1
Atrial flutter
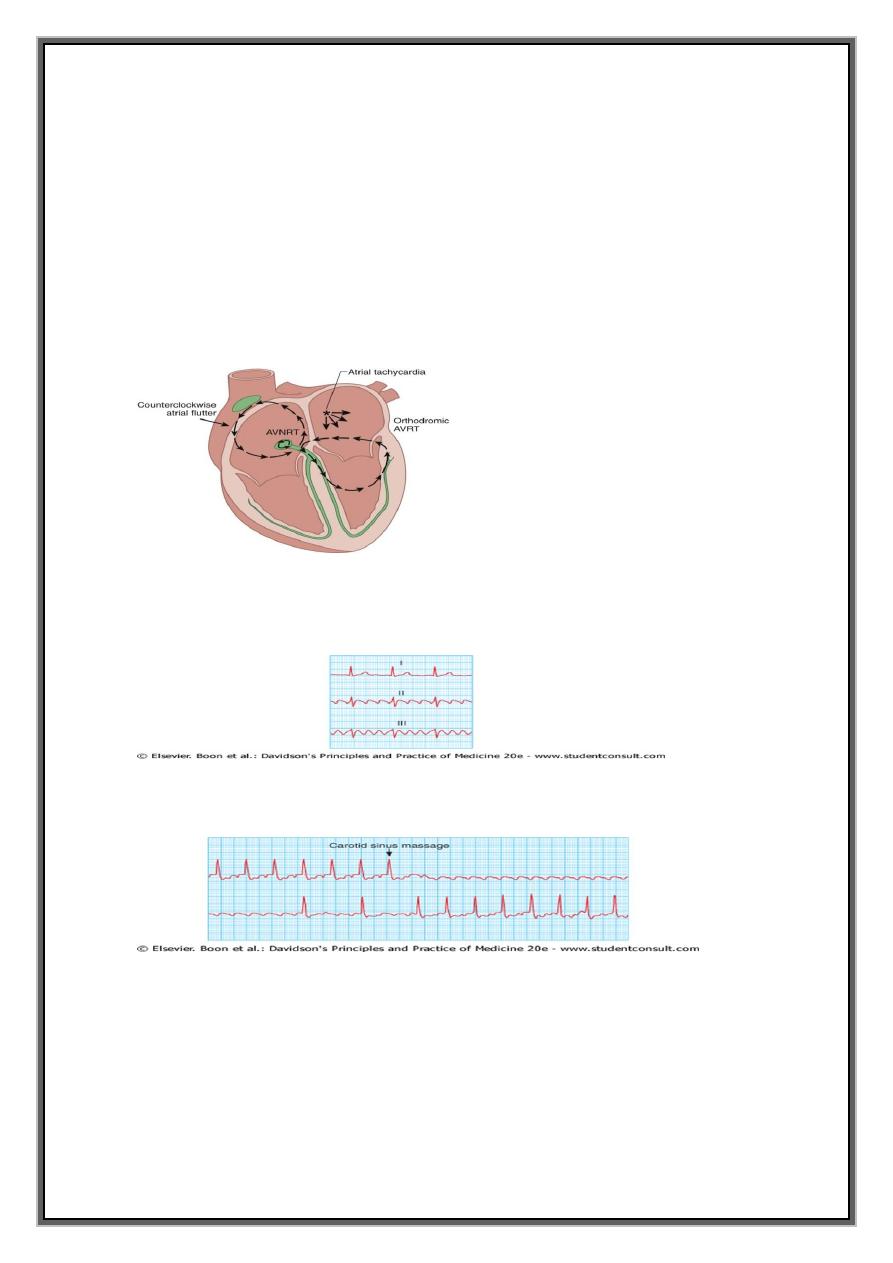
Mechanism:Characterised by large (macro) re-entry circuit within the right atrium,
usually encircling tricuspid annulus.
Atrial rate is approximately 300/min.
usually associated with 2:1, 3:1, or 4:1 atrioventricular block (with corresponding heart
rates of 150, 100, 75).
Rarely, in young patients, every beat is conducted, producing a heart rate of 300/min
and haemodynamic collapse
ECG = saw-toothed flutter waves .(if regular 2:1 AV block -difficult to identify flutter
waves --buried in the QRS complexes and T-waves. suspected Af=narrow complex
tachycardia of 150/min.)
CSM or IV adenosine = help to establish the diagnosis( by temporarily increasing the degree
of AV block and revealing the flutter waves )
2
Management OF Atrial Flutter
Treatment
Control ventricular rate=Digoxin
β-blockers or
verapamil
Restore sinus rhythm = direct current (DC) cardioversion or
drug therapy.
Prevention
Beta-blockers or amiodarone
Catheter ablation
offers a 90% chance of complete cure
-
ATRIAL FIBRILLATION
1-Mechanism
2-Classification
3-Causes
4-Clinical manifestations
5-Investigations
6-Management
Incidence and prevelance:
most common sustained cardiac arrhythmia,
Overall prevalence = 0.5% in adult population of UK.
