ARRHYTHMIAS
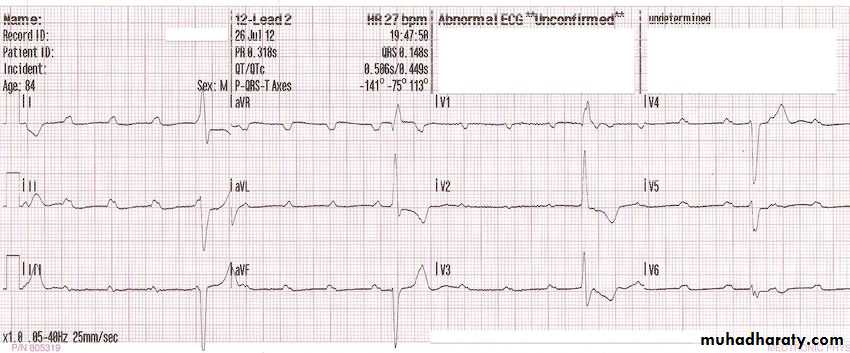
VENTRICULAR ARRHYTHMIASBRADYARRHYTHMIAS
MANAGEMENT
-
.
Clinical
Possibilty
V.Rate
SiteECG
Treatmen
Preventio
Irregular
ectopics
• atria
Normal QRS
• ventricleWide QRS
BBA.fib
SlowFast
Both atria
P absent
N. QRS
Acute
Chronic
Drugs+
AC
Regular
Sinus tachy
<150
SA node
P present
QRS N.
Underlying dis.+BB
Supraven
>150-220
Atria
P absent
N.QRS
CSM.DC
BB.CCB.
RF ablation
AV node
P absentN.QRS
CSM.DC
BB.CCB.
RF ablation
AV junctio
AccessaryP absent
?? QRS
CSM.DC
BB.CCB.?
RF ablation
A.Flutter
120-320
RT.Atrium
P absent
F wave
CSM.DC.
BB.CCB.D
RF ablation
V.tachy
>120Ventricle
P absent
Wide QRS
IV drugs
DC
VENTRICULAR TACHYARRHYTHMIAS
V.ECTOPICSV.TACHYCARDIA
V.FLUTTER
V.FIBRILLATION
IDIOVENTRICULAR RHYTHM
Types of Ventricular Arrhythmias
single beat =premature ventricular beat .Two consecutive beats =ventricular couplets.
Three or more consecutive beats =triplet
rate faster than 100 BPM= VT
slower rates<100 BPN =idioventricular rhythms.
Nonsustained VT= terminates spontaneously within 30 sec.
sustained VT =persists longer than 30 seconds.
monomorphic VT caused by repetitive activation from same source, QRS complexes the same from beat to beat.
polymorphic VT=continually changing activation sequence = changing QRS morphology.
VF = continuous irregular activation with no discrete QRS complexes
Arrhythmias =from right ventricle or septum =prominent S wave in V1=LBBB Like configuration.
Arrhythmias =from free wall of LV=prominent positive deflection in V1= RBBB-Like morphology
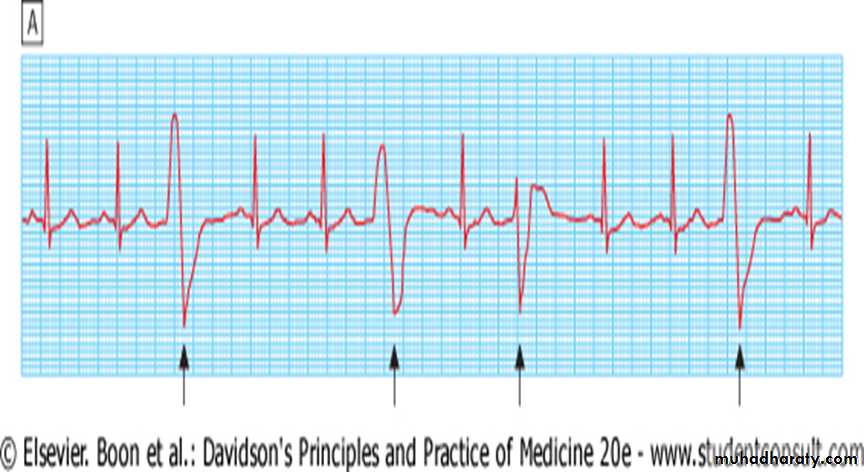
VENTRICULAR ECTOPIC BEATS(EXTRASYSTOLES PREMATURE BEAT
QRS complexes of VE beats - abnormal morphology ( bundle branches activated one after other, not simultaneously).ECG = premature broad, bizarre QRS complexes
unifocal (identical beats arising from a single ectopic focus) or
multifocal (varying morphology with multiple foci- 'Couplet' and 'triplet' = two or three successive ectopic beats,run of alternate sinus and ectopic beats = ventricular 'bigeminy'.
SYMPTOMS AND SIGNS
Ectopic beats low stroke volume (LV contraction occurs before filling is complete).pulse = irregular, with weak or missed beats .
Asymptomatic usually
Symptomatic=
irregular heart beat,
missed beats or
abnormally strong beats (increased output of post-ectopic sinus beat).
significance of VEBs= depends on
presence or absence of underlying heart disease
TREATMENT1-IN HEALTHY HEART & 2-IN DISEASED HEART1-Ventricular ectopic beats healthy subjects
frequently found in healthy people
prevalence increases with age.
more prominent at rest
disappear with exercise.
Treatment = not necessary
highly symptomatic= β-blockers.
2- subclinical heart disease esp. coronary artery disease.
no evidence that anti-arrhythmic therapy improves prognosis
discovery of frequent VEBs =general cardiac investigations.
2-V. Ectopic beats associated with heart disease
1-acute myocardial infarction = need no treatment. Persistent frequent (> 10 per hour) in acute phase of MI= poor long-term outcome.β-blockers
anti-arrhythmic drugs do not improve and may even worsen prognosis
2- heart failure = adverse prognosis,
outlook –same-suppressed with anti-arrhythmic drugs.Effective treatment of HF= suppress ectopic beats.
3-digoxin toxicity
mitral valve prolapse,'escape beats' in the presence of an underlying bradycardia. Treatment = directed at the underlying condition.
