1
ECG IN DISEASE STATES
ARRHYTHMIAS
HYPERTROPHY
BUNDLE BRANCH BLOCK
ISCHEMIC HEART DISEASE
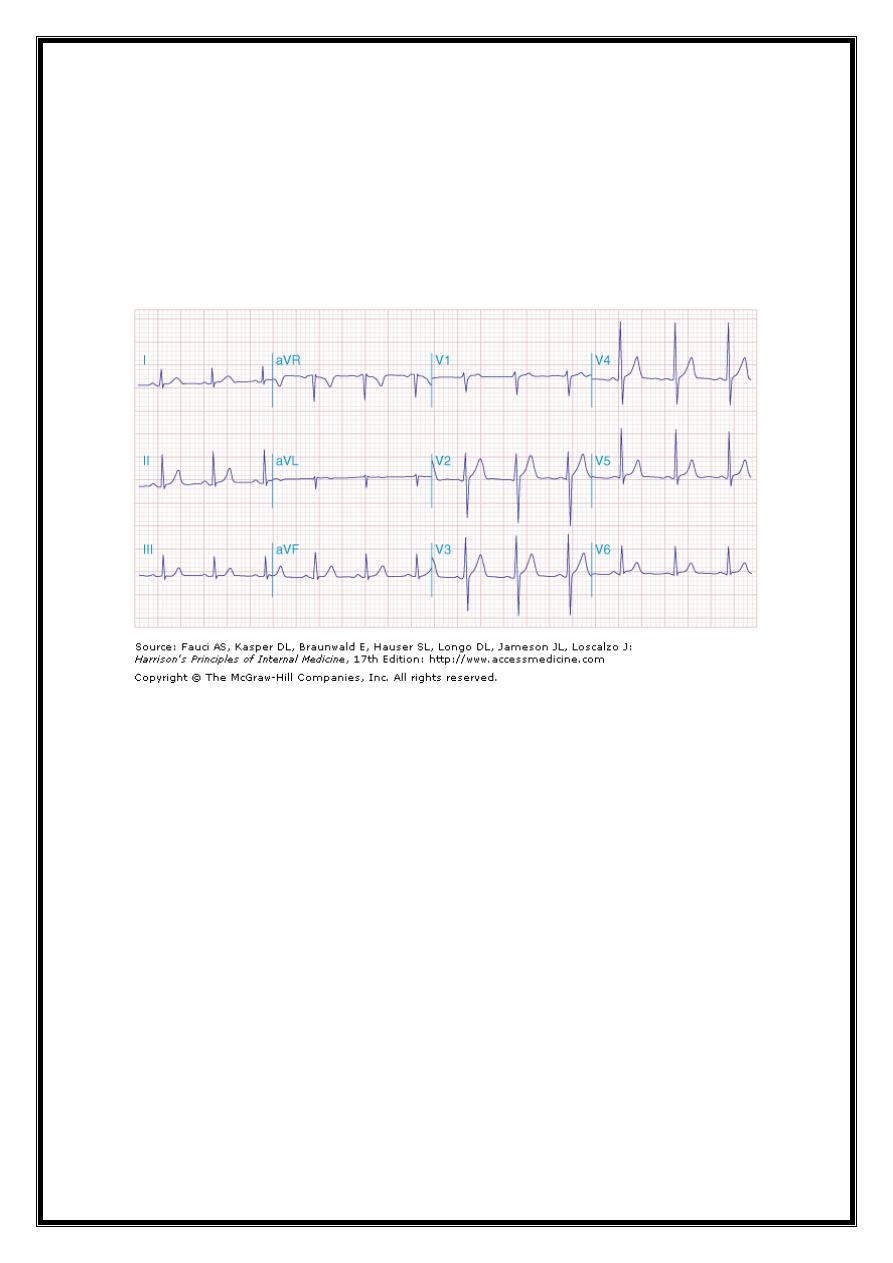
normal ECG
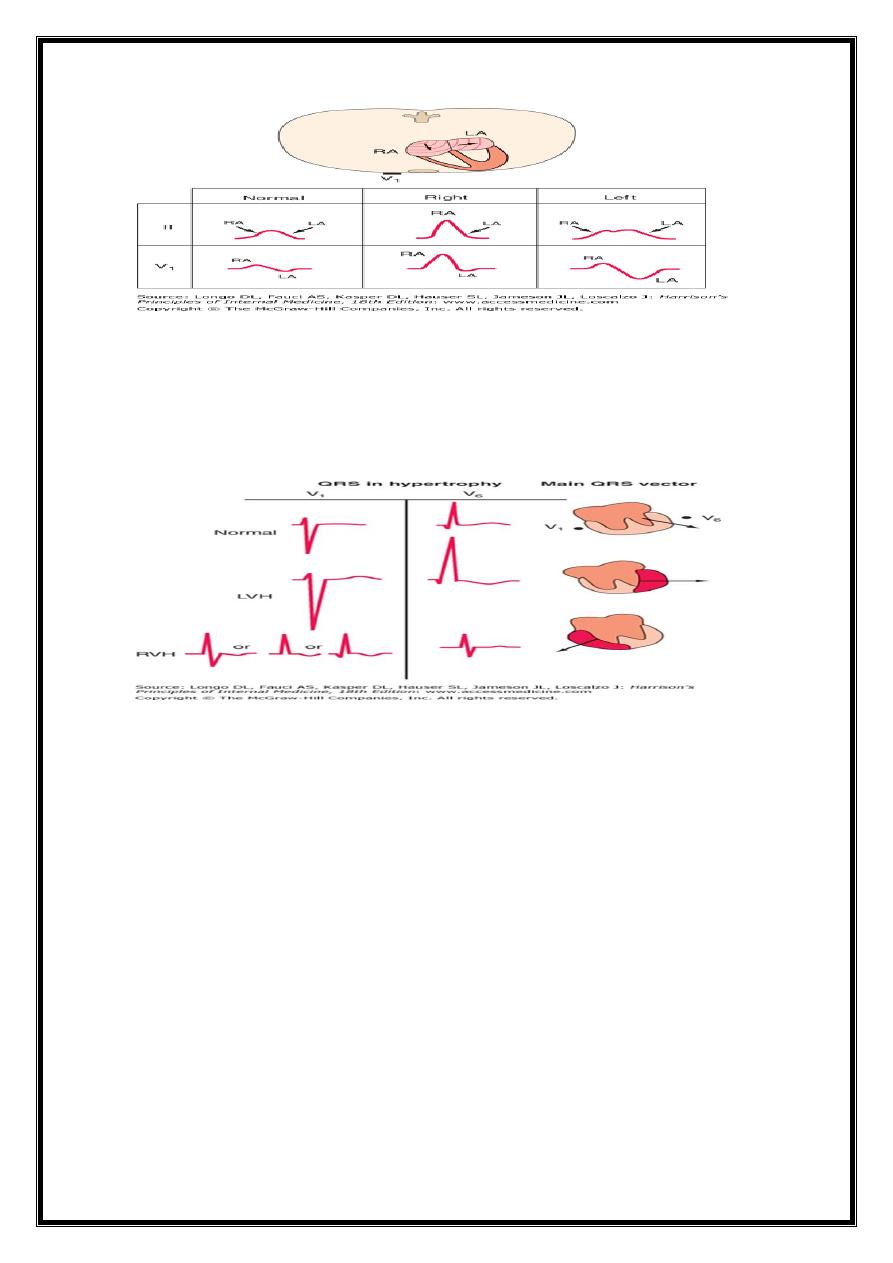
Cardiac Enlargement and Hypertrophy
Right A. overload (acute or chronic) ==> inc. P-wave amplitude ( 2.5 mm)
Left A. overload ==> biphasic P wave in V1 with a broad negative component or a broad
( 120 ms), (notched P wave in one or more limb leads)
left atrial conduction delays (in absence of actual atrial enlargement)==>LA
abnormality)
2
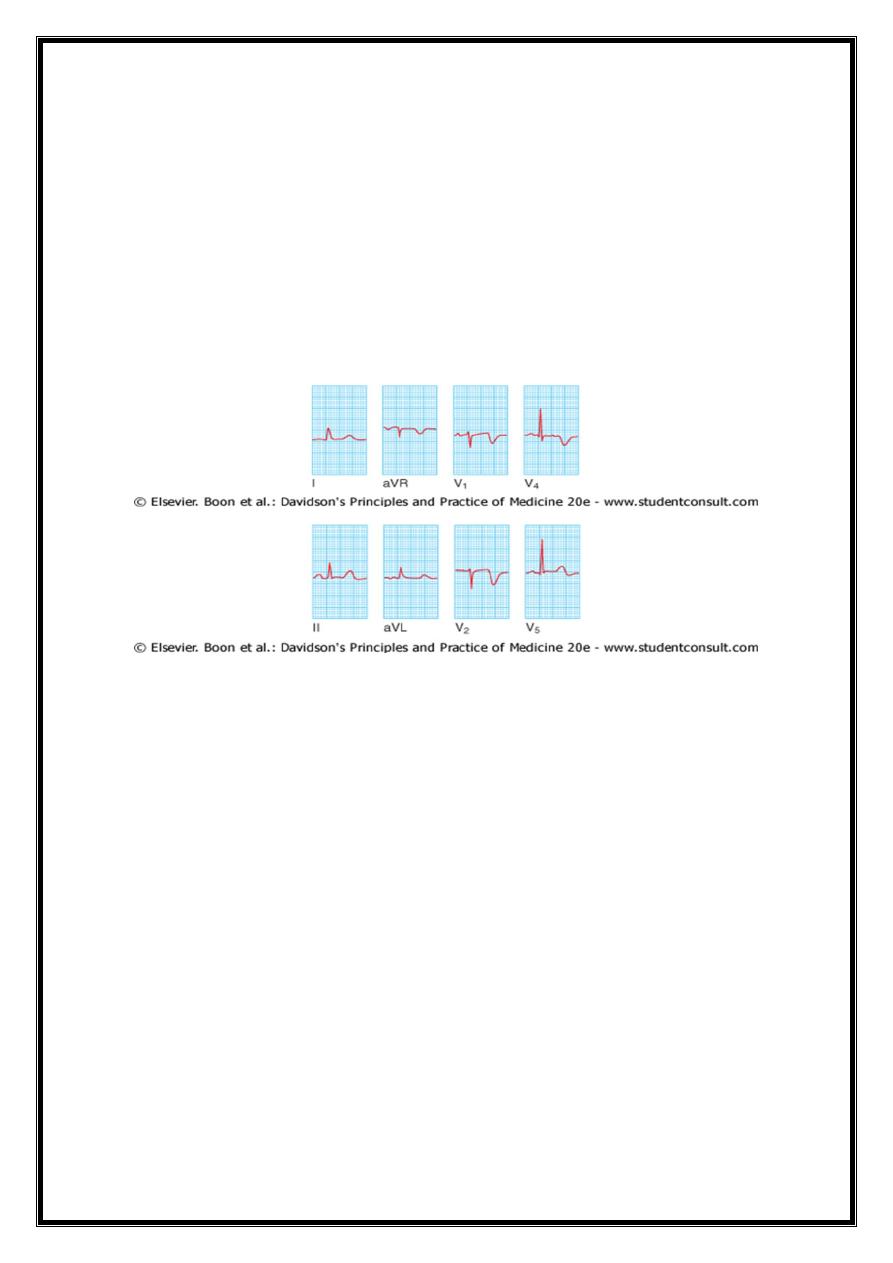
VENTRICLAR HYPERTROPHY
LVH=LV Leads(V5,V6,1,aVL)=Tall R
RV Leads(V1,V2)=Deep S (Strain pattern & LAD)
RVH=RV Leads(V1)=Tall R, Small initial slur notch or Q ( Strain pattern & RAD)
Right Ventricular hypertrophy
= pressure load (pulmonic v. stenosis or pulmonary a. hypertension) ==
relatively tall R wave in lead V1 (R versus S wave),(usually with Rs)
? qR pattern in V1 or V3R.