Prevalence rises with age, affecting 2-5% of 70-year-olds and 9% of those aged over 80
years.
Characteristics:
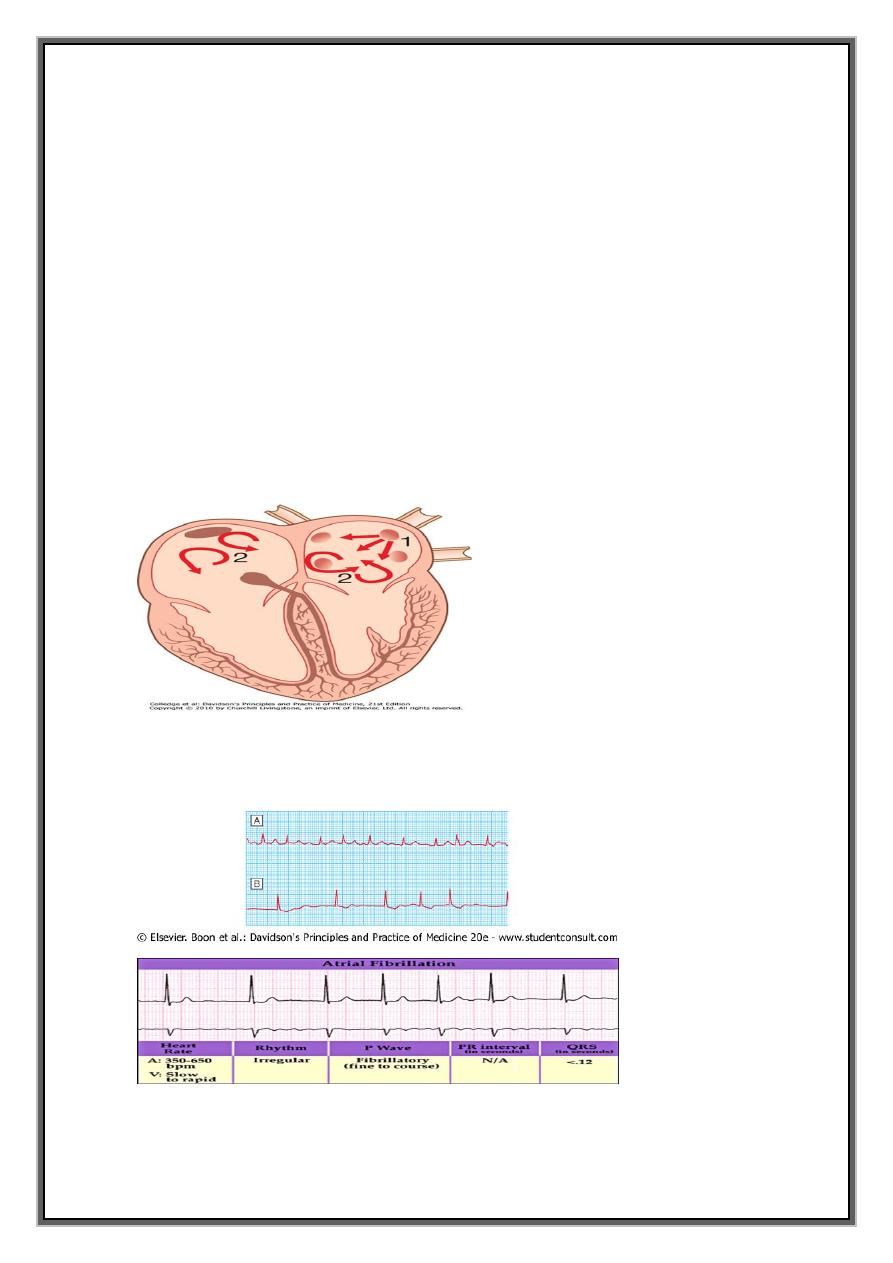
complex arrhythmia characterised by both
1-abnormal automatic firing
2- presence of multiple interacting re-entry circuits looping around atria
3
Mechanism
1-Episodes of atrial fibrillation -usually initiated by rapid bursts of ectopic beats arising
from conducting tissue in pulmonary veins or from diseased atrial tissue.
2- sustained by initiation of re-entrant conduction within atria or by continuous ectopic
firing .
Re-entry -more likely in enlarged atria , or in which conduction is slow
Consequences=
During episodes of AF, atria beat rapidly but in an uncoordinated and ineffective
manner.
Ventricles are activated irregularly at a rate determined by conduction through the AV
node==> characteristic 'irregularly irregular' pulse.