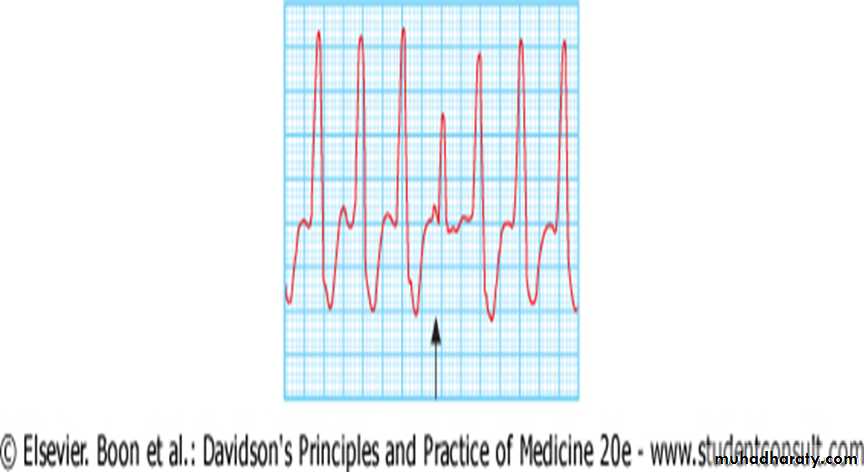
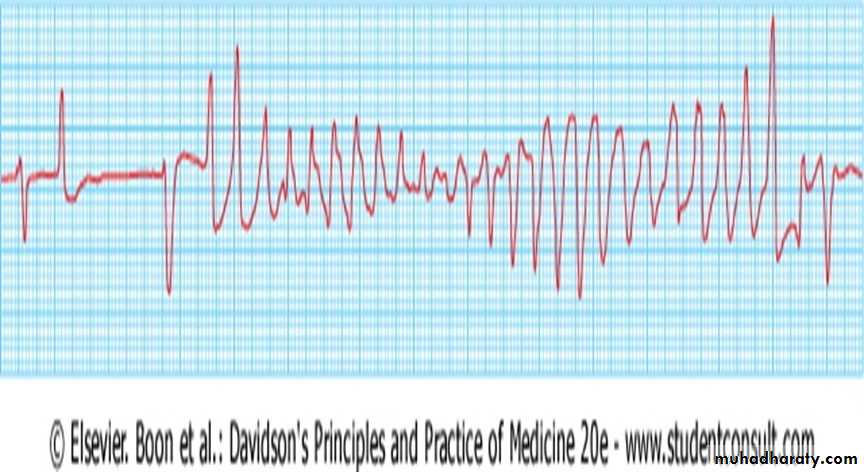
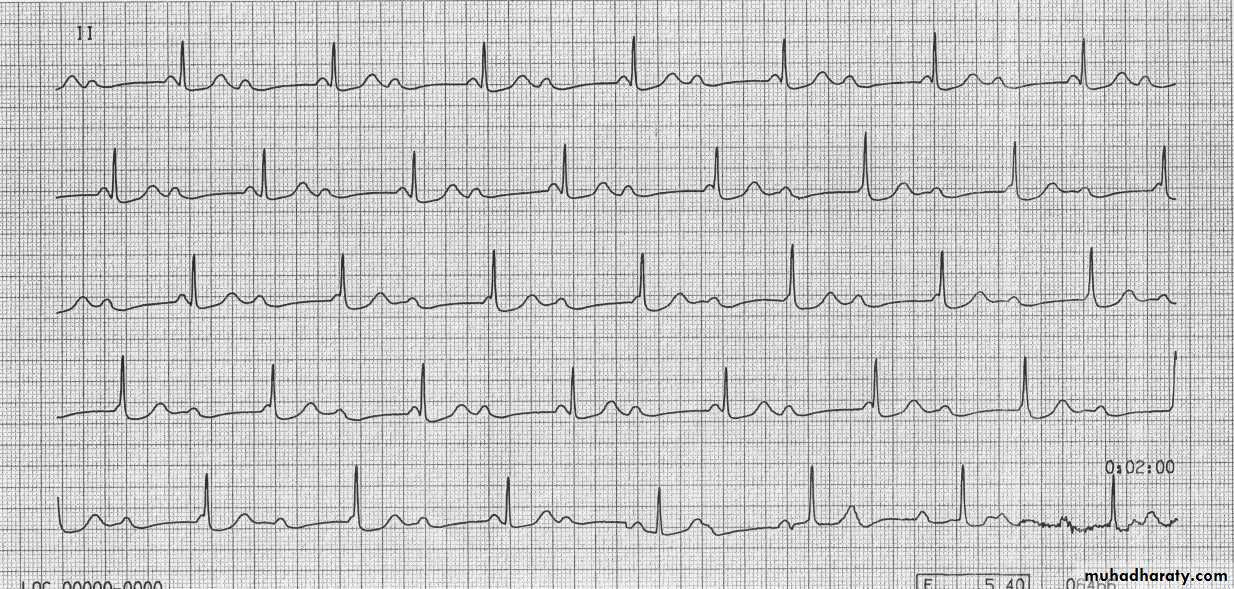
VENTRICULAR TACHYCARDIA (VT)
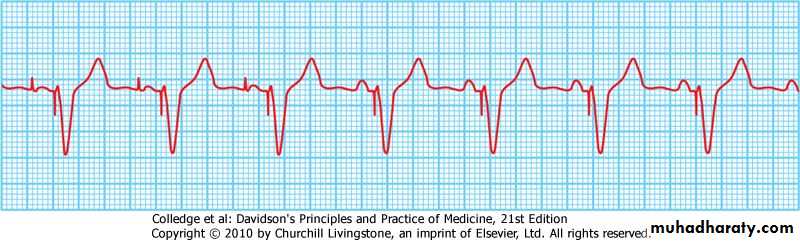
ECG=tachycardia with broad, abnormal QRS complexes
rate above 120/min
TYPES
1-NON-SUSTAINED <30 SEC.
2-SUSTAINED> 30 SEC.-stable
-unstable
(extra-systolic *idioventricular)
-
CAUSES=
coronary heart disease or
cardiomyopathies.
OUTCOME=
haemodynamic compromise ordegenerate into ventricular fibrillation .
MECHANISM=
ischaemic tissue abnormal automaticity or
triggered activity in
diseased ventricular tissue- re-entry within
SYMPTOMS=
palpitation or
symptoms of low cardiac output,
dizziness,
dyspnoea or
syncope.
TYPES OF VT
1-After Acute MI,CMP,IHD(+/-V aneurysm/LV dysfunction)
VT lasting > few beats
require treatment- emergency.2-Normal heart VT= healthy hearts ('normal heart VT'),
abnormal automaticity in RV outflow tract or one of fascicles of LBBprognosis - good
catheter ablation can be curative.
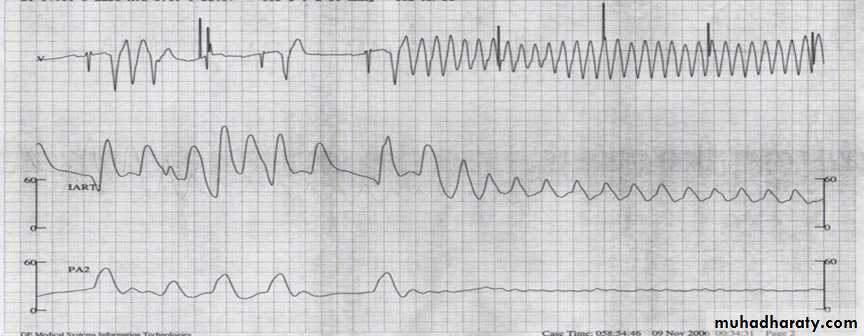
2-Idioventricular rhythm-Slow VT
Patients recovering from myocardial infarction =periods of idioventricular rhythm ('slow' VT) = rate =above preceding sinus rate and <120/min.reflect reperfusion of the infarct territory
may be a good sign.
usually self-limiting and asymptomatic
do not require treatment.
-
Management
Prompt action to restore sinus rhythm + prophylactic therapy.
1-Systolic BP <90 mmHg =
DC cardioversion
2-Well tolerated
IV amiodarone -- bolus IV infusion
IV lidocaine (depress LV function hypotension or acute HF.
Hypokalaemia, hypomagnesaemia, acidosis and hypoxaemia = aggravate situation = corrected.
PROPHYLAXIS
Beta-blockers -effective at suppressing VT.
Amiodarone -added if additional control is needed.
Class I anti-arrhythmic drugs = used acutely = dangerous in long term in patients with IHD.
implantable cardiac defibrillator== high risk of arrhythmic death (e.g with poor LV function, or VT is associated with haemodynamic compromise)=>
surgery or catheter ablation = Rarely= interrupt arrhythmia focus or circuit.
