1
Medicine Dr.Sabah
DISEASES OF THE MYOCARDIUM
1- MYOCARDITIS
2- CARDIOMYOPATHY
3- SPECIFIC DISEASES OF HEART MUSCLE
Z Myocarditis' and ‘Cardiomyopathy‘
Z conditions that primarily affect heart muscle
TYPES:
1- ACUTE-MYOCARDITIS, VIRAL, NON-VIRAL
2- ”CHRONIC”-CARDIOMYOPATHY, PRIMARY(IDIOPATHIC) & SECONDARY
TYPES DILATED
a. HYPERTROPHIC,
b. RESTRICTIVE,
c. OBLITERATIVE,
d. ARVD
ACUTE MYOCARDITIS:
j
Acute inflammatory condition complicating wide variety of infections
j
Aetiology:
1. infection of myocardium
2. effects of circulating toxins.
j
Viral infection - most common cause esp.
Coxsackie viruses (35 cases per 1000 infections)
influenza viruses A and B (25 cases per 1000 infections).
j
Direct effect
j
Several weeks after initial viral infection
j
susceptibility is increased by corticosteroid treatment, immunosuppression, radiation,
previous myocardial damage , exercise.
j
Bacterial and Protozoal infections .e.g. Lyme disease (Borrelia burgdorferi, )
j
Clinical picture
2
j
Symptomless
------
1. fulminant heart failure
2. inappropriate tachycardia
3. abnormal ECG
4. may be heralded by a 'flu'-like illness.
j
Investigations
a. ECG: changes , common - non-specific.
b. Biochemical markers of myocardial injury (e.g. troponin I and T, creatine kinase) -
elevated in proportion to extent of damage.
c. Echocardiography - left ventricular dysfunction - sometimes regional (due to focal
myocarditis), if diagnosis is uncertain-can be confirmed by endomyocardial biopsy.
j
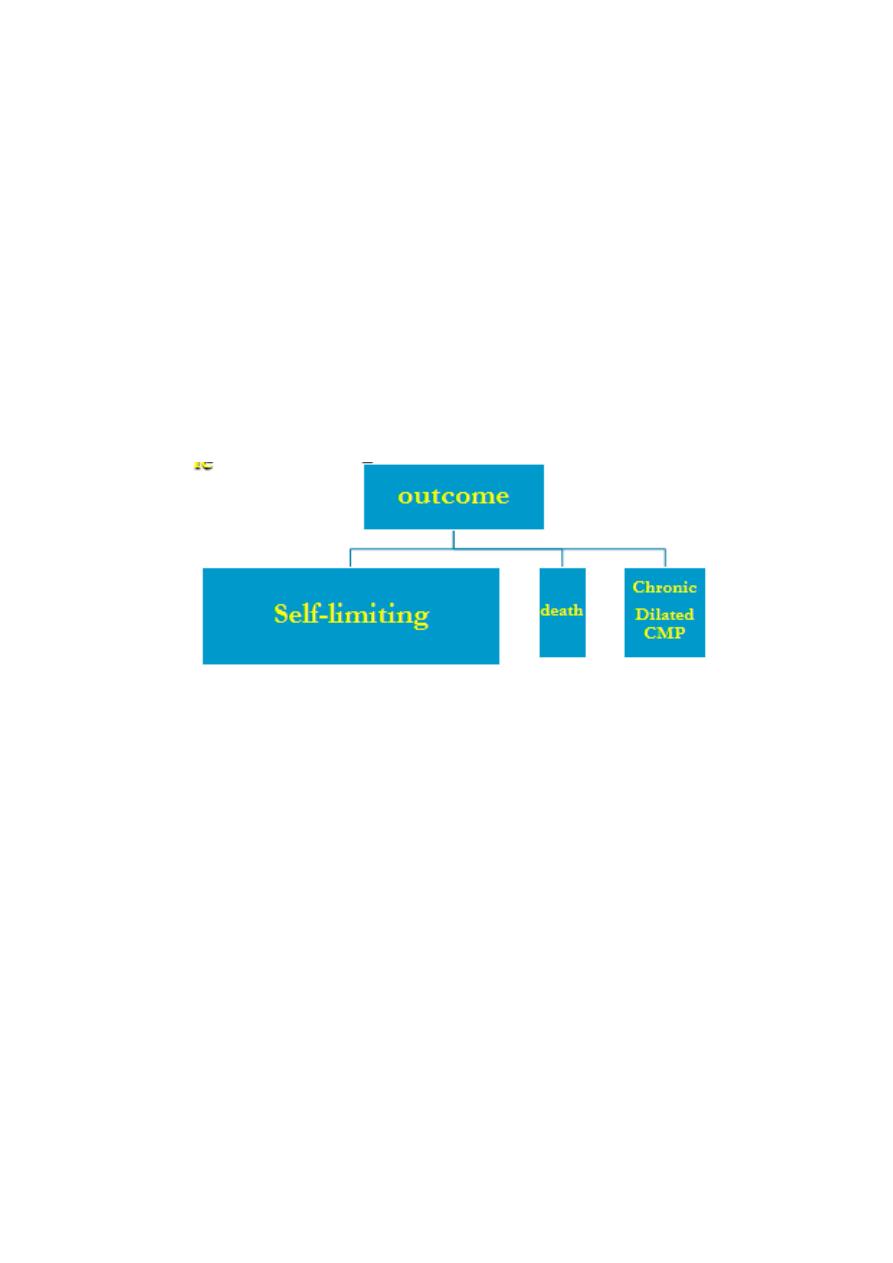
Outcome:
1) self-limiting- Most cases immediate prognosis = excellent.
2) death – ventricular arrhythmia, rapidly progressive heart failure. cause of sudden and
unexpected death young athletes.