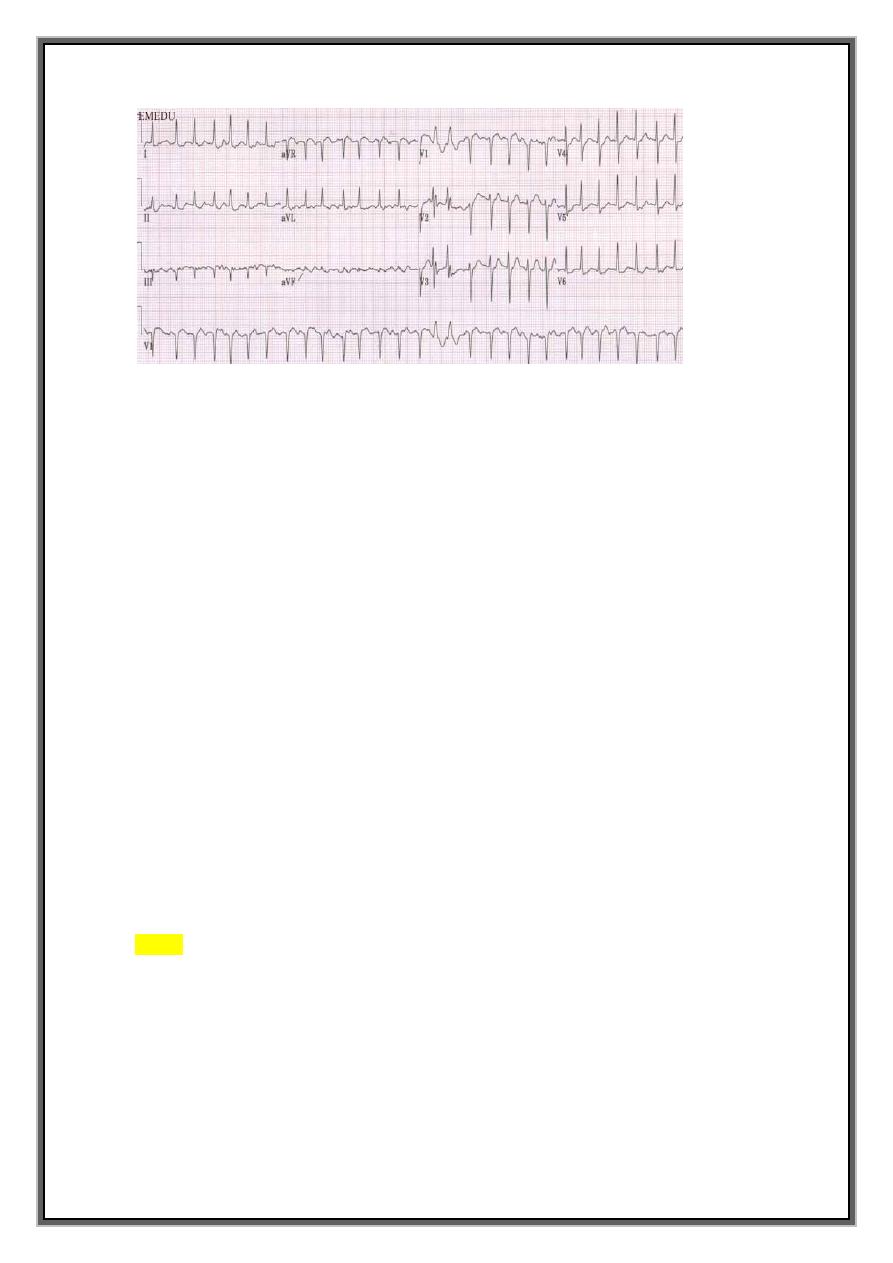
ATRIAL FIBRILLATION
ECG = normal but irregular QRS complexes
No P waves but the baseline may show irregular fibrillation waves
4
Classification
1-paroxysmal=intermittent= self-terminating episodes
2- persistent=prolonged episodes terminated by electrical or chemical
cardioversion) =7 days
3- permanent.
AF seen for the first time- difficult to identify which of these.
Many patients, paroxysmal AF will become permanent as the underlying disease
process that predisposes to AF progresses.
Pathgology
1- electrical remodelling.
Electrophysiological changes occur in the atria within few hours of the onset of AF that
tend to maintain fibrillation:
2- structural remodelling
When AF persists for a period of months, structural remodelling occurs with atrial
fibrosis and dilatation that further predispose to AF.
early treatment of AF will prevent this and reinitiation of the arrhythmia.
Causes
NORMAL & ABNORMAL HEART
1-Abnormal Heart – first manifestation of many forms heart dis.
(particularly those associated with enlargement or dilatation of the atria).
common causes of AF
Alcohol excess
5
hyperthyroidism
chronic lung disease
multiple aetiological factors often coexist such as the combination of alcohol,
hypertension and coronary disease.