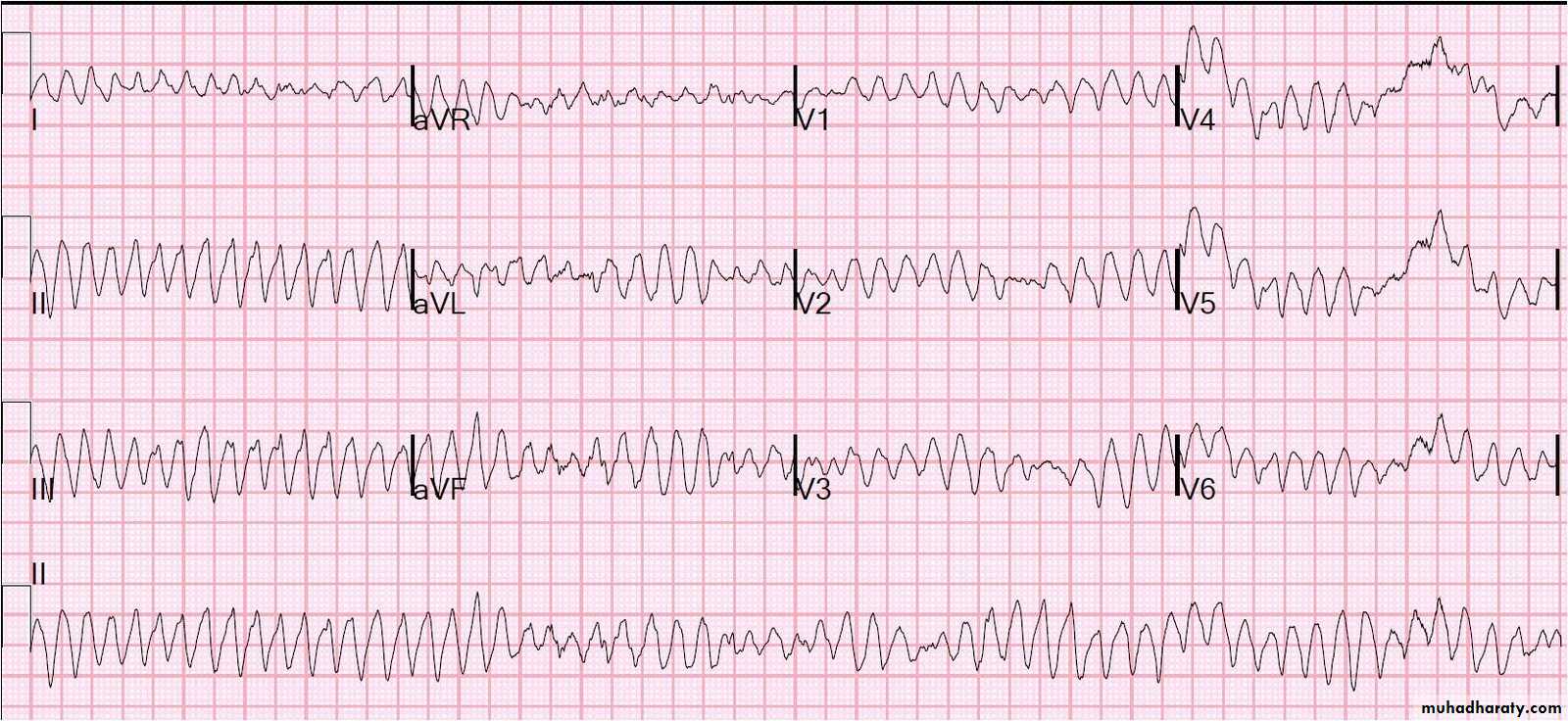
VT VERSUS SVT WITH BLOCK
VT -difficult to distinguish from SVTwith bundle branch block or pre-excitation (Wolff-Parkinson-White syndrome).
When there is doubt =safer to manage as VT=(most common cause of broad-complex tachycardia.)
common causes of ventricular tachycardia
1- acute myocardial infarction,
2-cardiomyopathy and
3- chronic ischaemic heart disease, particularly when it is associated with a ventricular aneurysm or poor left ventricular function
FEATURES IN FAVOUR OF VT IN BROAD-COMPLEX TACHYCARDIA
history of myocardial infarctionAV dissociation (pathognomonic)
Capture/fusion beats (pathognomonic,
Extreme left axis deviation
Very broad QRS complexes (> 140 ms)
No response to carotid sinus massage or i.v. adenos
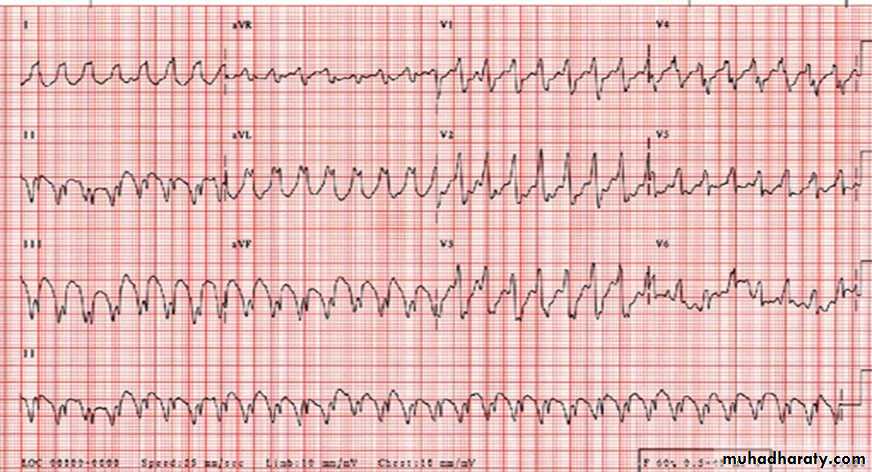
TORSADES DE POINTES (TWISTING POINTS)
form of polymorphic VT- complication of prolonged ventricular repolarisation (prolonged QT interval).ECG =rapid irregular complexes that oscillate from an upright to an inverted position +to twist around baseline as mean QRS axis changes
usually non-sustained and repetitive - may degenerate into VF
During sinus rhythm,ECG =prolonged QT interval.
more common in women
triggered by a combination of aetiological factors (e.g. multiple medications and hypokalaemia).
congenital long QT syndromes = genetic disorders -characterised by mutations in genes that code for cardiac sodium or potassium channels.
1-IV magnesium (8 mmol over 15 minutes, then 72 mmol over 24 hours)
2- Atrial pacing -suppress the arrhythmia through rate-dependent shortening of the QT interval.
IV isoprenaline -alternative to pacing -avoided congenital long QT
CAUSES OF LONG QT INTERVAL AND TORSADES DE POINTES
BradycardiaBradycardia compounds other factors that cause torsades de pointes
Electrolyte disturbance
Hypokalaemia/ Hypomagnesaemia /Hypocalcaemia
Drugs
Disopyramide (and other class la anti-arrhythmic drugs,
Sotalol, amiodarone (and other class III anti-arrhythmic drugs)
Amitriptyline (and other tricyclic antidepressants)
Chlorpromazine (and other phenothiazines)
Erythromycin (and other macrolides) … and many more
Congenital syndromes
Romano-Ward syndrome (autosomal dominant)
Jervell and Lange-Nielson syndrome (autosomal recessive, associated with congenital deafness)
Long-term therapy may not be necessary
Beta-blockers or left stellate ganglion block =congenital long QT syndrome.
implantable cardiac defibrillator -advisable.
Brugada syndrome =
related genetic disorder -present with polymorphic VT or sudden death
defect in sodium channel function,
abnormal ECG =RBBB+ ST elevation in V1 and V2, but no prolongation of QT in).