3) chronic low-grade myocarditis or dilated cardiomyopathy ; e.g., in Chagas disease .(some
forms ) patient frequently recovers from acute infection but goes on to develop a chronic
dilated cardiomyopathy 10 or 20 years later
j
Treatment
A. Most cases = only supportive therapy .
B. Specific antimicrobial therapy = used if a causative organism has been identified- rare
C. Treatment for cardiac failure or arrhythmias
D. Avoid intense physical exertion = can induce potentially fatal ventricular arrhythmias.
E. No benefit from corticosteroids and immunosuppressive agents.
3
CARDIOMYOPATHY:
Ó
TYPES
Ó
CAUSES
Ó
CLINICAL MANIFESTATIONS
Ó
INVESTIGATIONS
Ó
TREATMENT

4
Definition:
£
Group of diseases that primarily affect heart muscle
£
Not the result of
- congenital HD
- acquired valvular HD
- hypertensive HD
- coronary arterial D
- pericardial abnormalities.
£
The diffuse myocardial fibrosis that accompanies multiple myocardial scars produced by
myocardial infarctions can impair left ventricular (LV) function and is frequently referred to
as ischemic cardiomyopathy.
£
use of the term cardiomyopathy should be avoided; instead, term restricted to a condition
primarily involving the myocardium.
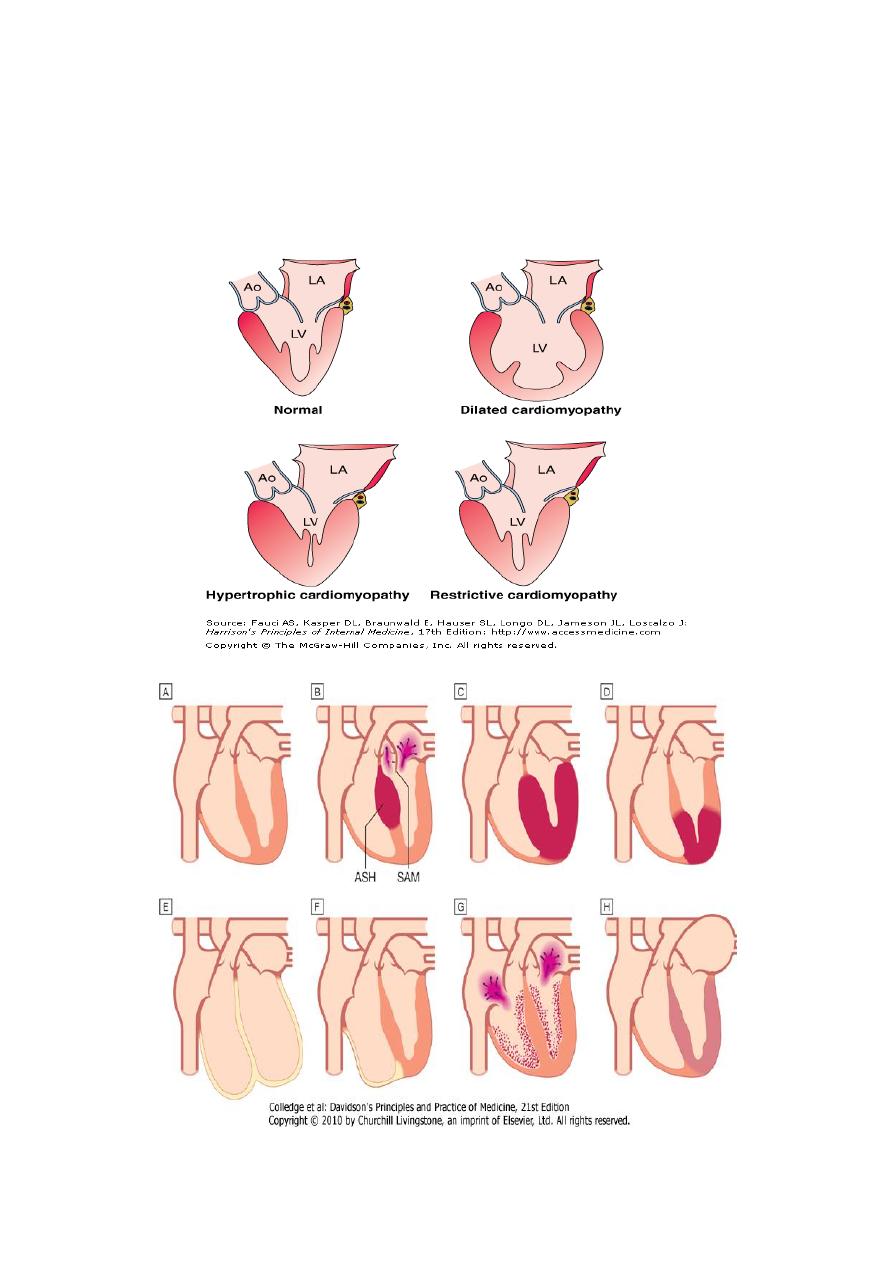
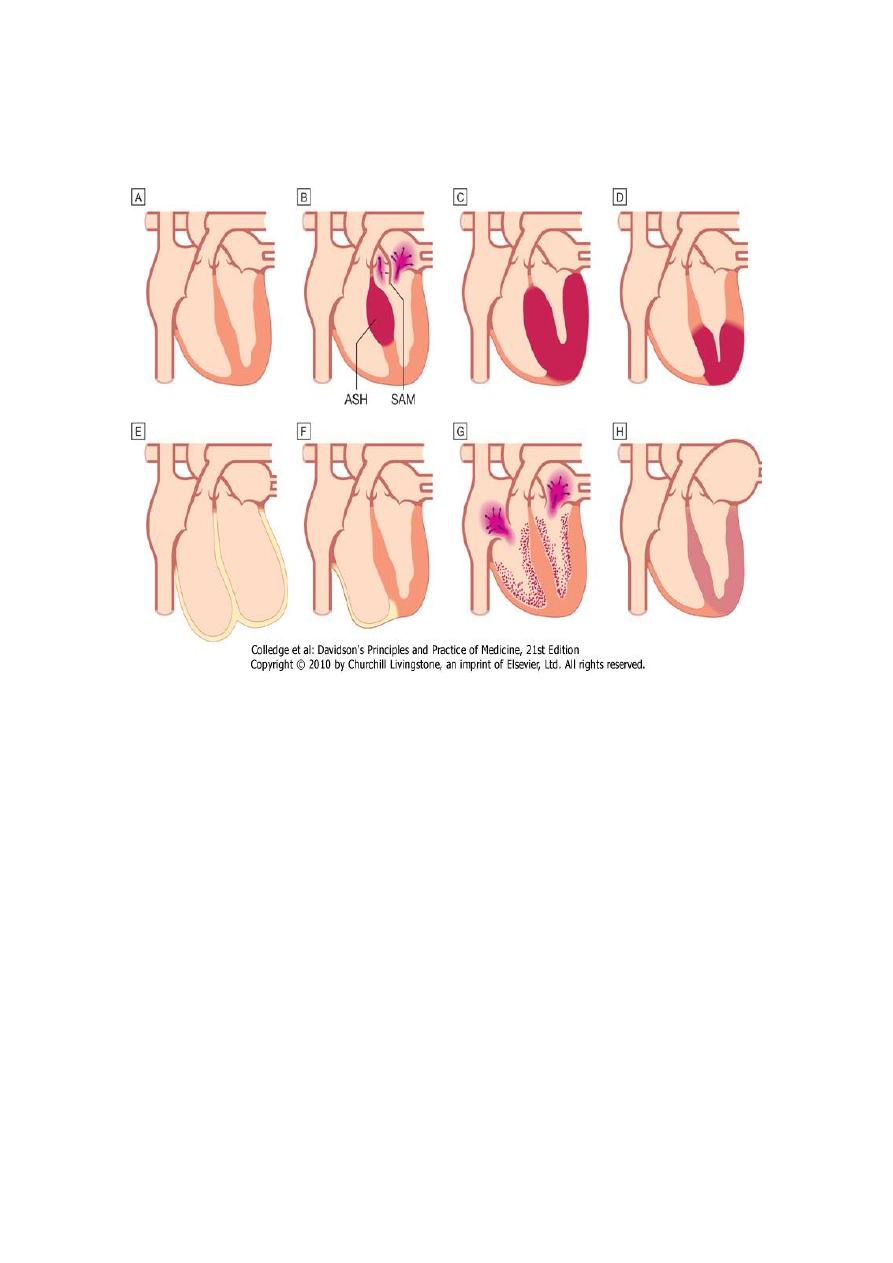
Clinical Classification:
1) Dilated: Left and/or right ventricular enlargement, impaired systolic function, congestive
heart failure, arrhythmias, emboli
2) Hypertrophic: Disproportionate left ventricular hypertrophy, typically involving septum more
than free wall, with or without an intraventricular systolic pressure gradient; usually of a
nondilated left ventricular cavity
3) Restrictive: Endomyocardial scarring or myocardial infiltration resulting in restriction to left
and/or right ventricular filling
Aetiology:
most intrinsic disorders of myocardium has not been elucidated functional
classification.
Morphologic types
1. Dilated
2. Hypertrophic
3. Restrictive
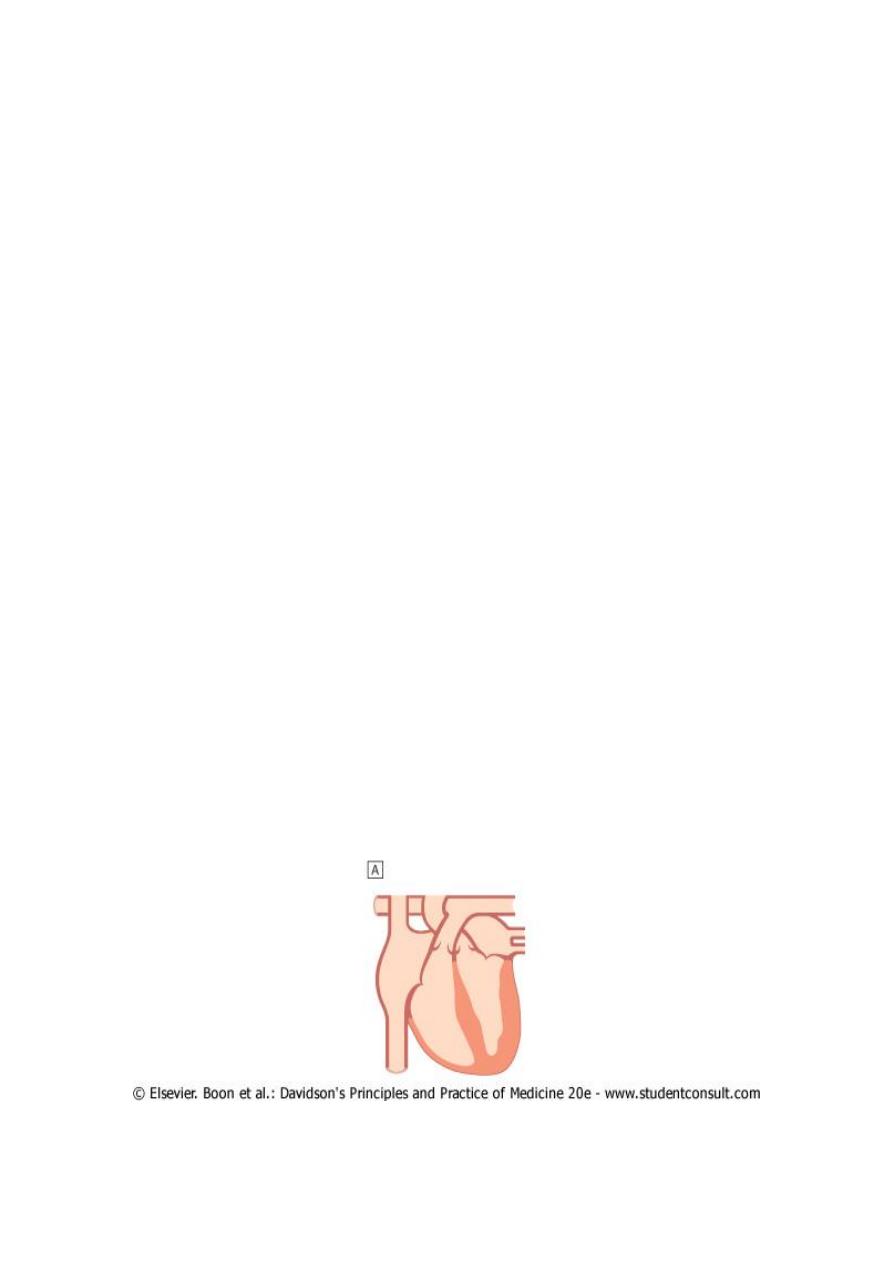
1- DILATED CARDIOMYOPATHY:
!