ST depression and T-wave inversion in right-to-midprecordial leads (right ventricular
"strain,“) =repol. ab. in acutely or ch. overloaded muscle
Prominent S waves may occur in left lateral precordial leads.
RVH =ostium secundum–ASD with the accompanying riRVght ventricular volume
overload=commonly associated with an incomplete or complete right bundle branch
block pattern with a rightward QRS axis.
3
left ventricular hypertrophy
LVH voltage criteria = tall left precordial R waves and deep right precordial S waves [SV1
+ (RV5 or RV6) >35 mm].
Repolarization abnormalities (ST depression with T-wave inversions, (left ventricular
"strain" pattern) - in leads with prominent R waves.
prominent precordial voltages =normal variant, esp. athletic or young
LVH= increase limb lead voltage with or without increased precordial voltage (e.g., RaVL
+ SV3 >20 mm in women and >28 mm in men).
LVH often progresses to incomplete or complete LBBB.
sensitivity of conventional voltage criteria for LVH dec.obese &smokers
4
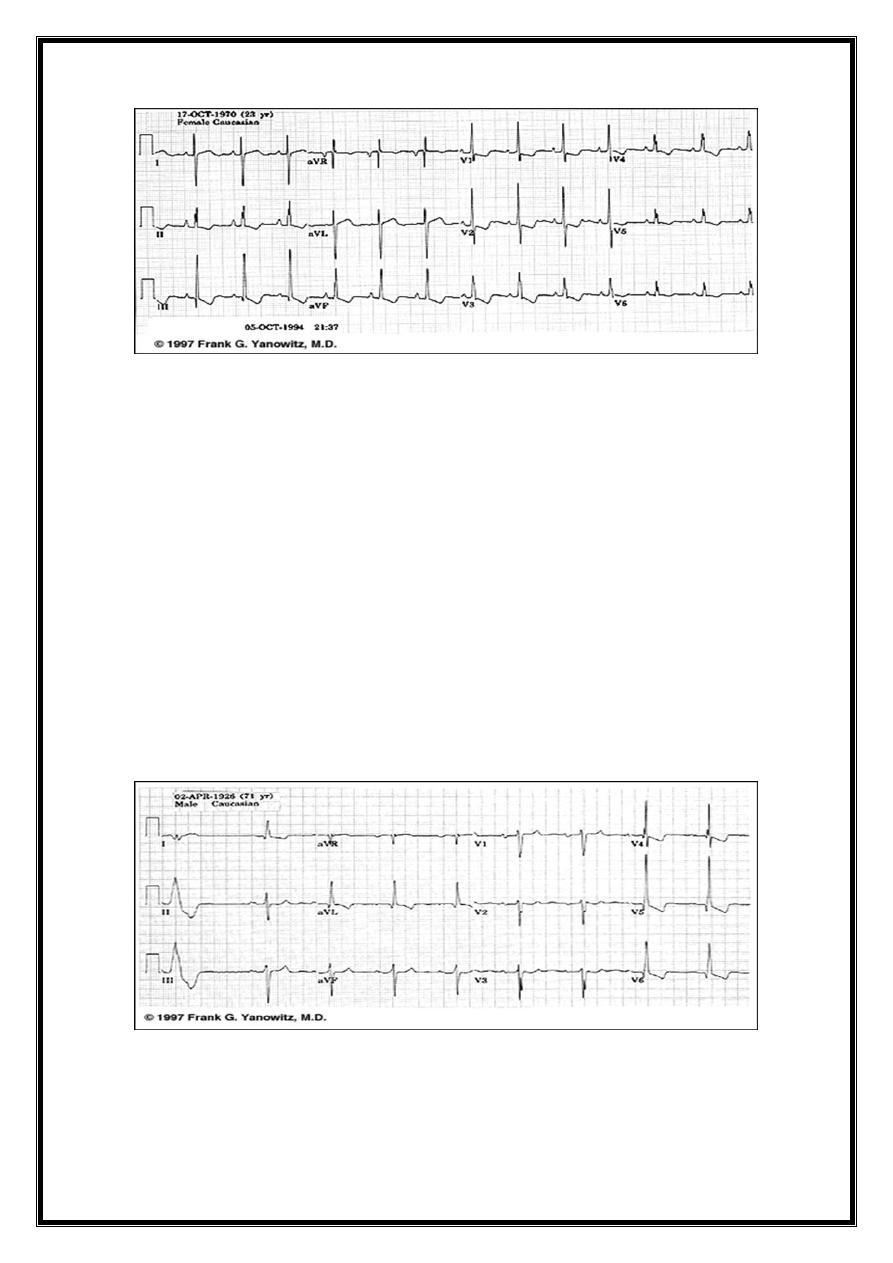
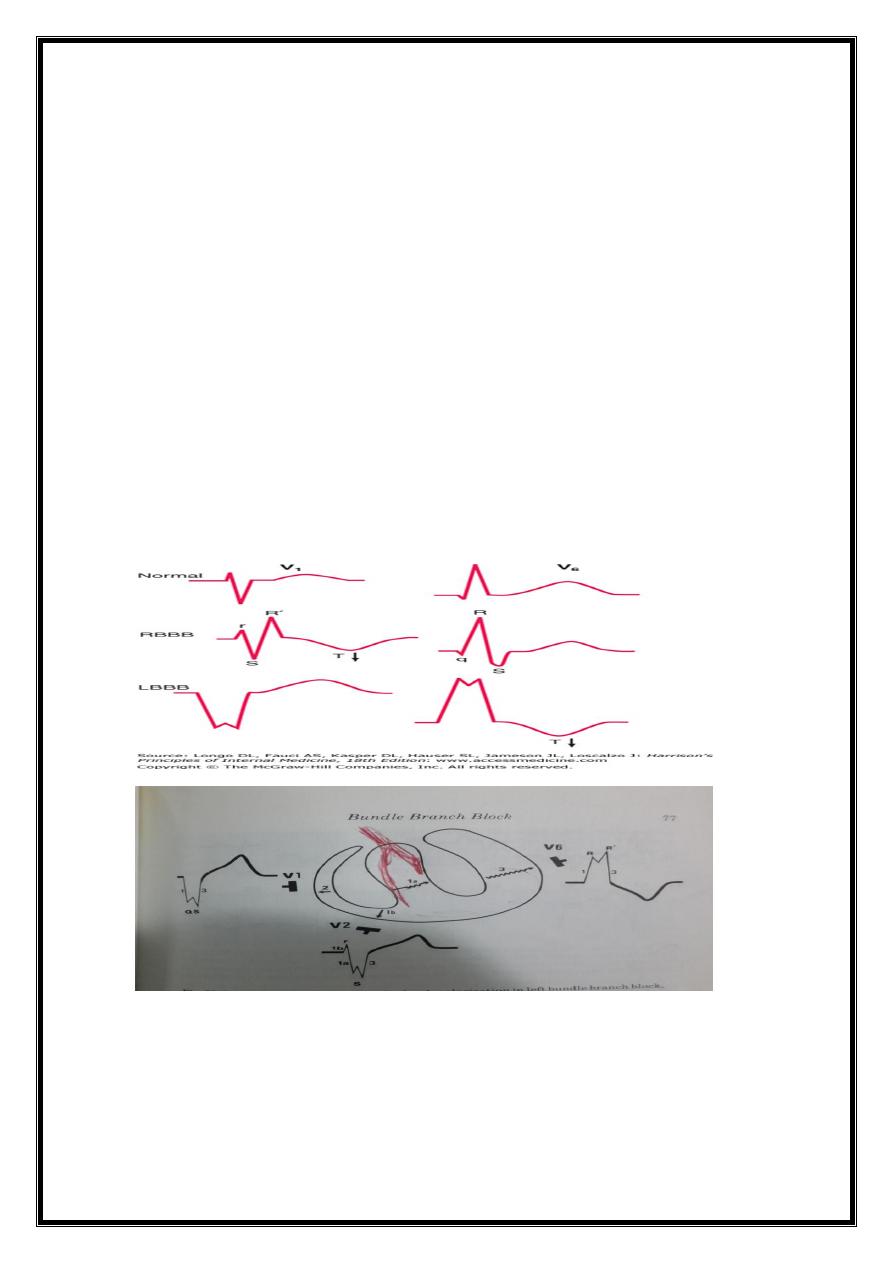
Bundle Branch Blocks
Intrinsic impairment of conduction in right or left B system (intraventricular conduction
disturbances) = prolongation of QRS interval.
complete bundle branch blocks, QRS interval >120 ms
incomplete blocks, QRS interval = 100 - 120 ms.
QRS vector= oriented in direction of myoc. region where depol.is delayed .
BBB affect ventricular depolarization (QRS) & characteristically associated with
secondary repolarization (ST-T) abnormalities.
T wave typically opposite in polarity to the last deflection of the QRS .
(altered sequence of repolarization -secondary to altered depolarization).
(Cf. primary repolarization abnormalities -Ischemia, electrolyte imbalance, and drugs
such as digitalis all cause such primary ST–T-wave changes).