VENTRICULAR FIBRILLATION
Disorganised choatic rhythm inefffective ventricular contractions = rapid haemo-dynamic collapse and death
ECG=coarse undulation,without identifiable QRS,ST OR T
Treatment –
nonsynch.DC.360 jouls.followed by iv amiodrone or xyllocaine
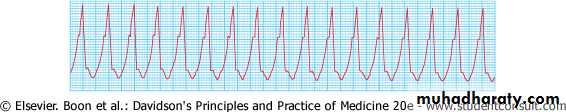
VENTRICULAR FLUTTER
form of monomorphic VToccurring at rate of 280-300 b/m
hemodynamically unstable rhythm
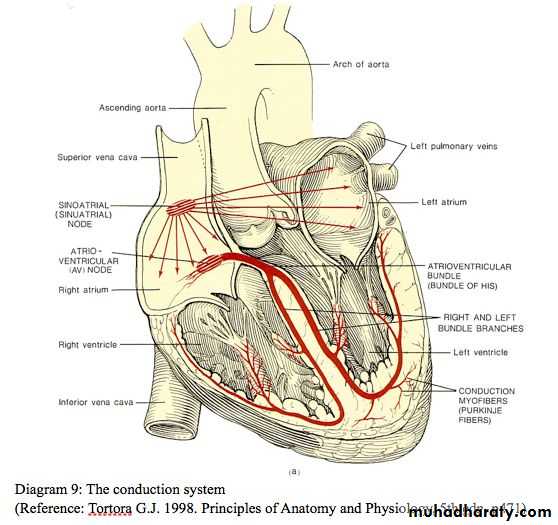
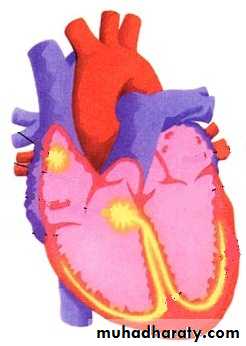
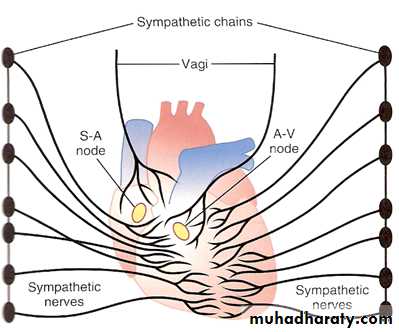
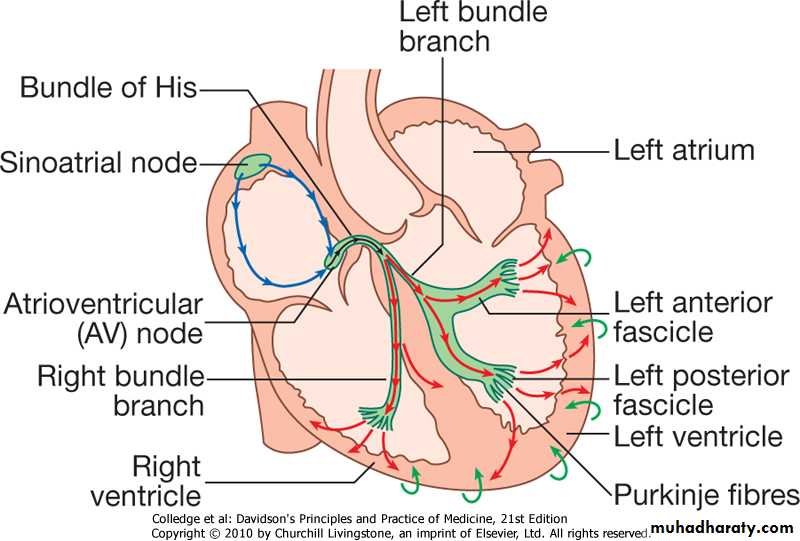
BRADY-ARRHYTHMIA
Impulse generation Sino-Atrial dis.Impulse formation Atrio-Ventricular block
1-SINOATRIAL DISEASE
2-ATRIOVENTRICULAR3-BUNDLE BRANCH BLOCK
SAN
AVN
Impulse conduction
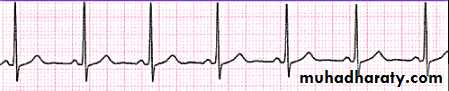
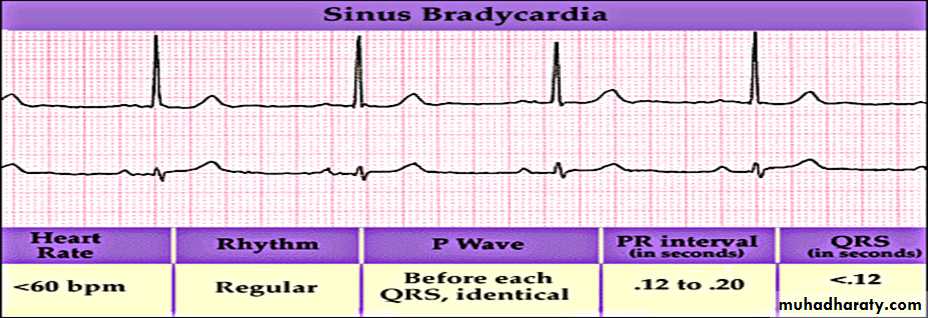
Impulses originate regularly at a frequency of 60-100 beat/ minSINUS BRADYCARDIA
sinus rate of <60/minPhysiological causes
healthy people at rest *common finding in athletes.
Pathological causes
Myocardial infarction *Sinus node disease (sick sinus syndrome)
Hypothermia *Hypothyroidism *Cholestatic jaundice
Raised intracranial pressure *Drugs, e.g. β-blocker, digoxin, verapamil
Treatment
Asymptomatic =no treatment.
Symptomatic =usually responds to i.v. atropine 0.6-1.2 mg.
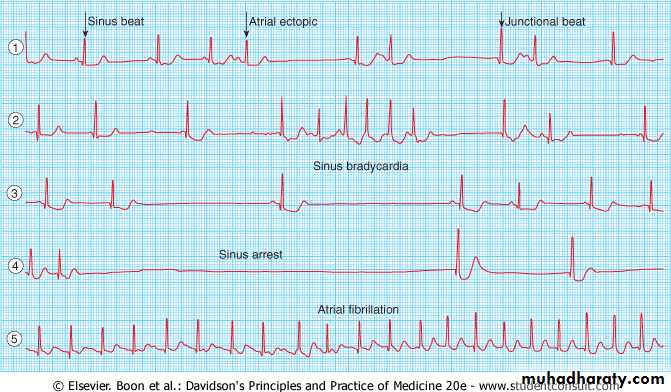
SINOATRIAL DISEASE (SICK SINUS SYNDROME(
Sino-atrial nodesSlows bradycardia
Stops for a whilesinus arrest
Stops and other atrial areas dominate
atrial arrhythmiasSVT &AF
Stopsatrio-ventricular block
COMMON FEATURES OF SINOATRIAL DISEASE
Sinus bradycardia
Sinoatrial block (sinus arrest)
Paroxysmal supraventricular tachycardia
Paroxysmal atrial fibrillation
Atrioventricular block
Sinoatrial disease
Age-any age- most common in elderly.
Underlying pathology
fibrosis, degenerative changes and/or ischaemia of SA (sinus) node.
Characterised by
variety of arrhythmias
Present with
palpitation, dizzy spells or syncope(intermittent tachycardia, bradycardia, or pauses with no atrial or ventricular activity (sinoatrial block or sinus arrest) .
Treatment
permanent pacemaker
spontaneous bradycardias, or
symptomatic bradycardias (drugs)
Atrial pacing --prevent episodes of atrial fibrillation.
Permanent pacing.
-
ATRIOVENTRICULAR AND BUNDLE BRANCH BLOCK
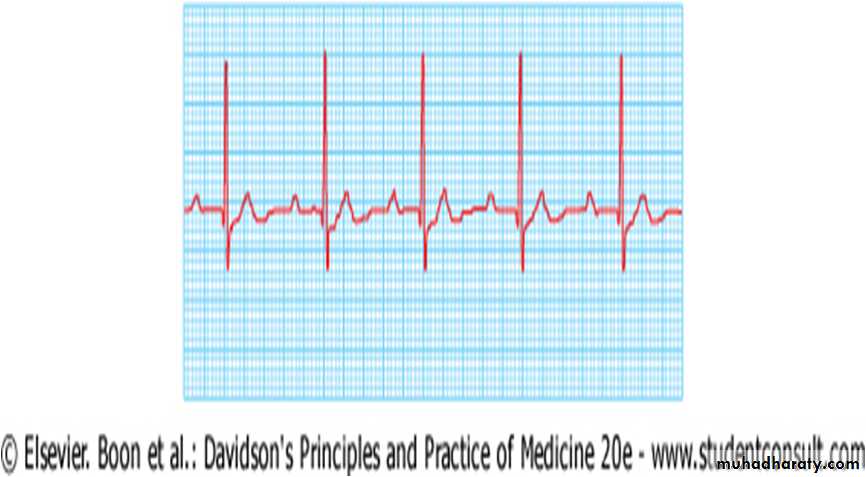
ATRIOVENTRICULAR BLOCK =1st.degree=2nd.degree
type 1
type 2
=3rd.degree
BUNDLE BRANCH BLOCK = RIGHT BBB
LEFT BBB
complete
incomplete-fascicular
ATRIOVENTRICULAR (AV) BLOCK
Atrioventricular conduction -- influenced by autonomic activity.AV block intermittent -- only evident when conducting tissue is stressed by rapid atrial rate
atrial tachyarrhythmias are often associated with AV block ,
First-degree AV block = AV conduction is delayed
PR interval is prolonged (> 0.20 seconds) .
rarely causes symptoms.