Characterised by
a. dilatation and impaired contraction of left (sometimes right) V
b. left ventricular mass is increased but wall thickness is normal or reduced).
c. histological changes = myofibrillary loss, interstitial fibrosis and T-cell infiltrates.
!
differential diagnosis = coronary artery disease and some specific disorders of heart muscle
, diagnosis of dilated cardiomyopathy =when these conditions have been excluded.
5
Pathogenesis-
1- Alcohol
2- Heridity: 25% of cases are inherited - autosomal dominant trait and a variety of single gene
mutations have been identified. mutations affect proteins in the cytoskeleton of the
myocyte
3- Autoimmune- late autoimmune reaction to viral myocarditis substantial subgroup of
patients with dilated cardiomyopathy; 10% of patients with advanced HIV infection
Clinical manifestations
a. Arrhythmia
b. Thromboembolism
c. Heart failure
d. Sudden death
e. sporadic chest pain
Incidence & Prevelance
u In North America and Europe, symptomatic dilated cardiomyopathy
incidence = 20 per 100 000
prevalence =38 per 100 000.
u Men are affected > twice as often as women.
u Most patients present with heart failure or
u found to have condition during routine investigation.
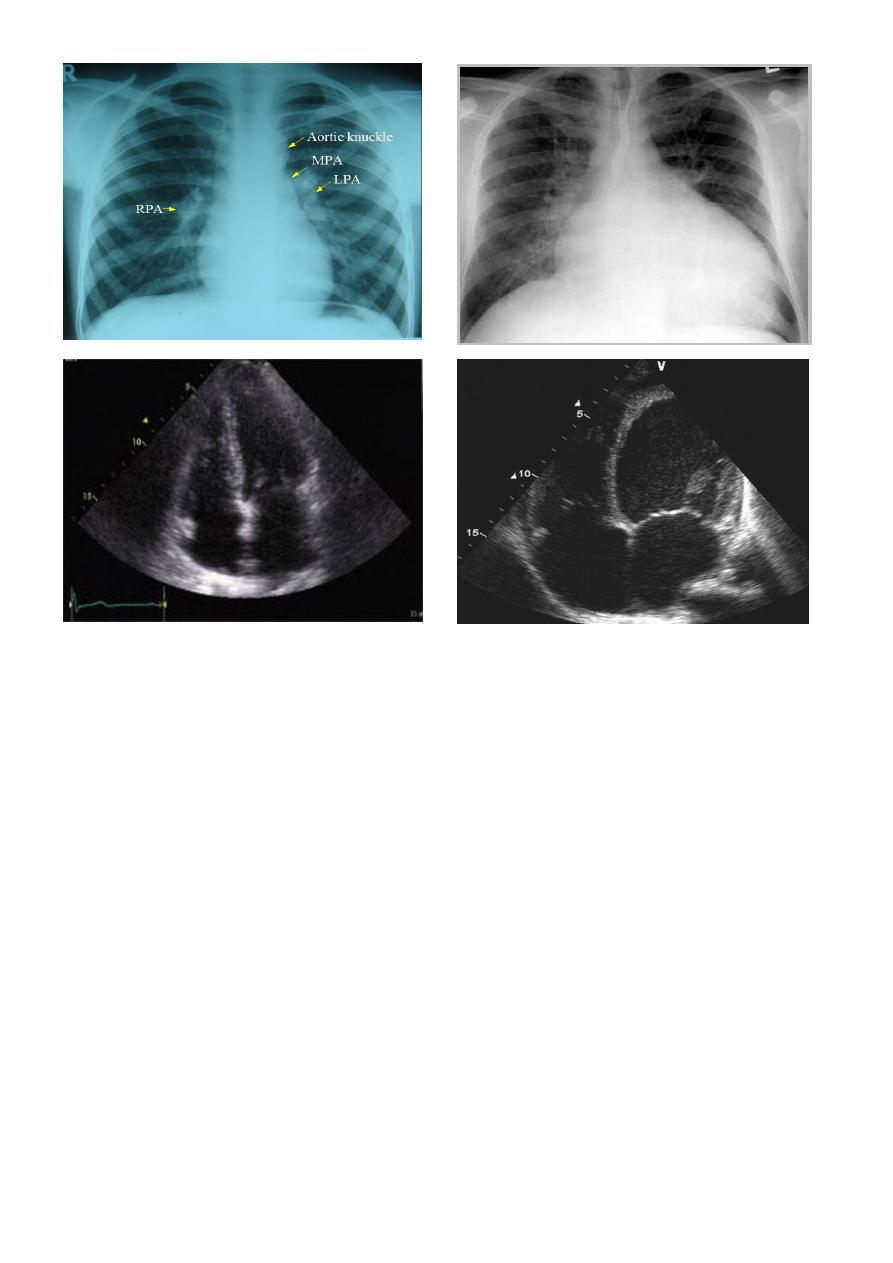
1. The ECG =non-specific changes
2. Chest X-ray=cardiomegaly
3. Echocardiography =establish diagnosis.
6
Treatment
controlling resulting heart failure.
prognosis = variable
cardiac transplantation may be indicated.
Patients with dilated cardiomyopathy and moderate or severe heart failure -- at risk of
sudden arrhythmic death.—
risk is substantially reduced by rigorous medical therapy
β-blockers and Angiotensin receptor antagonists.
Some patients may be considered for implantation of cardiac defibrillator and/or
cardiac resynchronisation therapy
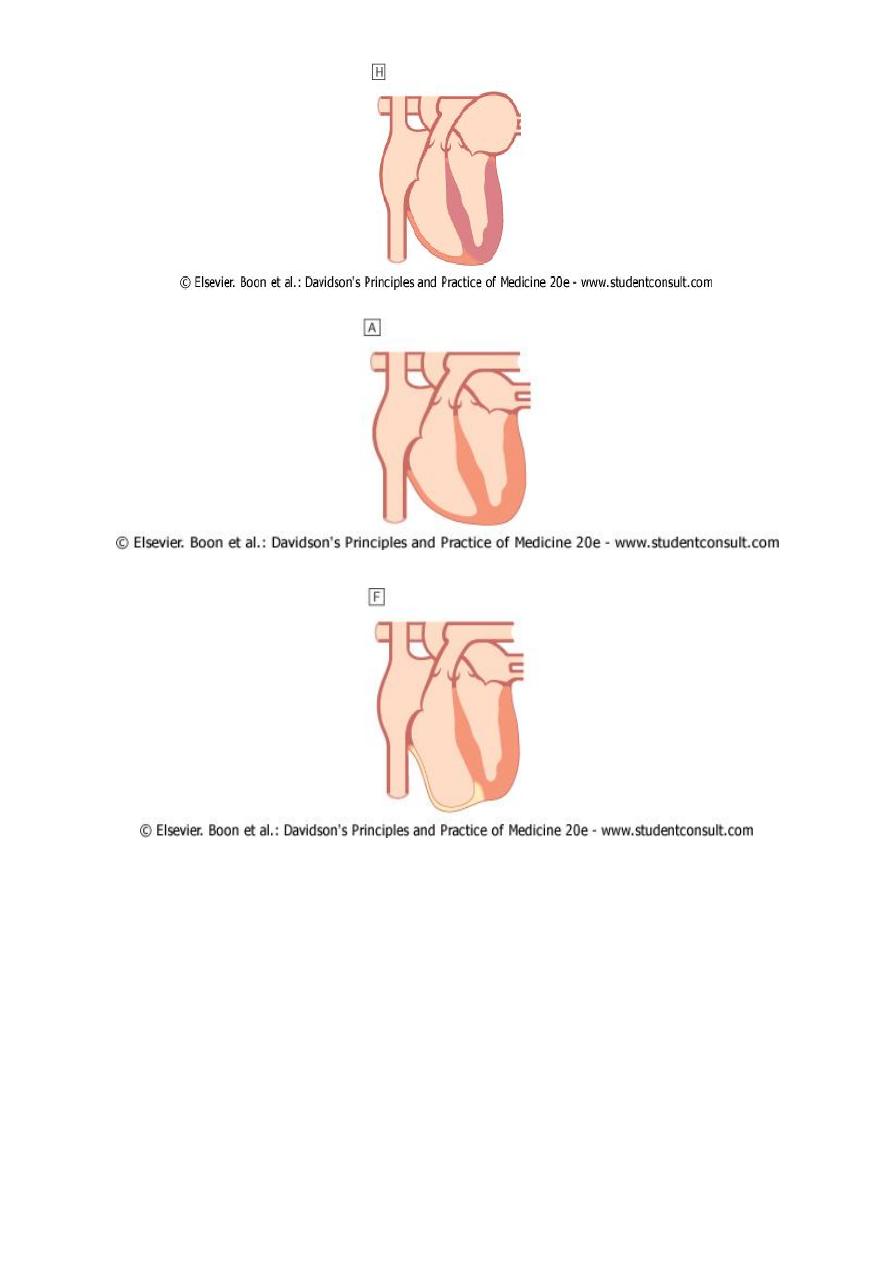
2- HYPERTROPHIC CARDIOMYOPATHY:
v
Most common form of cardiomyopathy
v
prevalence =approximately 100 per 100 000
v
Characterised by
1- inappropriate and elaborate left ventricular hypertrophy
2- malalignment of myocardial fibres.
7
v
Pattren of hypertrophy
a. Generalised (concentric) or
b. Confined (Focal) largely to interventricular septum (asymmetric septal hypertrophy,)
apical hypertrophic cardiomyopathy
Aetiology
1. genetic disorder autosomal dominant transmission, a high degree of penetrance and
variable expression. single point mutation in one of the genes that encode sarcomeric
contractile proteins.