2-Normal heart
About 50% of all patients with paroxysmal AF and
20% of patients with persistent or permanent AF= structurally normal hearts= ‘Lone atrial
fibrillation
Common causes
Coronary artery disease (including Acute MI)
Valvular heart disease, especially rheumatic MVD disease
Hypertension
Sinoatrial disease
Hyperthyroidism
Alcohol
Cardiomyopathy
Congenital heart disease
Chest infection
Pulmonary embolism
Pericardial disease
Idiopathic (lone AF)
Clinical Manifestations
completely asymptomatic (routine examination or ECG)
Symptomatic
1-palpitation
2- breathlessness
3- fatigue.
4- patients with poor ventricular function or valve disease ===> precipitate or
aggravate cardiac failure (loss of atrial function and heart rate control).
6
5- lightheadedness(A fall in blood pressure)
chest pain = with underlying coronary disease
Management
Assessment
full history, physical examination, 12-lead ECG, echocardiogram and thyroid function
tests.
Additional investigations --exercise testing -nature and extent of any underlying heart
disease.
Biochemical evidence of hyperthyroidism is found in a small minority of patients with
otherwise unexplained AF.
When AF complicates an acute illness (e.g. chest infection, pulmonary embolism),
effective treatment of the primary disorder will often restore sinus rhythm.
main objectives
1- restore sinus rhythm as soon as possible,
2- prevent recurrent episodes of AF,
3- optimise heart rate during periods of AF,
4- minimise risk of thromboembolism and
5- treat any underlying disease.
Summary of treatment
PAROXYSMAL-ACUTE
TREATMENT= Beta-blockers, Digoxin and verapamil
PREVENTION= Amiodarone , Class Ic drugs (propafenone or flecainide
Catheter ablation
CHRONIC (Persistant & Perminant)
Rhythm control= DC cardioversion /flecainide
Prevention: amiodarone or β-blockers
Rate control= Digoxin, β-blockers or calcium antagonists
7
1-Paroxysmal atrial fibrillation
Treatment
well tolerated (Occasional attacks) =no treatment.
Beta-blockers - first-line therapy
Troublesome symptoms/ AF associated with IHD, HT and HF.
Digoxin and verapamil = limit heart rate ( by blocking the AV node).
prevention
Class Ic ( propafenone or flecainide) +rate limiting β-blocker
Amiodarone - most effective agent for preventing AF
Digoxin and verapamil = not effective for preventing paroxysms of AF.
Catheter ablation
isolate electrically pulmonary veins from LA,
create lines of conduction block within atria to prevent re-entry.
prevents AF in 70% of patients with prior drug-resistant episodes.
associated with a small risk of embolic stroke or cardiac tamponade.
Specialised 'AF suppression' pacemakers
A.F
ACUTE
TREATMENT
BB/DIG./VERA
P
PREVENTION
Amiodarone ,
Class Ic
CHRO
NIC
RHYTM=CORRE
CTION
DC
SHOCK+PREV
RATE CONTROL
BB./DIG./CCB
8
2-Persistent and permanent atrial fibrillation
Two options :
A-Rhythm control:
DC Cardioversion (immediate or elective) or
flecainide
+ Anti-coagulant(<48 hr.=heparin
>48 hr.=warfarin)
B-Rate control: AF permanent
treatments to control ventricular rate
prevent embolic complications.
Digoxin, BB, CCB alone or combination
Pace and ablate
Rhythm control=DC (Immediate vs Elective)
TREATMENT
A-troublesome symptoms + modifiable or treatable underlying cause.
Electrical cardioversion - 1- AF has been present for < 3 months,
2- patient is young
3-no important structural heart disease.
Immediate DC cardioversion after the administration of IV heparin AF < 48 hours.
(infusing IV flecainide (2 mg/kg over 30 minutes, maximum dose 150 mg) safe
alternative
B- other situations, DC cardioversion deferred until
patient established on warfarin, with INR > 2.0 for a minimum of 4 weeks,
Anticoagulation maintained for 3 months following successful cardioversion;
PREVENTION
Concomitant therapy with amiodarone or β-B may reduce the risk of recurrence.
Catheter ablation -in resistant cases,
9
less effective treatment for persistent AF than for paroxysmal AF.
Risk stratification
1- high or very high risk of stroke= Warfarin .
relative contraindications =Comorbid conditions -peptic ulcer, uncontrolled hypertension,
alcohol misuse, frequent falls, poor drug compliance and potential drug interactions
2- moderate risk of stroke== warfarin or aspirin
warfarin or aspirin after discussing balance of risk and benefit with individual.
3- very low risk of stroke =Aspirin
Young patients (under 65 years) =no evidence of structural heart disease =very low risk of
stroke=do not require warfarin but may benefit from aspirin.