Second-degree AV block some impulses from the atria fail to conduct to the ventricles dropped beats
-
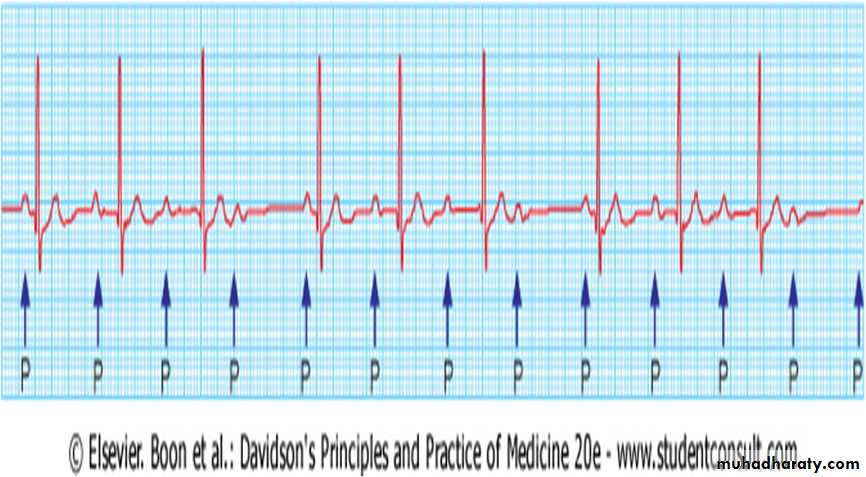
Second-degree AV block some impulses from atria fail to conduct to the ventricles dropped beats
1-Mobitz type I = progressive lengthening of successive PR intervals dropped beat.
cycle then repeats itself= Wenckebach's phenomenon - impaired conduction in AV node itself.
- physiological
-at rest or during sleep in athletic young adults with high vagal tone.
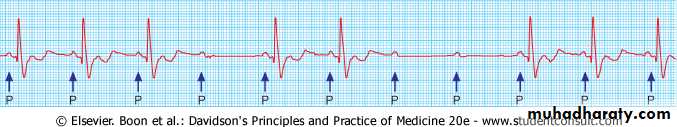
2-Mobitz type II-- PR interval of conducted impulses remains constant but some P waves are not conducted.
usually caused by disease of the His-Purkinje system and carries a risk of asystole.
In 2:1 AV block (,alternate P waves are conducted so it is impossible to distinguish between Mobitz type I and type II block
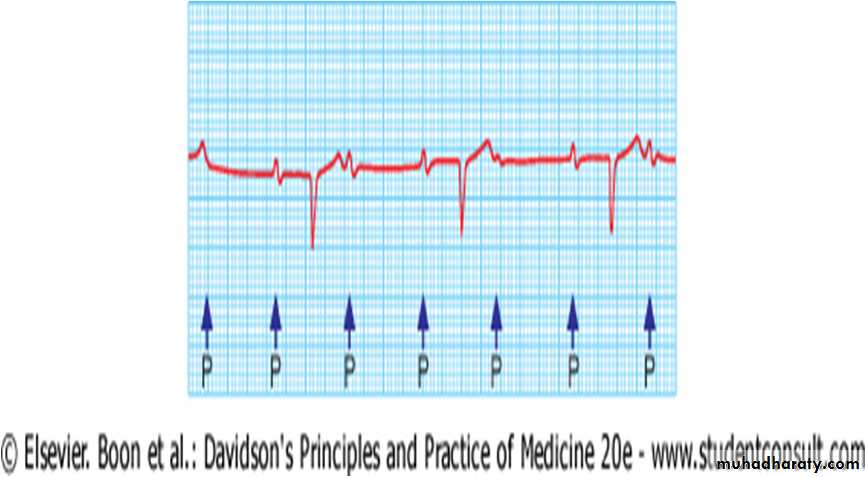
Third-degree (complete) AV block
- AV conduction fails completely,- the atria and ventricles beat independently (AV dissociation,
-Ventricular activity is maintained by
1- escape rhythm arising in tAV node or bundle of His (narrow QRS complexes) or
2- distal Purkinje tissues (broad QRS complexes). Distal escape rhythms tend to be slower and less reliable.
AETIOLOGY OF COMPLETE HEART BLOCK
CongenitalAcquired
Idiopathic fibrosis
Myocardial infarction/ischaemia
Inflammation
Acute (e.g. aortic root abscess in infective endocarditis)
Chronic (e.g. sarcoidosis, Chagas disease,
Trauma (e.g. cardiac surgery)
Drugs (e.g. digoxin, β-blocker
Clinical Features of CHB
PULSE-slow (25-50/min)pulse
regular pulse
does not vary with exercise.(except congenital complete HB )
usually a compensatory increase in stroke volume with a large volume pulse and systolic flow murmurs.
JVP=Cannon waves may be visible in neck
HS=t intensity of 1st.HS (loss of AV synchrony).
Stokes-Adams attacks –episode of asystole =syncope
Stokes-Adams attacks
Episodes of ventricular asystoleCAUSES 1-CHB or Mobitz type II 2nd. AV block
2-sinoatrial disease .
PRESENTATION= recurrent syncope or 'Stokes-Adams' attacks.
typical episode =
characterised by sudden loss of consciousness,
frequently occurs without warning and
may result in a fall.
Convulsions (cerebral ischaemia) can occur if --prolonged asystole.
pallor and a death-like appearance during the attack, but when the heart starts beating again there is a characteristic flush.
In contrast to epilepsy, recovery is rapid.
DD.
carotid sinus syndrome
vasovagal syndrome
Management of AV block-ACUTE
Management AV block complicating acute MI
Acute inferior MI is often complicated by transient AV block (R CA supplies the AV junction)= reliable escape rhythm,
patient remains well no treatment
Symptomatic 2nd. or CHB= may respond to atropine (0.6 mg i.v., repeated as necessary) or temporary pacemaker.
most cases the AV block will resolve within 7-10 days.
2nd. Or CHB complicating acute anterior MI
sign of extensive ventricular damage involving both bundle branches
carries a poor prognosis.//Asystole may ensue
temporary pacemaker - inserted as soon as possible.
Asystole i.v. atropine (3 mg) or i.v. isoprenaline (2 mg in 500 ml 5% dextrose, infused at 10-60 ml/hour) may help to maintain the circulation until a temporary pacing electrode can be inserted.
Transcutaneous pacing - effective temporary rhythm support.
Chronic AV block
Symptomaticbradyarrhythmias associated with AV block permanent pacemaker .
Asymptomatic
1st. or Mobitz type I 2nd. AV block (Wenckebach's phenomenon) no treatmentAsymptomatic
Mobitz type II 2nd. or CHB = permanent pacemaker
Exception (young asymptomatic patients with congenital CHB =mean daytime heart rate of >50 per minute
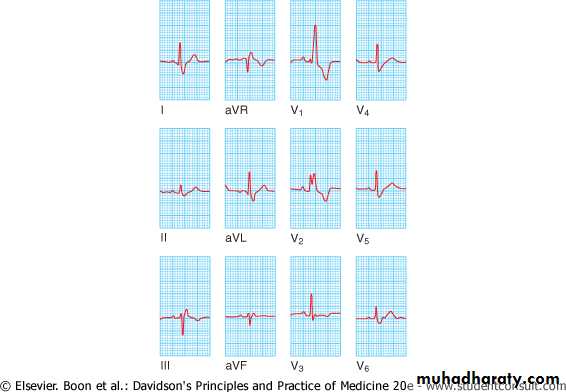
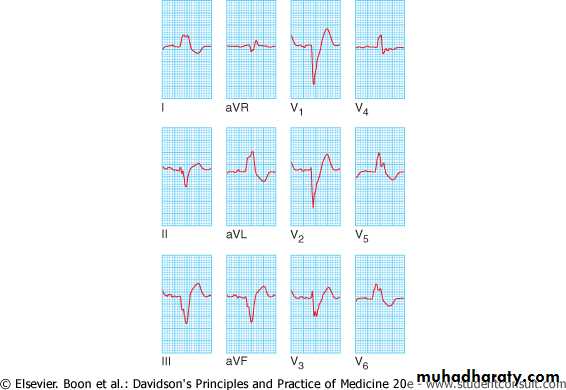
3-BUNDLE BRANCH BLOCK AND HEMIBLOCK
Interruption of right or left branch of bundle of His
delays activation of appropriate ventricle,
broadens the QRS complex (0.12 seconds or more) and
produces characteristic alterations in QRS morphology
RBBB =common normal variant but
LBBB =important underlying heart disease.
left branch of the bundle of His divides into an anterior and a posterior fascicle.