2. Beta-myosin heavy chain mutations = elaborate ventricular hypertrophy.
3. Troponin mutations = little, and sometimes even no hypertrophy but marked myocardial
fibre disarray, an abnormal vascular response (e.g. exercise-induced hypotension) and a high
risk of sudden death.
4. Myosin-binding protein C mutations = hypertension and arrhythmia.
Pathophysiology
]
Stiff non-compliant ventricles impede diastolic filling Heart failure
]
Septal hypertrophy dynamic left ventricular outflow tract obstruction (hypertrophic
obstructive cardiomyopathy, or HOCM) and Abnormal systolic anterior motion - anterior MV
valve leaflet
]
Mitral regurgitation-
8
Clinical manifestations
Effort-related symptoms
a. angina
b. breathlessness
c. arrhythmia
d. sudden death
Symptoms and signs are similar to those of aortic stenosis, (except that in HCM , character of
the arterial pulse is jerky).
CLINICAL FEATURES OF HYPERTROPHIC CARDIOMYOPATHY:
W Symptoms
1. Angina on effort
2. Dyspnoea on effort
3. Syncope on effort
4. Sudden death
W Signs
1) Jerky pulse*
2) Palpable left ventricular hypertrophy
3) Double impulse at the apex (palpable fourth heart sound due to left atrial hypertrophy)
4) Mid-systolic murmur at the base*
5) Pansystolic murmur (due to mitral regurgitation) at apex
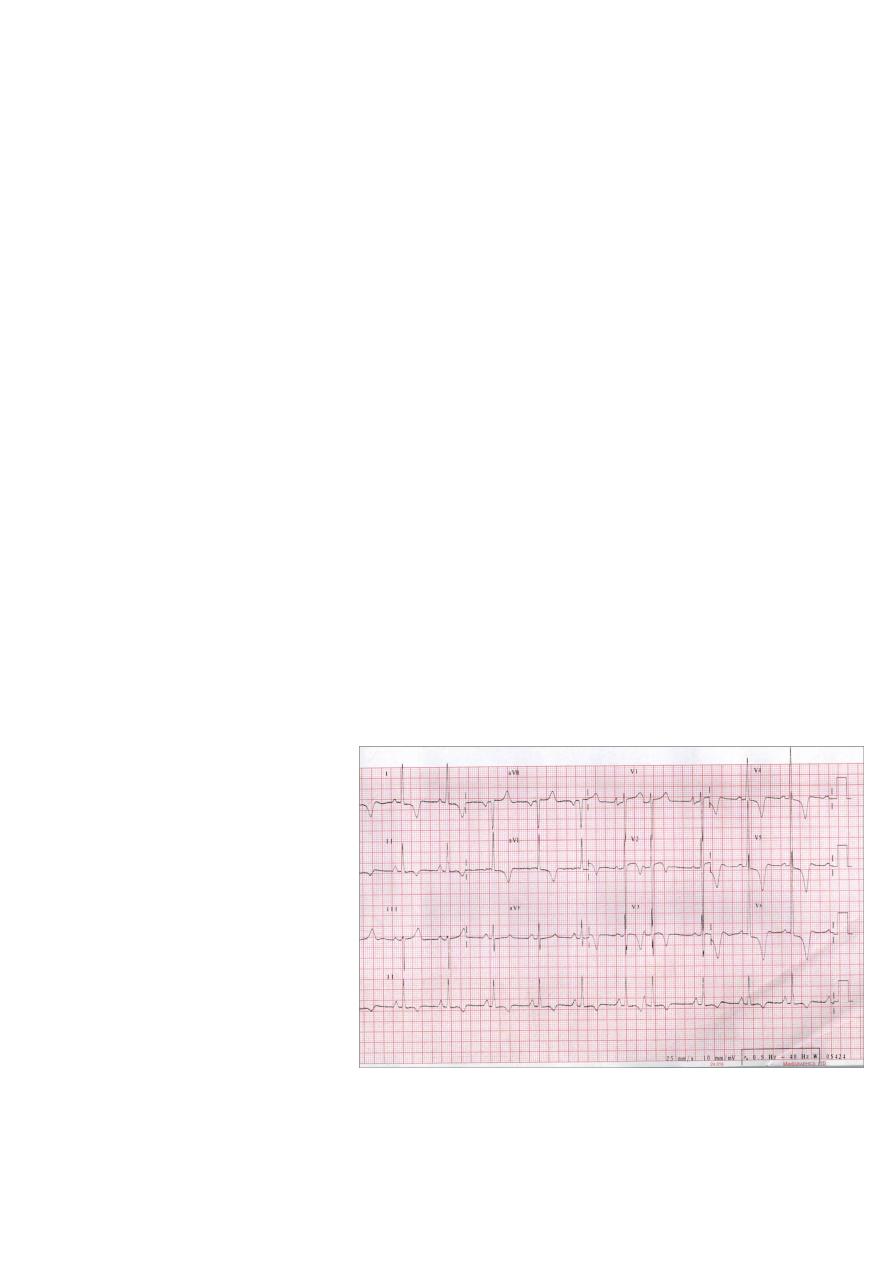
Investigations
1. ECG
features of left
ventricular hypertrophy with
a wide variety of often bizarre
abnormalities (e.g. pseudo-
infarct pattern, deep T-wave
inversion).