RISK FACTORS FOR THROMBOEMBOLISM IN A. FIBRILLATION
Previous ischaemic stroke or transient ischaemic attack
Mitral valve disease
Age over 65
Hypertension
Diabetes mellitus
Heart failure
Echocardiographic features of:
left ventricular dysfunction,
left atrial enlargeme.nt or
mitral annular calcification
ATRIAL FIBRILLATION IN OLD AGE
Prevalence:
rises with age, reaching more than 10% over 80 years
Symptoms:
sometimes asymptomatic but often accompanied by diastolic heart failure.
Hyperthyroidism:
AF may be the dominant feature of otherwise silent or occult hyperthyroidism.
11
Cardioversion: followed by high rates (∼70% at one year) of recurrent
Stroke:
important cause of cerebral embolism.
found in 15% of all stroke patients and 2-8% of those with TIAs.
Anticoagulation:
hazards of anticoagulation also rise with age because of increased comorbidity,
particularly cognitive impairment and falls.
Target INR:
over 75 years--maintain INR below 3.0 ( risk of intracranial haemorrhage.
Aspirin:
safer alternative if anticoagulation cannot be recommended,
benefits in reducing risk of stroke less significant and consistent
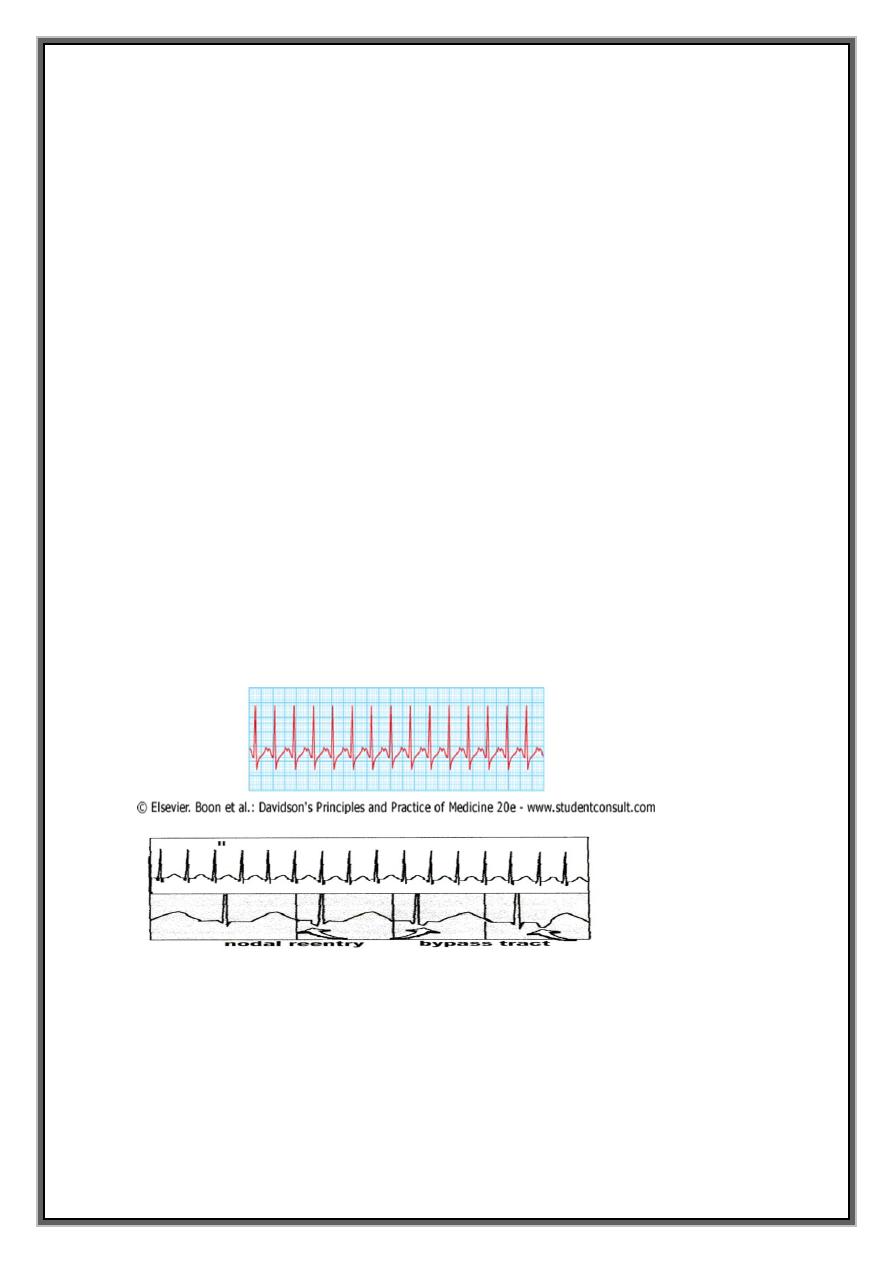
'SUPRAVENTRICULAR-JUNTIONAL TACHYCARDIAS
supraventricular tachycardia (SVT)= regular tachycardias =ECG =narrow QRS complex
+re-entry circuit or automatic focus involving atria.