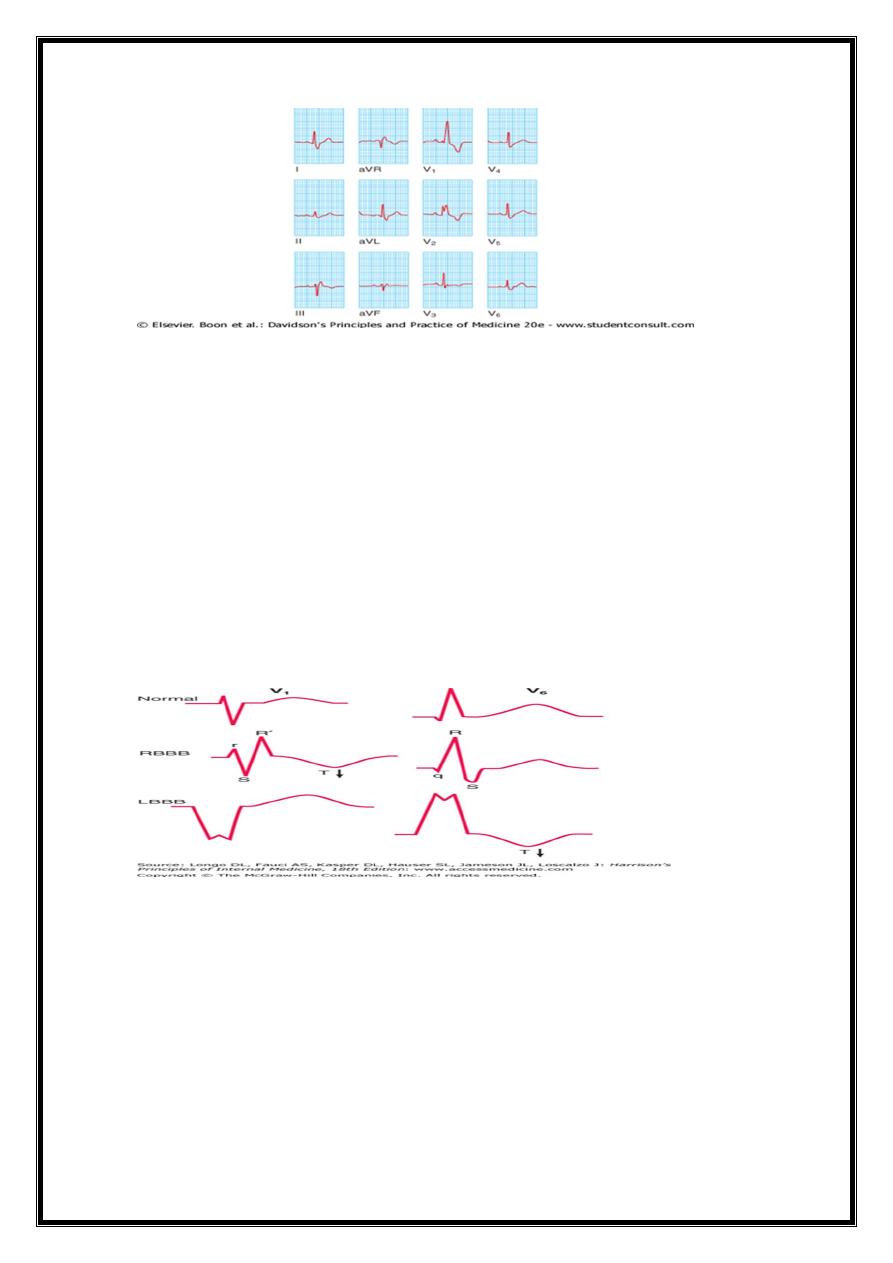
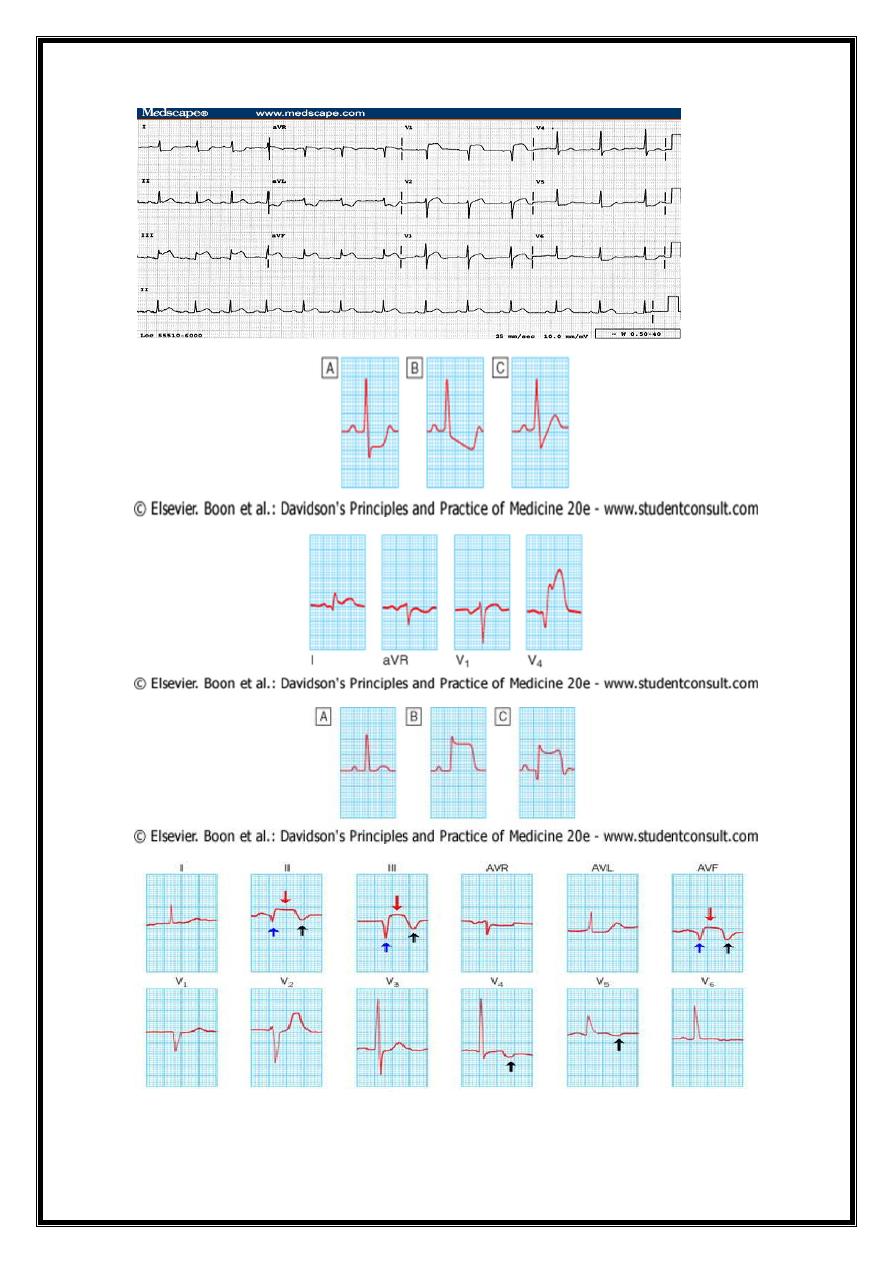
LBBB
Normal early left-to-right pattern of septal activation disrupted =septal depolarization
proceeds from right to left as well.
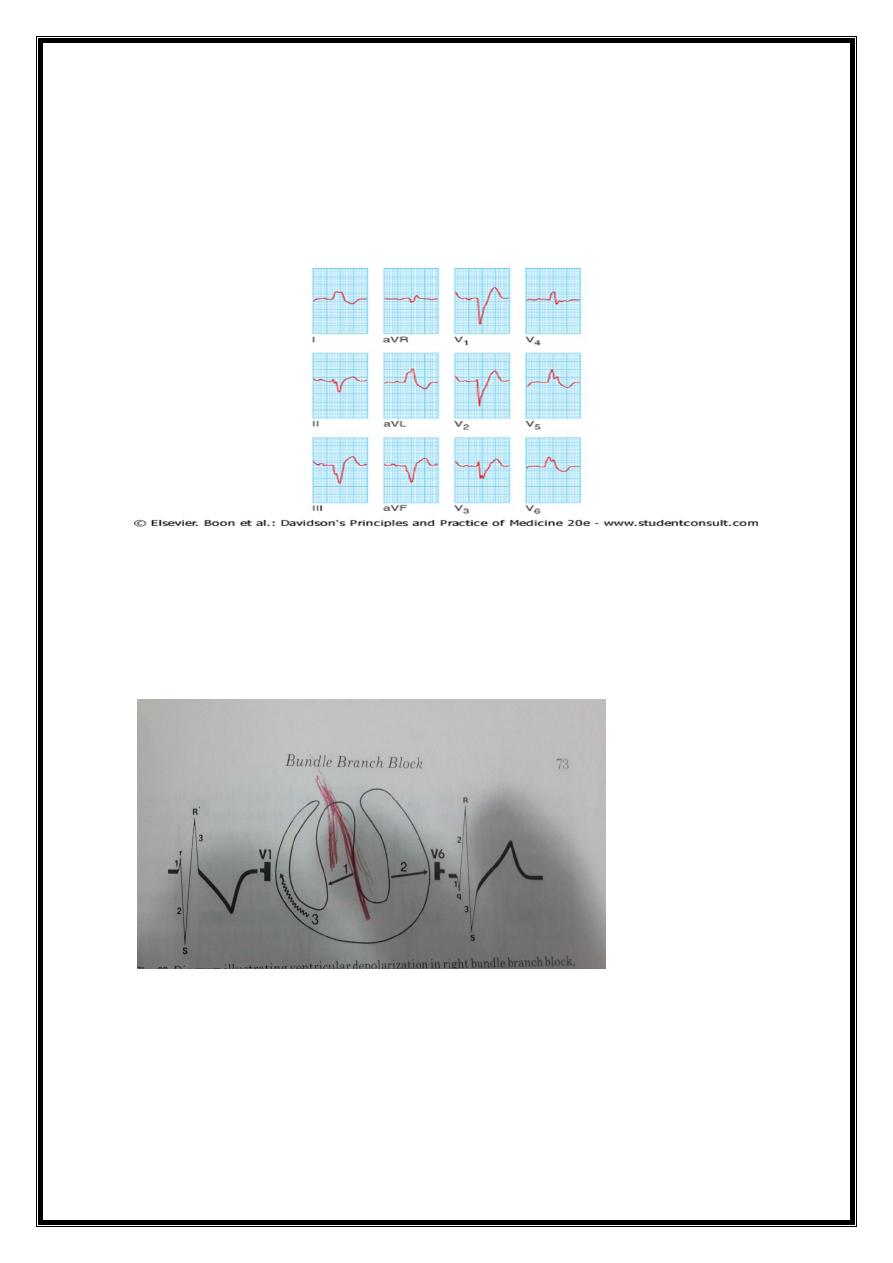
5
LBBB alters both early and later phases of v. depol.major QRS vector is directed to the
left and posteriorly
=wide, predominantly negative (QS) complexes in lead V1 and entirely positive (R)
complexes in lead V6.
CAD,HHD,AVD,CMP.RV pacing
RBBB
Right bundle branch block=terminal part of dep.QRS vector oriented to right and
anteriorly (rSR' in V1 and qRS in V6, ).
subjects without structural heart dis., RBBB more common than LBBB.
heart disease, both congenital (e.g., atrial septal defect) and acquired (e.g., valvular,
ischemic)..
6
BUNDLE BRANCH BLOCK-SUMMARY
RBBB-- prolonged QRS> 0.12 sec.
RT.leads= rSR or M-shaped complex in V1,V2
LT.leads= broad &slurred S wave in V5,V6,1,AVL (ST&T opposite terminal QRS)
LBBB— prolonged QRS >0.12 sec.
LT. leads= V5,V6,AVL,1
wide notched M-shaped or plateau- shaped QRS
wide notched R or R-R
RT.leads =V1 wide notched QS(ST & T opposite
terminal QRS
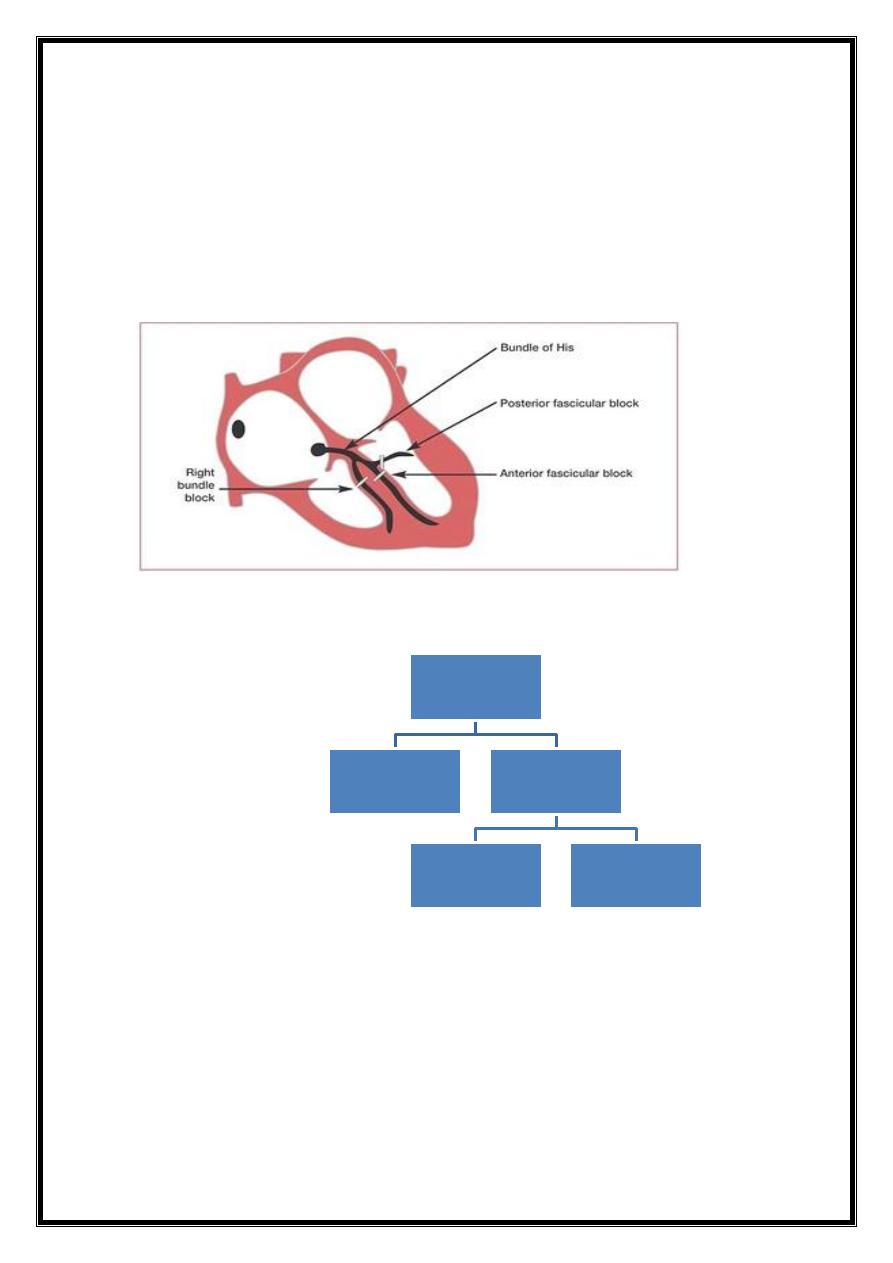
Partial blocks (fascicular or "hemiblocks")
left anterior or posterior fascicular blocks) = do not prolong the QRS duration
shifts in frontal plane QRS axis (leftward or rightward, respectively).