Damage to the conducting tissue at this point (hemiblock) =does not broaden the QRS complex
alters mean direction of ventricular depolarisation (mean QRS axis) left axis deviation in left ant. hemiblock and
right axis deviation in left post. Hemiblock
combination of RBBB and left anterior or posterior hemiblock =bifascicular block
Wide QRS, M in V1 & V2, Wide S in 1
Wide QRS,loss of Q wave or septal vector in 1, M V5,V6
COMMON CAUSES OF BUNDLE BRANCH BLOCK
Right bundle branch blockNormal variant
Right ventricular hypertrophy or strain, e.g. pulmonary embolism
Congenital heart disease, e.g. atrial septal defect
Coronary artery disease
Left bundle branch block
Coronary artery disease
Hypertension
Aortic valve disease
Cardiomyopathy
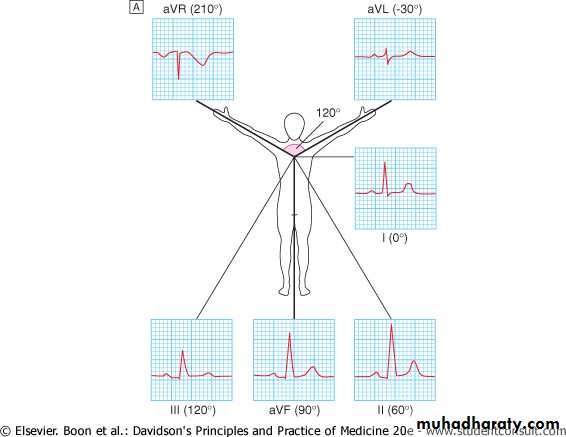
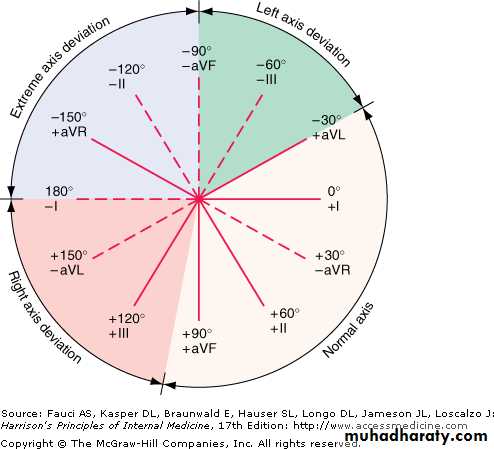
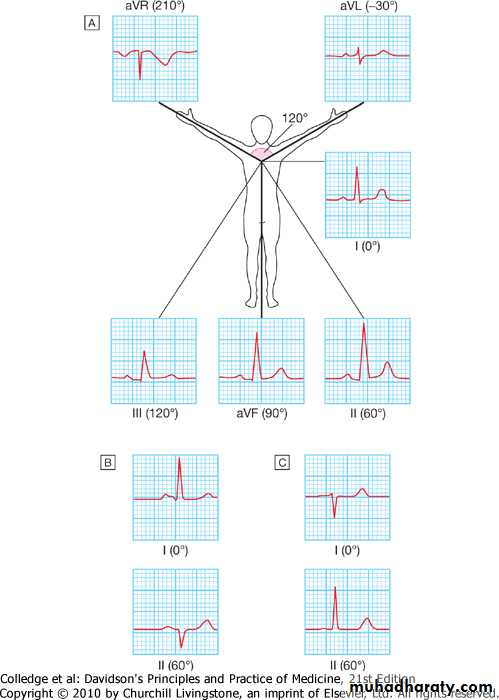
Cardiac axis
Average vector of ventricular depolarisation = frontal cardiac axis.When vector is at right angles to a lead=depolarisation in that lead is equally negative and positive (isoelectric).
Normally =QRS complex is
isoelectric in aVL,
negative in aVR and
most strongly positive in lead II;
main vector or axis of depolarisation is therefore 60 °.
Normal cardiac axis lies between -30 ° and +90 °.
Normal axis
-
Appearance of ECG in diff.frontal leadsA=normal B=LAD C=RAD
ARRHYTHMIA TREATMENT
1-NON-PHARMACOLOGICAL2-PHARMACOLOGICAL
BRADYARRHYTHMIAS
PHARMOCOLOGIC-parasympatholytic- Atropine
sympathomimetic
NON-PHARMACOLOGIC-
CARDIAC PACEMAKERS
PHARMACOLOGIC
Atropine sulphate (0.6 mg i.v., repeated if necessary to a maximum of 3 mg) sinus rate & sinoatrial and AV conduction1-severe bradycardia and/or hypotension (vagal overactivity).
2-initial management of symptomatic bradyarrhythmias complicating the early stages of inferior MI
cardiac arrest due to asystole.
Repeat dosing may be necessary ( drug disappears rapidly from the circulation after parenteral administration.
Side-effects = dry mouth,
thirst
blurred vision
both atrial and ventricular extrasystoles.
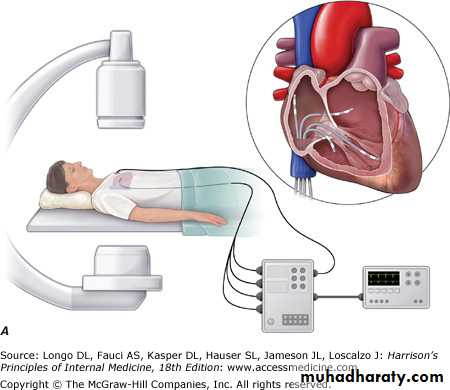
PACEMAKER delivery of an electrical impulse into heart to initiate tissue depolarisation and to trigger cardiac contraction
-
Temporary
.1-Transvenous pacing
Delivered by inserting a bipolar pacing electrode via the internal jugular, subclavian or femoral vein and positioning it at the apex of the right ventricle, using fluoroscopic imaging.
Electrode -connected to an external pulse generator which can be adjusted to alter the energy output or pacing rate.
2-Transcutaneous pacing
delivering an electrical stimulus that is sufficient to induce cardiac contraction
through two large adhesive gel pad electrodes
placed over the apex and upper right sternal edge, or over the precordium and back.
easy and quick to set up
causes significant discomfort
ECG of right ventricular pacing characterised by regular broad QRS complexes with LBBB pattern. Each complex is immediately preceded by a 'pacing spike
-
Indications of temporary pacing
Management of transient AV block and other arrhythmias complicating acute MI or cardiac surgery
Maintain the rhythm in other situations of reversible bradycardia (i.e. due to metabolic disturbance or drug overdose),
Bridge to permanent pacing.
Complications
PneumothoraxBrachial plexus or subclavian artery injury,
Local infection or septicaemia (usually Staphylococcus aureus), and pericarditis.
Failure of the system may be due to lead displacement or a progressive increase in the threshold (exit block) caused by tissue oedema.
Complication rates increase with time and so a temporary pacing system should not be used for more than 7 days.
Permanent pacemakers
small, flat, metal devices that are implanted under the skin, usually in the pectoral area.contain a battery, a pulse generator, and programmable electronics that allow adjustment of pacing and memory functions.
Pacing electrodes (leads) can be placed via the subclavian or cephalic veins into the RV (usually at the apex), the right atrial appendage or, for AV sequential (dual chamber) pacing, both (see Fig. 18.15, p. 536).
programmed using an external programmer via a wireless telemetry system.
TREATMENT OF TACHYARRHYTHMIAS
A-PHARMACOLOGIC-B-NON-PHARMACOLOGIC
1-DC CARDIOVERSION & DEFIBRILLATION
2-RF CATHETER ABLATION & IMPLANTABLE CARDIOVERTER- DEFIBRILLATER(ICD)
ANTI-ARRHYTHMIC DRUGS: PRINCIPLES OF USE
Drugs-potentially toxic –Many arrhythmias are benign and do not require treat.
Precipitating or causal factors. E.g. excess alcohol or caffeine consumption, myocardial ischaemia, hyperthyroidism, acidosis, hypokalaemia and hypomagnesaemia
best to use - few drugs
difficult cases
programmed electrical stimulation (electrophysiological study) - identify optimum therapy
life-threatening arrhythmias
ensure prophylactic treatment -
Patients on long-term anti-arrhythmic drugs - reviewed regularly withdraw therapy if the factors which precipitated the arrhythmias are no longer operative
For patients with recurrent SVT, radiofrequency ablation is often preferable to long-term drug therapy
THERAPEUTIC PROCEDURES
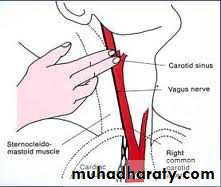
CAROTID SINUS MASSAGEDC SHOCK- Defibrillaters and Cardioversion
IMPLANTABLE CARDIAC DEFIBRILLATORS (ICDS)
CATHETER ABLATION
Carotid sinus massage
performed with patient in supine position
apply light pressure for 5 to 10 seconds
over carotid impulse at angle of jaw=
slowing of ventricular rate .
