
ECG =usually normal..
Complication
1) Persistent ductus with reversed shunting
2) If pulmonary vascular resistance increases=> pulmonary artery pressure rises =>equals or exceeds
aortic pressure.
3) shunt through defect =reverse=> central cyanosis (Eisenmenger's syndrome more apparent in the
feet and toes than in the upper part of the body.
9
4) murmur becomes quieter, may be confined to systole or may disappear.
5) ECG shows evidence of right ventricular hypertrophy
Management
Closure at cardiac catheterisation =implantable occlusive device
1. Closure =undertaken in infancy if shunt is significant and pulmonary resistance not elevated
2. delayed until later childhood in those with smaller shunt (closure remains advisable to reduce risk
of endocarditis).
3. Pharmacological treatment in neonatal period
When ductus is structurally intact, a prostaglandin synthetase inhibitor (indometacin or
ibuprofen) may be used in the first week of life to induce closure.
congenital defect with impaired lung perfusion (e.g. severe pulmonary stenosis and left-to-right
shunt through the ductus)=advisable to improve oxygenation by keeping ductus open with
prostaglandin treatment. Unfortunately, these treatments do not work if the ductus is
intrinsically abnormal.
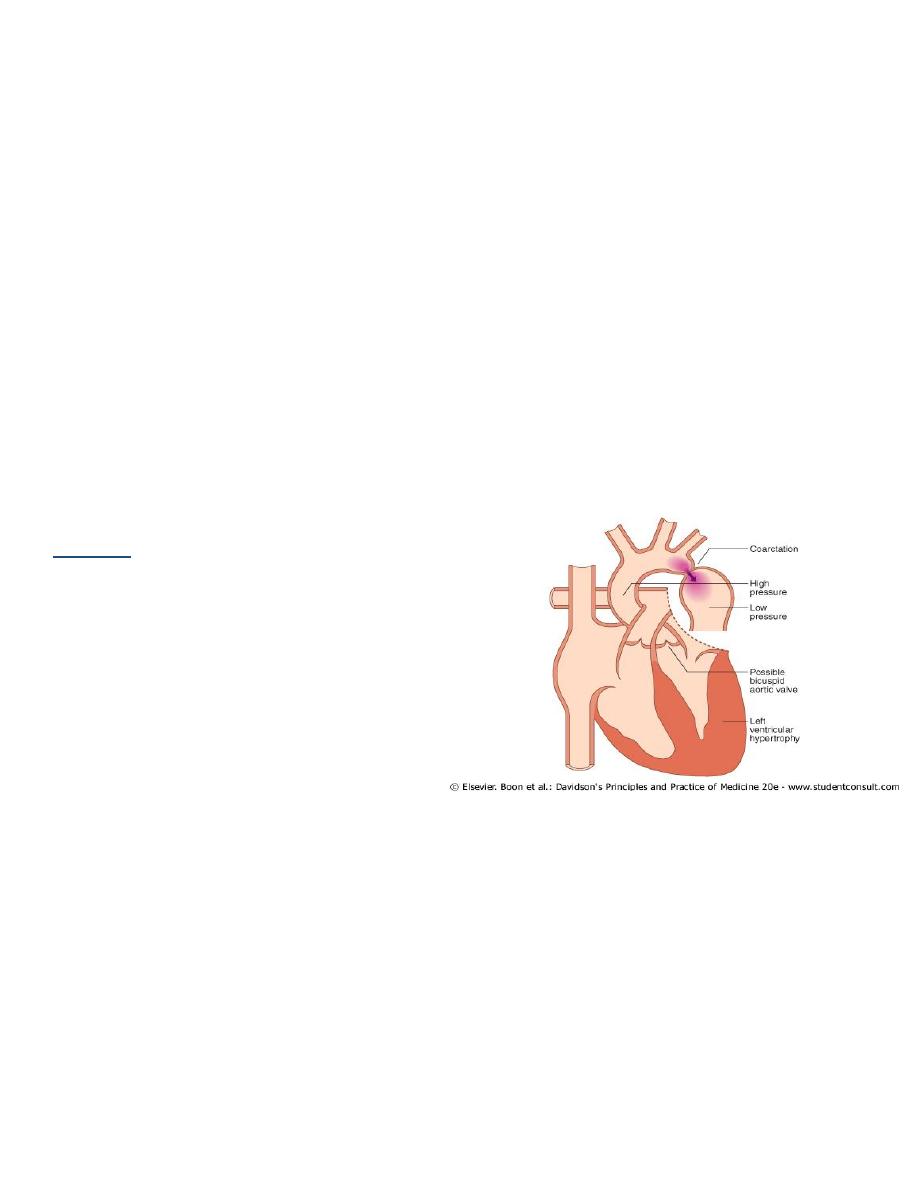
4- COARCTATION OF THE AORTA
Aetiology
twice as common in males as in females
occurs in 1 in 4000 children.
associated with other abnormalities, esp.
bicuspid aortic valve
'berry' aneurysms of the cerebral circulation
Acquired coarctation of aorta = rare may
follow trauma or occur as a complication of
a progressive arteritis (Takayasu's disease,
Clinical features
∞ cardiac failure in newborn, symptoms often absent =detected in older children or adults.