bifascicular block =
RBBB + left posterior fascicular block
RBBB+left anterior fascicular block
complete left bundle branch block.
7
trifascicular disease =
prolonged PR interval + bifascicular block
DIFF.DIAG.OF Prolongation of QRS duration
1- conduction delay
2-preexcitation of the ventricles via a bypass tract- Wolff-Parkinson-White (WPW)
patterns .
CAD
ANGINA-STABLE
STABLE PLAQUE
ACUTE
C.SYNDROME
VULNARABLE
PLAQUE
ST-ELEVATION MI
NON-ST-
ELEVATION MI
UNSTABLE ANGINA
8
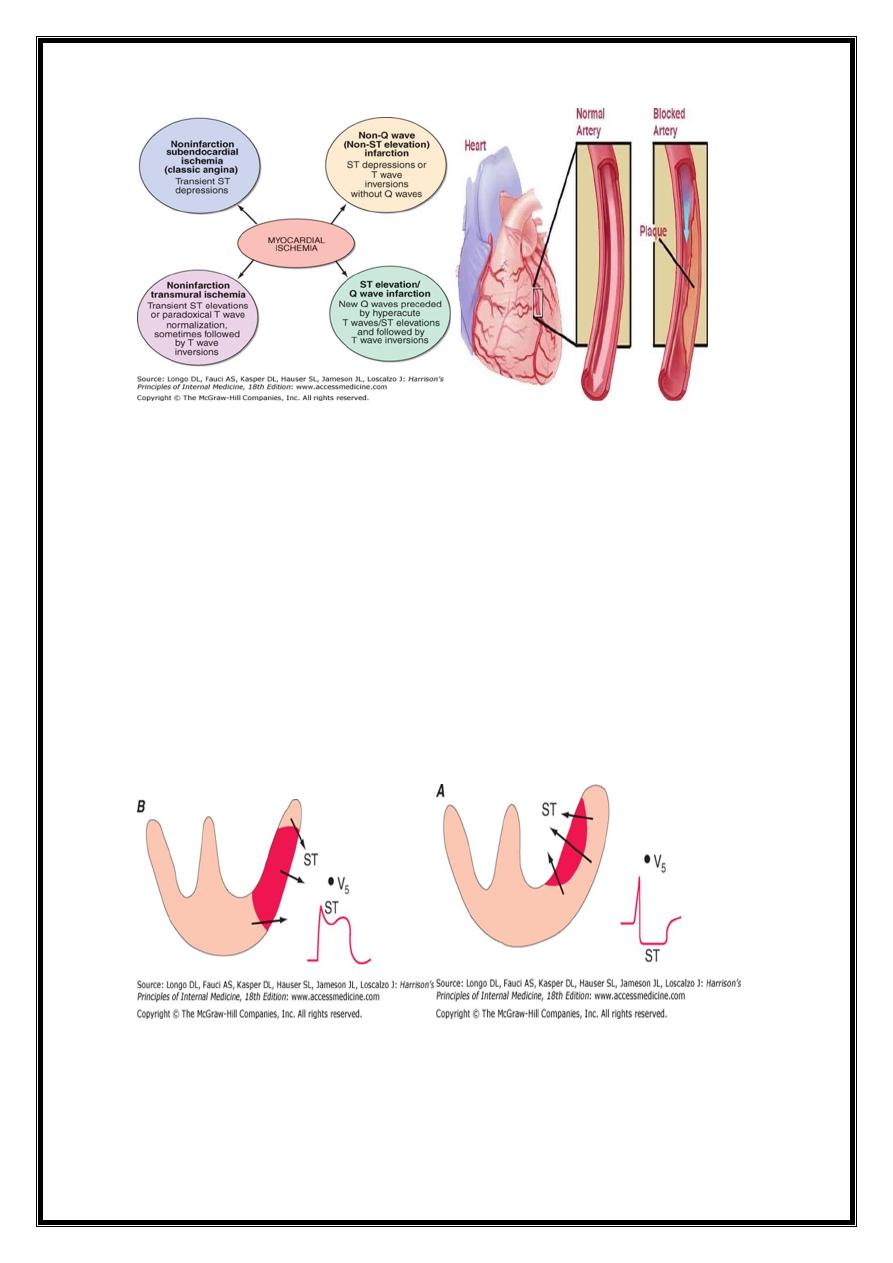
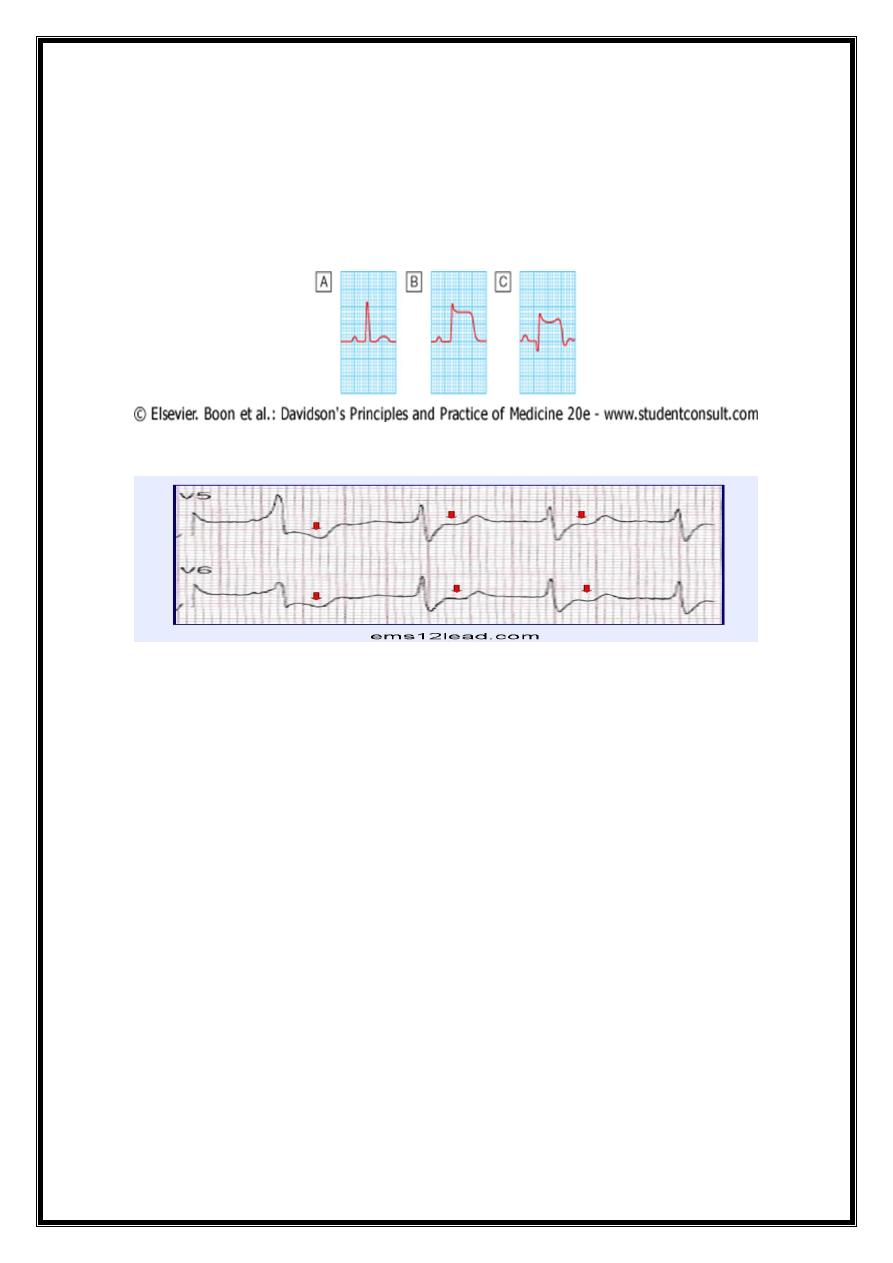
Changes of ST Segment
Severe, acute ischemia lowers resting membrane potential and shortens duration of
action potential==> voltage gradient between normal and ischemic zones= current flows
between those regions.
currents of injury =deviation of the ST segment .
1-acute ischemia is transmural ST vector shifted in direction of outer (epicardial)
layers==>ST elevations (sometimes, in earliest stages of ischemia, tall, positive s=
hyperacute T waves o).
2- ischemia confined primarily to subendocardium ST vector typically shifts toward
subendocardium and ventricular cavityST-segment depression (with ST elevation in
lead aVR).