If no effect
perform CSM over contralateral
carotid impulse.
Caution= carotid bruits
EXTERNAL DEFIBRILLATION AND CARDIOVERSION
2-IMPLANTABLE CARDIAC DEFIBRILLATORS (ICDS)
RF CATHETER ABLATION
EXTERNAL DEFIBRILLATION AND CARDIOVERSION
Heart completely depolarised by passing a sufficiently large electrical current through it from an external source. interrupt any arrhythmia
brief period of asystole resumption of normal sinus rhythm.
Defibrillators= deliver a direct current (DC), high-energy, short-duration shock via two metal paddles coated with conducting jelly or a gel pad, positioned over the upper right sternal edge and the apex.
Energy applied during a critical period around the peak of the T wave may provoke ventricular fibrillation,
treat organised rhythms -atrial fibrillation or v. tachycardia
shock synchronised with ECG and
Normally given 0.02 seconds after the peak of the R wave.
ventricular fibrillation=
Precise timing of the discharge is not importantDefibrillation
delivery of an unsynchronised shock
during a cardiac arrest caused by VF.
precise timing of discharge is not important.
In VF and other emergencies=energy of the first and second shocks should be 150 joules and thereafter up to 200 joules;
there is no need for an anaesthetic (patient is unconscious).
2-IMPLANTABLE CARDIAC DEFIBRILLATORS (ICDS)
resemble large cardiac pacemakerconsist of generator device, and lead or leads (implanted into heart via the subclavian or cephalic vein)
1-automatically sense and terminate life-threatening ventricular arrhythmias using tiered sequences of treatments.
2-ICDs have all of the functions of a pacemaker (to deal with bradycardias) but in addition
3- treat ventricular tachyarrhythmias BY
overdrive pacing, synchronised cardioversion, or defibrillation.
ICD implant procedures =similar complications as pacemaker implants (e.g. infection, erosion-see below). The indications for ICD implantation are expanding as devices
KEY INDICATIONS FOR ICD THERAPY
Primary preventionAfter myocardial infarction, if LV ejection fraction < 30%
Mild to moderate symptomatic heart failure, on optimal drug therapy, with LV ejection fraction < 35%
Secondary prevention
Survivors of VF or VT cardiac arrest not due to transient or reversible cause
VT with haemodynamic compromise or significant LV impairment (LV ejection fraction < 35%)
Cardiac resynchronisation therapy (CRT)
conduction defect associated with left ventricular dys-synchrony (poorly coordinated left ventricular contraction) =aggravate heart failure in susceptible patients.
CRT systems have an additional lead that is placed via the coronary sinus into one of the veins on the epicardial surface of the LV .
Simultaneous septal and left treatment for selected patients with heart failure
1- in sinus rhythm
2- have left bundle branch block.
ventricular epicardial pacing resynchronises left ventricular contraction.
improve effort tolerance and reduce heart failure symptoms
Most CRT devices are also defibrillators (CRT-D) because many patients with heart failure are predisposed to ventricular arrhythmias.
CRT-pacemakers (CRT-P) are used in patients considered to be at relatively low risk of these arrhythmias
CATHETER ABLATION
treatment of choice for many patients with recurrent arrhythmiasA series of catheter electrodes are inserted into heart via venous system,
used to record the activation sequence of the heart in sinus rhythm, during tachycardia and after pacing manoeuvres.
Once the arrhythmia focus or circuit is identified, a steerable catheter is placed into this critical zone (e.g. over an accessory pathway, in Wolff-Parkinson-White syndrome)
culprit tissue is selectively ablated using
1-heat (via radiofrequency current)
2- sometimes by freezing (cryoablation).
INDICATIONS OF CATHETER ABLATION
1- treatment of choice forAV nodal re-entry tachycardia and
atrioventricular re-entrant (accessory pathway) tachycardias, where it is curative in more than 90% of cases.
2-Focal atrial tachycardias and atrial flutter can also be eliminated by radiofrequency ablation, although some patients subsequently experience episodes of atrial fibrillation.
3- applications of the technique are expanding and it can now be used to treat some forms of ventricular tachycardia
ANTI-ARRHYTHMIC DRUG THERAPY
A-according to mode of action (IC ACTION P)Class 1
Class 11
Class 111
Class 1V
Unlassified
B-according to site of action
1-drugs acting on SA node2-drugs acting on AV node
3-drugs acting on the ventricle
4-drugs acting on atria,vent. &
accessory pathways
SAN
AVN
Impulse conduction
Impulses originate regularly at a frequency of 60-100 beat/ min-100
-80-60
-40
-20
0
20
Phase 0
Phase 1
Phase 2Phase 3
Phase 4
Na+ca++
ATPasemv
Cardiac Action Potential
Resting membrane Potential
Na+
m
Na+
Na+
Na+
Na+
Na+
h
K+
ca++
K+K+
K+
ca++
ca++
(Plateau Phase)
K+
K+
K+
Na+
K+
Depolarization
Repolarization
-100-80
-60
-40
-20
0
20
Phase 0
Phase 1
Phase 2Phase 3
Phase 4
Na+ca++
ATPasemv
Cardiac Action Potential
R.M.P
Na+
m
Na+
Na+
Na+
Na+
Na+
h
K+
ca++
K+K+
K+
ca++
ca++
(Plateau Phase)
K+
K+
K+
Na+
K+
Depolarization
Repolarization
Phase 4(only in pacemaker cells
AAD-ACCORDING TO EFFECT ON IC A.POTENTIAL
Class I-membrane-stabilising agents (sodium channel blockers)
(a) Block Na+ channel and prolong action potential
Quinidine, disopyramide –
MODERATE POTENCY
Manily atrial & vent.
(b) Block Na+ channel and shorten action potential
Lidocaine, mexiletine
-WEAK-
mainly vent.
(c) Block Na+ channel with no effect on action potential
Flecanide, propafenone-
POTENT-
manily supravent.
I
-
Class II
-β-adrenoceptor antagonists (β-blockers)
Atenolol, bisoprolol, metoprolol, I-sotalol
Class III
-drugs whose main effect is to prolong the action potential
Amiodarone, d-sotalol
Class IV
-slow calcium channel blockers
Verapamil, diltiazem
N.B.
Some drugs (e.g. digoxin and adenosine) have no place in this classification,
others have properties in more than one class, e.g. amiodarone, which has actions in all four classes.
-
Class I
suppress excitability and slow conduction in atrial or ventricular muscle.
1A-
Quinidine
S.E.= torsades de pointes, hypersensitivity and unpleasant gastrointestinal increase mortality in patients with paroxysmal atrial fibrillation
Disopyramide
S.E.
weak atropine-like effects - urinary retention or precipitate glaucoma.
depressant effect on ventricular function - avoided in cardiac failure.
used in patients with atrial flutter and AV block
risk of a paradoxical increase in heart rate as the atria slow and 2:1 block changes to 1:1 conduction; this can be prevented by pre-treatment with digoxin.
Procainamide
S.E
Lupus erythematosus-like syndrome (more common in slow acetylators), anorexia, nausea, neutropenia
Dose in SVT=P10–15 mg/kg5 mg/kg750–1500 mg qid
-
1B-
Lidocaine –
given parenterally
very short plasma half-life, so plasma concentration will depend on the rate of infusion.
urgent treatment or prophylaxis of ventricular tachycardia.
Mexiletine –
intravenously or orally
treatment or prophylaxis of ventricular arrhythmias.
Side-effects i= nausea, vomiting, confusion, dizziness, tremor and nystagmus
-
1C-
Flecainide
intravenously or orally
treatment or prophylaxis of supraventricular or ventricular arrhythmias
management of Wolff-Parkinson-White syndrome.
potent myocardial depressant XX poor left ventricular function.
pro-arrhythmic - hazardous in patients with a history of myocardial infarction.
Propafenone
treatment or prophylaxis of all tachyarrhythmias
particularly useful in paroxysmal atrial fibrillation, ventricular tachycardia and the Wolff-Parkinson-White syndrome.