SUPRA-VENTRICULARTACHYARRHYTHMIAS
1-ATRIAL=AT.AF.AF
2-JUNCTIONAL(AV-NODAL)=
AV NODAL DUAL REENTRY
TYPICAL-ant. Slow &retro. fast
11
ATYPICAL-
A-V ACCESSORY REENTRANT(BYPASS)
CONCEALED-ORTHO (in AV node)
MANIFEST-ANTI
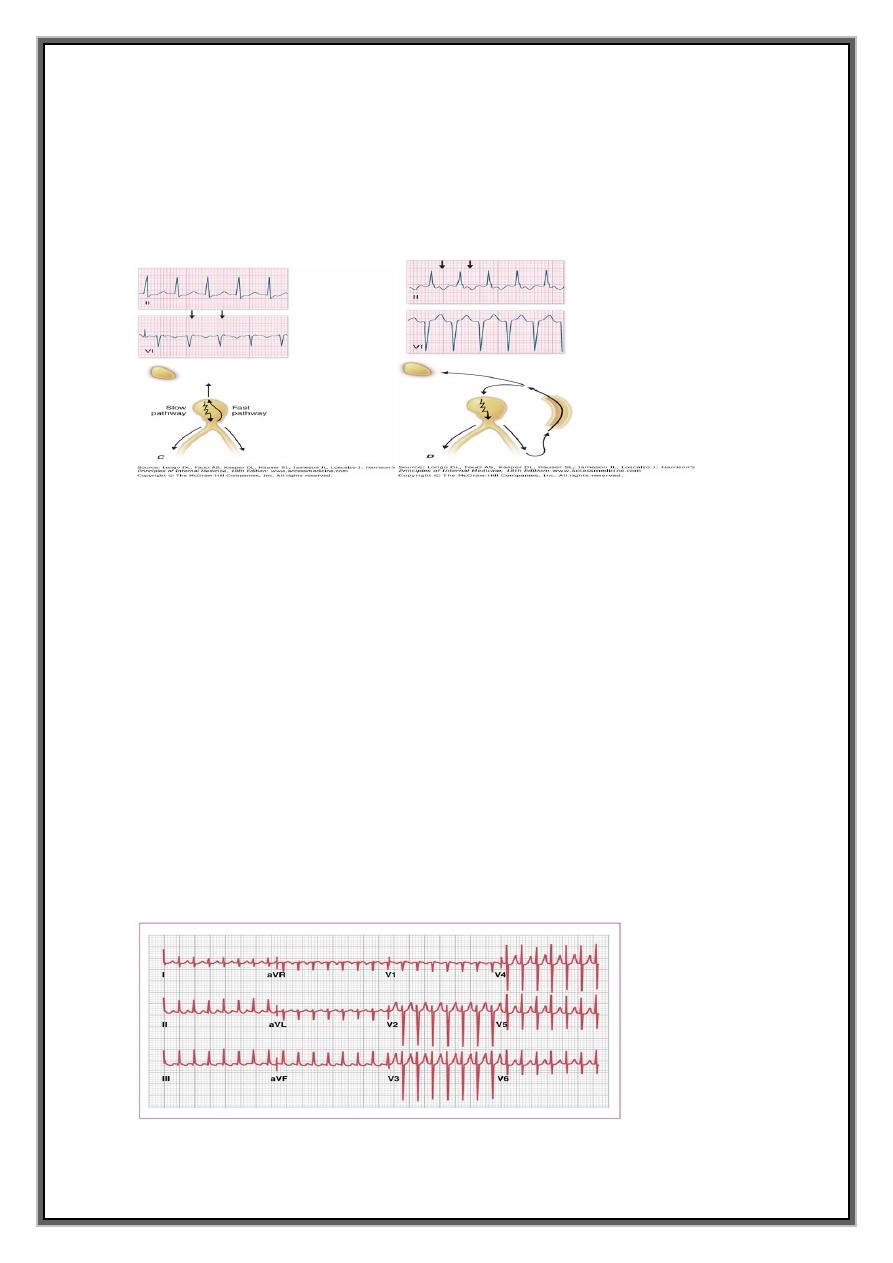
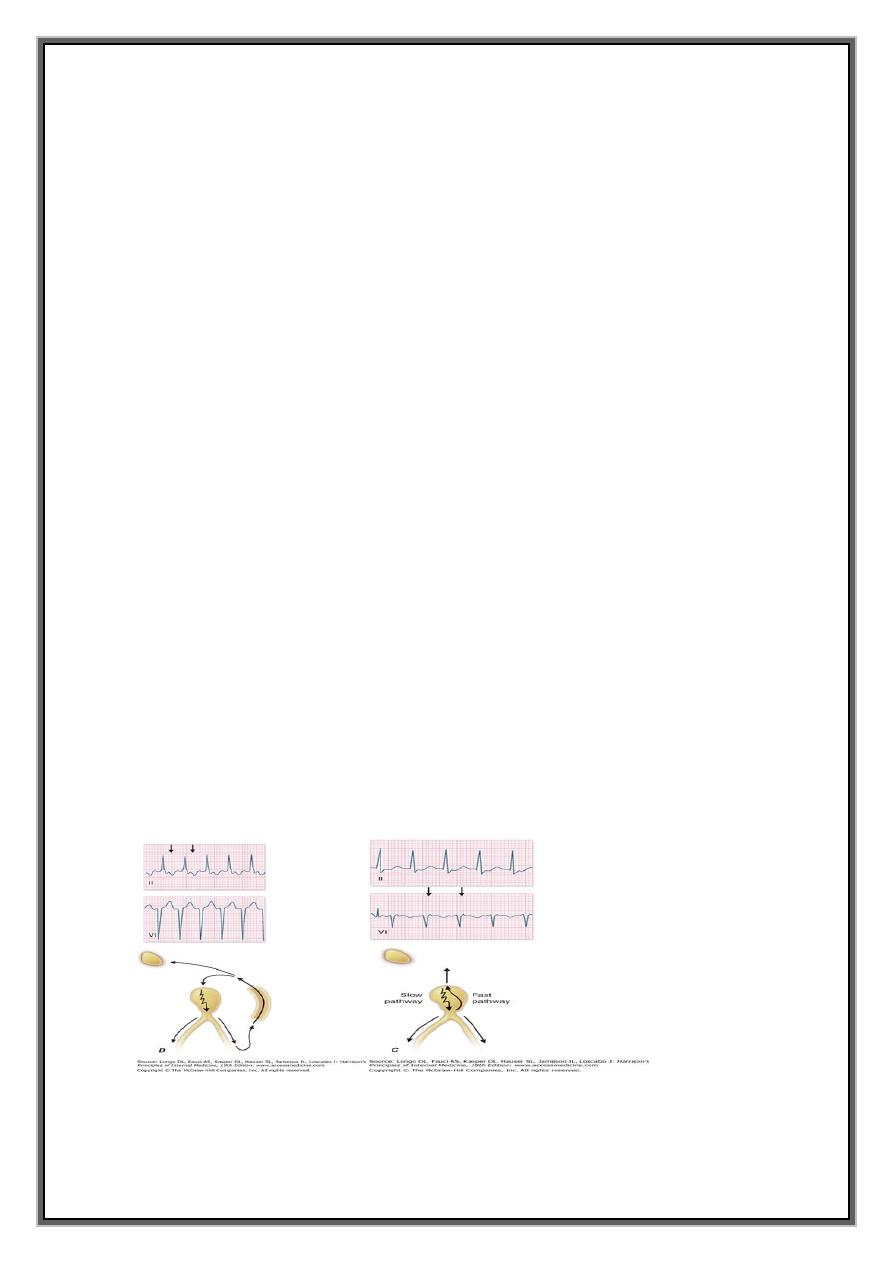
1-ATRIOVENTRICULAR NODAL REENTRANT TACHYCARDIA (AVNRT)
Due to re-entry in the circuit involving AV node and its two right atrial input pathways
: superior fast pathway and inferior slow pathway
tends to occur in normal hearts
episodes =few seconds to many hours.
usually aware of a fast heart beat
feel faint or breathless.
Polyuria, (release of atrial natriuretic peptide)
cardiac pain or heart failure ( coexisting structural heart dis
ECG =tachycardia with normal QRS complexes but occasionally -rate-dependent
bundle branch block
regular tachycardia with a rate of 140-220/min
12
Management
not always necessary.
attack terminated by carotid sinus pressure or measures that increase vagal tone
(Valsalva manoeuvre).
IV adenosine or verapamil - restore sinus rhythm
Suitable alternative / β-blockers, flecainide and digoxin.
emergency =severe haemodynamic compromise = DC cardioversion .
Prophylaxis
frequent or disabling= prophylactic oral therapy
β-blocker, verapamil, disopyramide or digoxin .