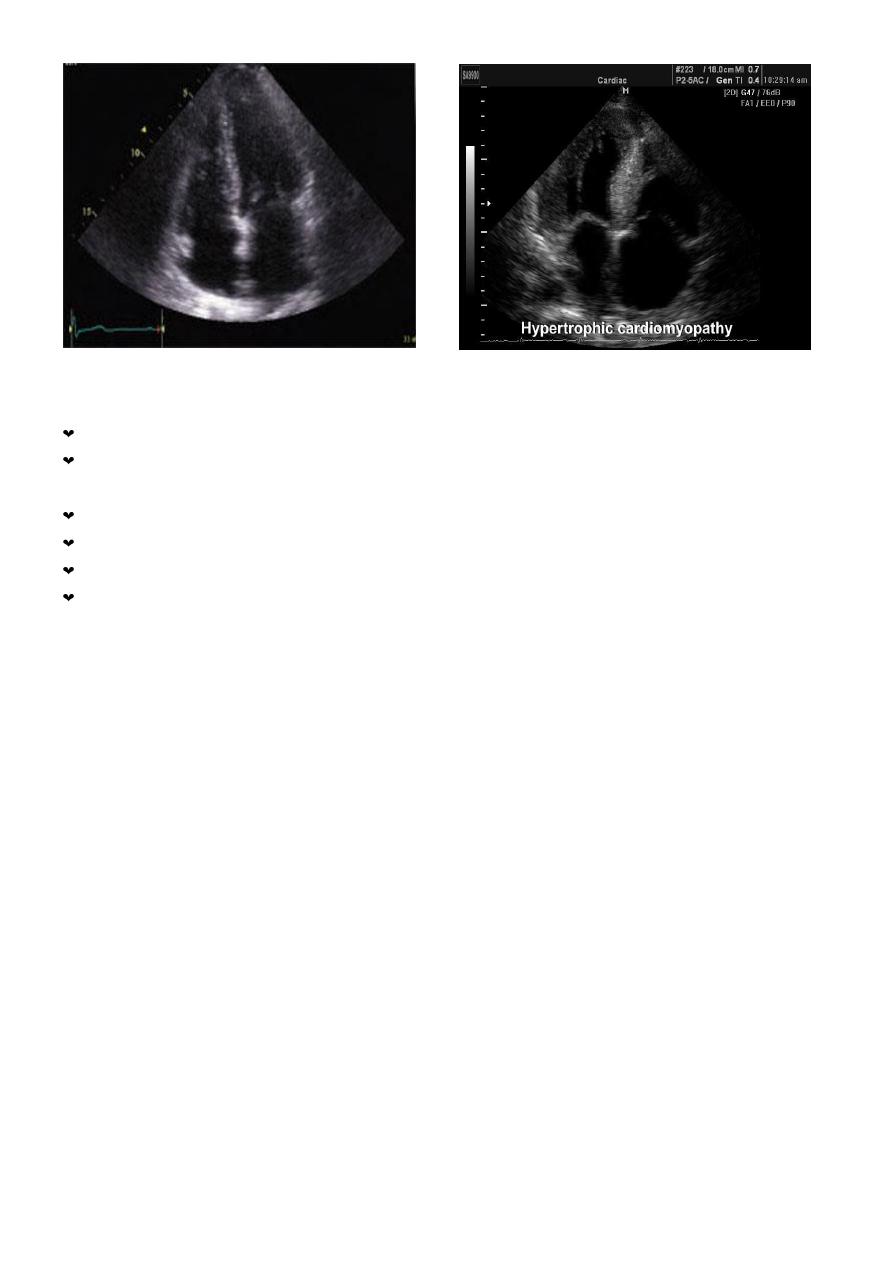
2. Echocardiography
diagnostic;
diagnosis = difficult when
another cause of left ventricular
hypertrophy is present (e.g.
physical training-athletes'
heart, hypertension) but the degree of hypertrophy is greater than expected.
3. Genetic testing may facilitate diagnosis in the future.
9
Outcome
natural history = variable but clinical deterioration is often slow.
annual mortality from sudden death = 2-3% among adults , 4-6% in children and
adolescents.
Sudden death
typically occurs during or just after vigorous physical activity
hypertrophic cardiomyopathy = most common cause of sudden death in young athletes.
Ventricular arrhythmias = thought to be responsible for many of these deaths.
RISK FACTORS FOR SUDDEN DEATH IN HYPERTROPHIC CARDIOMYOPATHY:
1) A history of previous cardiac arrest or sustained ventricular tachycardia
2) Recurrent syncope
3) An adverse genotype and/or family history
4) Exercise-induced hypotension
5) Multiple episodes of non-sustained ventricular tachycardia on ambulatory ECG monitoring
6) Marked increase in left ventricular wall thickness
Treatment of hypertrophic CMP:
g Beta-blockers + rate-limiting calcium antagonists (e.g. verapamil) =
g relieve angina
g prevent syncopal attacks;
g No pharmacological treatment -definitely known to improve prognosis.
g Arrhythmias = common and often respond to amiodarone.
g Outflow tract obstruction = improved
- by partial surgical resection (myectomy) or
- by iatrogenic infarction of basal septum (septal ablation) using a catheter-delivered
alcohol solution.
10
g Implantable cardiac defibrillator (ICD) = in patients with clinical risk factors for sudden
death).