Propafenone is a class Ic drug but also has some β-blocker (class II) properties
may precipitate heart failure or heart block in susceptible patients.
Important interactions with digoxin, warfarin and cimetidine have been described.
-
Class II drugs
β-adrenoceptor antagonists (β-blockers).
agents used most commonly
Atenolol, bisoprolol and metoprolol
cardioselective β-blockers - usually well tolerated.
Sotalol
racemic mixture of two isomers with non-selective β-blocker (mainly l-sotalol) and class III (mainly d-sotalol) activity.
may cause torsades de pointes.
Propranolol
not cardioselective
subject to extensive first-pass metabolism in the liver effective oral dose – unpredictable-must be titrated after treatment is started with a small dose.
-
Class III drugs
Class III drugs act by prolonging the plateau phase of the action potential, thus lengthening the refractory period. (k-channel blockers)
Amiodarone - principal drug in this class, ( disopyramide and sotalol have class III activity).
effective against a wide variety of atrial and ventricular arrhythmias.
t most effective drug currently available for controlling
1-paroxysmal atrial fibrillation
2-arrhythmias associated with the Wolff-Parkinson-White syndrome.
very useful in preventing episodes of recurrent ventricular tachycardia, particularly in patients with poor left ventricular function.
Amiodarone has an extraordinarily long tissue half-life (25-110 days). = onset of action after oral and intravenous therapy is delayed; - may take several months to reach steady state. drug's effects may last for weeks or months after treatment has been stopped.
Side-effects 1/3RD.
photosensitisation, corneal deposits, gastrointestinal problems, thyroid dysfunction (liver disease, pul-monary fibrosis and torsades de pointes. Drug interactions are also common; for example, the effects of digoxin and warfarin are potentiated by amiodarone
Dronedarone A related drug that has a short tissue half-life and fewer side effects. - effective at preventing episodes of atrial flutter and fibrillation
-
Class IV drugs
block 'slow calcium channel' esp. important = impulse generation and conduction in atrial and nodal tissue, (also present in ventricular muscle).
Verapamil
most widely used anti-arrhythmic drug
diltiazem- similar properties.
IV verapamil - cause profound bradycardia and/or hypotension
should not be used in conjunction with oral or intravenous β-blockers.
Other anti-arrhythmic drugs
ADENOSINE
DIGOXIN
-
ADENOSINE-
intravenously;
like CSM transient AV block lasting a few seconds.
1-used to terminate junctional tachycardias when the AV node is part of the re-entry circuit
2- establish the diagnosis in difficult arrhythmias such as atrial flutter with 2:1 AV block or broad-complex tachycardia (DOSAGE= iIV bolus = ascending dosage schedule.
initial dose is 3 mg given over 2 seconds= no response after 1-2 minutes 6 mg should be given = wait another 1-2 minutes b administer the maximum dose of 12 mg.
short-lived and sometimes distressing side-effects of
flushing, breathlessness and chest pain.
bronchospasm = avoided in asthmatics;
effects are greatly potentiated by dipyridamole a
inhibited by theophylline and other xanthines
RESPONSE TO INTRAVENOUS ADENOSINE
Arrhythmia Response========================
Supraventricular junctional tachycardia Termination
Atrial fibrillation, atrial flutter Transient AV block
Ventricular tachycardia No effect
-
DIGOXIN
purified glycoside from the European foxglove, Digitalis lanata,
slows conduction and prolongs the refractory period in the AV node.
1- control the ventricular rate in atrial fibrillation
2- interrupt re-entry tachycardias involving the AV node.
tends to shorten refractory periods and enhance excitability and conduction in other parts of the heart (including accessory conduction pathways); increase atrial and ventricular ectopic activity more complex atrial and ventricular tachyarrhythmias.
largely excreted by the kidneys,
maintenance dose (should be reduced in children, the elderly and those with renal impairment.
widely distributed and has a long tissue half-life (36 hours)
effects may persist several days after the last dose.
Measurements of plasma digoxin concentration are useful in demonstrating that the dose is inadequate and in confirming a clinical impression of toxicity (
DIGOXIN TOXICITY
Extracardiac manifestationsAnorexia, nausea, vomiting
Diarrhoea
Altered colour vision (xanthopsia)
Cardiac manifestations
Bradycardia
Multiple ventricular ectopics
Ventricular bigeminy (alternate ventricular ectopics)
Atrial tachycardia (with variable block)
Ventricular tachycardia
Ventricular fibrillation
THE MAIN USES, DOSAGES AND SIDE-EFFECTS OF THE MOST WIDELY USED ANTI-ARRHYTHMIC DRUGS
Drug Main uses Route Dose (adult) Important side-e
CLASS I
Disopyramide
Prevention and treatment of atrial and ventricular tachyarrhythmiasI.v.Oral2 mg/kg at 30 mg/min then 0.4 mg/kg/hr (max 800 mg/day)300-800 mg daily in divided dosageMyocardial depression, hypotension, dry mouth, urinary retention
Lidocaine
Treatment and short-term prevention of VT and VFI.v.Bolus 50-100 mg 4 mg/min for 30 mins, then 2 mg/min for 2 hrs, then 1 mg/min for 24 hrsMyocardial depression, confusion, convulsions
Mexiletine
Prevention and treatment of ventricular tachyarrhythmiasI.v.Loading dose: 100-250 mg at 25 mg/minthen 250 mg in 1 hrthen 250 mg in 2 hrsMaintenance therapy: 0.5 mg/minMyocardial depression, GI irritation, confusion, dizziness, tremor, nystagmus, ataxia Oral200-250 mg 8-hourly
Flecainide
Prevention and treatment of atrial and ventricular tachyarrhythmiasI.v.2 mg/kg over 10 mins then 1.5 mg/kg/hr for 1 hrthen 0.1 mg/kg/hrMyocardial depression, dizziness Oral50-100 mg 12-hourly
Propafenone Prevention and treatment of atrial and ventricular tachyarrhythmiasOral150 mg 8-hourly for 1 weekthen 300 mg 12-hourlyMyocardial depression, dizzinessCLASS II
-
CLASS II
Atenolol
Treatment and prevention of SVT and AFPrevention of VEs and exercise-induced VTI.v.2.5 mg at 1 mg/min repeated at 5 min intervals (max 10 mg)Myocardial depression, bradycardia, bronchospasm, fatigue, depression, nightmares, cold peripheriesSotalol can cause torsades de pointes Oral25-100 mg daily
Bisoprolol
Oral2.5-10 mg daily
Metoprolol
I.v.5 mg over 2 mins to a maximum of 15 mg Oral50-100 mg 8- or 12-hourlySotalolI.v.10-20 mg slowlySotalol can cause torsades de pointes Oral40-160 mg 12-hourly
CLASS III
Amiodarone
Serious or resistant atrial and ventricular tachyarrhythmiasI.v.5 mg/kg over 20-120 mins then up to 15 mg/kg/24 hrsPhotosensitivity, skin discoloration, corneal deposits, thyroid dysfunction, OralInitially 600-1200 mg/day then then 100-400 mg dailyalveolitis, nausea and vomiting, hepatotoxicity, peripheral neuropathy, torsades de pointes; potentiates digoxin and warfarinC
-
CLASS IV
Verapamil
Treatment of SVT, control of AFI.v.Oral5-10 mg over 30 secs40-120 mg 8-hourly or 240 mg SR dailyMyocardial depression, hypotension, bradycardia, constipation
OTHERS
Atropine
Treatment of bradycardia and/or hypotension due to vagal overactivityI.v.0.6-3 mgDry mouth, thirst, blurred vision, atrial and ventricular extrasystoles
Adenosine
Treatment of SVT, aid to diagnosis in unidentified tachycardiaI.v.3 mg over 2 secs, followed if necessary by 6 mg then 12 mg at intervals of 1-2 mins Flushing, dyspnoea, chest painAvoid in asthma
Digoxin
Treatment and prevention of SVT, rate control of AFI.v.Loading dose: 0.5-1 mg (total), 0.5 mg over 30 mins then 0.25-0.5 mg 4- to 8-hourly to maximum total of 1 mg, assessing response before each additional doseGI disturbance, xanthopsia, arrhythmias ( Oral0.5 mg 6-hourly for 2 doses, then0.125-0.25 mg daily