9
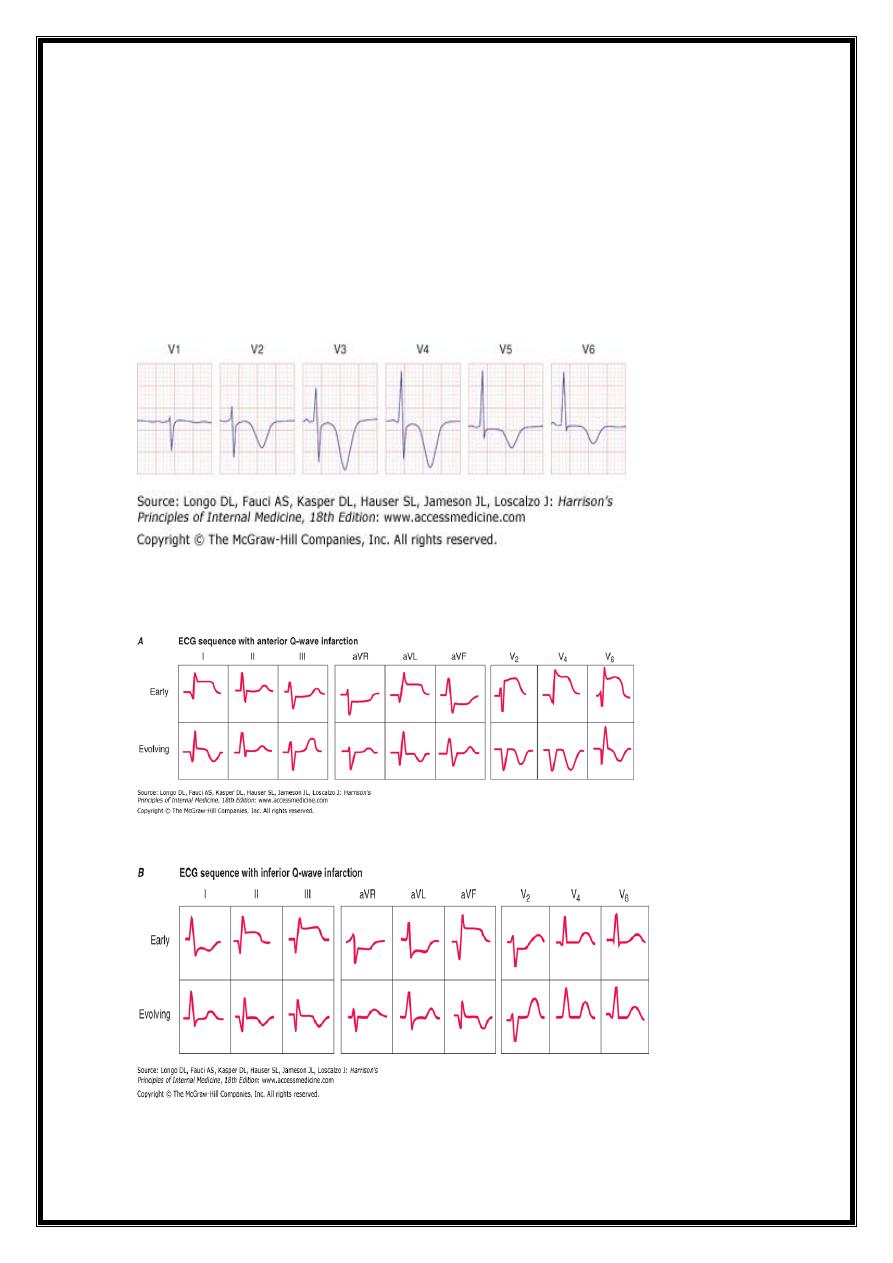
ECG IN MYOCARDIAL INFARCTION
1-ST-ELEVATION-TRANSMURAL,Q-WAVE
tall wide T,slope-elevation ST(later-coved,elevated)
pathological Q.inverted symmetrical T
Localization
ST Elevation
ECG leads helpful in localizing regions of ST elevation than non-ST elevation ischemia.
E.g.,
1-acute transmural anterior (including apical and lateral) wall ischemia =
ST elevations or increased T-wave positivity in one or more of the precordial leads (V1–V6)
and leads I and aVL.
2- Inferior wall ischemia produces
changes in leads II, III, and aVF.
3-"Posterior" wall ischemia (usually associated with lateral or inferior involvement)
=indirectly recognized by reciprocal ST depressions in leads V1 to V3 (=ST elevation
"equivalent" acute coronary syndrome).
4- Right ventricular ischemia =
ST elevations in right-sided chest leads ..
11
T inversion
ischemic chest pain +deep T-wave inversions in multiple precordial leads (e.g., V1–V4)
with or without cardiac enzyme elevations =
typically have severe obstruction in left anterior descending CA system .
baseline ECG already shows abnormal T-wave inversions may develop T-wave normalization
(pseudonormalization) during episodes of acute transmural ischemia.
11
12
ANGINA PECTORIS
1-CLASSIC ANGINA =
TRANSIENT SUBENDOCRDIAL INJURY
DEPRESSION OF ST SEGMENT
2-VARIENT ANGINA =
TRANSIENT SUBPERICARDIAL INJURY=
ST ELEVATION(TRANSIENT) AND TALL WIDENED T
Metabolic Factors and Drug Effects
metabolic and pharmacologic agents alter the ECG esp. changes in repolarization (ST-T-
U) and sometimes QRS prolongation.
Hyperkalemia = sequence of changes –
1-narrowing and peaking (tenting) of the T waves.
2-Further elevation of extracellular K+ ==> AV conduction disturbances, diminution in P-
wave amplitude, and widening of the QRS interval.
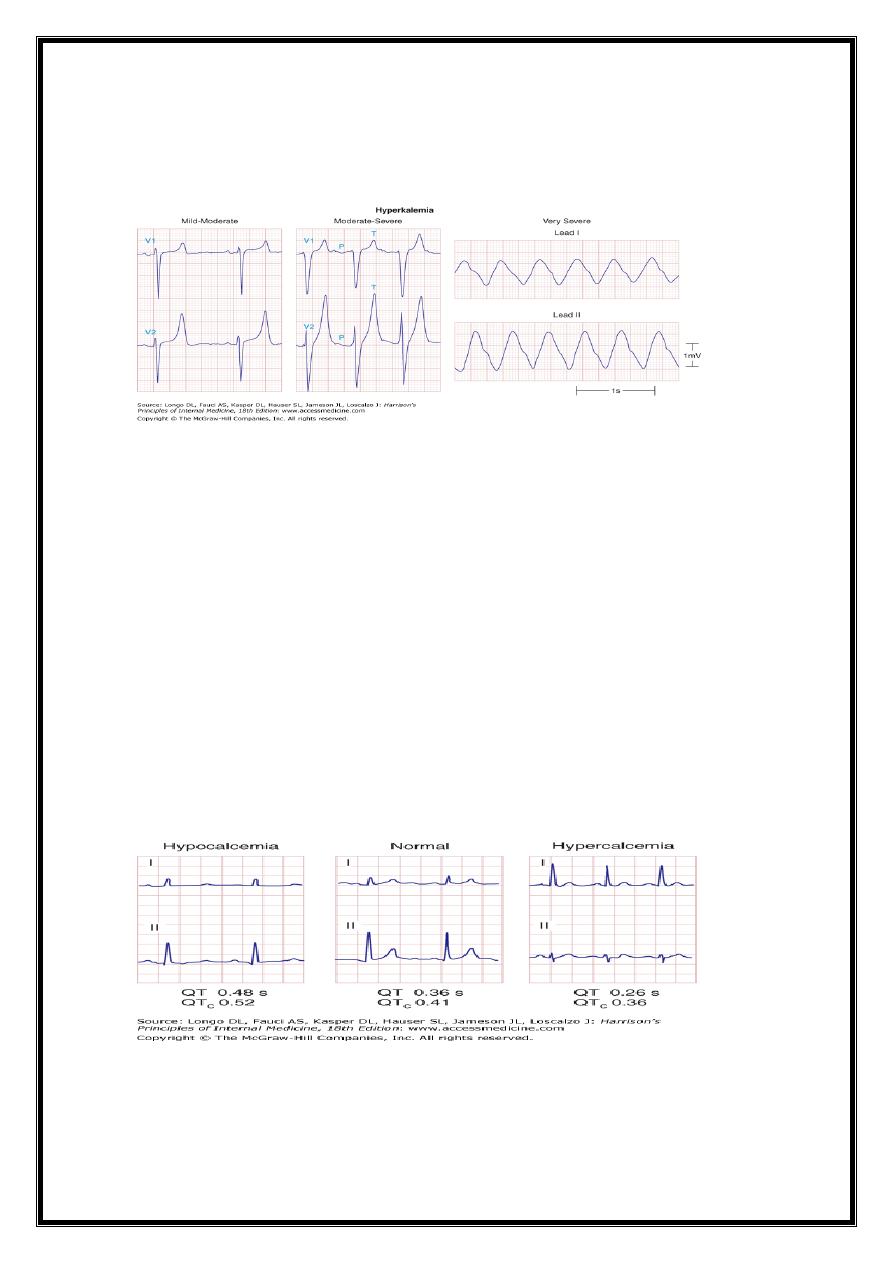
13
3-Severe hyperkalemia eventually causes cardiac arrest with a slow sinusoidal type of
mechanism ("sine-wave" pattern) followed by asystole.
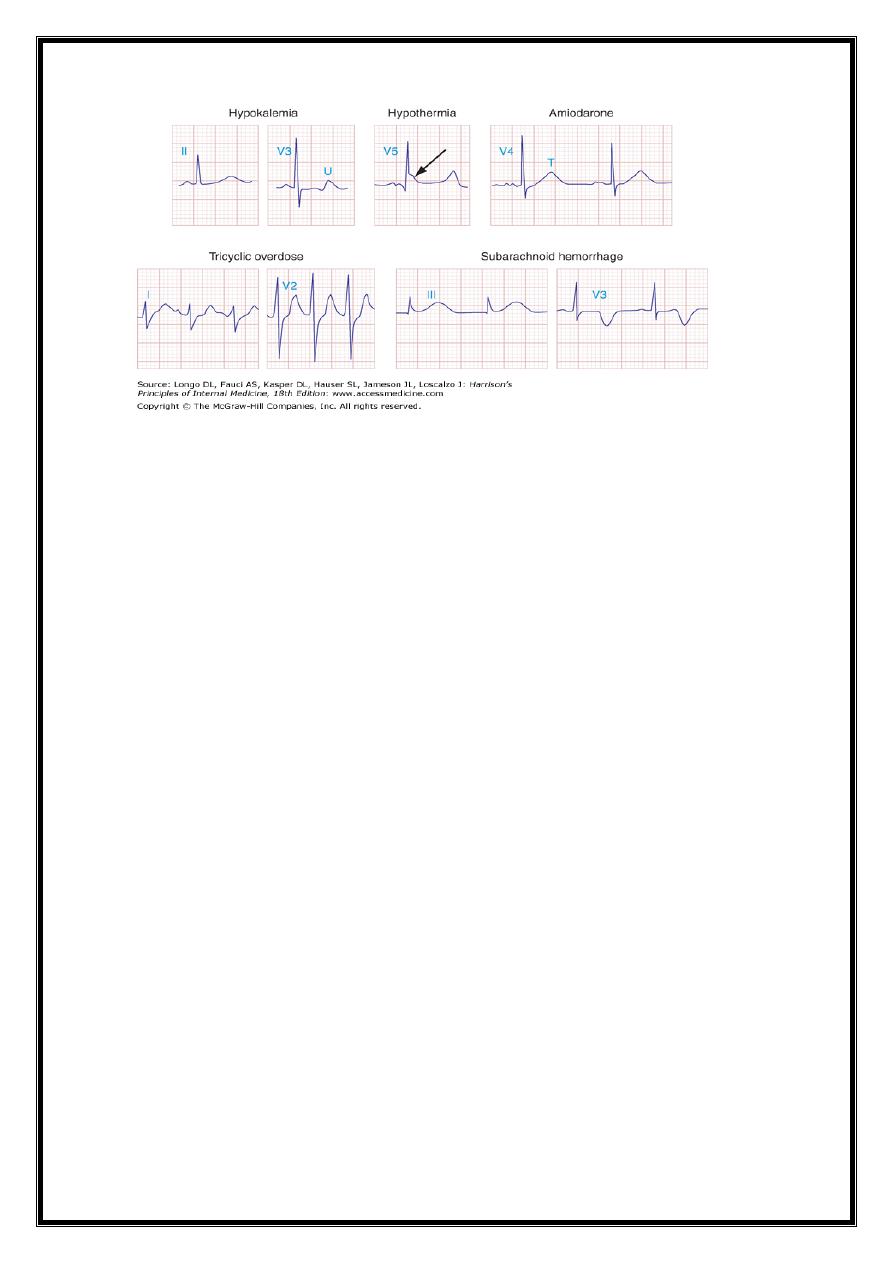
Hypokalemia prolongs ventricular repolarization=prominent U waves.