g Avoid Digoxin and vasodilators = increase outflow tract obstruction
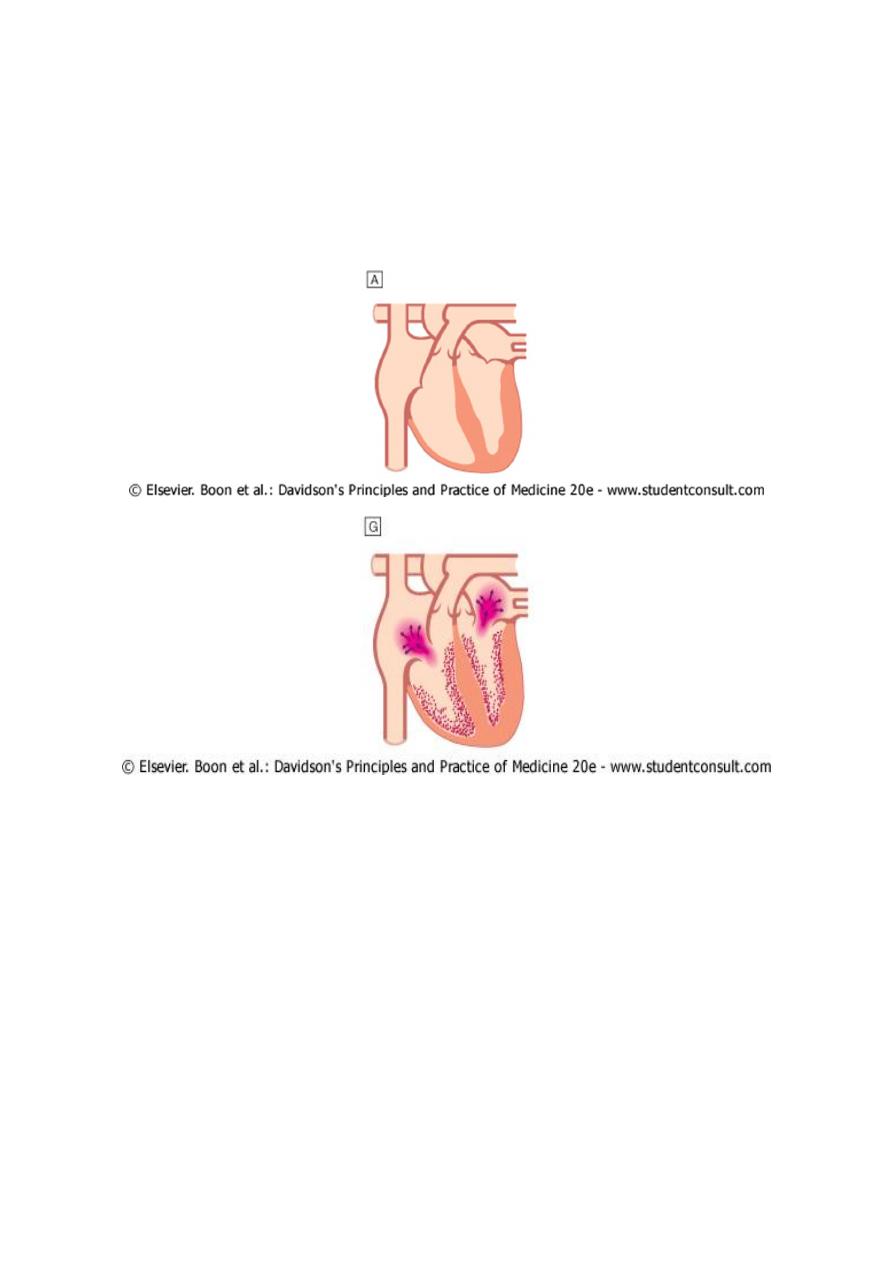
3- RESTRICTIVE CARDIOMYOPATHY
* rare condition
* ventricular filling is impaired because the ventricles are 'stiff'.
* high atrial pressures with atrial hypertrophy, dilatation atrial fibrillation.
* Amyloidosis =most common cause of restrictive cardiomyopathy in UK
* other forms of infiltration (e.g. glycogen storage diseases), idiopathic perimyocyte fibrosis
and a familial form of restrictive cardiomyopathy can present with this form of heart disease.
* Diagnosis can be very difficult and may require complex
* Doppler echocardiography, CT or MRI, and endomyocardial biopsy.
* Treatment is symptomatic but the prognosis is usually poor and transplantation may be
indicated.
4- ARRHYTHMOGENIC RIGHT VENTRICULAR DYSPLASIA
Patches of the right ventricular myocardium are replaced with =fibrous and fatty tissue).
inherited as an autosomal dominant trait.
prevalence in the UK - approximately 10 per 100 000.
clinical problems
- ventricular arrhythmias,
- sudden death
- right-sided cardiac failure.
ECG = slghtly braodened QRS and inverted T waves in Rprecordial leads.
MRI =useful diagnostic tool -used to screen the first-degree relatives of affected individuals.
Patients at high risk of sudden death can be offered an ICD.
11
5- OBLITERATIVE CARDIOMYOPATHY:
Endocardium of one or both ventricles
characterised by thrombosis and elaborate fibrosis with gradual obliteration of the
ventricular cavities (e.g. endomyocardial fibroelastosis,)
Regurgition of mitral and tricuspid valves.
Clinicsl features
1. Heart failure
2. pulmonary and systemic embolism.
3. sometimes be associated with eosinophilia (e.g. eosinophilic leukaemia, Churg-Strauss
syndrome,).
12
In tropical countries= responsible for up to 10% of cardiac deaths. Mortality is high (50% at 2
years).
Treatment
- Anticoagulation and antiplatelet
- diuretics may help symptoms of heart failure.
- Surgery (tricuspid and/or mitral valve replacement with decortication of the
endocardium)
SPECIFIC DISEASES OF HEART MUSCLE:
C Infections
- Viral, e.g. Coxsackie A and B, influenza, HIV
- Bacterial, e.g. diphtheria, Borrelia burgdorferi
- Protozoal, e.g. trypanosomiasis
C Endocrine and metabolic disorders e.g. Diabetes, hypo- and hyperthyroidism, acromegaly,
carcinoid syndrome, phaeochromocytoma, inherited storage diseases
C Connective tissue diseases e.g. Systemic sclerosis, systemic lupus erythematosus (SLE),
polyarteritis nodosa
C Infiltrative disorders e.g. Haemochromatosis, haemosiderosis, sarcoidosis, amyloidosis
C Toxin e.g. Doxorubicin, alcohol, cocaine, irradiation
C Neuromuscular disorders e.g. Dystrophia myotonica, Friedreich's ataxia .