∞ Headaches =hypertension proximal to coarctation
∞ occasionally weakness or cramps in legs may result from decreased circulation in the lower part of
the body.
∞ TBP raised in upper body but normal or low in the legs.
∞ femoral pulses = weak,
delayed in comparison with radial pulse
∞ systolic murmur -usually heard posteriorly, over coarctation.
∞ may also be an ejection click and systolic murmur in aortic area (bicuspid aortic valve).
∞ As a result of aortic narrowing, collaterals form, mainly involving periscapular, internal mammary
and intercostal arterieslocalised bruits
10
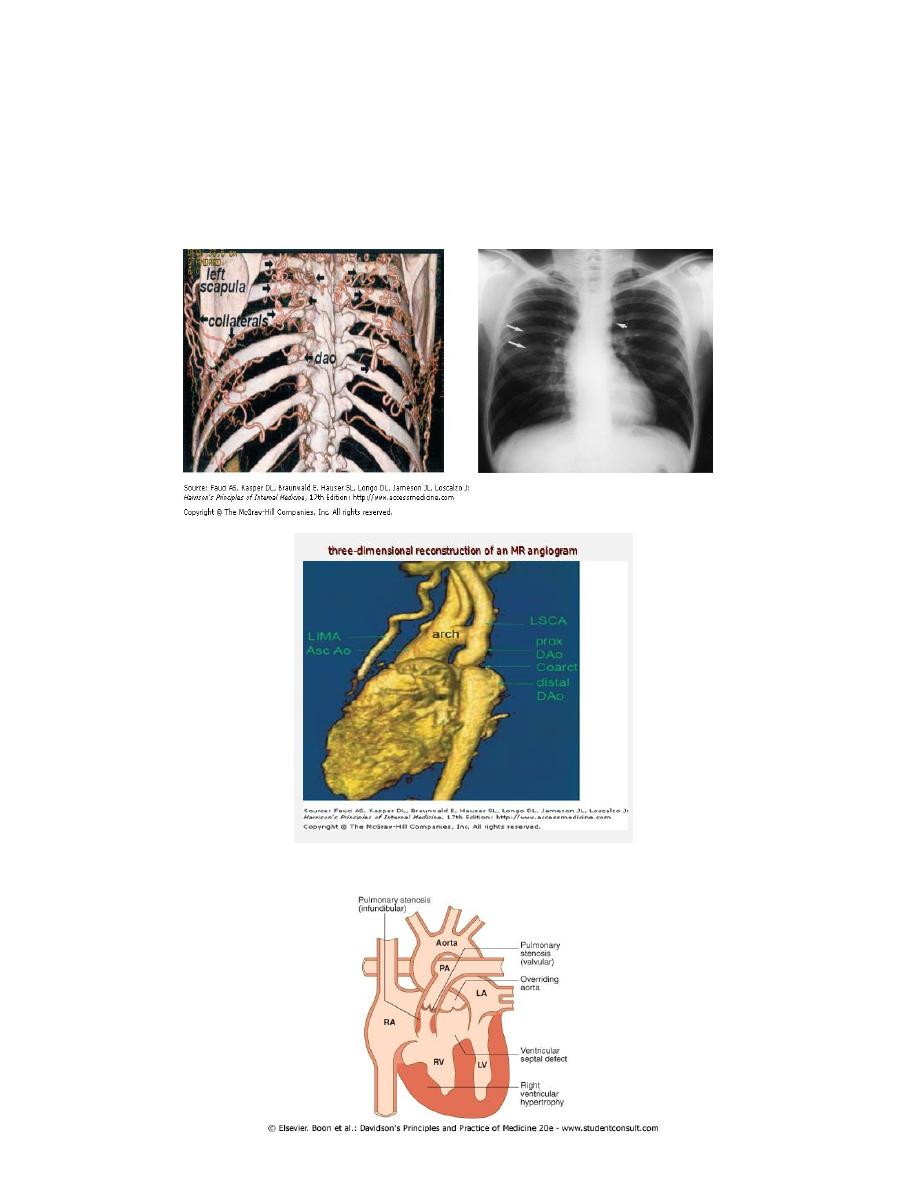
Investigation
Chest X-ray in early childhood is often normal at a later age may show
1- changes in contour of aorta (indentation of the descending aorta, '3 sign') and
2-notching of the under-surfaces of ribs from collaterals.
MRI =ideal for demonstrating the lesion
ECG =left ventricular hypertrophy
TETRALOGY OF FALLOT
-four components