Prolongation of the QT interval -drugs that increase duration of ventricular AP: class 1A
antiarrhythmic agents and related drugs (e.g., quinidine, disopyramide, procainamide,
tricyclic antidepressants, phenothiazines) and class III agents [e.g., amiodarone ,
dofetilide, dronedarone, sotalol, ibutilide].
Marked QT prolongation, sometimes with deep, wide T-wave inversions, =intracranial
bleeds, esp. subarachnoid hemorrhage ("CVA T-wave" pattern)
Systemic hypothermia = prolongs repolarization, usually with a distinctive convex
elevation of the J point (Osborn wave).
Hypocalcemia = prolongs QT interval (ST portion)
hypercalcemia =shortens QT
Digitalis glycosides = shorten the QT interval, often with a characteristic "scooping" of
the ST–T-wave complex (digitalis effect).
14
ARRHYTHMIAS
A-ACCORDING TO HAERT RATE:
1- TACHYARRHYTHMIAS
2-BRADYARRHYTHMIAS
B-ACCORDING TO THE SITE OF ORIGIN
1-SINUS
2-ATRIAL
3-AV JUNCTIONAL(NODAL)
4-VENTRICULAR
SUPRAVENTRICULAR
ATRIAL-
ECTOPIC
ATRIAL TACHYCARDIA
ATRIAL FLUTTER
ATRIAL FIBRILLATION
JUNCTIONAL/AV NODAL –
ECTOPIC
-TACHYCARDIA-SVT
15
VENTRICULAR –
ECTOPIC
-TACHYCARDIA
-FIBRILLATION
-Flutter
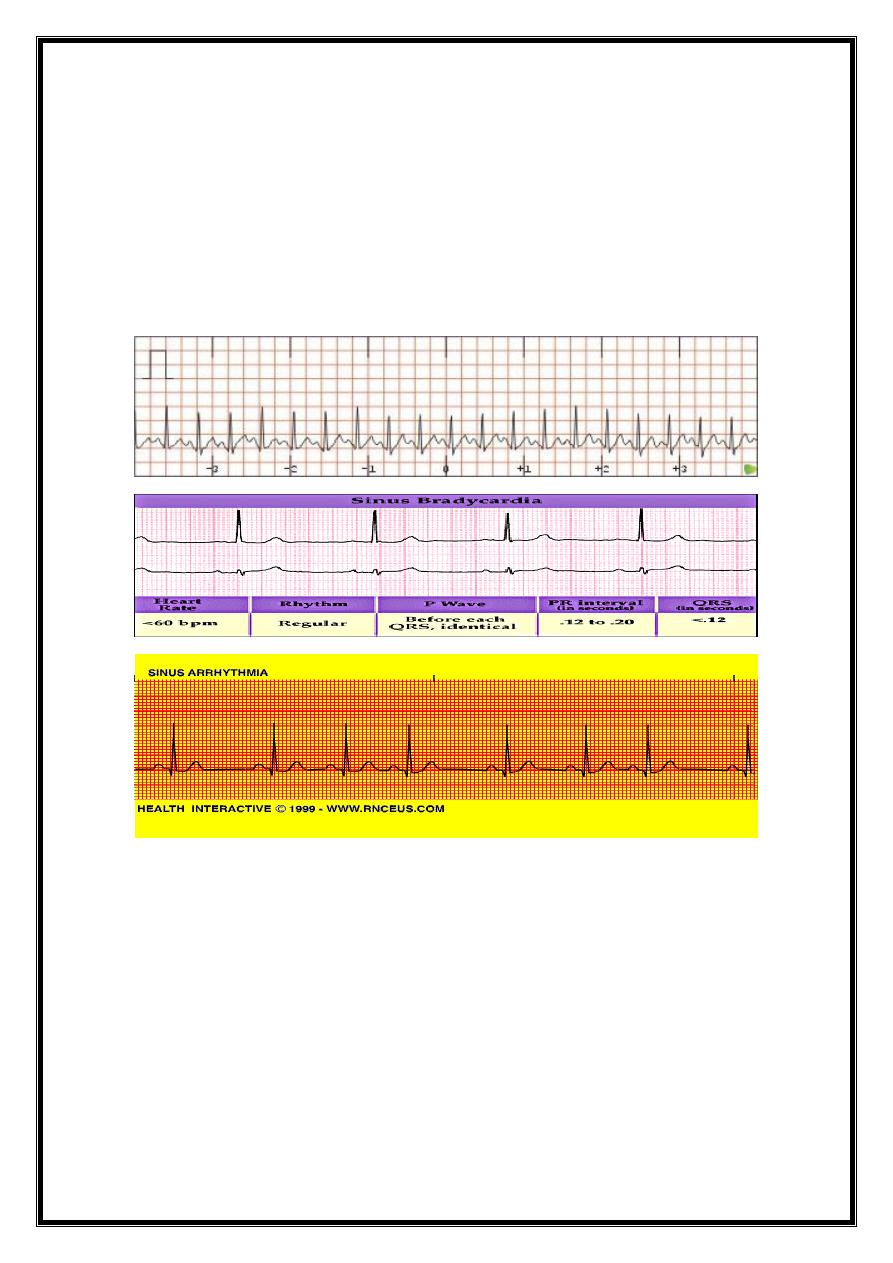
Sinus Rhythms
TACHYARRHYTHMIAS
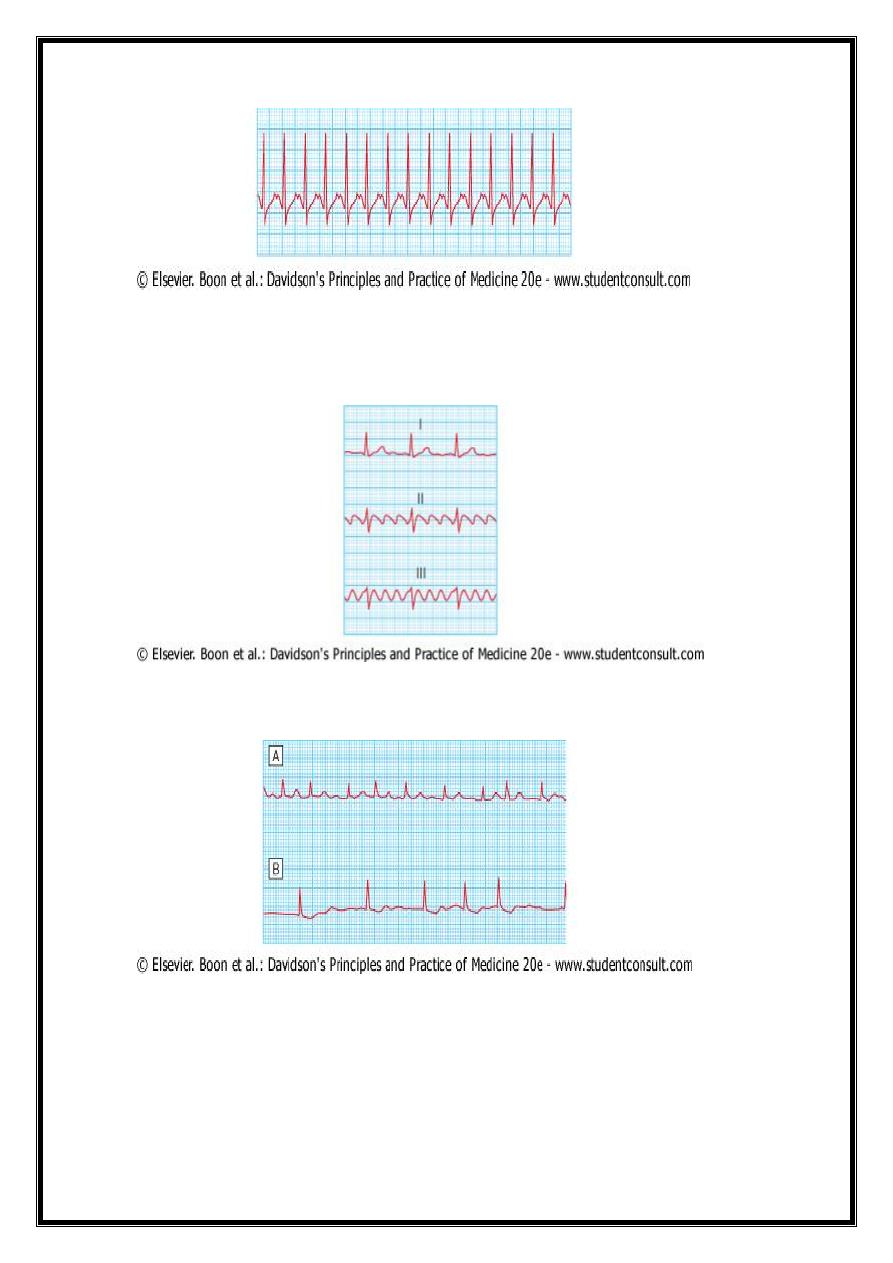
1-ATRIAL= AT.AF.Af
2-JUNCTIONAL(AV-NODAL)=
av nodal dual reentry
typical-anti slow,retro fast
atypical-
a-v accessory reentrant(bypass)
concealed-ortho (in av node)
16
manifest-anti
3-VENTRICULAR= VT.VFL.VF
Main ECG Changes in different types of arrhythmia
1- 'supraventricular' (sinus, atrial or junctional) = Supraventricular rhythms
narrow QRS complexes (ventricles depolarised normally through the AV node and
bundle of His).
2- ventricular:=
broad bizarre QRS complexes (ventricles activated abnormal sequence).