Catheter ablation =very high chance of complete cure
preferable to long-term drug treatment
2-ATRIOVENTRICULAR RE-ENTRANT TACHYCARDIA (AVRT) AND WOLFF-PARKINSON-
WHITE SYNDROME
ANOMALOUS TISSUE (accessory ,bypass) Macroreentrant
1-SINUS RHYTHM
2-SUPRAVENTRICULAR
3-ATRIAL FIBRILLATION & FLUTTER. Nodal reentry
Bypass tract
13
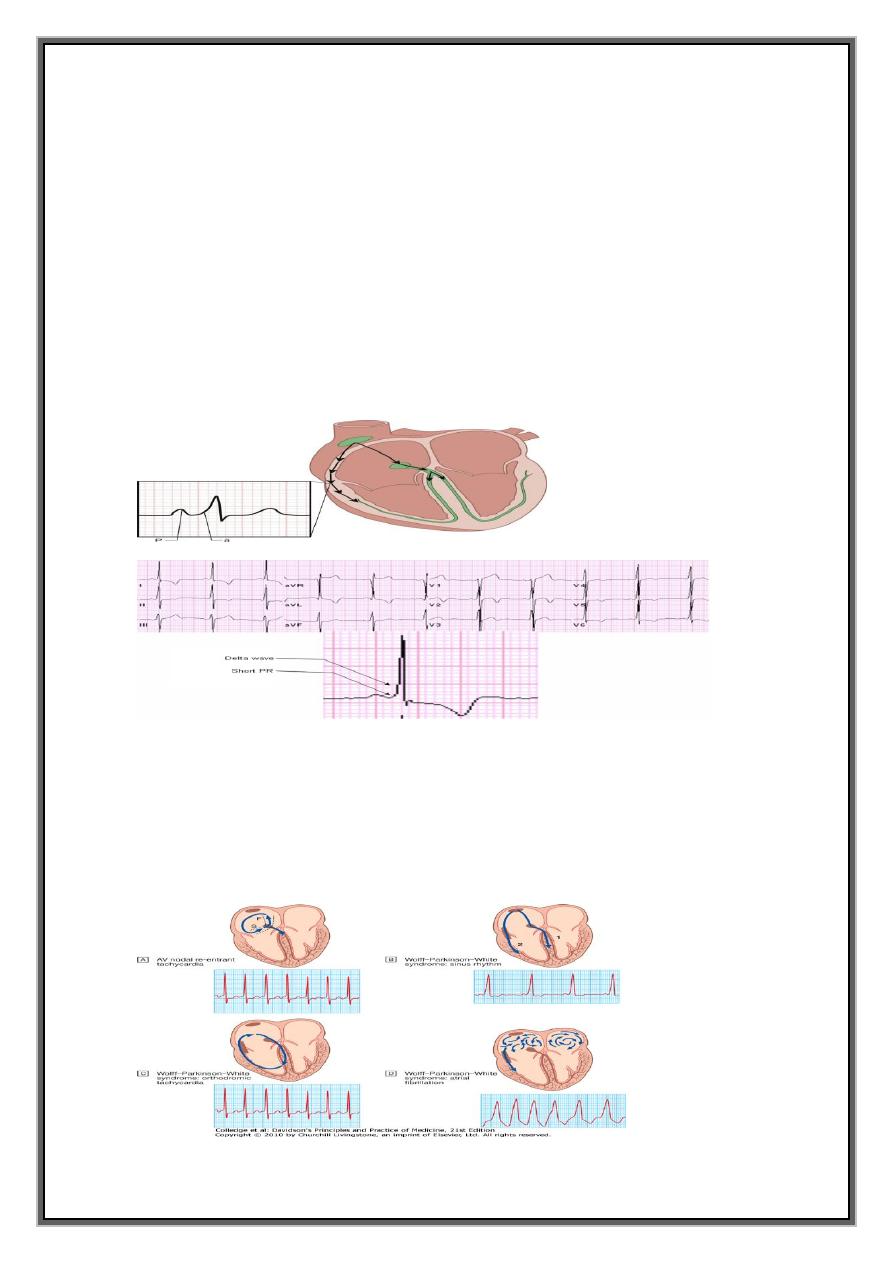
WPW
Abnormal band of conducting tissue - connects atria and ventricles.
Resembles Purkinje tissue - conducts very rapidly = accessory pathway.
Premature activation of ventricular tissue via pathway produces a short PR interval
and a 'slurring' of the QRS complex, called a delta wave =
(As the AV node and bypass tract have different conduction speeds and refractory
periods, a re-entry circuit can develop, causing tachycardia)
when associated with symptoms = Wolff-Parkinson-White syndrome.
1- concealed accessory pathway-half of cases pathway only conducts in retrograde
direction (from ventricles to atria) = does not alter the appearance of ECG in sinus
rhythm=
2- manifest accessory pathway= remainder of cases, conduction takes place partly
through the AV node and partly through rapidly conducting accessory pathway during
sinus rhythmè
14
Management
Tachycardia= Carotid sinus pressure or IV adenosine Atrial fibrillation = DC
cardioversion
AF produce a dangerously rapid ventricular rate (accessory pathway lacks rate-limiting
properties of the AV node )=( pre-excited atrial fibrillation) = collapse, syncope and
even death.
Treated as an emergency=with DC cardioversion (never AV nodal blocking drugs)
Catheter ablation = first-line treatment in symptomatic patients and is nearly always
curative.
Prophylactic anti-arrhythmic flecainide, propafenone or amiodarone ,( These slow the
conduction rate and prolong the refractory period of the accessory pathway).
Digoxin and verapamil shorten the refractory period of the accessory pathway and should
be avoided