occasionally a supraventricular rhythm can produce broad or wide QRS complexes due to
coexisting bundle branch block or the presence of accessory conducting tissue
Atrial & Ventricular ectopic
ATRIAL(spraventricular ) tachycardias-reg.narrow QRS
17
rapid regular with block (undulating,regular,closely spaced relat.wide deflect.f-
wavesreg.corrugated saw-tooth appearance
(400-600)-disorganised and chaotic-ragged baseline + numerous round or spiked
waves(chronic-low amplitude
18
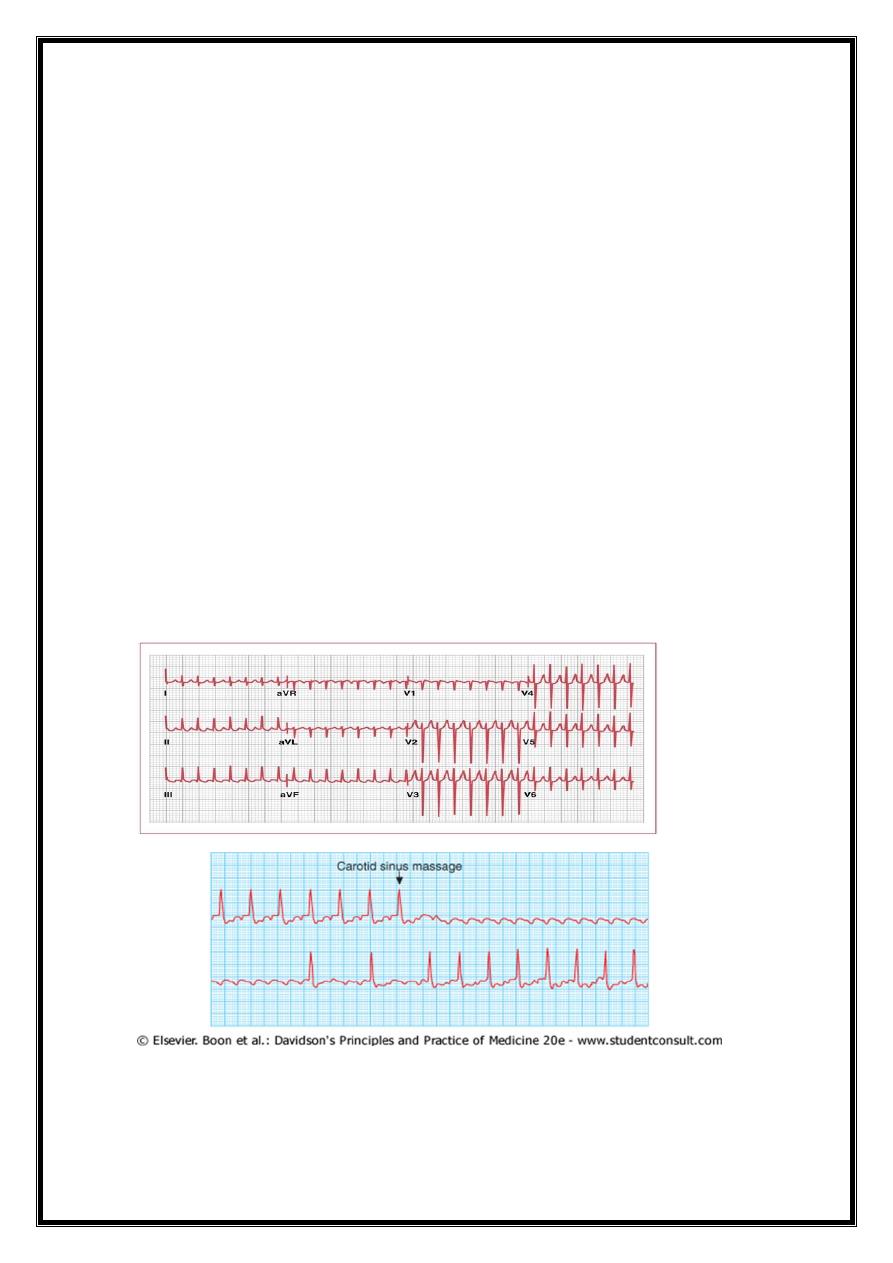
1-ATRIOVENTRICULAR NODAL REENTRANT TACHYCARDIA (AVNRT
Re-entry in circuit involving AV node &its two right atrial input pathways
superior fast pathway and inferior slow pathway ==>
regular tachycardia with a rate of 140-220/min.
tends to occur in hearts that are otherwise normal,
episodes may last from a few seconds to many hours.
Clinically=
patient is usually aware of a fast heart beat
may feel faint or breathless.
Polyuria, release of atrial natriuretic peptide, sometimes
cardiac pain or heart failure (if there is coexisting structural heart disease.)
ECG =
tachycardia with normal QRS complexes
( occasionally there may be rate-dependent BBB
2-ATRIOVENTRICULAR RE-ENTRANT TACHYCARDIA (AVRT) AND WOLFF-PARKINSON-
WHITE SYNDROME
ANOMALOUS TISSUE (accessory ,bypass) Macroreentrant
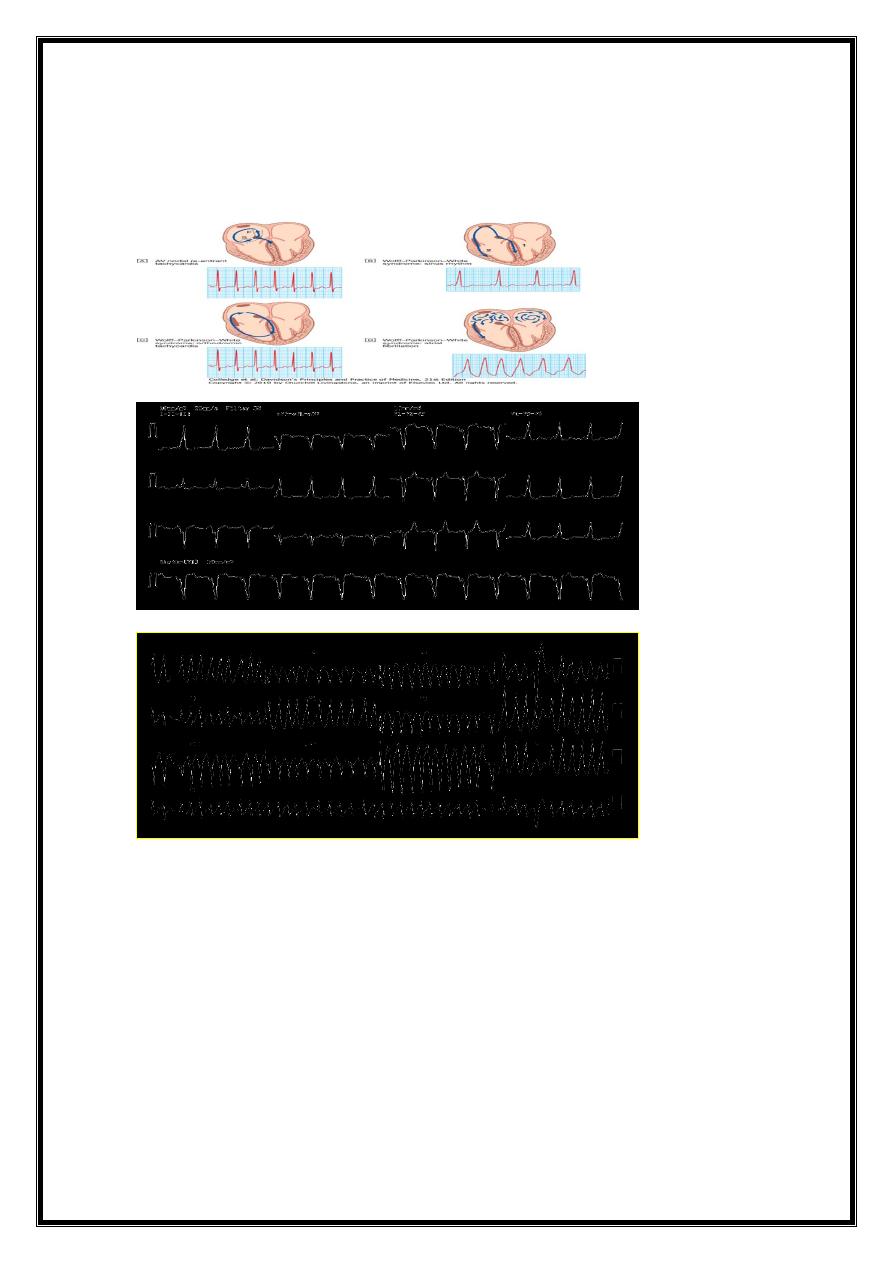
19
1-sinus rhythm
2-supraventricular
3-atrial fibrillation & flutter (no av drug
VENTRICULAR TACHYARRHYTHMIAS
V.ECTOPICS
V.TACHYCARDIA
V.FLUTTER
V.FIBRILLATION
IDIOVENTRICULAR RHYTHM
21
VE & VE FUSION BEATS
21
bradyarrthmia
1-ATRIOVENTRICULAR BLOCK
=1
st
.degree
=2
nd
.degree
type 1
type 2
=3
rd
.degree
2-BUNDLE BRANCH BLOCK
= RIGHT BBB
LEFT BB
complete
incomplete-fascicular
2-ATRIOVENTRICULAR (AV) BLOCK
Atrioventricular conduction influenced by autonomic activity.
AV block = intermittent and may only be evident when the conducting tissue is stressed
by a rapid atrial rate==>
atrial tachyarrhythmias are often associated with AV block ,
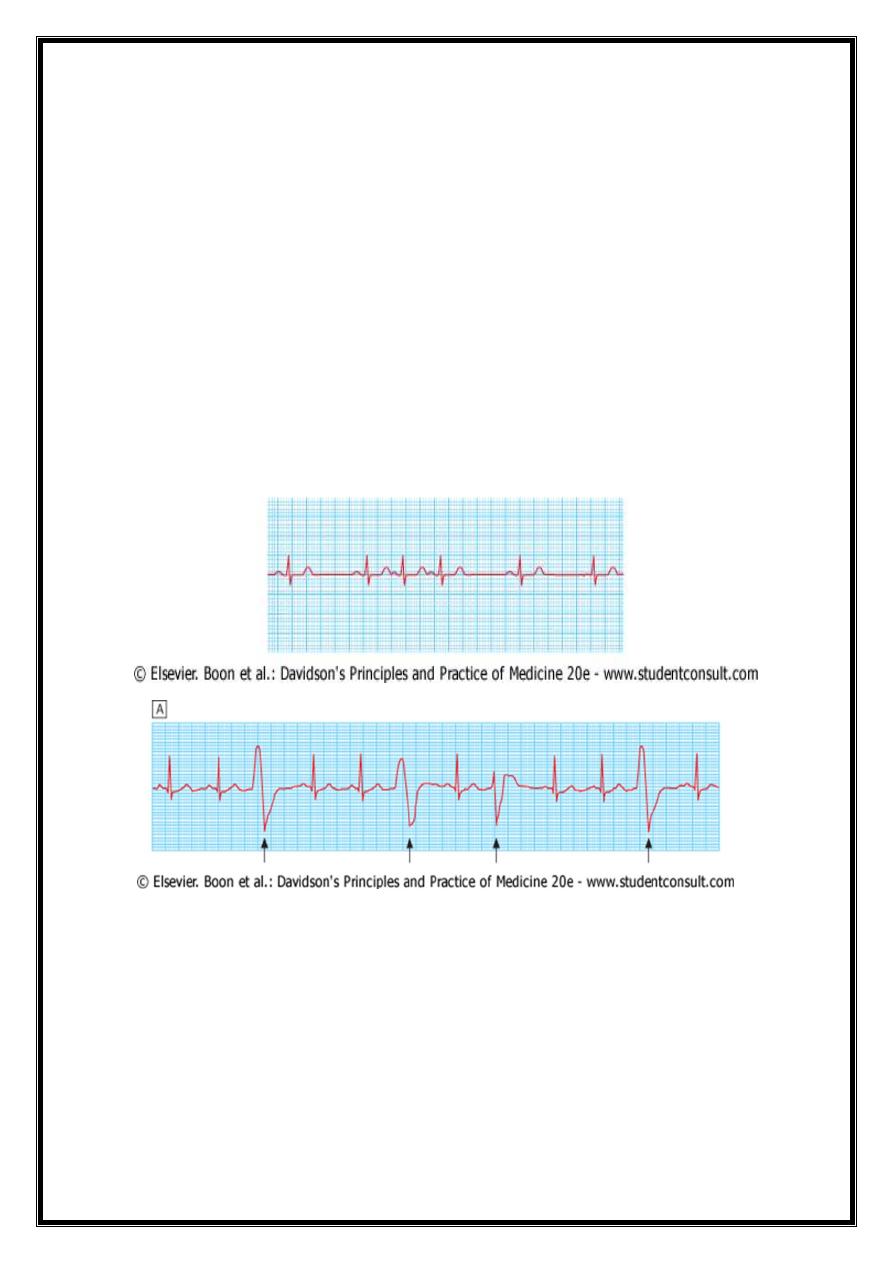
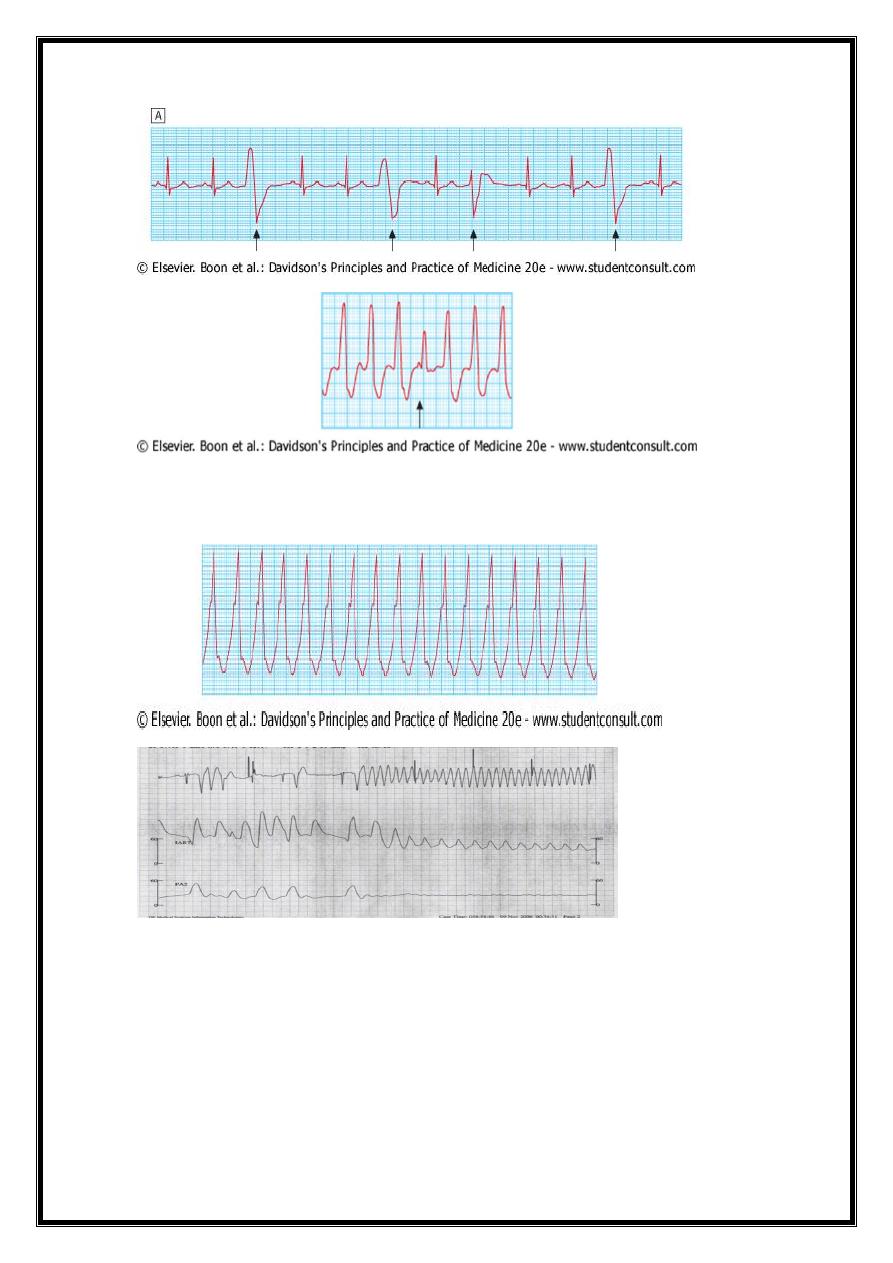
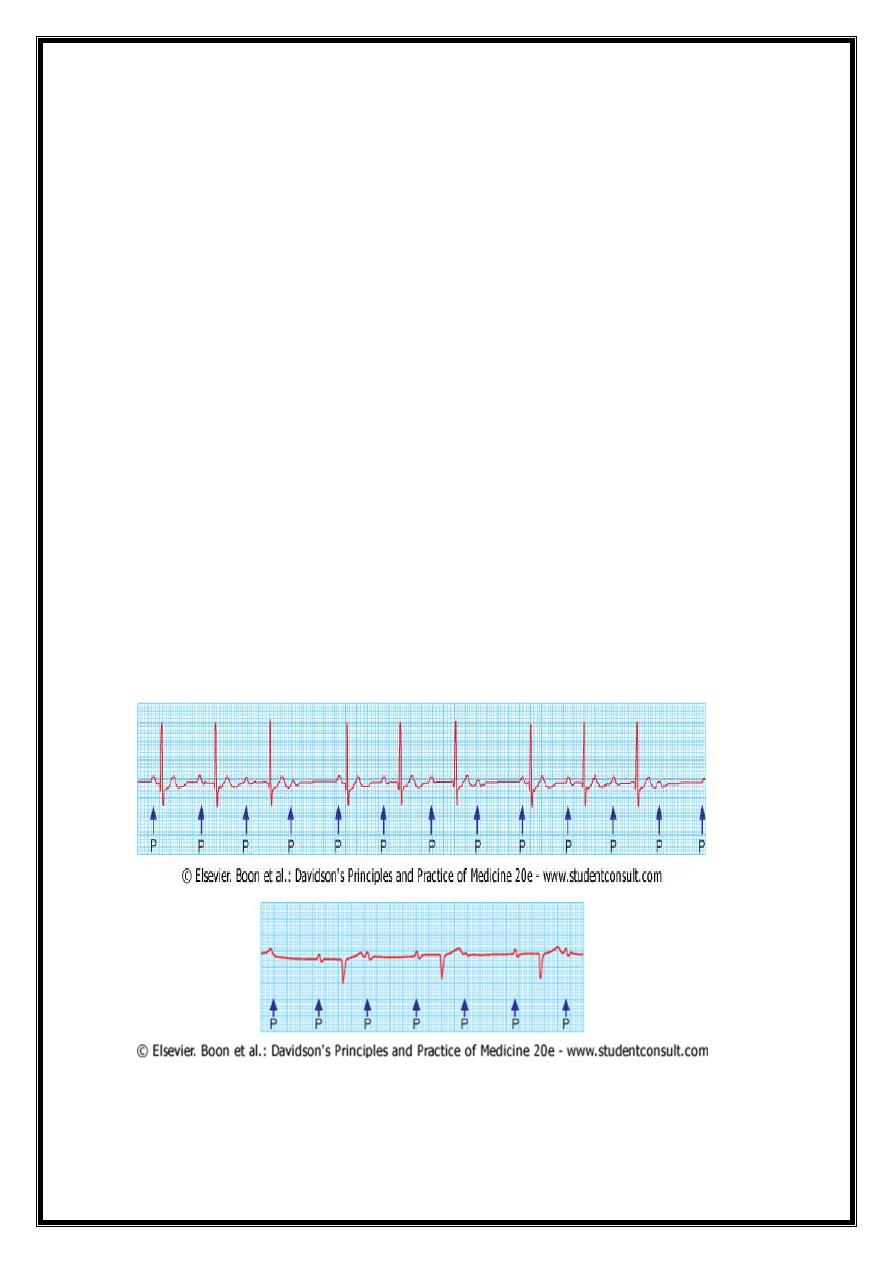
First-degree AV block
AV conduction is delayed
PR interval - prolonged (> 0.20 seconds) .
rarely causes symptoms
22
Second-degree AV block
some impulses from t atria fail to conduct to ventricles==> dropped beats
1-Mobitz type I second-degree AV block =
progressive lengthening of successive PR intervals = dropped beat.
cycle then repeats itself= Wenckebach's phenomenon –
impaired conduction in the AV node itself.
- physiological
-at rest or during sleep in athletic young adults with high vagal tone.
2-Mobitz type II second-degree AV block =
PR interval of conducted impulses remains constant but some P waves are not
conducted.
caused by disease of the His-Purkinje system
carries a risk of asystole.
In 2:1 AV block =,alternate P waves are conducted
(impossible to distinguish between Mobitz type I and type II block)
Third-degree (complete) AV block
- AV conduction fails completely,
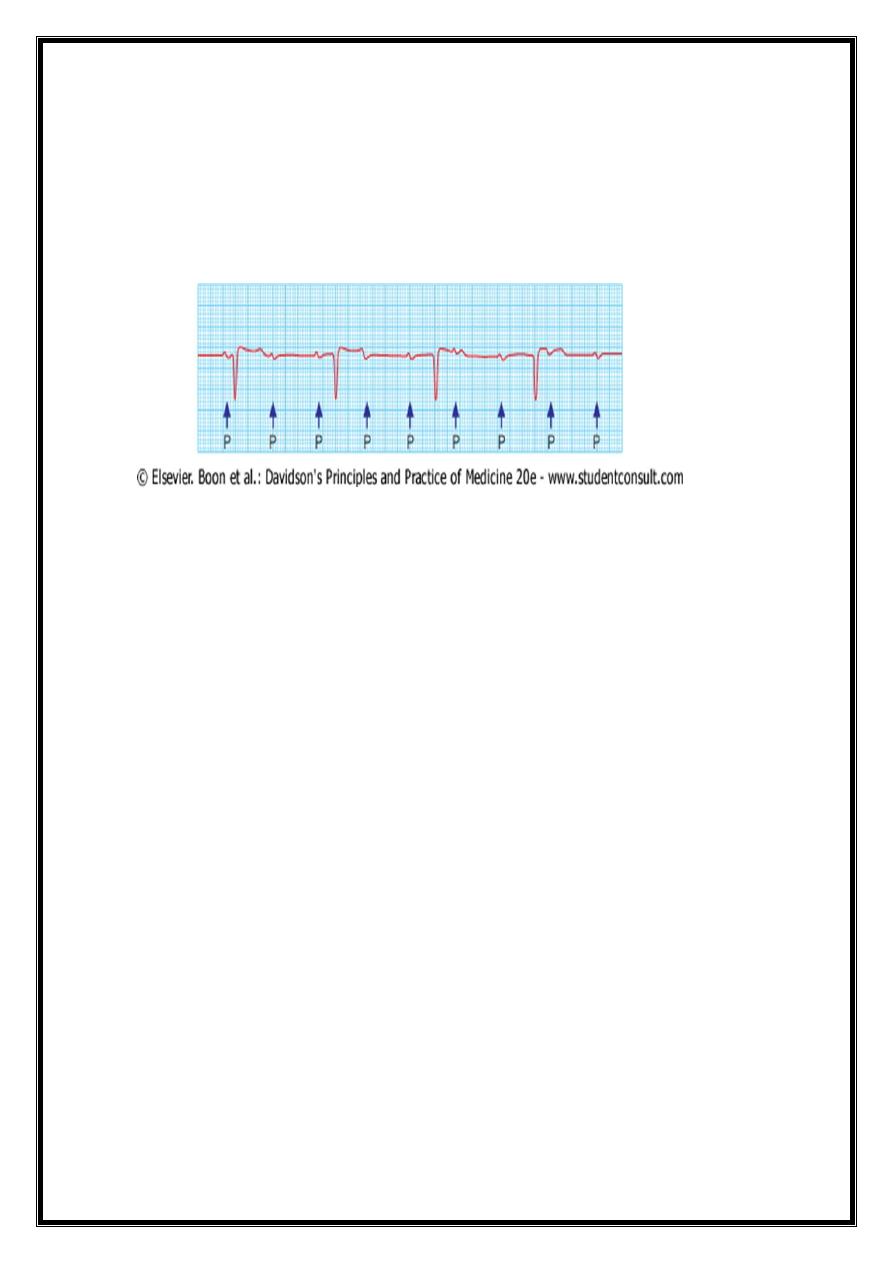
23
- the atria and ventricles beat independently (AV dissociation,
-Ventricular activity is maintained by
1- an escape rhythm arising in the AV node or bundle of His (narrow QRS complexes) or
3- the distal Purkinje tissues (broad QRS complexes). Distal escape rhythms tend to be
slower and less reliable
